Abstract
There are limited studies on the association between systemic autoimmune rheumatic diseases (SARDs) and leptospirosis. Therefore, this study aims to identify the effects of leptospirosis on the risks of developing SARDs with a nationwide retrospective cohort study. Patients with leptospirosis who did not have a diagnosis of SARDs before the index date were enrolled from the Taiwan National Health Insurance Research Database between 2000 and 2010, as the leptospirosis cohort. For each patient with leptospirosis, one control without a history of leptospirosis and SARDs was randomly selected (non-leptospirosis cohort). Cox proportional hazards regression models were used to analyze the risk of SARDs according to sex, age, and comorbidities. Among the 23 million people in the cohort, 3,393 patients with leptospirosis (68.91% men, mean age 52.65 years) and 33,930 controls were followed for 18,778 and 232,999 person-years, respectively. The incidence of SARDs was higher in the leptospirosis cohort than in the non-leptospirosis cohort (1.38 vs 0.33 per 1000 person-years), with a hazard ratio (HR) of 4.42 (95% confidence interval [CI] = 2.82–6.92). The risk of developing SARDs was highest for leptospirosis patients aged ≥65 years (HR = 2.81% CI = 1.07–7.36) compared with patients aged ≤39 years. Patients with leptospirosis have a 4.42-fold higher risk of SARDs than that in the general population. Further research is warranted to investigate the mechanism underlying this association.
Similar content being viewed by others
Introduction
Leptospirosis is a zoonotic disease caused by pathogenic spirochetes, genus Leptospira. Leptospirosis can be found globally, with a higher incidence in tropical and subtropical regions1. The pathogen can enter the host through wounds in the skin, the conjunctiva, and mucous membranes. By direct contact with the body fluids from the infected domestic and sylvatic animals, humans may also be infected. Once infected, patients can either be asymptomatic or manifested as an acute febrile illness, with fever, chills, arthralgia, headache, and severe myalgia. Occasionally, it can cause severe disease leading to multiorgan dysfunction and even death2. The nonspecific initial presentation and lack of a reliable point-of-care screening test make this disease a diagnostic challenge3,4.
Autoimmune diseases are conditions that are triggered by the immune system initiating an attack on self-molecules due to the worsening of immunologic tolerance to auto-reactive immune cells5. Both environmental and genetic are significant contributors to the pathogenesis of autoimmune diseases6. Autoimmune diseases can either be systemic, organ-specific or localized to specific tissue or region depending on the clinicopathology of each condition. Systemic autoimmune rheumatic diseases (SARDs) are a collective term for more than 80 systemic autoimmune diseases, including systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), and systemic sclerosis (SS), Sjogren’s syndrome, polymyositis, dermatomyositis. Female are inordinately affected, representing nearly 80% of people with autoimmune diseases7; for instance, the female to the male ratio of Sjögren’s syndrome or SLE were 9~10:18.
The relationship between infection and autoimmune diseases have been reported. Borrelia burgdorferi might induce chronic autoimmune disease called Lyme borreliosis9. The infection of Parvovirus B19 has been implicated in the pathogenesis of a variety of autoimmune disorders with the hallmark of inducing the production of autoantibodies in the host10. Cytomegalovirus (CMV) infections were correlated with the induction and expansion of a proinflammatory CD4+/CD28− T cells in RA patients11; and Epstein-Barr virus (EBV) was regarded as an important trigger in the pathogenesis of SLE as evidenced by the co-existence of anti-viral capsid antigen IgG and anti-dsDNA antibodies in the patients12. The relationship between leptospirosis and the development of SARDs is unclear; we thus conducted a longitudinal nationwide retrospective cohort study to investigate the occurrence of leptospirosis and the risk of developing SARDs subsequently in the same patients.
