Abstract
Although guidelines recommend BRCA testing for all women with non-mucinous epithelial ovarian cancer, there is significant variability in access to testing across the UK. A germline BRCA mutation (BRCAm) in ovarian cancer patients provides prognostic and predictive information and influences clinical management, such as the use of PARP inhibitors, which have demonstrated a progression-free survival benefit in the BRCAm cohort. Additionally, the finding of a BRCAm has significant implications for patients and their families in terms of cancer risk and prevention. We studied the impact of a newly-formed, oncologist-led ‘mainstreaming’ germline BRCA testing pathway in 255 ovarian cancer patients at Imperial College NHS Trust. Prior to the establishment of ‘mainstreaming’, uptake of germline BRCA testing was 14% with a mean turnaround time of 148.2 calendar days. The ‘mainstreaming’ approach led to a 95% uptake of germline BRCA testing and a mean turnaround time of 20.6 days. Thirty-four (13.33%) BRCAm patients were identified. At the time of data collection nine BRCAm patients had received a PARP inhibitor off-trial, three had entered a PARP inhibitor trial and 5 were receiving platinum-based chemotherapy with a plan to receive PARP inhibitor maintenance. This study provides further evidence of the impact of oncologist-led ‘mainstreaming’ programs.
Similar content being viewed by others
Introduction
In the United Kingdom (UK), over 7,000 cases of ovarian cancer are diagnosed annually, resulting in over 4,000 deaths per year – making ovarian cancer the 6th most common cancer in women1. There is a well-documented association between women carrying pathogenic germline mutations in breast cancer gene one (BRCA1) or breast cancer gene two (BRCA2) and their risk of developing ovarian cancer2,3. Identifying ovarian cancer patients carrying germline breast cancer gene (BRCA) mutations provides important insight into why the patient may have developed ovarian cancer, is indicative of the patient’s prognosis and can help determine the optimal therapeutic interventions and best approach to clinical management of their disease4,5.
Characteristics of BRCA-mutated (BRCAm) ovarian cancer and impact of BRCA status on clinical decision making
Previous studies indicate that the prevalence of germline BRCA mutation carriers in a non-mucinous ovarian cancer cohort is around 13–15%5,6,7,8,9. The mean age of diagnosis of ovarian cancer in patients carrying a BRCA1 mutation can be five to ten years lower than the mean age of diagnosis of BRCA wild-type (BRCAwt) patients (patients carrying BRCA2 mutations do not show such a marked difference in age of diagnosis from the BRCAwt population)7,9,10. Literature also suggests that BRCAm ovarian cancer is more likely to be diagnosed at an advanced stage of disease6, where survival outcomes are poorer.
There are significant differences in the response to treatment and survival outcomes between BRCAm and BRCAwt ovarian cancer populations, even when the same therapeutic intervention is applied irrespective of BRCA status6,11, resulting in greater median progression-free survival and median overall survival times in the BRCAm patient cohort6,12. Additionally, a patient’s BRCA status can inform decision making around risk-reducing procedures for both the individual and any subsequently-identified BRCA mutation carriers within the family5,11,12,13. Identifying further BRCAm carrier family members via cascade testing has also been demonstrated to be a cost-effective mechanism to prevent future cancers in relatives5,14.
Although the presence of a BRCA mutation is considered a predictive biomarker for response to treatment13, prior to the introduction of poly ADP-ribose polymerase (PARP) inhibitors into clinical practice the knowledge of a patient’s BRCA status had little impact on the management of their ovarian cancer. In December 2014 PARP inhibitor olaparib received European Medicines Agency (EMA) Marketing Authorisation for the treatment of relapsed, platinum-sensitive BRCAm ovarian cancer15 and was made available by the National Health Service (NHS) in early 201616. The availability of this targeted therapy for BRCA-mutated patients created a shift towards a more personalised approach to the management of ovarian cancer and further highlighted the need for BRCA testing5,6,13,17,18. Following the approval of olaparib, clinical utility has also been demonstrated in both BRCAm and BRCAwt cohorts with other licenced PARP inhibitors, niraparib and rucaparib19,20.
