Abstract
Exposure to childhood adverse events is associated with severe consequences for general health and structural and functional changes in the brain of its survivors. In order to unravel and in the end influence the pathway linking adversity and pathology, neuroimaging research is crucial. Up till now studies in minors are scarce and differ in type of adversity or methodology. Almost all studies report lower cortical thickness, but in a broad variety of regions. In this study we investigated cortical thickness measures and clinical data in a well circumscribed group of adolescents with PTSD related to childhood sexual abuse (CSA) (N = 21) and a healthy non-traumatised control group (N = 21). The ventromedial PFC (vmPFC), ACC, insula, and middle/superior temporal gyrus were chosen as ROI’s due to their respective roles in emotion and information processing. No significant effect of group was found for cortical thickness, surface area or volume in any of the ROIs. This is in line with the results of research in adult women with sexual abuse related PTSD, suggesting that this may be specific to this group, independent of age. Recent research points to differential biological and pathological consequences of different types of childhood adversity.
Similar content being viewed by others
Introduction
The experience of traumatic events in childhood is a strong predictor of psychiatric and somatic pathology later in life1,2,3, with substantial consequences for general health4,5. Recent epigenetic research further demonstrated the substantial impact of stress and trauma on the next generation6. In order to counter the negative effects of childhood psychological trauma, it is necessary to understand the neurobiological processes related to these trajectories. Results from preclinical and human studies link stress hormones like cortisol to structural changes in the brain, reflecting underlying alterations in neuron density and microstructure7,8,9. Psychological processes like threat processing, heightened emotional reactivity and altered emotional learning are thought to mediate between trauma exposure, structural changes in the brain and later psychopathology10. Understanding the developing and still malleable child or adolescent brain after trauma could provide an approach for thwarting negative consequences, particularly because even the adult brain is considered to be susceptible for structural changes after therapeutic interventions11,12. Structural neuroimaging research in traumatised children and adolescents may help to elucidate the effects of childhood adverse events on brain development, however, up till this moment such studies are scarce13.
Meta-analyses of structural MRI studies in adults with PTSD have reported smaller gray matter volume (GMV) in emotion and threat processing structures like the hippocampus, the anterior cingulate cortex (ACC) and the medial prefrontal cortex (mPFC)14,15. Apart from a smaller corpus callosum (CC), results of structural MRI studies in traumatised C&A however, are mixed and inconclusive13. Results from neuroimaging studies in adult victims of childhood trauma thus differ from findings in traumatised minors. While studies in adults with a history of childhood abuse or neglect consistently report smaller volume of the hippocampus compared to non-traumatised controls, this has not been replicated in minors16,17. In contrast, the decrease in volume of the corpus callosum, has consistently been reported in children and adolescents, but not in adults who have experienced childhood trauma18,19. Clearly, more research is needed in order to understand the neurodevelopmental trajectories related to trauma leading to the negative consequences in adulthood.
This study is part of the Emotional Pathways’ Imaging Study in Clinical Adolescents (EPISCA) project. Earlier research with the same groups, using VBM (Voxel Based Morphometry), DTI (Diffusion Tensor Imaging) and functional MRI techniques, have been published19,20,21,22,23,24,25,26 Cortical thickness is a relatively new neuroimaging analysis technique, which is considered complementary to VBM in studying grey mater integrity27.
Smaller cortical thickness in adult traumatised populations, mostly PTSD patients, has been reported in various brain regions like the mPFC, the ACC, the insula, and the superior and middle temporal gyrus28,29,30,31. Some studies even found an inverse correlation between cortical thickness and symptom severity28,32. A study in adult women with sexual abuse related PTSD, similar to our adolescent group, showed normal cortical thickness compared to healthy controls33. Greater cortical thickness has been associated with resilience in adults34,35. For those reasons, it is relevant to study cortical thickness in traumatised children and adolescents as well.
Cortical thickness studies in traumatised minors are, however, limited and show little concordance. To our knowledge there are only ten studies on cortical thickness in traumatised minors, almost all adolescents. In contrast to adult trauma research only two of these ten studies report about PTSD patients36,37, the others included minors having experienced different types of adversity. Studies found smaller cortical thickness, but not consistently, in several regions including the mPFC38,39,40,41,42, ACC36,43,44, insula36,37,45 temporal regions38,39,41, other frontal regions39,42,43,44,45 parahippocampal regions39 and parietal regions41,42 Exceptions are reported by Whittle et al.42 who compared maltreated with non-maltreated adolescents and found an association of maltreatment with accelerated as well as less thinning in frontal and precentral regions, and by Ahmed et al.36 who compared traumatised adolescents with and without PTSD and reported no significant difference in cortical thickness between groups in the insula, ACC, amygdala, CC and hippocampus using Freesurfer technique and a reduction in insula thickness when using Qdec. No clear distinction can be made between results from studies with inclusion based on the presence of PTSD or the presence of different types of trauma. Results of studies may vary due to differences in age and type of adversity.
In order to further elucidate the impact of trauma on the developing brain, we decided to examine cortical thickness, surface area and volume in our EPISCA sample, a well-defined group of adolescents with posttraumatic stress disorder based on childhood sexual abuse (CSA) with measures in non-traumatised controls. Based on the literature, we hypothesized differences in the following regions of interest (ROIs): the ventromedial PFC (vmPFC), ACC, insula, and middle/superior temporal gyrus, regions that are considered to play a role in emotion and information processing.