Patients and Methods
Data source
All data in this study were contained from the database retained by the National Health Research Institute, Taiwan, and were available for public access. Since no identifiable personal information was included in the database, the study was approved by the Research Ethics Committee of China Medical University and Hospital (CMUH-104-REC2-115) and waiver of informed consent was granted as well. The National Health Insurance (NHI) program, which was implemented in 1995, has covered more than 99% of the entire population (23 million residents) of Taiwan. The reliability of the database is secured since false diagnosis reports entail a high penalty. Dataset of the National Health Insurance Research Database (NHIRD) for the year 2000 to 2013 was used, including of registry of beneficiaries, the registry for catastrophic illness, and inpatients care claims released by the Taiwan National Health Research Institutes. In this study, we used the hospitalization claims data of all enrollees in Taiwan, which contained information about sex, birthday, and date of admission and discharge, diagnoses, data of inpatients visits, and diagnosis codes according to the International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM). The medical files in this subset contain all detail medical information of the patients, which include demographics, diagnoses, examinations, and drug prescription.
Exposure ascertainment
This study was a retrospective cohort study: among 3,393 patients aged 20 years and older who were newly diagnosed with leptospirosis disease (ICD-9-CM code 100.x) as recorded in the inpatients’ registry claim during the year 2000 to 2010. The new diagnosis date of leptospirosis was the index date. No diagnosis of leptospirosis patients was defined non-leptospirosis group (n = 17,308,905). Exclusion criteria included that patients less than 20 years, or missing information of sex or birthday, and diagnosed SARDs date before the index date in both cohort groups. To bolster comparability between the case of leptospirosis and non-leptospirosis patients, we randomly selected 1:10 ratios of leptospirosis and non-leptospirosis from each stratum of a combination of sex, age (per 5 years), and index years.
Study outcome
The primary outcome, newly diagnosis of SARDs, is one of the 31 categories of serious illnesses or injuries that subject the patients to Catastrophic Illness Certificate. SARDs is consisted of SLE (ICD-9-CM: 710.0), SS (ICD-9-CM: 710.1), RA (ICD-9-CM: 714.0), polyarticular juvenile RA (ICD-9-CM: 714.30~714.33), polymyositis (ICD-9-CM: 710.4), dermatomyositis (ICD-9-CM: 710.3), vasculitis (included polyarteritis nodosa, ICD-9-CM: 446.0), hypersensitivity angiitis (ICD-9-CM: 446.2), Wegener’s granulomatosis (ICD-9-CM: 446.4), giant cell arteritis (ICD-9-CM: 446.5), thromboangiitis obliterans (ICD-9-CM: 443.1), Takayasu’s disease (ICD-9-CM: 446.7), acute febrile mucocutaneous lymph node syndrome (ICD-9-CM: 446.1), Behcet’s syndrome (ICD-9-CM: 136.1), pemphigus (ICD-9-CM: 694.4), sicca syndrome (ICD-9-CM: 710.2), Crohn’s disease (ICD-9-CM: 555), and ulcerative colitis (ICD-9-CM: 556.0~556.6, 556.8~556.9). Each participant was followed up from index date to the date of incident SARDs, or withdrawal from NHI, or until December 31, 2013, whichever occurred first. Patients with inpatients’ claim reporting a history of diabetes mellitus (ICD-9-CM: 250.x), hypertension (ICD-9-CM: 401–405), coronary artery disease (ICD-9-CM: 410–414), and cerebrovascular disease (ICD-9-CM: 430–438) identified before the index date, were considered as potential confounders in this study.
Statistical analysis
The descriptive table was used to examine the baseline characteristics of the study cohort groups. We used the chi-square test for categorical variables and the t-test for continuous variables. We evaluated the Hazard Ratios (HRs) and 95% confidence interval (95% CI) for each variable using the Cox proportional hazards model. We estimated the cumulative risk of SARDs for both cohort by using the Kaplan-Meier method, and the log-rank test was used to assess the significance of the cumulative risk curves. All statistical analyses were performed with SAS statistical analysis software, version 9.4 (SAS Institute Inc, Cary, North Carolina), and the significance level was set at 0.05.