The announcement of the SOLO1 trial results21 in October 2018 has impacted further on the approach to treating BRCAm ovarian cancer. Results of this study show that patients receiving olaparib maintenance in the first line setting benefit from an estimated three year median progression free survival advantage versus those BRCAm patients who received placebo21. The recent licence extension for olaparib to allow maintenance treatment in the first line setting further highlights how knowledge of a patients BRCA status at the outset of their disease management has become increasingly important.
Access to BRCA testing in the United Kingdom
There is an overwhelming body of literature advocating that germline BRCA testing should be offered to all women with a diagnosis of non-mucinous ovarian cancer, irrespective of age at diagnosis or family history of BRCA-associated cancer5,6,7,9,17,22. The NICE Clinical Guideline on Familial Breast Cancer (CG164) recommends that BRCA testing be offered to any woman with ovarian cancer where the probability of carrying a BRCA mutation is 10% or greater23 – considering that the prevalence of BRCA mutation carriers in non-mucinous ovarian cancer cohorts is around 13–15%5,6,7,8,9, this would indicate that all patients with a diagnosis of non-mucinous ovarian cancer should be offered BRCA testing. This is further supported by the recommendation of the Independent Cancer Taskforce, who suggest that BRCA testing should be offered at the point of diagnosis to the aforementioned patient group24. Despite a clear clinical and scientific rationale, the implementation of these guidelines is at the discretion of each regional genetics centre – which has resulted in significant variability of access to BRCA testing across the UK13. Furthermore, there are currently no guidelines recommending somatic BRCA testing for women with ovarian cancer and currently there is no NHS funding for this in the UK.
Although relatively new, there is a growing body of evidence supporting the feasibility of an oncologist-led ‘mainstreaming’ approach5,8,17,18 – where the oncology team introduce the concept of genetic testing and obtain patient consent as part of routine appointments, deliver initial results and then refer any identified BRCAm patients or those with a Variant of Unknown Significance (VUS) on to specialised genetic departments for counselling and cascade testing of potentially affected family members.
Purpose of this study
With the increased clinical utility of BRCA testing and broader availability of PARP inhibitors for BRCAm patients, the landscape of ovarian cancer treatment is changing. This study aims to assess the impact of the introduction of an oncologist-led BRCA testing mainstreaming service at Imperial College Healthcare NHS Trust on 255 ovarian cancer patients, previously untested for germline BRCA mutations and to examine the epidemiology of the BRCAm and BRCAwt cohorts within this population, evaluate the impact of the knowledge of the patients’ BRCA status on clinical decision-making, and provide further evidence of the utility and success of this pathway.
In light of conflicting opinions on the implementation of an age-based threshold for access to BRCA testing, an additional aim of this study is to investigate the prevalence of BRCAm in older patients (diagnosis ≥ 70 years), and any subsequent impact a BRCA mutation status has on their clinical management.
Methods
Patient selection, consent to BRCA testing and ongoing clinical management
All patients with a confirmed diagnosis of non-mucinous ovarian cancer and an unknown BRCA status who were under the care of the gynaecological oncology team at Imperial College Healthcare NHS Trust, on or after the 1st April 2016, were eligible for germline BRCA testing through the Imperial College Hospital Mainstreaming Programme (ICHMP). During the time of this study we identified 312 patients at ICHNT with non-mucinous ovarian cancer. Of this cohort, 14% had already undergone BRCA testing via alterative mechanisms. Of the 268 untested patients who remained eligible for testing, there was a 95% uptake of BRCA testing via the mainstreaming route. The remaining 5% either declined BRCA testing or were deceased prior to BRCA testing taking place.
The ICHMP could be introduced, and the patient subsequently consented for germline BRCA testing, by any member of the gynaecological oncology team who had completed the Mainstreaming Cancer Genetics online training program (available at http://www.mcgprogramme.com/BRCAtoolkit/). This could occur at any scheduled appointment during the patient’s treatment or routine surveillance. The consenting process involved discussion of what the BRCA gene is, what a mutation and VUS is and what the relevance of the finding of a mutation might be to the patient (in terms of treatment of their ovarian cancer and future screening and prevention for other BRCA-associated disease) as well as the relevance of the finding to other blood relatives. Patients were given time to decide on whether they wished to proceed with BRCA testing. Patients were also provided with written information developed by the oncology and genetics teams at Hammersmith Hospital and the Royal Marsden Hospital.
