Abstract
Headache is a common reason to visit the emergency department (ED). Tension-type headache (TTH) is the commonest headache. The diagnosis of TTH implies a mild condition, with no need for special tests. We evaluated the use of the International Classification of Headache Disorders (ICHD) criteria for TTH in the ED. We performed a cross-sectional study including all ED patients with a definite TTH diagnosis in their discharge report for 2.5 years. We evaluated whether the ICHD criteria for TTH were referenced and met. We analysed discrepancies concerning anamnesis or prior history and reclassified patients. A total of 211 out of 2132 patients fulfilled the criteria (9.9%). Only five patients fulfilled TTH criteria. Criteria A-D were referenced in 60–84% of patients and met in 16–74% of these patients. Anamnesis was discrepant in 87.5% as was prior history in 20.8%. After re-reclassification, 21 patients fulfilled the criteria for TTH (five) or probable TTH (16). In 106 patients, another headache was diagnosed, with migraine in 40 (18.9%), secondary headache in 64 (30.3%), and a life-threatening disorder in 13 (6.1%). In our sample, TTH was overdiagnosed. Only a minority of patients fulfilled the ICHD criteria. Inconsistencies in prior medical history or anamnesis were frequent.
Similar content being viewed by others
Introduction
Tension-type headache (TTH) is the most common primary headache disorder1,2. The prevalence of TTH is estimated to be between 30 and 70% of the general population according to different studies2. The diagnostic criteria proposed by the International Classification of Headache Disorders (ICHD) have remained unaltered since the first edition in 19883,4,5,6. The criteria are based on bilateral, oppressive and mild pain, without typical migraine features and with no better explanation6. Given the mild nature of the disorder, few patients seek assistance, and in headache unit-based series, it is not a frequent diagnosis, accounting for 16% of all diagnoses7. On the other hand, it is not uncommon for migraine patients to be erroneously diagnosed with TTH8.
Headache is one of the main reasons for consultation in the emergency department (ED). It seems remarkable that in some ED-based series, TTH diagnosis accounts for up to 25–33% of all headache visits;9,10 particularly when other series are performed by neurologists or using ICHD criteria diagnosis, TTH represents only 1–6% of total headache patients11,12,13,14,15. In the ED setting, secondary headache detection represents the main priority. TTH is particularly threatening, as its typical phenotype is relatively unspecific, and many secondary headaches may mimic it.
The use and knowledge of the ICHD criteria in the ED setting may be difficult. Most clinicians use red flag lists to rule out secondary headaches16. However, we hypothesize that TTH is probably overdiagnosed in the ED setting, which might represent a risk for patients with nondetected secondary headaches. Establishing TTH diagnosis might be dangerous, as it implies that the patient has a harmless disorder.
In this study, the first objective was to analyse the percentage of patients who fulfilled the ICHD6 criteria for tension-type headache and the percentage of patients presenting each of the different criteria. The second objective was to analyse the presence of data in the discharge reports that contradicted TTH diagnosis, such as relevant prior medical data, atypical symptoms or abnormal findings in the examination. The third objective was to analyse whether patients could be re-classified as having other headache disorders by using the ICHD-3 criteria.
Patients and Methods
This is an observational study with a cross-sectional design. Our study population included patients who visited the emergency department due to headache. The study was performed according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines17.
The study took place at the ED of the Clínico San Carlos University Hospital, Madrid (Spain), a third-level hospital with a reference population of 700.000 people. The study period was between January 2012 and July 2014.
Eligibility
The inclusion criteria were as follows: 1) patients visiting the ED because of headache and 2) patients with a definite diagnosis of “tension-type headache” in the ED discharge report. We excluded patients with 1) some degree of uncertainty in the diagnosis, such as “possible” or “probable”; 2) another headache diagnosed at the same time; and 3) no available information in the patient chart.
We screened all the patients who visited the ED during the study period because of headache by using the ED database, which codifies patients by initial reason for consultation. We reviewed the digitalized reports and gathered the information from the discharge reports. We did not review any additional sources, and we did not evaluate any patients. The rationale for this was that we aimed to see if with the information present in the ED reports, TTH diagnosis was appropriate or not.
The included demographic variables were sex; age; and relevant prior medical history, including current or past cancer, pathology of the immune system, and prior headache history. Clinical variables included headache description, with special attention to the presence of any red flag, neurological examination and abnormal focal signs, vital signs and general examination.
