Abstract
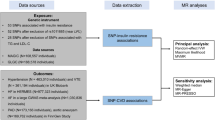
Resistant hypertension (RH) is defined as uncontrolled blood pressure despite treatment with three or more antihypertensive medications, including, if tolerated, a diuretic in adequate doses. It has been widely known that race is associated with blood pressure control. However, intense debate persists as to whether this is solely explained by unadjusted socioeconomical variables or genetic variation. In this scenario, the main aim was to evaluate the association between genetic ancestry and resistant hypertension in a large sample from a multicenter trial of stage II hypertension, the ReHOT study. Samples from 1,358 patients were analyzed, of which 167 were defined as resistant hypertensive. Genetic ancestry was defined using a panel of 192 polymorphic markers. The genetic ancestry was similar in resistant (52.0% European, 36.7% African and 11.3% Amerindian) and nonresistant hypertensive patients (54.0% European, 34.4% African and 11.6% Amerindian) (p > 0.05). However, we observed a statistically suggestive association of African ancestry with resistant hypertension in brown patient group. In conclusion, increased African genetic ancestry was not associated with RH in Brazilian patients from a prospective randomized hypertension clinical trial.
Similar content being viewed by others
Introduction
Hypertension is one of the predominant driver of cardiovascular diseases1. Many studies have correlated the predisposition to hypertension with African ancestry2,3,4,5. In particular, apart from the association with Black race (which has been extensively described), much discussion persists on the reasons for this association. For one point, socioeconomically inequalities are pervasive in most Western populations and known to be very difficult to adjust for in epidemiological studies6. Nonetheless, several lines of evidence also point to a higher frequency of potentially deleterious alleles in individuals with high African ancestry, leaving the question of into what degree the association between hypertension and race is biologically defined7. This may have wide impact on the future management of hypertension from a medical standpoint, as well as in the development of health policies targeted as reducing the impact of chronic disease in the general population.
Resistant hypertension (RH) is defined by uncontrolled blood pressure despite treatment with three or more antihypertensive medications, including, if tolerated, a diuretic in adequate doses8,9. Patients with RH have even higher risk of cardiovascular complications than hypertensive patients10. It is estimated that 10–20% of people with hypertension are resistant, underscoring the importance of understanding the determinants of this condition11,12,13.
In Brazil, self-declared race/color is based on a complex subjective phenotypic and cultural assessment because the Brazilian population is highly admixed with the main ancestral contributing populations being European, African and Amerindian14,15. Of particular importance to the present work most Brazilians are defined as a mosaic of these three main ancestries and a much higher degree of discordance between self-referred race and genetic ancestry is seem as compared to the US16,17,18.
In this scenario, we have an interesting hypertensive population to evaluate, with systolic blood pressure >160 mmHg and <220 mmHg, and/or diastolic >100 mmHg, in the seated position19. These measurements were taken until two consecutive measurements differing less than 4 mmHg between them, with a very controlled methodology and prospectively, being a robust way to identify RH patients. Thus, with a significant number of diagnosed RH patients, we sought to evaluate a possible association of genetic ancestry with RH in a large multicenter prospective randomized clinical trial from the ReHOT study20.
Material and Methods
Study population
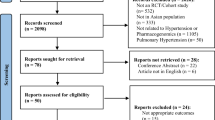
The patients come from a prospective randomized clinical trial (Resistant Hypertension Optimal Treatment - ReHOT) that was conducted between 2012 and 2014. It included hypertensive patients from 26 sites located in different states in Brazil20. The Ethics Committee for Human Medical Research of the Clinical Hospital of the School of Medicine, University of São Paulo approved the study protocol (protocol number 0758/09) and all individuals signed an informed consent form in accordance with the Declaration of Helsinki and good clinical practice guidelines. This study was registered at clinicaltrials.gov under the number NTC1643434.
Genotyping data
Individuals from the ReHOT project were genotyped using genomic DNA in the Open Array platform with QuantStudioTM 12 K FlexTM. A commercial genotyping custom chip from Applied BiosystemsTM, containing 192 single nucleotide polymorphisms (SNPs which can be seen in Supplementary Table 1), was used to perform genotyping through real-time PCR. In this method, each chip had enough arrays to obtain the 192 genotypes of 15 individuals at the same time and a further negative control reaction to evaluate the quality of genotyping. Estimates of individual admixture using this 192 AIM panels were highly correlated with estimates using ~370 000 genome-wide SNPs: 91%, 92%, and 74% of, respectively, African, European, and Native American ancestry components21.
