Abstract
Collective cell migration plays important roles in various physiological processes. To investigate this collective cellular movement, various wound-healing assays have been developed. In these assays, a “wound” is created mechanically, chemically, optically, or electrically out of a cellular monolayer. Most of these assays are subject to drawbacks of run-to-run variations in wound size/shape and damages to cells/substrate. Moreover, in all these assays, cells are cultured in open, static (non-circulating) environments. In this study, we reported a microfluidics-based wound-healing assay by using the trypsin flow-focusing technique. Fibroblasts were first cultured inside this chip to a cellular monolayer. Then three parallel fluidic flows (containing normal medium and trypsin solution) were introduced into the channels, and cells exposed to protease trypsin were enzymatically detached from the surface. Wounds of three different widths were generated, and subsequent wound-healing processes were observed. This assay is capable of creating three or more wounds of different widths for investigating the effects of various physical and chemical stimuli on wound-healing speeds. The effects of shear stresses, wound widths, and β-lapachone (a wound healing-promoting chemical) on wound-healing speeds were studied. It was found that the wound-healing speed (total area healed per unit time) increased with increasing shear stress and wound width, but under a shear stress of 0.174 mPa the linear healing speed (percent area healed per unit time) was independent of the wound width. Also, the addition of β-lapachone up to 0.5 μM did not accelerate wound healing. This microfluidics-based assay can definitely help in understanding the mechanisms of the wound-healing process and developing new wound-healing therapies.
Similar content being viewed by others
Introduction
Collective cell migration plays important roles in various physiological processes such as embryonic development, tissue repair, angiogenesis, and wound healing1,2. Recently, researchers found that collective cell migration is highly involved in the invasion and spread of malignant cells3. When migrating collectively, cells often form the so-called self-assembled monolayers where they are attached to each other in mechanical and biochemical ways. This complicated phenomenon is observed to occur in cellular proliferation, cell-cell communication, and cell-micro-environment interaction. To investigate how cells migrate collectively, a number of different in vitro techniques have been developed4,5,6,7,8. For example, wound-healing assays are routinely used because they are convenient and easy-to-use. In these assays, cellular shape and collective movement can be followed in real-time for quantitative analysis of morphology and migration speed.
In a typical wound-healing experiment, it is necessary to create a “wound” out of a monolayer of cells. Then surrounding cells grow and migrate to cover this empty space9. For example, in the scratch wound-healing assay, a tip or needle is used to create a cell-free region10,11. This assay has been commercialized for investigating collective cell migration (the CellPlayer Migration Assay by Essen BioScience). Advantages of this assay include easy and quick procedures, applicability to any substrates, and easy records of cellular morphology and migration12. However, it does have some limitations13. First, in creating the cell-free region, the number of removed cells and the shape of the region can be different from experiment to experiment. Therefore, it is difficult to make a comparison in between. Second, in creating a wound, cells may be damaged mechanically, leading to the release of certain cellular chemicals into the micro-environment. The degree to which cells are damaged cannot be easily controlled, so the complexity in analyzing cell migration will highly increase. Thirdly, when an extracellular matrix (ECM) is coated on the surface for better cell attachment and proliferation, a mechanical scratch may cause partial loss or damage to the ECM. In contrast, the barrier wound-healing assay is more suitable for cell migration studies13,14. It provides a controllable wound shape/size and maintains surface integrity by using a barrier to keep cells away from the wound. This assay has been reported to give similar wound-healing responses compared to the scratch-based one15,16,17. In conducting the barrier wound-healing assay, a barrier is put onto the substrate prior to seeding cells to grow into a confluent monolayer, and then the barrier is removed to allow cells to migrate and recover the gap. Cell Biolabs (San Diego, CA USA) has commercialized the barrier assay named the CytoSelect™ Wound Healing Assay. Other wound-healing assays such as laser photoablation and electrical wound-healing assays have also been developed as substitutes13,18,19,20. Recently, our group developed an alternative wound-healing assay based on ultraviolet (UV) light ablation21. As reported, this UV wound-healing assay resulted in similar wound closure responses compared to the scratch assay, and it provides unique advantages such as fast, easy procedure and high throughput21.