Study objectives
For the first objective, we reviewed the ICHD criteria for TTH4,5,6 (Table 1). We analysed whether each criterion was referenced in the report and if it was fulfilled or not. Criterion A, alluding to the number of episodes, was considered to be met for an infrequent tension-type headache diagnosis if the patient had a minimum of 10 episodes. We did not differentiate the ICHD edition in the manuscript, given that there were no differences between the TTH ICHD criteria in the second, third beta and third editions of the classification4,5,6 (Supplementary material).
For the second objective, we analysed discrepancies concerning both anamnesis and prior medical history. Anamnesis discrepancies were classified into five groups:
- 1.
Presence of symptoms highly suggestive of another headache disorder, including pulsating quality, presence of both photophobia and phonophobia, worsening with exercise, cervical topography, neuralgiform pain, or highly localized pain.
- 2.
Presence of abnormal neurological symptoms or signs, such as aphasia, dysarthria, sensory disturbances, paresis, visual symptoms, vertigo, instability, and papilledema.
- 3.
Presence of red flags related to the headache description, such as thunderclap onset, severe intensity (>9/10), progressive worsening, recent onset, worsening with Valsalva manoeuvre, precipitation by exercise, and refractoriness to appropriate treatment.
- 4.
Systemic symptoms, such as fever, chest pain, abdominal pain, arthralgia, diarrhoea, urethral syndrome, and localized ocular pain.
- 5.
Close temporal relation with an event able to produce headache, including cranial trauma, high blood pressure, lumbar puncture, and cranial surgery.
Discrepancies in prior medical history included prior headache disorders, cancer affecting encephalic structures, sinus disease, ophthalmological diseases able to produce ocular pain, sleep apnoea syndrome, and any other intra- or extracranial conditions able to produce headache.
For the third objective, two headache specialists (NGG, DGA) independently reviewed each case and analysed the information present in the discharge reports. With that information, when possible, patients were re-assessed according to ICHD-3 (77). In case of discrepancies, a third headache specialist (JPE) solved the disputes.
We also evaluated the management of patients. We determined the total duration of the emergency department stay, from when the patient was admitted to discharge. We analysed whether patients had been examined, specifically reviewing whether fundoscopy had been done. Complementary exam referrals were also addressed, including lumbar puncture, cranial tomography (CT), X-ray, and laboratory exams. Management at discharge was reviewed, inspecting if any treatment had been prescribed and if patients were referred to the neurological department. We compared whether patients who had undergone neurological exams or complementary exams had a longer stay and if they were more often diagnosed correctly.
The local ethics committee board approved the study. The study was performed according to the principles of the Declaration of Helsinki. Informed consent was obtained from all the participants.
Statistics
Qualitative variables are presented as frequencies and percentages. Quantitative variables are presented as the means and standard deviations (sds) or medians and interquartile ranges (IQRs) in the case of a nonnormal distribution. Normality was tested by using the Kolmogorov-Smirnov test. The first three endpoints did not include statistical analysis and were based on descriptive qualitative data. As we analysed only patients with a definite TTH diagnosis, we only determined the positive predictive value of TTH diagnosis. In the analysis of the management of patients, for the comparison of qualitative variables, we used the chi squared test. When comparing two continuous variables, we used Student’s t test if a normal distribution was shown in the Kolmogorov-Smirnov test, and we used the Kruskal-Wallis test if the data were not normally distributed. We considered a p-value as significant if it was lower than 0.05 and specified degrees of freedom (df). In case of missing data, we performed complete-case analysis. We did not anticipate any sample size a priori but included all possible patients during the study period.
Ethics approval and consent to participate
The Clinical Research Ethics Committee of Hospital Clínico San Carlos approved the study. Informed consent forms were obtained from the participants.
Consent for publication
All authors gave their consent for publication.
Results
During the study period, 2132 patients visited the ED because of headache. The inclusion/exclusion criteria were satisfied by 211 patients (9.9% of the total sample), and these patients were included in the study. The median age of the patients was 42.6 years [30.9–57.3], and 75.6% were female.
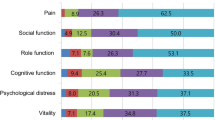
Tension-type headache criteria
Only five patients fulfilled all ICHD criteria for TTH (2.4% of the included patients). The frequencies at which each criterion was referenced were as follows: criterion A was referenced in 81% of patients and fulfilled in 16% of patients, criterion B was referenced in 84% of patients and fulfilled in 74% of patients, criterion C was mentioned in 72% of patients and fulfilled in 43% of patients, and criterion D was referenced in 60% of patients and fulfilled in 56% of patients. Figure 1 shows the percentage of patients who fulfilled each criterion.