Methods
Participants
Participants were selected from the Emotional Pathways’ Imaging Study in Clinical Adolescents (EPISCA). EPISCA is a longitudinal MRI study in which adolescents with clinical depression, adolescents with a history of sexual trauma and healthy controls were followed over a six-month period in which they received treatment. The adolescents were assessed and underwent scanning at three time points: upon inclusion at baseline, three months after baseline, and six months after baseline20,46. The current study reports on cross-sectional baseline data from the adolescents with a history of sexual trauma and healthy non-traumatised controls. See also previous reports from neuroimaging research with the same population19,20,21,22,23,24,25,26. Inclusion criteria for the adolescents with a history of sexual trauma were: having experienced sexual abuse during their lifetime more than once by one or more perpetrators inside or outside the family, and being referred for treatment to the Psychotrauma Center of mental health institute GGZ Rivierduinen in Leiden or the child and adolescent psychotrauma center KJTC in Haarlem, both located in the Netherlands. Experienced psychotherapists in these specialised psychotrauma centers obtained the trauma histories from the adolescents as well as from their caregivers during clinical interviews. To objectify any abuse or neglect as well as risk for functional impairment and morbidity, we verified police reports, involvement of child welfare, and family custody or other child protection measures as to have an estimate of the severity and impact of problems. (For more details about the participants in the CSA- group see van Hoof et al.46).
Presence of PTSD was not an inclusion criterion, although clinical assessments (see below) showed that all patients but one were diagnosed with PTSD related to CSA. Inclusion criteria for the control group were: no current or past DSM-IV classifications, no clinical scores on validated mood and behavioural questionnaires, no history of traumatic experiences, and no current psychotherapeutic and/or psychopharmacological intervention of any kind. Exclusion criteria for all participants were: primary DSM-IV clinical diagnosis of attention-deficit hyperactivity disorder (ADHD), oppositional defiant disorder (ODD), conduct disorder (CD), pervasive developmental disorders, Tourette’s syndrome, obsessive–compulsive disorder, bipolar disorder, and psychotic disorders; current use of psychotropic medication other than stable use of SSRI’s, or amphetamine medication, but not on the day of scanning; current substance abuse; history of neurological disorders or severe head injury; age <12 or >21 years; pregnancy; left-handedness; IQ score <80 as measured by the Wechsler Intelligence Scale for Children (WISC)47 or adults48; and general MRI contraindications.
Fifty-four participants were included in the study: 32 healthy non-traumatised controls and 22 patients with a history of sexual trauma. From this group, two controls were excluded because of technical problems during scanning or poor imaging data quality, one participant with CSA because of complete segmentation failure. One control was excluded due to high scores on clinical symptom rating scales, and one control was excluded due to a history of sexual trauma that was not reported until the day of scanning. This resulted in a final sample of 21 adolescents with CSA and 28 controls.
Of the 21 CSA-participants, 20 fulfilled all PTSD criteria on the ADIS, while one had sufficient PTSD symptoms, but with limited interference. Since earlier research showed that persons with sub threshold PTSD in many aspects resemble PTSD patients, we decided to include this patient in the (CSA-related) PTSD group49.
The study was approved by the Medical Ethics Committees of the Leiden University Medical Center and written informed assent and consent was obtained from the participants and their parents respectively.
Clinical assessment
A standardized set of instruments was used to assess symptomatology in both groups of adolescents.
The Anxiety Disorders Interview Schedule Child and Parent Versions (ADIS-C/P)50 are semi structured interviews for the classification of DSM-IV anxiety and depressive disorders in children. Classification is reached by a minimal interference score of 4 obtained by trained examiners based on the ADIS-C and ADIS-P. The ADIS is known to have good reliability and validity51 with reported strong test–retest reliability statistics for the ADIS-C/P for combined diagnoses (0.80–0.92) and individual diagnoses (0.62–0.88). The Trauma Symptom Checklist for Children (TSCC)52 is a 54-item self-report for children and adolescents aged 8 through 18 but often used up to 21 years53,54 which measures trauma-related symptoms. On a 4-point scale (never to almost all of the time), the adolescent indicates how often a thought, a feeling or a behaviour occurs. The items are grouped into six clinical scales. The clinical scales are Anxiety (Anx), Depression (Dep), Post-traumatic Stress (Pts), Sexual Concerns (Sc), Dissociation (Dis) and Anger (Ang). The TSCC total score is used as the main measure on post-traumatic symptomatology. Cronbach’s alpha coefficients reported range from 0.77 to 0.89 for subscales and 0.84 for the total scale. The questionnaire has extensively been studied, which has confirmed its good psychometric qualities55,56. The internal consistency of the TSCC subscales varied between 0.85 and 0.94, except for the Sexual Concerns subscale that measured 0.68.
The Adolescent Dissociative Experiences Scale (A-DES) contains 30 items to assess adolescents of 11–18 years of age for pathological dissociation. The A-DES items inquire about four domains reflecting basic aspects of dissociation: experiences of dissociative amnesia, depersonalization/derealisation, absorption/imaginative involvement and passive influence. The items are rated by the adolescent on an 11-point Likert-scale ranging from 0 = “never” to 10 = “always” with no midpoint scores. The total A-DES score is based on the mean of all item scores. A mean score of 4 or above on the A-DES signifies pathological dissociation57. The scale has good internal reliability and validity.