The first 32 patients tested via the ICHMP were consented following a group consenting process. They had responded to a written invitation from the oncology team to attend a lecture on BRCA testing and were subsequently offered a consultation and blood test that day if they agreed to it. This method was used to study whether such an approach could reduce the number of untested patients in the prevalent pool of patients within the ovarian cancer clinic.
Patients who received a BRCAm or VUS result were referred on to The Royal Marsden genetics department for genetic counselling and follow up. Patients with a negative result but a significant family history of cancer were also offered an appointment with a genetic counsellor if they wished. Clinical management of the patient’s disease continued under the gynaecological oncology team at Imperial College Healthcare NHS Trust.
All patients who underwent testing via the ICHMP between April 2016 and April 2018 (inclusive) were included in this analysis.
BRCA testing methodology and recording of results
All germline BRCA testing was undertaken by TGLclinical (Institute of Cancer Research, 15 Cotswold Road, Sutton SM2 5NG). Samples were tested using the Illumina TruSight Cancer Panel. Although panel gene testing was undertaken, no pathogenic mutations or rare variants other than in BRCA1 and BRCA2 were released or reported, as was explained to patients prior to consenting to BRCA testing. Further information on the methodologies, analysis and reporting procedures can be found at www.TGLclinical.com.
Collection of patient data
All patient data was obtained via a review of patient clinical records in the Imperial College Healthcare NHS Trust record management systems. Patient data has been collected as it was recorded by the treating clinicians.
Results
Clinical characteristics of the patient cohort
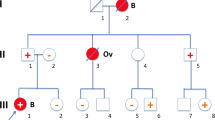
Patients who underwent testing via the ICHMP ranged from those who were newly-diagnosed to those who had undergone several relapses and multiple lines of prior therapy. Of the 255 patients tested, 34 (13.33%) patients were found to be carrying a germline BRCA mutation - 19 BRCA1 mutation carriers and 15 BRCA2 mutation carriers were identified (Table 1). No patients with a VUS were identified.
The mean age of diagnosis was 57.8 years for the BRCAm cohort and 62.9 years for the BRCAwt cohort (Table 2). The mean age of diagnosis for BRCA1 carriers was 54.2 years, whilst the mean age of diagnosis for BRCA2 carriers was 62.3 years. Fifteen (44.1%) BRCAm patients were aged ≥60 years at the time of diagnosis, with five (14.7%) BRCAm patients aged ≥70 years at the time of diagnosis. The mean time between diagnosis and obtaining a BRCA test result was 28.36 months (range 0–312 months).This was as due to the fact that although many patients in this study underwent BRCA mainstreaming at diagnosis, some patients within the study underwent BRCA testing at relapse having not had BRCA testing prior to the implementation of the ICHMP.
Clinical characteristics of the BRCAm cohort
Of the 34 identified BRCAm patients, five (14.7%) had prior breast cancer, one (2.9%) had prior oesophageal cancer, 26 (76.5%) had no prior cancer, and two (5.9%) patients had an unknown/undocumented personal cancer history. When considering these patients’ family history of BRCA-associated cancer (breast, gynaecological, pancreas or prostate), 15 (44.1%) reported a family history of BRCA-associated cancer, 13 (38.2%) reported no family history and six (17.6%) had an unknown/undocumented family history. Three patients (8.8%) had both a personal and family history of BRCA-associated cancer.
Twenty-nine different BRCA mutations were identified amongst the 34 patients, with three mutations identified in more than one patient. Six founder mutations of Ashkenazi Jewish origin were identified within the cohort.