Discrepancies in TTH diagnosis
There was at least one discrepancy in regard to anamnesis in 184 patients (87.2%). Symptoms suggestive of another headache disorder were present in 131 subjects (62.1%); 87 patients (41.2%) described other neurological symptoms; red flags were identified in 55 patients (26.1%); 57 subjects (27.0%) also reported systemic symptoms; and in 31 patients (14.6%), an event able to produce headache was described.
Concerning events related to headache onset, in 12 patients, traumatic injury to the head had occurred in the prior 7 days and was mentioned by patients; in 11 patients, an acute increase in blood pressure (BP) over 180/140 was documented, with cessation of headache after proper BP management; in three patients, headache started after dental manipulation with no prior history of headache; in two patients, headache began after the use of corticosteroids or amisulpride and olanzapine; in two patients, headache started after lumbar puncture; and in one patient, an intracranial aneurism was embolized the same day the headache started.
Regarding prior medical history, 44 patients (20.85%) had some condition able to produce headache. In 17 patients, a prior history of migraine was present. Those patients referred to an unchanged headache phenotype that was resistant to treatment; nine patients had acute sinusitis, four patients had painful ophthalmological conditions (glaucoma in two, ophthalmic herpes in one and acute uveitis in one), three patients had cerebral and arteriovenous malformation, two patients had a recent history of subarachnoid haemorrhage, two patients had a history of intracranial cerebrospinal fluid (CSF) hypotension, one patient had cerebellar haemangioblastoma, one patient had Erdheim-Chester disease, one patient had a history of temporal arteritis, one patient had a history of occipital neuralgia, one patient had sleep apnoea, one patient had intracranial aneurism and one patient had polycythaemia vera with hyperviscosity syndrome.
Re-classification according to ICHD-3
After reviewing all the discharge reports, only 21 patients (9.9% of the included sample, 0.98% of the total sample) fulfilled the ICHD-3 criteria for tension-type headache (five) or probable tension-type headache (16). The positive predictive value of TTH diagnosis was 0.099. In 106 patients, another ICHD-3 diagnosis was met (50.2% of patients). In 64 patients, a secondary headache was the final diagnosis (30.3%), with 13 having high-risk secondary headaches (6.1%). Figure 2 and Table 2 show the number of patients encoded in each classification group and the specific diagnoses.
Management of patients
The total duration of the ED visits, from admission to discharge, had a median length of 3.59 hours [IQR: 2.5–5.1], with a range between 0.35 and 19.10 hours. Neurological examination was described in the reports of 90.5% of patients and was abnormal in 6.8% of these patients. When the neurological exam was done, the duration of the ED visit was 4.0 hours vs. 3.9 hours when it was not done (Student’s t test, 22 df, p = 0.87). Fundoscopy was performed in 10.9% of patients, and the results were normal in all cases.
The diagnosis was more often appropriate in patients who underwent fundoscopy (chi-square test, 1 df, p = 0.004).
Regarding complementary exams, laboratory exams were performed in 32.6% of patients. Laboratory exams including erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP) were performed in 48.6% of patients older than 65 years old. Cranial CT was performed in 11.3% of patients, and cervical or sinus X-ray was performed in 12.7% of patients. Only 2 CT exams were abnormal, one exhibiting a vascular malformation and the other with acute inflammation of the frontal sinuses. Figure 3 summarizes the percentage of patients who underwent each examination.
When complementary exams were performed, the mean duration of the stay increased from 3.28 to 4.94 hours (Student’s t test, 217 df, p < 0.001). Requests for complementary exams were not associated with a higher probability of proper diagnosis (chi-square, 1 df, p = 0.71). At discharge, 21.3% of patients were referred for a neurological examination. In 90% of the discharge reports, some acute medications were prescribed.
Discussion
The present study was performed in the emergency department setting. We systematically analysed a series of patients with definite TTH diagnosis according to whether the diagnostic criteria were mentioned and fulfilled in the discharge report. We screened the reports for the presence of data that would contradict TTH diagnosis, and finally, we tried to reclassify patients based on the information provided in the reports.