Result
Characteristics of the participants
A total of 3,393 patients with leptospirosis and 33,930 matched patients without leptospirosis were included in the study. The mean (±SD) ages of the leptospirosis cohort and non-leptospirosis cohort were 52.65 (±16.52) years old and 52.59 (±16.57) years old, respectively. The proportion of male and female were 68.91% and 31.09%, respectively. The proportion of diabetes, hypertension, coronary artery disease and cerebrovascular disease in leptospirosis cohort were higher than non-leptospirosis cohort. Table 1 summarized the demographic characteristics and baseline comorbidities of the subjects. The mean (median) of the follow-up periods was 5.53 (5.63) years and 6.87 (7.00) years for leptospirosis cohort and compared cohort group, respectively.
Associations in subgroups
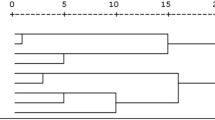
The leptospirosis patients had a higher cumulative incidence of developing SARDs when compared to the comparison cohort during the follow-up period (Log-rank test, p < 0.0001, Fig. 1). Table 2 shows the uni- and multivariate Cox’s proportional hazard model. In univariate analysis, there was a 4.16-fold higher risk of SARDs in the study cohort compared with the comparison cohort (crude HR = 4.16, 95% CI = 2.67–6.50). After adjusted for age, gender, and comorbidities (included diabetes, hypertension, coronary artery disease, and cerebrovascular disease), leptospirosis patients had a higher risk of SARDs than the non-leptospirosis patients (adjusted HR = 4.42, 95% CI = 2.82–6.92).
Incidence rate
We determined the incidence of SARDs in leptospirosis and non-leptospirosis cohorts, and the result indicated that patients with leptospirosis had a higher significant risk of SARDs (Table 3). Incidence rates (per 1,000 person-years) of SARDs were 1.38 and 0.33 for leptospirosis cohort and non-leptospirosis cohort, respectively. The incidence of SARDs with leptospirosis cohort were 2.55 and 0.85 (per 1,000 person-years) for female and male, respectively, which was higher than non-leptospirosis cohort. Besides, female showed 4.37-fold (95% CI: 2.43–7.87), and male showed 4.63-fold (95% CI: 2.31–9.26) higher risk of developing SARDs than the compared cohort. Leptospirosis had a higher risk of SLE (adjusted HR: 10.48, 95% CI: 3.47–31.67) and SS (adjusted HR: 10.15, 95% CI: 1.62–63.71) than non-leptospirosis cohort (Supplementary Table 1).
Discussion
The etiology of the majority of autoimmune diseases is not well-defined. Some factors, which include genetics, environmental toxins, and the microbiome, can influence or induce autoimmunity13,14,15. The inappropriate immune activation which targets to self-antigens causes sustainable pathologies that make an individual subjected to a various grade of autoimmune diseases. Some pathogens have been reported to be associated with the pathogenesis of autoimmune disorders16,17. These infectious agents trigger autoimmune diseases via various mechanisms. Many bacterial infections have been related to the development of autoimmune-like response and resulting as an essential clinical problem18.
The proposed mechanisms include molecular mimicry, which antibodies against bacterial antigens that are similar to the host19. For example, autoimmune diseases such as Crohn’s disease, ulcerative colitis, and sarcoidosis are commonly found in Mycobacterium tuberculosis patients20. Streptococcus pyogenes infection can lead to rheumatic heart disease, while Chlamydia and Campylobacter bacteria cause reactive arthritis21. These associations between various bacterial infections and SARDs consist of the observation herein that leptospiral infection is a crucial factor for the risk of autoimmune disease. It has been proposed that antibiotics that are customarily prescribed for treating infectious pathogens can offer effects upon curing/alleviating autoimmune diseases22,23.