Impact of BRCAm status on patient management
At the time of data collection nine of the 34 identified BRCAm patients had received a PARP inhibitor as a direct consequence of the identification of a BRCA mutation. Six of these nine patients received olaparib post third-line therapy through NHS reimbursement, two received niraparib and one received rucaparib after second-line therapy via Early Access Programs. A further five BRCAm patients were receiving platinum-based chemotherapy for relapsed disease, where the intent of the clinical team was to initiate treatment with a PARP inhibitor following the completion of chemotherapy, assuming that a response to therapy was achieved. Fifteen BRCAm patients were either still receiving first-line (adjuvant) treatment or were in remission, and therefore not eligible to receive a PARP inhibitor at that time. Three of these patients receiving first-line therapy were subsequently recruited to the PRIMA trial (NCT02655016), a study of niraparib maintenance treatment in patients with advanced ovarian cancer following response on first-line platinum-based chemotherapy. The finding of a BRCA mutation influenced their decision to take part in this trial given the potential access to a PARP inhibitor maintenance therapy in the first-line setting. Five BRCAm patients were ineligible to receive PARP inhibitors either due to poor performance status (n = 2), platinum resistant disease at a time when there was no access to PARP inhibitors in this setting (n = 2) or death prior to further therapy (n = 1). Summary information on the characteristics of the BRCAm patients who received a PARP inhibitor can be seen in Table 3.
Of the 221 BRCAwt patients who underwent germline BRCA testing via the ICHMP, five received niraparib. This was via the Early Access Program which provided niraparib as a maintenance therapy for patients with platinum-sensitive relapsed ovarian cancer who were in response to further platinum therapy.
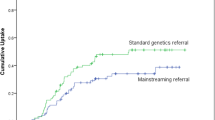
Uptake and utility of mainstreaming pathway
There was a 95% uptake of BRCA testing via the ICHMP. The remaining 5% of patients either declined BRCA testing or were deceased prior to BRCA testing taking place. This compared to a figure of 14% of patients who underwent BRCA testing prior to the implementation of the ICHMP, when patients required referral to the regional genetics centres for counselling and consideration of BRCA testing.
Turnaround time was assessed in the 199 samples where both the date of sample acquisition and the date of test result was recorded. The mean turnaround time between blood sample acquisition and return of BRCA result to the treating oncologist was 20.6 calendar days, with a range of 11–42 calendar days. This compares favourably to the mean turnaround time of 148.2 calendar days prior to the implementation of the ICHMP.
Discussion
Epidemiology of Imperial College Healthcare NHS Trust cohort, and comparisons to other published literature
When considering the epidemiology of this cohort, these results are generally in line with other cohorts of ovarian cancer patients who have undergone systematic BRCA testing at other centres in the UK or abroad5,6,7,8,11. The age of diagnosis is lower in the BRCAm population than BRCAwt population, which reflects one of the hallmarks of BRCA-associated disease6,7,9. All BRCAm patients in this cohort had high grade serous histology. Although it is unusual that no other histologies were detected in the BRCAm population in this cohort, it is to be expected that the majority would have high grade serous histology given that this was the most common histology observed in other non-mucinous ovarian cancer cohorts5,11. The absence of any other histological subtypes is likely attributable to the relatively small sample size of this population. We would still advocate BRCA testing in all non-mucinous subtypes given the observation of BRCA mutations in non-mucinous, non-high grade serous groups in other studies5,11. These results are also consistent with previous findings that BRCAm ovarian cancer is more likely to be diagnosed at an advanced stage of disease6. Comparisons to other similarly-sized UK cohorts can be seen in Tables 4 and 5.
This study reports that approximately half of the BRCAm carriers do not have any relevant family history of BRCA-associated cancer (or at least, are not aware or cannot recall any family history in order to communicate this to their care team), which is similar to other cohorts in the UK (Table 5) and abroad6,17. This result further strengthens the argument that family history alone should not be used to predict BRCA status, or be applied as a criterion to determine eligibility for BRCA testing. There is significant variability in the proportion of women with a personal breast cancer history across the different BRCAm cohorts in the UK (Table 5), also indicating that personal cancer history alone is also not a reliable predictor of BRCA status.
Impact of BRCAm testing on patient management and access to PARP inhibitors
All 34 patients with identified BRCA mutations were offered genetic counselling, which was attended by 31 patients. Where appropriate, patients were offered enhanced breast surveillance, ‘To whom it may concern’ information to be passed on to other potentially-affected family members, and entry onto The Royal Marsden’s carrier register.