Genetic ancestry
Ancestry informative markers (AIM) are important tools to differentiate populations and estimate proportions of ancestry. These analyze are based on genetic ancestry (GA) whose allelic polymorphisms frequencies vary markedly in different racial and ethnic groups and they can be used to control wrong results from stratifications and analyses by race22. The implementation of the panels of AIM, in platforms high-throughput genotyping, would facilitate simultaneous mapping of characteristics of complex diseases23.
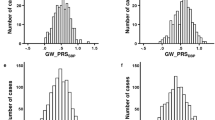
The analysis of GA was performed using the Admixture program24, which is a tool for estimating the maximum likelihood of individual ancestors of data sets of multilocus SNP genotypes. The ancestry proportions were estimated for our samples using the panel of AIMs and samples from HapMap, HGDP and 1000 Genomes projects as reference for European, African and Native American populations21.
The reference populations used for African were ASW, LWK and YRI from HapMap3 (Americans of African Ancestry in SW USA; Luhya in Webuye, Kenya; Yoruba in Ibadan, Nigeria); Bantu and Mandenka from HGDP (Sub-Saharan Africa). The populations used for European were CEU and TSI from HapMap3 (Utah Residents with Northern and Western European ancestry; Tuscany in Italy); GBR and IBS from 1000 Genomes (British in England and Scotland; Iberian population in Spain) and Orcadian, Russian from HGDP (Northern Europe). In the end, the populations used for Amerindian were MEX from 1000 Genomes (Mexican Ancestry from Los Angeles USA); Pima, Maya, Karytiana and Surui from HGDP (Mexico and Brazil). After choosing the populations, the GA of each patient in the Admixture program was calculated24.
Statistical analysis
Manipulation of the genotypic database was done by the PLINK program25. For the statistical analysis, we used the R program (version 3.0.0). Chi-square or Fisher’s exact tests were used to compare categorical variables. Resistant hypertension was used as a binary variable. T-test, Mann-Whitney, Anova and Kruskal-Wallis were used to determine differences between the means of numerical variables.
Results
Samples from 1,358 patients were analyzed for the proportions of EUR, AFR and AMR ancestry. From these, 165 were resistant hypertensive patients. Table 1 shows general and clinical characteristics of patients according to self-declared race/color groups. The average age was 54.7 years for whites and 52.9 years for non-whites. The mean blood pressure was 172.5/102.6 mmHg and 42% of the patients were males and 58% females. As expected there was a highly significant association between genetic ancestry (GA) and self-declared race/color (Supplementary Table 2). Table 2 shows that the proportion of ancestry was not associated with resistant or nonresistant hypertensive patients. The GA proportions were similar in both groups with 52.0% European, 36.7% African and 11.3% Amerindian for resistant and 54.0% European, 34.4% African and 11.6% Amerindian (p > 0.05) for nonresistant patients.
A stratified analysis was performed on two groups (white and non-white) (Table 3). The group of non-whites (black and brown patients) had 684 nonresistant and 99 resistant patients, whereas the group of whites had 509 nonresistant and 66 resistant patients, but no significant difference was found between these groups.
In an analysis stratified by white, brown and black, no significant association of the GA with RH was observed (Supplementary Table 3). However, we observed a statistically suggestive association of African ancestry with resistant hypertension in brown patient group in a model shown in Supplementary Table 4. Thus, we evaluated a possible association of general variables on African ancestry (dividing into 2 groups among African ancestry median), in this brown group. We did not find association of general variables with African ancestry in this analysis (Supplementary Table 5).
Discussion
The ReHOT study identified 11.7% of hypertensive patients that fulfilled the RH criteria. In the study, there was no association between self-declared race/color with RH26. In the present study, our hypothesis of a possible association of genetic ancestry with RH was not confirmed.
Some studies showed an association of black race/color with higher prevalence of RH patients. One of them showed a prevalence of RH of 7.3% in European Americans, while there was a greater proportion of RH patients in African Americans (10.6%)27. Another study, developed in an ethnically and socioeconomically diverse population from California, identified a RH cohort of 12.8% from hypertensive patients. It found that they were more likely to be black8. Some variables, such as advanced age, increased body mass index, male gender, genetic variants and others chronic diseases were also associated with RH or uncontrolled hypertension28,29,30,31.