To date, there have been few studies evaluating the exposure of spirochete infection in newly diagnosed autoimmune disease. A high frequency of Borrelia burgdorfeii infections complicating autoimmune symptom, especially arthritis, has been reported previously24. Treponema denticola causes periodontitis and induces RA25. The other type of spiral bacteria-Campylobacter jejuni has also been reported to be associated with an autoimmune post-infectious polyradiculoneuropathy called Guillain Barre Syndrome26. Our study showed that SARDs occurred more frequently among patients with leptospirosis. Using a nationwide retrospective cohort database, our study is the first to reveal that patients with leptospirosis exhibited a 4.42-fold greater risk of developing subsequent SARDs than that of the general population (Table 2). Our findings are etiologic importance, which may offer useful predictive information for future clinical management.
The prevalence of autoimmune diseases in the female is higher than male27,28. In this report, we found that the HR of SARDs associated with leptospirosis is similar in female and male (Table 3, F/M: 4.37/4.63). The incidence ratio (IR) of SARDs in both non-leptospirosis (Table 3, F/M:0.64/0.19) and leptospirosis (Table 3, F/M: 2.55/0.85) are higher in the female. Some reports suggested that sex hormones might mediate the immune response by alternating T cell development and function29. Sex-based changes due to environmental factors or exposure to sex hormones could modify the induction of various autoimmune diseases27,28,30. Thus, it is very important to elucidate whether sex hormones are among the risk factors in leptospirosis patients that subsequently developing SARDs.
We further demonstrated that age was an independent predictor for newly diagnosed SARDs in patients with leptospirosis (Table 3). Previous studies demonstrated a more severe symptom of leptospirosis in adult as compared with infected children, and male predominance of severe leptospirosis in children and adolescents was also noted31. It is noteworthy that both analyses identified age as an independent variable associated with an increased risk of leptospirosis. We further identified a significantly high risk of young age with leptospirosis associated SARDs (Table 3. Crude HRs of age 20/40/65:12.88/3.8/2.68). In leptospiral infection, it was reported that patients with mild leptospirosis had a background level of pre-existing IgG, while patients with severe leptospirosis demonstrated a gradual increase of IgM antibody profile typical of first exposure32. Pre-existing IgG against leptospira is suspected to be protective against severe clinical manifestations.
In general, leptospiral infection is associated with increased susceptibility to SARDs. However, no sufficient data exists for the effect of age on the risk of developing SARDs; our study demonstrated that the presence of the leptospiral infection in elderly with SARDs. The mechanism may be due to abnormalities of the host immune response, particularly immune senescence, resulted in many inflammatory responses, increasing susceptibility to infections, and enhancing the production of autoantibodies33. Another possible explanation is the expansion of many protective regulatory mechanisms in the elderly (e.g., higher production of peripheral T-regulatory cells), resulting in higher autoimmunity but yet a lower prevalence of autoimmune diseases34. The decrease of thymic T-regulatory cells has been reported in association with the loss of thymic capacity to generate new T cells in the elderly35, which could be a hint that people with older age tend to have an inadequacy in response to pathogens. These premises need to be explored in the future by recruiting more younger patients for additional analysis.
Limitation
The present study is not without its limitations: firstly, we have performed analysis by disease subtypes-SLE, RA, vasculitis, and Sicca syndrome, in our non-leptospirosis and leptospirosis cohorts (Supplementary Table 1), however, the sample size is too small to reach an apparent conclusion. We found that leptospirosis had a higher risk of SLE (adjusted HR: 10.48, 95% CI: 3.47–31.67), and SS (adjusted HR: 10.15, 95% CI: 1.62–63.71) than non-leptospirosis cohort. Secondly, no data were available on medical history, lifestyle, and vaccination status of the enrollees, raising concerns about the involvement of other residual confounding factors. Thirdly, leptospirosis is diagnosed on clinical grounds and confirmed by microscopic agglutination test (MAT) or polymerase chain reaction (PCR) practically. However, the retrieval data from the National Health Insurance Database is based on clinical diagnosis (ICD-9 code) judged by the physicians; thus, it is not a confirmed diagnosis. The correlation between leptospirosis and the subsequent SARDs has to be validated in the future.