In line with other literature sources5,8,18, this study highlights that knowledge of a patient’s BRCAm status had an impact on the management of their ovarian cancer and their ability to access PARP inhibitor treatment. At the time of this study, NHS-funded PARP inhibitor treatment was only accessible to BRCAm patients, and no BRCAwt patient at Imperial College Healthcare NHS Trust was eligible for PARP inhibitor treatment outside of a clinical trial or Expanded Access Program. It is likely that discrepancies in the proportion of patients able to access PARP inhibitors across the various studies is due to the restrictions on access to NHS-reimbursed PARP inhibitor treatment at various points in time, and variability in relevant PARP inhibitor clinical trial availability at the time of the different studies. It is hypothesised that where clinical trials were open and/or Early Access Programs/Compassionate Use Programs initiated by the sponsoring company were available, a greater percentage of BRCAm patients may have been able to access PARP inhibitor treatment allowing for improved patient outcomes across the cohort. When considering the 15 (44.2%) BRCAm patients who have not yet relapsed, the knowledge of their BRCA status may well inform future treatment planning if they do present with disease recurrence.
Although consideration must be given to the low numbers of patients who accessed PARP inhibitors following a BRCAm result obtained through ICHMP, it must also be noted that all seven of the patients who had completed their treatment with a PARP inhibitor had a shorter treatment duration than the median time on treatment reported in the respective PARP inhibitor clinical trials19,25 (two patients were still undergoing PARP inhibitor treatment at the time of data collection, following recent initiations). One explanation could be the fact that these are ‘real world data’ and patients were not subjected to a controlled clinical trial protocol with extensive follow up. It is also hypothesised that the fact that only three patients (33.3%) received PARP inhibitors after two lines of platinum therapy, whereas six (66.6%) of patients had received three or more prior lines of chemotherapy before receiving a PARP inhibitor contributed to their shorter treatment duration. The proportion of patients treated with PARP inhibitor therapy following fewer lines of therapy was higher in clinical trials such as SOLO2 (56% receiving olaparib after two lines of therapy and 31% receiving PARP inhibitor after three lines)26 and ARIEL3 (63% received rucaparib after only two lines of platinum-based chemotherapy)20. This is important given that earlier use of PARP inhibitors is considered to be associated with better outcomes. Furthermore, it is unknown whether patients in this cohort had a higher ECOG performance status than those treated in the PARP inhibitor trials (where the majority of patients had an ECOG performance status of 0), and this may have impacted the duration of their treatment. Only one patient discontinued PARP inhibitor treatment due to unacceptable toxicities, which is in keeping with clinical trials results and speaks to the general tolerability of PARP inhibitors19,25.
Patients aged ≥70 years: access to BRCA testing and clinical utility of BRCAm result
Previous publications argue that age should not be a discriminating factor preventing access to BRCAm testing14,22, although it is noted that this does seem to occur in clinical practice14. Zhang et al.7 and Alsop et al.6 report a BRCAm prevalence of 8.4% and 8.3% in patients who were aged ≥60 at the time of diagnosis, respectively. Plaskocinska et al.11 also recommend that in order to meet the 10% threshold required by NICE, women aged ≥70 should only be tested if they have personal or family history of a BRCA-associated cancer. However, the results of this study provide evidence against the imposition of an age-based threshold for BRCAm testing. These results show a BRCAm prevalence of 11.7% patients aged ≥60 at the time of diagnosis, and a BRCAm prevalence of 11.6% in patients who were diagnosed with ovarian cancer aged 70–79 - indicating that patients aged ≥70 still meet the 10% threshold required under NICE Guidelines23. Two BRCAm patients who were aged ≥70 at the time of diagnosis subsequently received a PARP inhibitor – with a further two BRCAm patients aged ≥70 at the time of diagnosis in remission, but will possibly receive PARP inhibitors at a subsequent relapse. The access to PARP inhibitors by patients aged ≥70 highlights the continued utility of BRCAm testing in an older population.