On the other hand, some studies, including the present study, did not find an association of self-reported race/color with RH. A study with 9,361 hypertensive patients from the US, did not find differences in RH proportions according to race32. In addition, a meta-analysis, which analyzed the global prevalence of RH from data of 3.2 million patients, did not observe differences33. Some studies have observed genetic variants associated with risk for resistant hypertension2,34,35. However, to the best of our knowledge, studies of genetic ancestry and RH are not identified in the literature. Our hypothesis was that an increased proportion of African ancestry might be a risk factor for RH, in the overall group or even in subgroups among self-declared race/color, but this was not confirmed. However, in brown patient group, we identified a statistically suggestive association of African ancestry with resistant hypertension. This statistically suggestive association suggests that the criteria applied to segregate the race/color groups, according Brazilian Institute of Geography and Statistics, are possibly distorting the real distribution and, at least in part, leading a limitation for dividing into homogeneous groups. Thus, further investigations and new hypothesis should be tested to elucidate possible associations.
The prevalence and incidence of RH will grow considerably because there is a large number of overweight/obese individuals36. In addition, the cutoff blood pressure criteria for RH was reduced from 140/90 mmHg to < 130/80 mmHg9. Thus, prevent damages by RH and identify better treatments is important, because the number of RH patients can increase with this new cutoff37,38,39,40. A possible limitation of our study is the low statistical power to differentiate mean values of African ancestry among patient groups.
Conclusion
In the present study, genetic ancestry was not associated with resistant hypertension in Brazilian patients from a prospective randomized clinical trial.
References
Franklin, S. S. & Wong, N. D. Hypertension and cardiovascular disease: contributions of the framingham heart study. Glob Heart. 8, 49–57 (2013).
Jones, E. S. et al. High Frequency of Variants of Candidate Genes in Black Africans with Low Renin-Resistant Hypertension. Am J. Hypertens. 30, 478–483 (2017).
Yaméogo, N. V. et al. [Epidemiological characteristics and clinical features of black African subject’s resistant hypertension]. Ann Cardiol Angeiol (Paris) 63, 83–8 (2014).
Sim, J. J. et al. Characteristics of resistant hypertension in a large, ethnically diverse hypertension population of an integrated health system. Mayo Clin Proc. 88, 1099–107 (2013).
Padmanabhan, S. & Joe, B. Towards Precision Medicine for Hypertension: A Review of Genomic, Epigenomic, and Microbiomic Effects on Blood Pressure in Experimental Rat Models and Humans. Physiol Rev. 97, 1469–1528 (2017).
Lima-Costa, M. F. et al. Socioeconomic Position, But Not African Genomic Ancestry, Is Associated With Blood Pressure in the Bambui-Epigen (Brazil) Cohort Study of Aging. Hypertension. 67, 349–55 (2016).
Santos, H. C. et al. Self-declared ethnicity associated with risk factors of cardiovascular diseases in an urban sample of the Brazilian population: the role of educational status in the association. Int J Cardiol. 168, 2973–5 (2013).
James, P. A. et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 311, 507–20 (2014).
Whelton, P. K. et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 71, e13–e115 (2018).
Wei, F. F. et al. Diagnosis and management of resistant hypertension: state of the art. Nat Rev Nephrol. 14, 428–441 (2018).
Bortolotto, L. A. et al. Renal denervation by ablation with innovative technique in resistant hypertension. Arq Bras Cardiol. 101, e77–9 (2013).
Kumbhani, D. J. et al. Resistant hypertension: a frequent and ominous finding among hypertensive patients with atherothrombosis. Eur Heart J. 34, 1204–14 (2013).
Sarafidis, P. A. Epidemiology of resistant hypertension. J Clin Hypertens (Greenwich). 13, 523–8 (2011).
Gonçalves, V. F. et al. The phylogeography of African Brazilians. Hum Hered. 65, 23–32 (2008).
Pena, S. D. et al. The genomic ancestry of individuals from different geographical regions of Brazil is more uniform than expected. PLoS One. 6, e17063 (2011).
Kehdy, F. S. et al. Origin and dynamics of admixture in Brazilians and its effect on the pattern of deleterious mutations. Proc Natl Acad Sci USA 112, 8696–701 (2015).
Cardena, M. M. et al. Assessment of the relationship between self-declared ethnicity, mitochondrial haplogroups and genomic ancestry in Brazilian individuals. PLoS One. 8, e62005 (2013).
Lima-Costa, M. F. et al. Genomic ancestry and ethnoracial self-classification based on 5,871 community-dwelling Brazilians (The Epigen Initiative). Sci Rep. 5, 9812 (2015).
Cardiologia, S. B. D., Hipertensão, S. B. D. & Nefrologia, S. B. D. [VI Brazilian Guidelines on Hypertension]. Arq Bras Cardiol. 95, 1–51 (2010).