The main findings of our study were that only a minority of patients, only 2.4% of the whole sample, fulfilled the ICHD criteria for TTH. In over 80% of patients, a discrepancy was found in the anamnesis, and in one-fifth of patients, prior medical history made TTH diagnosis unlikely. Finally, when we tried to reclassify patients, migraine diagnosis was two-times more frequent than TTH diagnosis. In almost 40% of patients, the information was not sufficient for a diagnosis, so in the best possible scenario, only half of patients with TTH diagnosis would have this condition, leading to a total percentage of 4.9% of the whole sample.
Concerning the ICHD criteria6, the most frequently mentioned criterion was duration, followed by number of episodes and phenotype. The most surprising data were that criterion A, describing the number of episodes, was mentioned in 81% of cases, but it was only fulfilled in 16% of cases. This fact may reflect the idea that many patients visit the emergency department due to recent-onset headaches. New onset headache and progressive worsening are two of the main red flags18. In patients with primary headaches, a previous history of similar unchanged attacks might constitute a green flag.
The ICHD Criteria for TTH, unchanged since the first edition3, attempt to differentiate TTH from the other main primary headache, migraine. The criteria include positive, negative and exclusion criteria. The positive criteria describe the typical characteristics of TTH: bilateral, pressing, and relatively mild. The negative criteria rule out the presence of typical migraine features, such as nausea, vomiting, photophobia and phonophobia or worsening as a result of activity. Finally, as in every ICHD diagnosis, the condition should not be better described by any other diagnosis. In the literature, some series have diagnosed TTH in 53% of patients with nausea19. Other series included patients who were diagnosed with TTH who had pulsating (23.8%) and hemicranial headaches (20.1%)20.
The typical TTH phenotype is probably the most unspecific, and many conditions might have similar features, such as migraine, hemicrania continua, primary cough headache, primary exercise headache, primary headache associated with sexual activity, external-pressure headache, hypnic headache, new daily persistent headache and the vast majority of secondary headache disorders6,8. Misdiagnosis might be related to the classification of patients based on pain phenotype; however, headache diagnosis should be performed by integrating prior medical history, headache anamnesis, presence of other symptoms and neurological examination, not solely by headache phenotype8,21.
The confusion surrounding TTH diagnosis might be partly influenced by the many names that have been used to describe this condition: tension headache, muscle contraction headache, psychomyogenic headache, stress headache, ordinary headache, essential headache, idiopathic headache, or psychogenic headache3,4,5,6. Some of these names may suggest a psychogenic cause. Currently, we consider stress and affective disorders a cause of worsening or a trigger rather than the cause of headache22,23.
Medical attention at the emergency department usually prioritizes the detection of life-threatening conditions. The frequent saturation, rush and wide variety of conditions complicate the thorough and meticulous anamnesis that headache disorders require. In our sample, 30% of patients had a secondary headache, and 5% of patients had a secondary headache with potential morbimortality. In a previous series, up to 10% of patients diagnosed with TTH had an abnormal examination18.
One of the biggest needs in the headache field is the development of reliable biomarkers. Unlike other painful syndromes, such as chest or abdominal pain, we still base our diagnosis on anamnesis and neurological examination18. Some rules16 and lists of red flags have been proposed to detect secondary headaches24. CT and lumbar puncture, although frequently requested18,25,26, do not always rule out many entities, such as cerebral venous sinus thrombosis, intracranial space-occupying lesions, or cerebrospinal fluid pressure disorders.
Headache is one of the leading reasons for consultation, accounting for 2.3% of all ED visits;14,15,18 therefore, all ED physicians should be trained in headache medicine. In our sample, just a minority of patients underwent fundoscopy, and in many cases, even plain X-ray was requested. The use of lab tests was not properly selected for elderly patients, as less than half of the patients had an ESR or CRP exam.
Sometimes an accurate diagnosis cannot be made; in our study, up to 38% of patients had an unspecific diagnosis, with this figure reaching 38–45% in the literature24,27. In those cases, it is important to note that declaring a primary headache disorder without certainty might implicate the end of the diagnostic work-up and a higher risk of complications. In case of doubt, final diagnosis should be “possible” or “headache not otherwise specified”11,13,24.
The consequences of inaccurate diagnosis are the risk of morbimortality among patients, inappropriate use of diagnostic resources, and the potential cost of establishing the proper diagnosis. Treatment of different secondary headaches differs widely, and in many conditions, prognosis is correlated with a prompt and proper treatment, as in the case of temporal arteritis, cerebral venous sinus thrombosis, or central nervous system infections13.