In most of above-mentioned wound-healing assays, cells are cultured in open, static (non-circulating) systems. Experimental results found in these in vitro assays could be different from those occurring in vivo22. Therefore, microfluidic devices provide a more suitable platform for both culturing cells in an in vivo-like micro-environment and applying external stimuli in a precise and controllable manner. The first microfluidics-based wound-healing assay was reported by Nie et al. in 200723. Trypsin solutions in microfluidic channels form laminar flows to detach a portion of cellular monolayer, creating wounds similar to those occur in vivo. A migration distance of around 600 μm was observed after treating cells with epidermal growth factor-contained culture medium for 24 hr. Other similar microfluidics-based assays were reported to study wound-healing processes of various cell types including vascular smooth muscle cells24, endothelial cells25, and alveolar epithelial-like cells (A549)26,27. However, all these assays were limited to creating only one wound in one experiment, and the external stimuli to be applied were limited to chemicals. To increase the experimental throughput as well as to apply various physical/chemical stimuli, here we designed and developed a microfluidic chip serving as a novel, alternative wound-healing assay. By using the trypsin flow-focusing technique, this assay is capable of creating three or more wounds of different widths. The effects of shear stresses, wound widths, and β-lapachone on wound-healing speeds were studied. Although some scratch-based, barrier-based, and laser photoablation-based wound-healing assays have been reported to be high throughput19,28, the present microfluidic device can perform the assay in a non-contacting, fluid-circulating, and increased-throughput (compared with other microfluidics-based wound-healing assays) manner. This will definitely help in understanding the in vivo mechanisms of the wound-healing process.
Results and Discussions
Simulation and calculation of laminar flow and shear stress
Figure 1a shows the three-dimensional (3D) numerical simulation of trypsin concentration inside the microfluidic chip, where the concentrations in the central and side inlets were set to be 0.0214 mole/m3 and 0 mole/m3, respectively. As clearly seen, laminar flows were formed and flow-focusing was achieved inside the chip. Although the concentrations decreased from the upstream to the downstream, being average 0.0212 mole/m3, 0.0205 mole/m3, and 0.018 mole/m3 in the central flows of Area 1, Area 2, and Area 3, respectively, the values were close to the initial 0.0214 mole/m3. The one-dimensional (1D) concentration profiles along the widths of the microfluidic chip are shown in Fig. 1b. A stable trypsin concentration was formed in the center flow, which was used to detach cells and create the wound. As indicated by the dash lines, the regions where the trypsin concentration was constant had widths of around 1.42 mm, 0.91 mm, and 0.46 mm in Area 1, Area 2, and Area 3, respectively (double the lengths between zero and the dash lines). These values corresponded to 24%, 20%, and 15% of the channel widths (width = 6 mm, 4.5 mm, and 3 mm in Area 1, Area 2, and Area 3, respectively) and could be compared with the widths of the actual wounds.
(a) 3D numerical simulation of trypsin concentration inside the microfluidic chip. The concentrations in the central and side inlets were 0.0214 mole/m3 and 0 mole/m3, respectively. Scale bar = 6 mm. (b) 1D concentration profiles along different widths of the microfluidic chip. Three colors represent x positions along three different widths, starting from the middle to the right, as shown in the left (blue: the 6-mm width; green: the 4.5-mm width; red: the 3-mm width). Scale bar = 6 mm. The dash lines indicate the regions where the concentrations of trypsin were close to the initial value of 0.0214 mole/m3.
The shear stress inside the microfluidic chip was also simulated (data not shown). The simulated together with calculated values under different flow rates are listed in Table 1. In the treatment stage, the flow rate was set to be 1200 μL/min (800 μL/min in the side inlet and 400 μL/min in the central inlet), giving simulated shear stresses of around 158 mPa, 213 mPa, and 328 mPa in Area 1, Area 2, and Area 3, respectively. These extreme stresses were used to strip off cells and lasted for 10 min. In the healing stage, the flow rate was varied from 40 μL/hr to 400 μL/hr to investigate the effects of shear stresses on the wound-healing process. These rates corresponded to simulated shear stresses of 0.088 mPa (Area 1 under 40 μL/hr) to 1.83 mPa (Area 3 under 400 μL/hr). As indicated in the table, the errors between simulated and calculated values were in general less than 5%.