Evaluation of mainstreaming approach
The ICHMP has successfully tested 255 patients over a period of two years, with 34 BRCAm patients identified, providing further proof-of-concept of the oncologist-led mainstreaming model in an NHS centre. In the two years prior to the establishment of the ICHMP only 14% of patients underwent germline BRCA testing (these patients were tested via a direct referral to the regional genetics centres, where the mean turnaround time from referral to result was 148.2 calendar days (range 98–175)). However, following the implementation of the ICHMP, 95% of patients had obtained a germline BRCA result and this was impactful on patient management. The result of a mean turnaround time (from sample acquisition to receipt of result by treating oncologist) of 20.6 calendar days (range 11–42) highlights one of the key benefits of the IHCMP. The IHCMP allowed a reduction in mean turnaround time from 148.2 days to 20.6 days. This is particularly significant given the outcomes of the SOLO1 trial21, and the recent licence extension to allow maintenance treatment with olaparib in the first-line setting. The IHCMP allows the majority of patients to undergo germline BRCA testing at their first consultation with their oncologist, and the mean turnaround time of 20.6 days is a sufficient to enable the treating oncologist adequate time to make choices around the most appropriate therapy in this setting. This includes making informed decisions regarding treatment with olaparib where indicated, and alternatively, bevacizumab, in cases where treatment with olaparib is not appropriate. The study also demonstrated the feasibility of a group consenting process for BRCA testing that can be used within a ‘mainstreaming’ program and that could be reproduced in other centres with a large pool of untested patients that may be eligible for testing or that may require testing in a timely manner.
Limitations of this study
As this study was based on patient record data, in some cases not all data points were recorded accurately or available to be included in analysis. In addition, it was evident that not every patient under the care of the gynaecological oncology team had been offered BRCAm testing through the ICHMP – it should be considered that some patients may have declined testing, or not been offered testing due to clinician bias or error. Although prior to the ICHMP BRCA testing was not routine clinical practice at this centre, low numbers of patients under the care of this team had received BRCA testing before the implementation of the ICHMP. Some caution should be applied when interpreting this data as it cannot be said with certainty that this is representative of the entire ovarian cancer cohort at this centre within the stated timeframe. Grant funding for somatic BRCA testing was not available during this study and NHS funding for such testing is still not available within our oncology clinics in the UK. This study aimed to assess the role of germline BRCA testing via a ‘mainstreaming’ process but we acknowledge that somatic BRCA testing would have further impact on a small group within this patient cohort in terms of identifying those patients with a somatic BRCA mutation who may also have derived benefit from a PARP inhibitor.
Conclusions & future directions
This study has examined the epidemiology of the BRCAm and BRCAwt cohorts within the Imperial College Healthcare NHS Trust and concluded that it is highly similar to other cohorts examined across the UK5,8,11. It is evident that there is significant impact of the knowledge of the patients’ BRCA status on clinical decision-making, as demonstrated by patient access to PARP inhibitors (through NHS-funded olaparib, restricted to BRCAm patients - or through Expanded Access Programs for BRCAm patients) or patient eligibility to enter clinical trials. Additionally, the knowledge of a patient’s BRCAm status has triggered referral to genetic counselling, providing additional management of the BRCAm patient as well as an introduction to cascade testing for related family members. The fact that these outcomes were achieved for this cohort provides evidence of the utility and success of an oncologist-led BRCA testing mainstreaming service, as implemented at Imperial College Healthcare NHS Trust.
Following the introduction of PARP inhibitors to the clinic, a patient’s BRCA status is of greater significance than ever before. Previous publications cite that the time between diagnosis and obtaining a BRCAm result has not had an impact on the selection of therapy, as patients tested were generally undergoing primary treatment or in remission17 – but with the recent approval of olaparib in the first line treatment setting for BRCAm patients and the significant progression-free survival benefits and trends towards a greater overall survival that can be derived from this21, clinicians will need to ensure that BRCA testing occurs at the very outset of disease management and treatment planning. Results must also be returned in a timely manner so that BRCAm patients do not miss the opportunity to benefit from first-line olaparib. The growing body of evidence demonstrating the utility of oncologist-led mainstreaming should be given due consideration by those centres who have not yet achieved routine testing of all non-mucinous ovarian cancer patients, or who are unable to ensure BRCA testing is carried out within the recommended timeframes. Furthermore, group education sessions and consenting could be adopted to allow quicker and more efficient testing of untested patients within the ovarian cancer clinics.
As previously mentioned, this study does not look at the testing pathways for somatic (tumour) BRCA mutations. In order to optimise clinical management for all ovarian cancer patients, it is key that the testing pathways and processes for germline BRCA and somatic BRCA mutations are integrated5, and both deliver timely results. It is only through up-front, routine testing of all non-mucinous ovarian cancer patients will we be able to ensure that all eligible BRCAm patients get the opportunity to benefit from PARP inhibitor therapy.