References
Levett, P. N. Leptospirosis. Clin. Microbiol. Rev. 14, 296–326 (2001).
Haake, D. A. & Levett, P. N. Leptospirosis in humans. Curr. Top. Microbiol. Immunol. 387, 65–97 (2015).
Dittrich, S. et al. A Prospective Hospital Study to Evaluate the Diagnostic Accuracy of Rapid Diagnostic Tests for the Early Detection of Leptospirosis in Laos. Am. J. Trop. Med. Hyg. 98, 1056–1060 (2018).
Toyokawa, T., Ohnishi, M. & Koizumi, N. Diagnosis of acute leptospirosis. Expert. Rev. Anti. Infect. Ther. 9, 111–121 (2011).
Smith, D. A. & Germolec, D. R. Introduction to immunology and autoimmunity. Environ. Health. Perspect. 107(Suppl 5), 661–665 (1999).
Ceccarelli, F., Agmon-Levin, N. & Perricone, C. Genetic Factors of Autoimmune Diseases. J. Immunol. Res. 2016, 3476023 (2016).
Fairweather, D. & Rose, N. R. Women and autoimmune diseases. Emerg. Infect. Dis. 10, 2005–2011 (2004).
Saccucci, M. et al. Autoimmune Diseases and Their Manifestations on Oral Cavity: Diagnosis and Clinical Management. J. Immunol. Res. 2018, 6061825 (2018).
Singh, S. K. & Girschick, H. J. Lyme borreliosis: from infection to autoimmunity. Clin. Microbiol. Infect. 10, 598–614 (2004).
Kerr, J. R. The role of parvovirus B19 in the pathogenesis of autoimmunity and autoimmune disease. J. Clin. Pathol. 69, 279–291 (2016).
Halenius, A. & Hengel, H. Human cytomegalovirus and autoimmune disease. Biomed. Res. Int. 2014, 472978 (2014).
Chougule, D. et al. Association of clinical and serological parameters of systemic lupus erythematosus patients with Epstein-Barr virus antibody profile. J. Med. Virol. 90, 559–563 (2018).
Ramos, P. S., Shedlock, A. M. & Langefeld, C. D. Genetics of autoimmune diseases: insights from population genetics. J. Hum. Genet. 60, 657–664 (2015).
Vojdani, A. A Potential Link between Environmental Triggers and Autoimmunity. Autoimmune. Dis. 2014, 437231 (2014).
Vojdani, A., Pollard, K. M. & Campbell, A. W. Environmental triggers and autoimmunity. Autoimmune. Dis. 2014, 79802 (2014).
Picchianti-Diamanti, A., Rosado, M. M. & D’Amelio, R. Infectious Agents and Inflammation: The Role of Microbiota in Autoimmune Arthritis. Front. Microbiol. 8, 2696 (2017).
Winston, A. et al. Host and disease factors are associated with cognitive function in European HIV-infected adults prior to initiation of antiretroviral therapy. HIV. Med. 17, 471–478 (2016).
Chervonsky, A. V. Influence of microbial environment on autoimmunity. Nat. Immunol. 11, 28–35 (2010).
Rivera-Correa, J. & Rodriguez, A. Divergent Roles of Antiself Antibodies during Infection. Trends. Immunol. 39, 515–522 (2018).
Elkington, P., Tebruegge, M. & Mansour, S. Tuberculosis: An Infection-Initiated Autoimmune Disease? Trends. Immunol. 37, 815–818 (2016).
Ercolini, A. M. & Miller, S. D. The role of infections in autoimmune disease. Clin. Exp. Immunol. 155, 1–15 (2009).