Flow focusing to create wounds
Figure 2 shows representative pictures of the wound-healing processes under a flow rate of 200 μL/hr and a β-lapachone concentration of 0.5 μM in the healing stage. The wound widths in Area 1, Area 2, and Area 3 were around 1.45 mm, 1.05 mm, and 0.59 mm, respectively. These values corresponded to 102%, 115%, and 128% of the widths where the trypsin concentration was constant in the simulation (see Fig. 1b). By increasing the number of segments having different widths in the microfluidic chip, more wounds of different sizes could be created to enhance the experimental throughput. After creating the wounds, time-lapse images were taken at 0 hr, 3 hr, 6 hr, 12 hr, and 24 hr to calculate the wound-healing speeds in the unit of μm2/min under different conditions.
Effects of shear stress on wound-healing process
Fluidic shear stresses were reported to affect cells in various aspects including attachment, morphology, alignment, living cycle, and damage29,30,31. In the molecular level, these stresses could alter gene expression and signaling cascades in cells such as retinal microvascular endothelial cells32, Schlemm’s canal cells33, and corneal endothelial cells34. Especially for endothelial cells, since they are in vivo exposed to continual flows, wound closure must occur under fluidic shear stresses. Wounds occurring in the endothelium are critical to a variety of cardiovascular disorders such as ischemic injury, vein bypass graft failure, coarctation the aorta, and mechanical trauma35.
The wound-healing speeds after 24 hr under different healing-stage flow rates are shown in Fig. 3. By changing the flow rate from 40 μL/hr to 400 μL/hr, the shear stresses varied from 0.087 mPa, 0.116 mPa, and 0.174 mPa to 0.872 mPa, 1.16 mPa, and 1.74 mPa in Area 1 (width = 6 mm), Area 2 (width = 4.5 mm), and Area 3 (width = 3 mm), respectively (see Table 1). As indicated in this figure, in Area 1, a 1.7-fold increase in the speed was noticed as the shear stress became ten times larger. With the same enhancement in the fluidic shear stress, the healing speeds exhibited 2.5- and 3.3-fold increases in Area 2 and Area 3, respectively. By plotting the wound-healing speeds against shear stresses in three different widths (see Fig. S1), the ranges of shear stresses in these three widths are very close. In the overlapping range (from 0.174 mPa to 0.872 mPa, marked between two dash lines), the healing speed in general increased with an enhanced shear stress.
Wound-healing speeds under different wound widths and flow rates. The number of experiments N = 9, and the error bars represent the standard errors of the mean (SEM) (see Data analysis in Methods). Statistical analysis was performed. ns: no statistically significant difference (p > 0.05); *p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001.
Conventionally, the wound-healing assays are conducted under static conditions (in petri dishes for example) without the mechanical cues of shear stresses. It was reported that the shear stress accelerated the wound-healing process in human umbilical vein endothelial cells (HUVECs) and human coronary artery endothelial cells (HCAECs)36. For example, HUVEC wounds exposed to shear stresses of 3 dyn/cm2, 12 dyn/cm2, and 20 dyn/cm2 closed to 21%, 39%, and 50% of original wounding areas after 6 hr, respectively, compared to only 59% in the static condition36. Gojova et al. found that bovine aortic endothelial cell wound closure under flow was critically sensitive to the shear stress level to which the cells were exposed 37. After 12 hr, low levels of shear stress (3 dyn/cm2) led to dramatically retarded wound closure rates relative to high shear stress levels (19 dyn/cm2)37. However, other studies revealed totally contrary results using human corneal epithelial cells (HCECs) as the model. It was reported that after 24 hr, the wound-healing rate at 12 dyne/cm2 decreased significantly compared with the static control38. A possible reason was that fluidic shear stress on the HCECs affected transforming growth factor-β signaling, which was associated with delayed wound healing38. Another study showed that the wound-healing process was impaired in both low (4 dyne/cm2) and high (8 dyne/cm2) shear stresses after 48 hr, compared to the no-shear condition39. HCECs exposed to shear stresses showed cytoskeletal rearrangement with more prominent, organized and elongated filamentous actin39, and this phenomenon has been shown to be related to the migration and proliferation of epithelial cells40,41. For fibroblasts, four hours of 20 dyn/cm2 shear stress significantly enhanced sub-confluent (30 ~ 50% confluence) fibroblast migration while it suppressed full-confluent fibroblast migratory activity42. However, four hours of 1 dyn/cm2 shear stress did not significantly alter either sub- or full-confluence fibroblast migration levels42. It was also found that fibroblasts exposed to fluid shear stress structurally rearranged pre-coated surface fibronectin43. Summarizing these results, we suggest that the effects of fluidic shear stress on the wound-healing process could be cell type-dependent, and the underlying mechanisms remain to be studied.