Krieger, E. M. et al. Resistant hypertension optimal treatment trial: a randomized controlled trial. Clin Cardiol. 37, 1–6 (2014).
Santos, H. C. et al. A minimum set of ancestry informative markers for determining admixture proportions in a mixed American population: the Brazilian set. Eur J Hum Genet. 24, 725–31 (2016).
Marini, S. et al. Comparison of Genetic and Self-Identified Ancestry in Modeling Intracerebral Hemorrhage Risk. Front Neurol. 9, 514 (2018).
Zhang, X. et al. Ancestry-informative markers for African Americans based on the Affymetrix Pan-African genotyping array. PeerJ. 2, e660 (2014).
Alexander, D. H., Novembre, J. & Lange, K. Fast model-based estimation of ancestry in unrelated individuals. Genome Res. 19, 1655–64 (2009).
Purcell, S. et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet. 81, 559–75 (2007).
Krieger, E. M. et al. Spironolactone Versus Clonidine as a Fourth-Drug Therapy for Resistant. Hypertension: The ReHOT Randomized Study (Resistant Hypertension Optimal Treatment). Hypertension 71, 681–690 (2018).
Shuey, M. M. et al. Characteristics and treatment of African-American and European-American patients with resistant hypertension identified using the electronic health record in an academic health centre: a case-control study. BMJ Open. 8, e021640 (2018).
Dudenbostel, T. et al. Refractory Hypertension: A Novel Phenotype of Antihypertensive Treatment Failure. Hypertension. 67, 1085–92 (2016).
Huan, T. et al. A meta-analysis of gene expression signatures of blood pressure and hypertension. PLoS Genet. 11, e1005035 (2015).
Scuteri, A. et al. Gender specific profiles of white coat and masked hypertension impacts on arterial structure and function in the SardiNIA study. Int J Cardiol. 217, 92–8 (2016).
Di Daniele, N. et al. Circadian blood pressure patterns and blood pressure control in patients with chronic kidney disease. Atherosclerosis. 267, 139–145 (2017).
Smith, S. M. et al. Optimal Systolic Blood Pressure Target in Resistant and Non-Resistant Hypertension: A Pooled Analysis of Patient-Level Data from SPRINT and ACCORD. Am J Med. 131, 1463–1472.e7 (2018).
Noubiap, J. J. et al. Global prevalence of resistant hypertension: a meta-analysis of data from 3.2 million patients. Heart. 105, 98–105 (2019).
Tragante, V. et al. Gene-centric meta-analysis in 87,736 individuals of European ancestry identifies multiple blood-pressure-related loci. Am J Hum Genet. 94, 349–60 (2014).
Franceschini, N. et al. Genome-wide association analysis of blood-pressure traits in African-ancestry individuals reveals common associated genes in African and non-African populations. Am J Hum Genet. 93, 545–54 (2013).
Pio-Abreu, A. & Drager, L. F. Resistant Hypertension: Time to Consider the Best Fifth Anti-Hypertensive Treatment. Curr Hypertens Rep. 20, 67 (2018).
Calhoun, D. A. Advances in resistant hypertension. Ann Transl Med. 6, 294 (2018).
Teixeira, S. K., Pereira, A. C. & Krieger, J. E. Genetics of Resistant Hypertension: the Missing Heritability and Opportunities. Curr Hypertens Rep. 20, 48 (2018).
James, A. et al. Impact of a Population Health Management Intervention on Disparities in Cardiovascular Disease Control. J Gen Intern Med. 33, 463–470 (2018).
Acelajado, M. C. et al. Refractory hypertension: definition, prevalence, and patient characteristics. J Clin Hypertens (Greenwich). 14, 7–12 (2012).
Acknowledgements
We thank the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP, São Paulo, Brazil) - projects - 2013/09295-3 and 2013/24440-0 and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq, Brasília, Brazil). This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001.
Author information
Authors and Affiliations
Contributions
C.T.B., A.C.P. and P.C.J.L.S. drafted the study protocol. A.C.P., E.M.K. and J.E.K. participated in the design of the ReHOT study. C.T.B., H.C.S., L.M.G.G., A.R.V.R.H. and P.C.J.L.S. carried out the genetic tests and statistical analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bueno, C.T., Pereira, A.C., Santos, H.C. et al. Association of the genetic ancestry with resistant hypertension in the ReHOT (Resistant Hypertension Optimal Treatment) randomized study. Sci Rep 10, 1476 (2020). https://doi.org/10.1038/s41598-020-58540-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-58540-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.