As brain development is known to be influenced by sexual development, corporal sexual development was measured with the self-report Puberty Development Scale58. The PDS consists of 5 items that are measured on a 5-point scale by the examiner: 1= pre-pubertal, 2= early pubertal, 3= mid-pubertal, 4= late pubertal, 5= post-pubertal. The PDS is considered a valuable instrument determining pubertal stage59,60.
Six subscales from the Wechsler Intelligence scales scores (picture completion, similarities, picture concepts, arithmetic, block design and comprehension) were converted into Full IQ estimates20,46.
All methods were performed in accordance with the relevant guidelines and regulations.
MRI data acquisition
Images were acquired on a Philips 3T magnetic resonance imaging system (Philips Healthcare, Best, The Netherlands), equipped with a SENSE-8 head coil. Scanning took place at the Leiden University Medical Center. Prior to scanning, all participants were introduced to the scanning situation by lying in a dummy scanner and hearing scanner sounds. For each subject, a sagittal 3-dimensional gradient-echo T1-weighted image was acquired (repetition time = 9.8 ms; echo time = 4.6 ms; flip angle = 8°; 140 sagittal slices; no slice gap; field of view =256 × 256 mm; 1.17 × 1.17 × 1.2 mm voxels; duration =4:56 min) as part of a larger, fixed imaging protocol.
Image processing and analysis
Cortical parcellations of 68 cortical grey matter regions, 34 regions in each cerebral hemisphere, were performed using FreeSurfer (Software version 5.3.0) based on the Desikan-Killiany atlas. In addition, two whole-hemisphere measures were extracted using FreeSurfer. The segmentations of all 68 cortical grey matter regions and the two whole-hemisphere measures were followed by a statistical outlier assessment and a visual inspection for artefacts and abnormal clinical findings, which was done independently by three different researchers using standardized ENIGMA-protocol: http://enigma.ini.usc.edu/protocols/imaging-protocols/protocol-for-quality-control-and-summary-statistics/ After visual inspection, both the left and right insula were excluded from further analyses due to frequent inadequate or complete failure of segmentation.
Statistical analyses
Statistical analyses for all data were performed with the Statistical Package for Social Sciences Software (SPSS, version 25). Demographic and clinical characteristics were analysed using independent-sample t-tests. If the data did not meet the assumptions necessary for parametric analyses, which was the case for the total scores on the A-DES and TSCC, the non-parametric Mann-Whitney U-test was used. Categorical variables were assessed with the Chi-square test. All tests were performed with the significance set at p < 0.05.
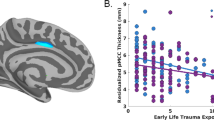
Total volume for each ROI was calculated by multiplying cortical thickness with surface area. The effect of PTSD on cortical morphometric measures in all ROIs was tested using a multivariate analyses of covariance (MANCOVA). Considering that age and intracranial volume are strongly correlated with cortical measures, both were included as covariates61. In line with previous research, puberty development (PDS score) was also accounted for in the model19. Three separate MANCOVAs were used to assess group differences, one for cortical thickness, one for surface area and one for volume of the selected ROI as dependent factors. Therefore, we corrected for multiple testing by dividing the p-value of 0.05 by 3 (p < 0.017). The ROIs included left and right ACC (caudal and rostral ACC in Freesurfer), middle temporal gyrus, superior temporal gyrus, vmPFC (medial orbitofrontal cortex in FreeSurfer). (Fig. 1). Post-hoc, between-group effects were correlated with symptom severity scores within the CSA-related PTSD group. Post-hoc, between-group effects were correlated with symptom severity scores within the CSA-related PTSD group.
Regions of Interest (ROIs): medial orbitofrontal (MOF), caudal anterior cingulate cortex (CAcc), rostral anterior cingulate cortex (RAcc), superior temporal gyrus (STG), middle temporal gyrus (MTG). The left and right insula were excluded from further analyses due to frequent inadequate or complete failure of segmentation.
Results
Sample characteristics
The means and standard deviations of demographic and clinical characteristics are presented in Table 1. The majority of participants was female (85.7%). The adolescents with CSA-related PTSD had a significantly lower TIQ (mean 99.3, SD 8.8) than controls (mean 107.0, SD 8.3) [t(47)= −3.120, p = 0.003]. In addition, adolescents with PTSD (mean 16.4, SD 2.0) were significantly older than controls (mean 15.2, SD 1.6) [t (47)=−2.338, p = 0.024]. As expected, there was a significant difference between the total scores on the A-DES and TSCC between adolescents with CSA-related PTSD and healthy non-traumatised controls, with a higher mean total score for CSA-participants. There was one adolescent in the CSA-related PTSD group with comorbid anxiety disorder not otherwise specified. Among the adolescents with CSA, 2 adolescents were on SSRI treatment and 2 used amphetamines, the latter were not used on the day of the MRI scan.
Cortical thickness, surface area and volume
Differences in cortical thickness, surface area and volume between adolescents with CSA-related PTSD and non-traumatised controls were assessed in the selected ROI. Overall, no significant effect of group was found in the MANCOVAs for cortical thickness (F(10,35) = 1.130, p = 0.369) (Table 2), surface area (F(10,35) = 0.850, p = 0.586) (Table 3) or volume (F(10,35) = 1.050, p = 0.425) (Table 4). Excluding the 2 CSA-participants that were using medication from the analyses did not change the results.