Effects of wound width on wound-healing process
The main advantage of the present microfluidic chip is that wounds of different widths could be created simultaneously to follow their healing processes. As indicated in the two columns with square marks in Fig. 3, under a shear stress of 0.174 mPa (see Table 1), the wound-healing speed decreased from 375.5 μm2/min to 155.8 μm2/min as the wound width was reduced from 1.45 mm to 0.59 mm (observation values). Similarly, when the shear stress was increased to 0.872 mPa (see Table 1), a decrease in the healing speed from 738.6 μm2/min to 479.7 μm2/min was observed with a reduced wound width (see the two columns with circle marks in Fig. 3). It seems that cells tended to migrate faster as the cell-free area was larger. However, in clinical trials investigating the influence of wound geometry on the measurement of wound healing rates, it was proposed that not the total area healed per unit time but the linear growth of wound edge per unit time should be calculated and compared44. This means that the percent area healed per unit time should be determined, and in the present study the initial widths of the wounds should be normalized. From this point of view, under a shear stress of 0.174 mPa, the normalized wound-healing speeds for two different widths were both close to 0.26 μm/min. But under a higher shear stress of 0.872 mPa, the normalized wound-healing speed for the 0.59-mm-width wound was about 1.6 times larger than that for the 1.45-mm-width one. Under a lower shear stress (0.174 mPa) the percent area healed per unit time was independent of the size of the wound. But at a higher shear stress (0.872 mPa) the percent area healed per unit time increased with a decreasing wound width. This trend is generally true as shown in Fig. S2 where the normalized wound-healing speeds are plotted against shear stresses in three different widths. In the overlapping range (from 0.174 mPa to 0.872 mPa), the normalized healing speed was independent of the size of the wound under a low shear stress (all close to 0.25 ~ 0.3 μm/min), but this speed increased with a decreasing wound width under a higher shear stress.
To the best of our knowledge, the effects of wound widths on the wound-healing process have only been rarely studied due to the difficulty in creating wounds of precise sizes and shapes. In clinical trials involving 39 patients with venous stasis ulcers, it was found that the linear healing per day was not affected by any geometric variable, including area, perimeter, length, width, and ratio of width to length44. Without presenting quantitative data, another study concluded that the wound-healing response of bovine corneal endothelial cells depended only on the presence of extracellular matrix (ECM) but not on the size and geometry of the wounds45. Using NIH/3T3 fibroblasts as the model, the effects of initial geometry on the wound-healing process were investigated46. As reported, the linear healing rates were similar in three different wound geometries including square, circle, and triangle46. All these findings, both in vivo and in vitro, were similar to what we have observed in the low shear stress case. Experimental results similar to those observed in the high shear stress case were not found; therefore, detailed investigations involving cell-cell communication and signaling under different shear stresses and wound sizes are required.
Effects of β-lapachone on wound-healing process
β-lapachone, a derivative of naturally occurring lapachol, was shown to exhibit various pharmacological properties including anti-bacterial, anti-inflammatory, anti-angiogenic, anti-metastatic, and anti-invasive effects47,48. For studying its effects on the wound-healing speed in a dose-dependent manner, it was flowed into the microfluidic chip at a healing-stage flow rate of 200 μL/hr. Surprisingly, as shown in Fig. 4, β-lapachone in general decreased the healing speed. In Area 1, the speeds were 623.8 μm2/min, 496.2 μm2/min, and 443.4 μm2/min under β-lapachone concentrations of 0 μM, 0.2 μM, and 0.5 μM, respectively. In Area 2, the speed decreased from 619.3 μm2/min without β-lapachone to 433.8 μm2/min and 390.5 μm2/min when concentrations of 0.2 μM and 0.5 μM were added, respectively. In Area 3, the speed decreased as 0.2 μM β-lapachone was added, but the value increased when the concentration was 0.5 μM.