Yossi, R., Merav, L. & Yehuda, S. Antibiotic therapy in autoimmune disorders. Clinical. Practice. 11, 91–103 (2014).
Cristina, R. Chapter 16 - Can Antibiotics Cure Autoimmune Diseases? Infection and Autoimmunity (Second Edition). 279–298. (2015).
Arvikar, S. L., Crowley, J. T., Sulka, K. B. & Steere, A. C. Autoimmune Arthritides, Rheumatoid Arthritis, Psoriatic Arthritis, or Peripheral Spondyloarthritis Following Lyme Disease. Arthritis. Rheumatol. 69, 194–202 (2017).
Lee, A. et al. Treponema denticola enolase contributes to the production of antibodies against ENO1 but not to the progression of periodontitis. Virulence. 9, 1263–1272 (2018).
Willison, H. J., Jacobs, B. C. & van Doorn, P. A. Guillain-Barre syndrome. Lancet. 388, 717–727 (2016).
Pennell, L. M., Galligan, C. L. & Fish, E. N. Sex affects immunity. J. Autoimmun. 38, J282–291 (2012).
Tiniakou, E., Costenbader, K. H. & Kriegel, M. A. Sex-specific environmental influences on the development of autoimmune diseases. Clin. Immunol. 149, 182–191 (2013).
Brown, M. A. & Su, M. A. An Inconvenient Variable: Sex Hormones and Their Impact on T Cell Responses. J. Immunol. 202, 1927–1933 (2019).
Edwards, M., Dai, R. & Ahmed, S. A. Our Environment Shapes Us: The Importance of Environment and Sex Differences in Regulation of Autoantibody Production. Front. Immunol. 9, 478 (2018).
Guerrier, G. et al. Association between age and severity to leptospirosis in children. PLoS. Negl. Trop. Dis. 7, e2436 (2013).
Lessa-Aquino, C. et al. Distinct antibody responses of patients with mild and severe leptospirosis determined by whole proteome microarray analysis. PLoS. Negl. Trop. Dis. 11, e0005349 (2017).
Ma, S., Wang, C., Mao, X. & Hao, Y. B Cell Dysfunction Associated With Aging and Autoimmune Diseases. Front. Immunol. 10, 318 (2019).
Vadasz, Z., Haj, T., Kessel, A. & Toubi, E. Age-related autoimmunity. BMC. Med. 11, 94 (2013).
Fessler, J., Ficjan, A., Duftner, C. & Dejaco, C. The impact of aging on regulatory T-cells. Front. Immunol. 4, 231 (2013).
Acknowledgements
We want to express our greatest gratitude to Dr. Ling-Yi Wang, Epidemiology and Biostatistics Consulting Center, Hualien Tzu Chi General Hospital, Buddhist Tzu Chi Medical Foundation, Hualien, Taiwan, for her assistance in statistical analysis and critical review of this manuscript. This study is supported in part by the Taiwan Ministry of Health and Welfare Clinical Trial Center (MOHW108-TDU-B-212-133004), China Medical University Hospital, Academia Sinica Stroke Biosignature Project (BM10701010021), MOST Clinical Trial Consortium for Stroke (MOST 108-2321-B-039-003-), Tseng-Lien Lin Foundation, Taichung, Taiwan, and Katsuzo and Kiyo Aoshima Memorial Funds, Japan.
Author information
Authors and Affiliations
Contributions
Study conception and design: S.H.T., R.I.Y., Y.C.Y., C.Y.H., C.Y.P. Acquisition of data: Y.C.Y. Drafting and writing of the manuscript: S.H.T., R.I.Y., Y.C.Y., C.Y.P.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Teh, SH., You, RI., Yang, YC. et al. A cohort study: The Association Between Autoimmune Disorders and Leptospirosis. Sci Rep 10, 3276 (2020). https://doi.org/10.1038/s41598-020-60267-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-60267-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.