Also, excluding the one CSA-participant with sufficient PTSD symptoms, but limited interference from the analyses, did not change the results. As the CSA-related PTSD group had a significant lower TIQ than the controls, we report correlations with IQ within groups in the Supplementary Material Table S1. There were no significant correlations. There were significant correlations between PDS scores and age (Pearson’s r.632; p 0.001) and between PDS scores and ICV (Pearson’s r-0.298; p 0.005). There was no significant correlation between age and ICV (Pearson’s r-0.250). The variance inflation factor (VIF) between these three variables varied between 1.07 and 1.66, which indicates that there was low multicollinearity. As age, ICV and PDS were all included as covariates in the primary model, we did not perform any post hoc analysis in which one of these covariates was omitted. In addition, in post hoc analysis we tested for associations between structural brain measures and TSCC and ADES scores. These analyses only showed a significant overall correlation between regional volume and TSCC score. However, this result failed to reach significance when correcting for multiple comparisons. (Supplementary Material Table S2). Post hoc, we performed a power analysis based on comparable studies in the literature and concluded that the effect size is in the range of comparable studies. (Suplementary Material Analysis A1).
Whole brain analysis
The exploratory whole-brain analysis did not reveal any overall differences in cortical thickness, surface area and volume between CSA-related PTSD and controls (cortical thickness (F(1,44) = 1.093, p = 0.656), surface area (F(1,44) = 0.885, p = 0.706) or volume (F(1,44) = 3.596 p = 0.339)). Also, there were no significant regional differences when corrected for multiple comparisons.
Discussion
This study investigated cortical thickness, surface area and volume in a group of adolescents with CSA-related PTSD and a group of healthy non-traumatised controls. In contrast to our hypothesis, we found no significant difference between the two groups on any cortical morphometric measure in the ventromedial prefrontal cortex, anterior cingulate gyri, middle temporal gyri and superior temporal gyri.
To our knowledge this is the first study investigating cortical thickness in a group of minors with childhood sexual abuse. Up to this moment, cortical thickness studies in traumatised children and adolescents are scarce and mostly report smaller cortical thickness, but in a broad variety of regions. There are many methodological differences that hamper direct comparison of these studies, including selection of participants and controls, type of abuse, imaging parameters and methodology. There is one other study in minors, investigating traumatised adolescents with and without PTSD, which reported no abnormalities in cortical thickness in the insula, ACC, amygdala, CC and hippocampus36. However, in contrast to our study, this study included various types of trauma.
Our previous VBM study in the same population of the EPISCA project found smaller volumes of the dorsal ACC compared to healthy controls22. The current study does not implicate the ACC, but has used a different technique with a different delineation of cortical areas, which might explain the discrepancy in results.
Studies in traumatised adults, mostly in male war veterans with PTSD, consistently show reduced cortical thickness in several regions, such as the ACC and mPFC. In traumatised minors smaller ACC volume is not consistently reported13. Remarkably, however, the only study in a sample of adult women with sexual abuse related PTSD by Landré et al., similar to our study found normal cortical thickness compared to healthy controls33. The authors hypothesize that apart from gender, the specific type of trauma (i.e. sexual abuse versus combat related) might explain this difference with most other studies on trauma in adults. Interestingly, Heim et al. studied the cortical thickness in a sample of adult women with different forms of childhood abuse. They found in their adult sample that childhood sexual abuse was specifically associated with thinning of the somatosensory cortex representing the clitoris and the surrounding female genital area. In contrast to our study, they used a vertex based whole brain analysis and their sample consisted of adult women with CSA with and without depression or PTSD, potentially including resilient women62.
Apart from the methodological heterogeneity of studies, the dynamics of growth and development typically appearing in the brains of children and adolescents may in part explain the equivocal results in the literature. (See for example Weems et al. for the development of the amygdala in youth in relation to stress63).
In general, there is a growing awareness that different types of adversity may have different neurobiological sequelae and subsequent psychiatric and somatic disorders64,65. For instance, dysregulation of the immune system has been suggested by recent research as a possible biological mediator between adverse childhood experiences (ACE) and adulthood pathology. Baumeister et al., in a recent meta-analysis, conclude that there is strong evidence for the impact of ACE on the inflammatory immune system, where specific types of trauma (sexual, physical or emotional abuse) differentially impact on specific inflammatory markers and potentially pathogenic pro-inflammatory phenotypes associated with physical and mental illnesses66. The increased immune activation might be caused by changes in epigenetic regulation of gene expression. This appears plausible because of the considerable evidence for association of modifications of HPA- and neuroplasticity-related methylation patterns with childhood trauma67. Trauma specific research could thus contribute to more explicit implementation of interventions that reduce long term risks of childhood adversity and help defining specific treatments for children and adult survivors with psychopathology.