Although tension-type headache is supposed to be the most prevalent primary headache disorder28,29, it is seldom treated in headache outpatient clinics30, and some authors even suggest that patients diagnosed with TTH suffer from improperly diagnosed migraines in at least one-third of the cases31,32. Research on TTH and knowledge about its pathophysiology are also scarcer than those of other primary headaches, such as cluster headache or migraine2,33.
In many cases, TTH has been related to psychosocial factors22, and when patients complain of stress or mood disorders, TTH diagnosis is often made. It is well known that primary headache disorders are associated with significant personal, societal and familiar burdens30.
The pre-test probability of having TTH is 60–70%1,2 in the general population, but in the ED setting, it is important to clarify whether the headache that motivated the consult has changed, worsened progressively, resisted treatment or had new features. With regard to prior medical history, in our sample, one-fifth of the patients had conditions able to produce headaches, and 8% of the subjects were migraineurs. It is well known that chronic migraine exhibits a less typical phenotype, and some of the episodes might resemble TTH episodes34. In the diagnosis of chronic migraine, only 8 out of the minimum 15 headaches per month are needed to fulfil the migraine without or with aura criteria6.
The main limitations of the present study are the participation of a single centre, which might affect the generalizability of the results. Because of the design of the study, some data could have been asked and evaluated but not written; however, from a legal perspective, non-written data did not “occur”. The re-classification was performed without evaluating patients; therefore, there was potential for misclassification, and we used the current ICHD instead of the two editions valid during the study period (ICHD-2 and ICHD-3 beta). We did not follow up with patients to confirm the final diagnosis. The strengths of the study are the thorough review of every patient chart, the participation of headache experts and the three different analyses performed.
Conclusion
In our sample, TTH was overdiagnosed in an emergency department, as only 2.4% of the patients fulfilled all ICHD criteria for TTH. Inconsistencies in prior medical history or anamnesis were present in the discharge reports in one-fifth and four-fifths of patients, respectively. Our analysis of medical records allowed us to reclassify these patients as having other primary or secondary headaches. Efforts to improve knowledge on headache disorders and ICHD are needed among ED physicians.
Data availability
Study material and supplementary material are available upon request from the corresponding author.
References
Jensen, R. H. Tension-type headache – the normal and most prevalent headache. Headache. 58(2), 339–345 (2018).
Bendtsen, L. & Jensen, R. Tension-type headache: the most common, but also the most neglected, headache disorder. Curr. Opin. Neurol. 19, 305–309 (2006).
Headache Classification Committee of the International Headache Society. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalalgia. 8(suppl 7), 1–96 (1988).
Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders, 2nd Edition. Cephalalgia. 24(suppl 1), 9–160 (2004).
Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disroders, 3rd edition (beta version). Cephalalgia. 33(9), 629–808 (2013).
Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 38, 1–211 (2018).
Guerrero, A. L. et al. Characteristics of the first 1000 headaches in an outpatient headache clinic registry. Headache. 51(2), 226–31 (2011).
Crystal, S. C. & Robbins, M. S. Tension-type headache mimics. Curr. Pain. Headache. Rep. 15, 459–466 (2011).
Maizels, M. Headache evaluation and treatment by primary care physicians in an emergency department in the era of triptans. Arch. Intern. Med. 161, 1969–1973 (2001).
Dermitzakis, E. V. et al. Headache patients in the emergency department of a Greek tertiary care hospital. J. Headache. Pain. 11, 123–128 (2010).
Sahai-Srivastava, S., Desai, P. & Zheng, L. Analysis of headache management in a busy emergency room in the United States. Headache. 48, 931–938 (2008).
Friedman, B. W. et al. Applying the International Classification of Headache Disorders to the Emergency Department: An assessment of reproducibility and the frequency with which unique diagnosis can be assigned to every acute headache presentation. Ann. Emerg. Med. 49, 409–419 (2007).
Relja, G. et al. Nontraumatic headache in the Emergency Department: a survey in the province of Trieste. J. Headache. Pain. 6, 290–300 (2005).
Barton, C. W. Evaluation and treatment of headache patients in the emergency department: A survey. Headache. 34, 91–94 (1994).
Munoz-Ceron, J., Marin-Careaga, V., Peña, L., Mutis, J. & Ortiz, G. Headache at the emergency room: etiologies, diagnostic usefulness of ICHD-3 criteria, red and green flags. Plos One. 14(1), e0209728 (2019).