Finally, future work will assess the impact of the ICHMP on measures taken to reduce risk or prevent other BRCA-associated cancers in the BRCAm patient cohort, and in the uptake of BRCA testing and the consequences thereof in their blood relatives. This is likely to add a further dimension of supportive evidence for the ICHMP and other similar mainstreaming processes.
Ethics approval and consent to participate
This is a review of a new clinical service within an institution and specific ethical approval was not therefore not sought or required. Patients whose data are described in the study did give informed consent. Patients all signed consent forms that stipulated that they agreed to undertake genetic testing and that the samples, demographics, results and information could be used anonymously for research purposes.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Ovarian cancer statistics. Cancer Research UK https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/ovarian-cancer#heading-Zero (2018).
Antoniou, A. et al. Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case Series unselected for family history: a combined analysis of 22 studies. Am. J. Hum. Genet. 72, 1117–1130 (2003).
Lewis, K. E., Lu, K. H., Klimczak, A. M. & Mok, S. C. Recommendations and Choices for BRCA Mutation Carriers at Risk for Ovarian Cancer: A Complicated Decision. Cancers. 10, 57 (2018).
Candido-dos-Reis, F. et al. Germline Mutation in BRCA1 or BRCA2 and Ten-Year Survival for Women Diagnosed with Epithelial Ovarian Cancer. Clin. Cancer Res. 21(3), 652–657 (2015).
George, A. et al. Implementing rapid, robust, cost-effective, patient-centred, routine genetic testing in ovarian cancer patients. Sci. Rep. 6, 29506 (2016).
Alsop, K. et al. BRCA mutation frequency and patterns of treatment response in BRCA mutation-positive women with ovarian cancer: A report from the Australian ovarian cancer study group. J. Clin. Oncol. 30(21), 2654–2663 (2012).
Zhang, S. et al. Frequencies of BRCA1 and BRCA2 mutations among 1,342 unselected patients with invasive ovarian cancer. Gynecol. Oncol. 121(2), 353–357 (2011).
Rahman, B. et al. Mainstreamed genetic testing for women with ovarian cancer: First-year experience. J. Med. Genet. 56, 195–198 (2019).
Pal, T. et al. BRCA1 and BRCA2 mutations account for a large proportion of ovarian carcinoma cases. Cancer. 104(12), 2807–2816 (2005).
Kentwell, M. et al. Mainstreaming cancer genetics: A model integrating germline BRCA testing into routine ovarian cancer clinics. Gynecol. Oncol. 145(1), 130–136 (2017).
Plaskocinska, I. et al. New paradigms for BRCA1/BRCA2 testing in women with ovarian cancer: results of the Genetic Testing in Epithelial Ovarian Cancer (GTEOC) study. J. Med. Genet. 53(10), 655–661 (2016).
Fox, E. et al. The sooner the better: Genetic testing following ovarian cancer diagnosis. Gynecol. Oncol. 137(3), 423–429 (2015).
George, A., Kaye, S. & Banerjee, S. Delivering widespread BRCA testing and PARP inhibition to patients with ovarian cancer. Nat. Rev. Clin. Oncol. 14(5), 284–296 (2017).
Demsky, R. et al. Keeping it simple: Genetics referrals for all invasive serous ovarian cancers. Gynecol. Oncol. 130(2), 329–333 (2013).
Lynparza (olaparib). European Medicines Agency https://www.ema.europa.eu/en/medicines/human/EPAR/lynparza (2018).
NICE Technology appraisal guidance [TA381]. Olaparib for maintenance treatment of relapsed, platinum-sensitive, BRCA mutation-positive ovarian, fallopian tube and peritoneal cancer after response to second-line or subsequent platinum-based chemotherapy. National Institute for Health and Care Excellence (NICE) https://www.nice.org.uk/guidance/ta381/chapter/1-Recommendations (2018).
Colombo, N. et al. Evaluation of a Streamlined Oncologist-Led BRCA Mutation Testing and Counseling Model for Patients With Ovarian Cancer. J. Clin. Oncol. 36(13), 1300–1307 (2018).
Percival, N. et al. The integration of BRCA testing into oncology clinics. Br. J. Nurs. 25(12), 690–694 (2016).