We believe that our study has several strengths. Although this was not an inclusion criterion, all participants in our study met DSM-IV criteria for PTSD, signalling that it is a clinically robust group. This study is part of the EPISCA project, in which we investigated the same groups with other structural and functional neuroimaging techniques that yielded results that were in line with the existing literature19,20,21,22,23,24. The homogeneous and well circumscribed sample of adolescents with CSA-related PTSD is a strength of this study. Some limitations should be mentioned. The CSA-related PTSD group in this study was significantly older than the control group and also more advanced in pubertal development. Longitudinal studies of typical adolescent brain development, however, show little change in most of our ROIs (mPFC, ACC, middle/sup temp gyrus) within the age range of participants of both groups68. Furthermore, we controlled for age and pubertal development in our analyses. In the statistical analysis we also controlled for total intracranial volume. Full-scale IQ measures were significantly lower in the CSA-related PTSD group than in the control group. As PTSD has been shown to supress IQ values, groups might originally have been more equal with respect to intellectual ability69. Brain development as well as the reaction to trauma is known to be susceptible to gender influences. We could not address this topic because our participants were mainly girls. Finally, as in our study several of the perpetrators of the CSA adolescents were family members, it was not possible to reliably assess timing and frequency of the traumatic experience retrospectively.
In conclusion, we found no differences in cortical measures between a group of adolescents with CSA-related PTSD and healthy non-traumatised controls. These findings support the suggestion that different types of adversity may have different neurobiological sequelae and subsequent psychiatric and somatic disorders. As childhood trauma is a highly relevant issue for society with severe consequences for psychological and general health, more and preferably longitudinal research into the neurobiological sequelae is needed.
References
Anda, R. F. et al. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. Eur. Arch. Psychiatry Clin. Neurosci 256, 174–186, https://doi.org/10.1007/s00406-005-0624-4 (2006).
Kessler, R. C. et al. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. Br. J. Psychiatry 197, 378–385, https://doi.org/10.1192/bjp.bp.110.080499 (2010).
MacMillan, H. L. et al. Childhood abuse and lifetime psychopathology in a community sample. Am. J. Psychiatry 158, 1878–1883 (2001).
Gilbert, R. et al. Burden and consequences of child maltreatment in high-income countries. Lancet 373, 68–81, https://doi.org/10.1016/S0140-6736(08)61706-7 (2009).
Shonkoff, J. P. Protecting brains, not simply stimulating minds. Science 333, 982–983, https://doi.org/10.1126/science.1206014 (2011).
Provencal, N. & Binder, E. B. The neurobiological effects of stress as contributors to psychiatric disorders: focus on epigenetics. Curr. Opin. Neurobiol 30, 31–37, https://doi.org/10.1016/j.conb.2014.08.007 (2015).
Sanchez, M. M., Ladd, C. O. & Plotsky, P. M. Early adverse experience as a developmental risk factor for later psychopathology: evidence from rodent and primate models. Dev. Psychopathol 13, 419–449 (2001).
Kaufman, J., Plotsky, P. M., Nemeroff, C. B. & Charney, D. S. Effects of early adverse experiences on brain structure and function: clinical implications. Biol. Psychiatry 48, 778–790 (2000).
McCrory, E., De Brito, S. A. & Viding, E. Research review: the neurobiology and genetics of maltreatment and adversity. J. Child Psychol. Psychiatry 51, 1079–1095, https://doi.org/10.1111/j.1469-7610.2010.02271.x (2010).
McLaughlin, K. A. & Lambert, H. K. Child Trauma Exposure and Psychopathology: Mechanisms of Risk and Resilience. Curr. Opin. Psychol 14, 29–34, https://doi.org/10.1016/j.copsyc.2016.10.004 (2017).
Davidson, R. J. & McEwen, B. S. Social influences on neuroplasticity: stress and interventions to promote well-being. Nat. Neurosci 15, 689–695, https://doi.org/10.1038/nn.3093 (2012).
Thomaes, K. et al. Can pharmacological and psychological treatment change brain structure and function in PTSD? A systematic review. J. Psychiatr. Res. 50, 1–15, https://doi.org/10.1016/j.jpsychires.2013.11.002 (2014).
Rinne-Albers, M. A., van der Wee, N. J., Lamers-Winkelman, F. & Vermeiren, R. R. Neuroimaging in children, adolescents and young adults with psychological trauma. Eur. Child Adolesc. Psychiatry 22, 745–755, https://doi.org/10.1007/s00787-013-0410-1 (2013).
Kuhn, S. & Gallinat, J. Gray matter correlates of posttraumatic stress disorder: a quantitative meta-analysis. Biol. Psychiatry 73, 70–74, https://doi.org/10.1016/j.biopsych.2012.06.029 (2013).
O'Doherty, D. C., Chitty, K. M., Saddiqui, S., Bennett, M. R. & Lagopoulos, J. A systematic review and meta-analysis of magnetic resonance imaging measurement of structural volumes in posttraumatic stress disorder. Psychiatry Res. 232, 1–33, https://doi.org/10.1016/j.pscychresns.2015.01.002 (2015).
Bremner, J. D. Neuroimaging in posttraumatic stress disorder and other stress-related disorders. 1. Neuroimaging Clin. N. Am. 17, 523–538, ix (2007).
Woon, F. L. & Hedges, D. W. Hippocampal and amygdala volumes in children and adults with childhood maltreatment-related posttraumatic stress disorder: a meta-analysis. Hippocampus 18, 729–736, https://doi.org/10.1002/hipo.20437 (2008).