Do, T. P. et al. Red and orange flags for secondary headaches in clinical practice. SNNOOP10 list. Neurology. 92, 134–144 (2019).
Vandenbroucke, J. P. et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. PLoS Med. 4(10), e297 (2007).
Locker, T., Mason, S. & Rigby, A. Headache management- Are we doing enough? An observational study of patients presenting with headache to the emergency department. Emer. Med. J. 21, 327–332 (2004).
Bo, S. H., Davidsen, E. M., Guldbrandsen, P. & Dietrichs, E. Acute headache: a prospective work-up of patients admitted to a general hospital. Eur. J. Neurology. 15, 1293–1299 (2008).
Li, X. et al. Clinical characteristics of tension-type headache in the neurological clinic of university hospital in China. Neurol. Sci. 33, 283–287 (2012).
Kaniecki, R. G. Tension-type headache. Continuum Lifelong Learning Neurol. 18(4), 823–834 (2012).
Kaynak Key, F. N., Donmez, S. & Tuzun, U. Epidemiological and clinical characteristics with psychosocial aspects of tension-type headache in Turkish college students. Cephalalgia. 24, 669–674 (2004).
Ashina, S. et al. Neuroticism, depression and pain perception in migraine and tension-type headache. Acta Neurol. Scand. 136, 470–476 (2017).
Chu, K. H. et al. Acute headache presentations to the Emergency Department: A statewide cross-sectional study. Acad. Emerg. Med. 24(1), 53–62 (2017).
Morgenstern, L. B. et al. Headache in the emergency department. Headache. 41, 537–541 (2001).
Goldstein, J. N., Camargo, C. A. Jr., Pelletier, A. J. & Edlow, J. A. Headache in United States Emergency Departments: demographics, work-up and frequency of pathological diagnoses. Cephalalgia. 26, 684–690 (2006).
Ruiz, F. B., Santos, M. S., Siqueira, H. S. & Cotta, U. C. Clinical features, diagnosis and treatment of acute primary headaches at an emergency center. Acta Neuropsiquiatr. 65(4-B), 1130–1133 (2007).
Stovner, L. J. et al. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia. 27, 193–210 (2007).
Sahler, K. Epidemiology and cultural differences in Tension-type headache. Curr. Pain Headache Rep. 16, 525–532 (2012).
Rasmussen, B. K., Jensen, R. & Olesen, J. Impact of headache on sickness absence and utilisation of medical services: a Danish population study. J Epidemiol. Community Health. 46(4), 443–446 (1992).
Lipton, R. B., Cady, R. K., Stewart, W. F., Wilks, K. & Hall, C. Diagnostic lessons from the Spectrum Study. Neurology. 58(suppl 6), S27–S31 (2002).
Blumenfeld, A., Schim, J. & Brower, J. Pure tension-type Headache versus Tension-type headache in the migraneur. Curr. Pain Headache Rep. 14, 465–469 (2010).
Fernandez-de-las-Peñas, C. & Arendt-Nielsen, L. Improving understanding of trigger points and widespread pressure pain sensitivity in tension-type headache patients: clinical implications. Expert Rev. Neurother. 17(9), 933–939 (2017).
Turkdogan, D. et al. Characteristic and overlapping features of Migraine and Tension-Type Headache. Headache. 46, 461–468 (2006).
Acknowledgements
We acknowledge our emergency department colleagues for all their support.
Author information
Authors and Affiliations
Contributions
All authors participated in the design of the study. D.G.A. and M.F. created the questionnaire, A.L.G.P., J.P.E., M.G. and N.G.G. reviewed the questionnaire. M.F. and D.G.A. reviewed all cases and N.G.G. and M.G. solved the disputes. D.G.A. wrote the first draft and all the authors reviewed and approved the final draft.
Corresponding author
Ethics declarations
Competing interests
We assure that this study represents original work. The present was been partially presented at the 2nd European Academy of Neurology Congress.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
García-Azorín, D., Farid-Zahran, M., Gutiérrez-Sánchez, M. et al. Tension-type headache in the Emergency Department Diagnosis and misdiagnosis: The TEDDi study. Sci Rep 10, 2446 (2020). https://doi.org/10.1038/s41598-020-59171-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-59171-4
This article is cited by
-
Health equity, care access and quality in headache – part 1
The Journal of Headache and Pain (2024)
-
Lost diagnoses in not otherwise specified headache in Emergency Department
Acta Neurologica Belgica (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.