Mirza, M. et al. Niraparib Maintenance Therapy in Platinum-Sensitive, Recurrent Ovarian Cancer. N. Engl. J. Med. 375(22), 2154–2164 (2016).
Coleman, R. et al. Rucaparib maintenance treatment for recurrent ovarian carcinoma after response to platinum therapy (ARIEL3): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 390(10106), 1949–1961 (2017).
Moore, K. et al. Maintenance Olaparib in Patients with Newly Diagnosed Advanced Ovarian Cancer. N. Engl. J. Med. 379, 2495–2505 (2018).
Vergote, I. et al. Current perspectives on recommendations for BRCA genetic testing in ovarian cancer patients. Eur. J. Cancer 69, 127–134 (2016).
NICE Clinical guideline [CG164]. Familial breast cancer: classification, care and managing breast cancer and related risks in people with a family history of breast cancer. National Institute for Health and Care Excellence (NICE) https://www.nice.org.uk/guidance/cg164 (2018).
Achieving world class cancer outcomes: A strategy for England 2015–2020. Independent Cancer Taskforce https://www.cancerresearchuk.org/sites/default/files/achieving_world-class_cancer_outcomes_-_a_strategy_for_england_2015-2020.pdf (2018).
Ledermann, J. et al. Olaparib maintenance therapy in patients with platinum-sensitive relapsed serous ovarian cancer: A preplanned retrospective analysis of outcomes by BRCA status in a randomised phase 2 trial. Lancet Oncol. 15(8), 852–861 (2014).
Pujade-Lauraine, E. et al. Olaparib tablets as maintenance therapy in patients with platinum-sensitive, relapsed ovarian cancer and a BRCA1/2 mutation (SOLO2/ENGOT-Ov21): a double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Oncol. 18(9), 1274–1284 (2017).
Acknowledgements
Funding for the BRCA testing of patient blood samples was provided by The Royal Marsden and The Institute of Cancer Research and Imperial College Biomedical Research Centres grant A165.
Author information
Authors and Affiliations
Contributions
J.K., H.G., A.G., N.R. planned the study and were involved in its conduct, reporting and manuscript development. M.R. and M.L. were involved in data collection, data interpretation, reporting and manuscript development. I.M. and L.T. were involved in patient recruitment, conduct of the study and data collection.
Corresponding author
Ethics declarations
Competing interests
Summary of competing financial and non-financial interests: M.R. was employed by AstraZeneca throughout the duration of this project. H.G. has received honoraria from AstraZeneca, was employed at Imperial College at the time that this work was undertaken but now works for AstraZeneca whilst also still holding a position of employment at Imperial College. A.G. has received honoraria paid to departmental research account from AstraZeneca, Roche and Tesaro. I.M. has received honoraria from Clovis Oncology, Tesaro, AstraZeneca and Takeda, and has also received grants from AstraZeneca, outside the submitted work. J.K. has received honoraria from Clovis Oncology, Tesaro and AstraZeneca, outside the submitted work. N.R. is a non-executive director of AstraZeneca. L.T. has received Tesaro and AstraZeneca, outside the submitted work. M.L. has no disclosures. None of the aforementioned companies had any input into the study design, data collection, reporting or preparation of the manuscript.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rumford, M., Lythgoe, M., McNeish, I. et al. Oncologist-led BRCA ‘mainstreaming’ in the ovarian cancer clinic: A study of 255 patients and its impact on their management. Sci Rep 10, 3390 (2020). https://doi.org/10.1038/s41598-020-60149-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-60149-5
This article is cited by
-
A pilot study investigating feasibility of mainstreaming germline BRCA1 and BRCA2 testing in high-risk patients with breast and/or ovarian cancer in three tertiary Cancer Centres in Ireland
Familial Cancer (2023)
-
Mainstream germline genetic testing in men with metastatic prostate cancer: design and protocol for a multicenter observational study
BMC Cancer (2022)
-
Mainstream genetic testing for women with ovarian cancer provides a solid basis for patients to make a well-informed decision about genetic testing
Hereditary Cancer in Clinical Practice (2022)
-
Positive experiences of healthcare professionals with a mainstreaming approach of germline genetic testing for women with ovarian cancer
Familial Cancer (2022)
-
Mechanism of tumor synthetic lethal-related targets
Oncology and Translational Medicine (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.