McCrory, E., De Brito, S. A. & Viding, E. The impact of childhood maltreatment: a review of neurobiological and genetic factors. Front Psychiatry 2, 48, https://doi.org/10.3389/fpsyt.2011.00048 (2011).
Rinne-Albers, M. A. et al. Abnormalities of white matter integrity in the corpus callosum of adolescents with PTSD after childhood sexual abuse: a DTI study. Eur. Child Adolesc. Psychiatry 25, 869–878, https://doi.org/10.1007/s00787-015-0805-2 (2016).
Aghajani, M. et al. Abnormal functional architecture of amygdala-centered networks in adolescent posttraumatic stress disorder. Hum. Brain Mapp 37, 1120–1135, https://doi.org/10.1002/hbm.23093 (2016).
Riem, M. M. E. et al. General psychopathology factor and unresolved-disorganized attachment uniquely correlated to white matter integrity using diffusion tensor imaging. Behav. Brain Res. 359, 1–8, https://doi.org/10.1016/j.bbr.2018.10.014 (2018).
Rinne-Albers, M. A. et al. Anterior cingulate cortex grey matter volume abnormalities in adolescents with PTSD after childhood sexual abuse. Eur. Neuropsychopharmacol 27, 1163–1171, https://doi.org/10.1016/j.euroneuro.2017.08.432 (2017).
van den Bulk, B. G. et al. Amygdala habituation to emotional faces in adolescents with internalizing disorders, adolescents with childhood sexual abuse related PTSD and healthy adolescents. Dev. Cogn Neurosci 21, 15–25, https://doi.org/10.1016/j.dcn.2016.08.002 (2016).
van Hoof, M. J. et al. Emotional face processing in adolescents with childhood sexual abuse-related posttraumatic stress disorder, internalizing disorders and healthy controls. Psychiatry Res. 264, 52–59, https://doi.org/10.1016/j.pscychresns.2017.04.006 (2017).
van Hoof, M. J. et al. Unresolved-Disorganized Attachment is Associated With Smaller Hippocampus and Increased Functional Connectivity Beyond Psychopathology. J. Trauma Stress 32, 742–752, https://doi.org/10.1002/jts.22432 (2019).
van Hoof, M. J. et al. Unresolved-disorganized attachment adjusted for a general psychopathology factor associated with atypical amygdala resting-state functional connectivity. Eur. J. Psychotraumatol 10, 1583525, https://doi.org/10.1080/20008198.2019.1583525 (2019).
Clarkson, M. J. et al. A comparison of voxel and surface based cortical thickness estimation methods. Neuroimage 57, 856–865, https://doi.org/10.1016/j.neuroimage.2011.05.053 (2011).
Corbo, V. et al. Reduced cortical thickness in veterans exposed to early life trauma. Psychiatry Res. 223, 53–60, https://doi.org/10.1016/j.pscychresns.2014.04.013 (2014).
Geuze, E. et al. Thinner prefrontal cortex in veterans with posttraumatic stress disorder. Neuroimage 41, 675–681, https://doi.org/10.1016/j.neuroimage.2008.03.007 (2008).
Ansell, E. B., Rando, K., Tuit, K., Guarnaccia, J. & Sinha, R. Cumulative adversity and smaller gray matter volume in medial prefrontal, anterior cingulate, and insula regions. Biol. Psychiatry 72, 57–64, https://doi.org/10.1016/j.biopsych.2011.11.022 (2012).
Woodward, S. H., Schaer, M., Kaloupek, D. G., Cediel, L. & Eliez, S. Smaller global and regional cortical volume in combat-related posttraumatic stress disorder. Arch. Gen. Psychiatry 66, 1373–1382, https://doi.org/10.1001/archgenpsychiatry.2009.160 (2009).
Lindemer, E. R., Salat, D. H., Leritz, E. C., McGlinchey, R. E. & Milberg, W. P. Reduced cortical thickness with increased lifetime burden of PTSD in OEF/OIF Veterans and the impact of comorbid TBI. Neuroimage. Clin 2, 601–611, https://doi.org/10.1016/j.nicl.2013.04.009 (2013).
Landre, L. et al. Preserved subcortical volumes and cortical thickness in women with sexual abuse-related PTSD. Psychiatry Res 183, 181–186, https://doi.org/10.1016/j.pscychresns.2010.01.015 (2010).
Dickie, E. W., Brunet, A., Akerib, V. & Armony, J. L. Anterior cingulate cortical thickness is a stable predictor of recovery from post-traumatic stress disorder. Psychol. Med. 43, 645–653, https://doi.org/10.1017/S0033291712001328 (2013).
Kahl, M., Wagner, G., de la Cruz, F., Kohler, S. & Schultz, C. C. Resilience and cortical thickness: a MRI study. Eur. Arch. Psychiatry Clin. Neurosci. https://doi.org/10.1007/s00406-018-0963-6 (2018).
Ahmed, F., Spottiswoode, B. S., Carey, P. D., Stein, D. J. & Seedat, S. Relationship between neurocognition and regional brain volumes in traumatized adolescents with and without posttraumatic stress disorder. Neuropsychobiology 66, 174–184, https://doi.org/10.1159/000339558 (2012).
Klabunde, M., Weems, C. F. & Raman, M. & Carrion, V. G. The moderating effects of sex on insula subdivision structure in youth with posttraumatic stress symptoms. Depress. Anxiety 34, 51–58, https://doi.org/10.1002/da.22577 (2017).
Busso, D. S. et al. Child Abuse, Neural Structure, and Adolescent Psychopathology: A Longitudinal Study. J. Am. Acad. Child Adolesc. Psychiatry 56, 321–328, https://doi.org/10.1016/j.jaac.2017.01.013 (2017).
Gold, A. L. et al. Childhood abuse and reduced cortical thickness in brain regions involved in emotional processing. J. Child Psychol. Psychiatry 57, 1154–1164, https://doi.org/10.1111/jcpp.12630 (2016).
Hodel, A. S. et al. Duration of early adversity and structural brain development in post-institutionalized adolescents. Neuroimage 105, 112–119, https://doi.org/10.1016/j.neuroimage.2014.10.020 (2015).
McLaughlin, K. A. et al. Widespread reductions in cortical thickness following severe early-life deprivation: a neurodevelopmental pathway to attention-deficit/hyperactivity disorder. Biol. Psychiatry 76, 629–638, https://doi.org/10.1016/j.biopsych.2013.08.016 (2014).
Whittle, S. et al. Childhood maltreatment and psychopathology affect brain development during adolescence. J. Am. Acad. Child Adolesc. Psychiatry 52, 940–952, https://doi.org/10.1016/j.jaac.2013.06.007 (2013).
Kelly, P. A. et al. Cortical thickness, surface area, and gyrification abnormalities in children exposed to maltreatment: neural markers of vulnerability? Biol. Psychiatry 74, 845–852, https://doi.org/10.1016/j.biopsych.2013.06.020 (2013).
Kelly, P. A. et al. The sexually dimorphic impact of maltreatment on cortical thickness, surface area and gyrification. J. Neural Transm. (Vienna. 123, 1069–1083, https://doi.org/10.1007/s00702-016-1523-8 (2016).
Lim, L. et al. Grey matter volume and thickness abnormalities in young people with a history of childhood abuse. Psychol. Med. 48, 1034–1046, https://doi.org/10.1017/S0033291717002392 (2018).
van Hoof, M. J., van Lang, N. D., Speekenbrink, S., van IJzendoorn, M. H. & Vermeiren, R. R. Adult Attachment Interview differentiates adolescents with Childhood Sexual Abuse from those with clinical depression and non-clinical controls. Attach. Hum. Dev. 17, 354–375, https://doi.org/10.1080/14616734.2015.1050420 (2015).
Wechsler, D. Wechsler Intelligence Scale for Children. (The Psychological Corporation, 1997).
Wechsler, D. Wechsler Adult Intelligence Scale. (The Psychological Corporation, 1991).
Cukor, J., Wyka, K., Jayasinghe, N. & Difede, J. The nature and course of subthreshold PTSD. J. Anxiety. Disord 24, 918–923, https://doi.org/10.1016/j.janxdis.2010.06.017 (2010).
Silverman, W. K. & Ollendick, T. H. Evidence-based assessment of anxiety and its disorders in children and adolescents. J. Clin. Child Adolesc. Psychol 34, 380–411, https://doi.org/10.1207/s15374424jccp3403_2 (2005).
Silverman, W. K., Saavedra, L. M. & Pina, A. A. Test-retest reliability of anxiety symptoms and diagnoses with the Anxiety Disorders Interview Schedule for DSM-IV: child and parent versions. J. Am. Acad. Child Adolesc. Psychiatry 40, 937–944, https://doi.org/10.1097/00004583-200108000-00016 (2001).
Briere, J. Trauma Symptoms Checklist for Children (TSCC), Professional Manual. (Psychological Assessment Resources, 1996).
Barakat, L. P. et al. Families surviving childhood cancer: a comparison of posttraumatic stress symptoms with families of healthy children. J. Pediatr. Psychol 22, 843–859 (1997).
Gustafsson, P. E., Nilsson, D. & Svedin, C. G. Polytraumatization and psychological symptoms in children and adolescents. Eur. Child Adolesc. Psychiatry 18, 274–283, https://doi.org/10.1007/s00787-008-0728-2 (2009).
Lanktree, C. B. et al. Multi-informant assessment of maltreated children: convergent and discriminant validity of the TSCC and TSCYC. Child Abuse Negl 32, 621–625, https://doi.org/10.1016/j.chiabu.2007.10.003 (2008).
Nilsson, D., Wadsby, M. & Svedin, C. G. The psychometric properties of the Trauma Symptom Checklist For Children (TSCC) in a sample of Swedish children. Child Abuse Negl. 32, 627–636, https://doi.org/10.1016/j.chiabu.2007.09.009 (2008).
Kisiel, C. L. & Lyons, J. S. Dissociation as a mediator of psychopathology among sexually abused children and adolescents. Am. J. Psychiatry 158, 1034–1039, https://doi.org/10.1176/appi.ajp.158.7.1034 (2001).
Petersen, A. C. Adolescent development. Annu. Rev. Psychol. 39, 583–607, https://doi.org/10.1146/annurev.ps.39.020188.003055 (1988).
Bond, L. et al. A comparison of self-reported puberty using the Pubertal Development Scale and the Sexual Maturation Scale in a school-based epidemiologic survey. J. Adolesc 29, 709–720, https://doi.org/10.1016/j.adolescence.2005.10.001 (2006).
Herting, M. M., Maxwell, E. C., Irvine, C. & Nagel, B. J. The impact of sex, puberty, and hormones on white matter microstructure in adolescents. Cereb. Cortex 22, 1979–1992, https://doi.org/10.1093/cercor/bhr246 (2012).
Luciana, M. Adolescent brain development in normality and psychopathology. Dev. Psychopathol 25, 1325–1345, https://doi.org/10.1017/S0954579413000643 (2013).
Heim, C. M., Mayberg, H. S., Mletzko, T., Nemeroff, C. B. & Pruessner, J. C. Decreased cortical representation of genital somatosensory field after childhood sexual abuse. Am. J. Psychiatry 170, 616–623, https://doi.org/10.1176/appi.ajp.2013.12070950 (2013).
Weems, C. F. Severe stress and the development of the amygdala in youth: a theory and its statistical implications. Developmental Review 46, 44–53 (2017).
Herzog, J. I. & Schmahl, C. Adverse Childhood Experiences and the Consequences on Neurobiological, Psychosocial, and Somatic Conditions Across the Lifespan. Front Psychiatry 9, 420, https://doi.org/10.3389/fpsyt.2018.00420 (2018).
Norman, R. E. et al. The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS. Med. 9, e1001349, https://doi.org/10.1371/journal.pmed.1001349 (2012).
Baumeister, D., Akhtar, R., Ciufolini, S., Pariante, C. M. & Mondelli, V. Childhood trauma and adulthood inflammation: a meta-analysis of peripheral C-reactive protein, interleukin-6 and tumour necrosis factor-alpha. Mol. Psychiatry 21, 642–649, https://doi.org/10.1038/mp.2015.67 (2016).
Labonte, B. et al. Genome-wide epigenetic regulation by early-life trauma. Arch. Gen. Psychiatry 69, 722–731, https://doi.org/10.1001/archgenpsychiatry.2011.2287 (2012).
Giedd, J. N. et al. Brain development during childhood and adolescence: a longitudinal MRI study. Nat. Neurosci 2, 861–863, https://doi.org/10.1038/13158 (1999).
Pechtel, P. & Pizzagalli, D. A. Effects of early life stress on cognitive and affective function: an integrated review of human literature. Psychopharmacology (Berl) 214, 55–70, https://doi.org/10.1007/s00213-010-2009-2 (2011).
Acknowledgements
Adolescents and their parents involved in the EPISCA study are gratefully acknowledged, as well as the participating centers: the Department of Child and Adolescent Psychiatry and the Psychotrauma Center of GGZ Rivierduinen, The Kinder en Jeugd Traumacentrum (KJTC) in Haarlem, the LUMC Departments of Psychiatry and Radiology, and the Leiden Institute for Brain and Cognition. The EPISCA project is funded by a grant from the LUMC. M.J. van Hoof was supported by WOP GGZ Rivierduinen, which also made assistance in patient recruitment, data collection and data management by C.I. Gelderblom possible. S.A. Rombouts was also supported through the Netherlands Organization for Scientific Research: NWO Vici project (grant number 016130677). The authors also gratefully acknowledge the financial support given by the participating centers.
Author information
Authors and Affiliations
Contributions
Mirjam A. Rinne-Albers contributed substantively to the design of the EPISCA project and the specific study of this article, to the acquisition of participants, to the analysis and interpretation of the data, to drafting and revising the documents. Charlotte P. Boateng contributed substantively to the design of the specific study of this article, to the analysis (specific statistical analysis) and interpretation of the data, to drafting and revising the documents. Steven J. van der Werff contributed substantively to the design of the specific study of this article, to the analysis and interpretation of the data, to drafting and revising the documents. Francien Lamers-Winkelman contributed substantively to the design of the EPISCA project and the specific study of this article, to the acquisition of participants, to the analysis and interpretation of the data, to drafting and revising the documents. Serge A. Rombouts contributed substantively to the design of the EPISCA project and the specific study of this article, to the analysis and interpretation of the data, to drafting and revising the documents. Robert R. Vermeiren contributed substantively to the design and supervision of the EPISCA project and the specific study of this article, to the analysis and interpretation of the data, to drafting and revising the documents. Nic J. van der Wee contributed substantively to the design and supervision of the EPISCA project and the specific study of this article, to the analysis and interpretation of the data, to drafting and revising the documents.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rinne-Albers, M.A., Boateng, C.P., van der Werff, S.J. et al. Preserved cortical thickness, surface area and volume in adolescents with PTSD after childhood sexual abuse. Sci Rep 10, 3266 (2020). https://doi.org/10.1038/s41598-020-60256-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-60256-3
This article is cited by
-
Examining the association between posttraumatic stress disorder and disruptions in cortical networks identified using data-driven methods
Neuropsychopharmacology (2024)
-
Differential relationships of PTSD symptom clusters with cortical thickness and grey matter volumes among women with PTSD
Scientific Reports (2021)
-
Repeated cocaine exposure prior to fear conditioning induces persistency of PTSD-like symptoms and enhancement of hippocampal and amygdala cell density in male rats
Brain Structure and Function (2021)
-
Examination of the association between exposure to childhood maltreatment and brain structure in young adults: a machine learning analysis
Neuropsychopharmacology (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.