Wound-healing speeds under different wound widths and β-lapachone concentrations. The number of experiments N = 9, and the error bars represent the standard errors of the mean (SEM) (see Data analysis in Methods). Statistical analysis was performed. ns: no statistically significant difference (p > 0.05); *p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001.
β-lapachone was shown to have wound healing-promoting activities both in vivo and in vitro49,50. Application of ointment with β-lapachone to punched wounds in normal and diabetic mice showed accelerated wound-healing processes50. Also, a low dose of β-lapachone (up to 1 μM) enhanced the proliferation in several cells, facilitated the migration of mouse 3T3 fibroblasts, and accelerated scratch-wound healing in vitro50. By using a microfluidic electrical-stimulated wound-healing chip, it was reported that β-lapachone alone (up to 2 μM) or low concentrations of β-lapachone (up to 0.5 μM) combined with electric fields (EFs) increased the wound-healing rate of NIH/3T3 cells, but overdose of β-lapachone (over 1 μM) in the presence of EFs decreased the rate instead probably due to excess ROS production51. From above-mentioned findings, the effects of β-lapachone on the wound-healing process were uncertain, which could depend on experimental conditions such as its concentration, the type of cells, the type of the assay (ex: scratch, barrier…), the micro-environment (ex: static or circulating), and the application of other stimuli (ex: EF…). Again, further studies are necessary.
Limitations of the present microfluidic chip
Currently wounds of three different widths were created, and this is not very high throughput. But it did increase compared with other microfluidics-based wound-healing assays (where only one wound width was created). The throughput of the present chip can be further increased by increasing the number of different widths in the microfluidic channel (see Fig. 5, currently 3, 4.5, and 6 mm). The inability to vary wound width and shear stress independently is another limitation of this device. To study the dependence of wound-healing process on the shear stress or on the wound width, additional experiments are required. Finally, the fact that one wound is downstream from another means that the cells at the beginning of the chip could be releasing molecules that affect the wound healing downstream. This a general issue in fluid-circulating, microfluidic-based wound-healing assays.
Conclusion
The wound-healing assay is a useful method for investigating collective cell migration under various chemical and physical stimuli. Traditional scratch- and barrier-based assays have drawbacks of unprecise wound sizes/shapes, damages to cells/substrate, and experiment-to-experiment variations. In this paper, we reported a microfluidics-based wound-healing assay to study the effects of shear stresses, wound widths, and β-lapachone on the wound-healing process. By using the trypsin flow-focusing technique, wounds of different widths were created. Experimental results indicated that the wound-healing speed increased with increasing shear stress and wound width, but under a 0.172 mPa shear stress the linear healing speeds were similar for two different widths. The addition of β-lapachone up to 0.5 μM did not accelerate wound healing. The present platform can serve as an alternative assay for further investigating the mechanisms of the wound-healing process in a non-contacting, fluid-circulating, and increased-throughput manner.
Methods
Chip design and fabrication
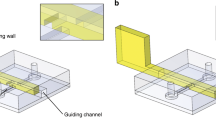
The design and fabrication of the microfluidic chip is shown in Fig. 5. It consisted of a central inlet for trypsin flow, a side inlet for medium flow, and an outlet. The cell culture area had three different widths, 6 mm (Area 1), 4.5 mm (Area 2), and 3 (Area 3) mm, for creating wounds of different sizes. The shrinking angle between two widths was set to be around 14° to prevent air bubble formation near the corners. The pattern was drawn in AutoCAD (Autodesk) and then loaded into a CO2 laser scriber (MS640D, Ming-Cheng Technics Corp.) to ablate desired patterns on polymethylmethacrylate (PMMA) substrates and double-sided tapes (8018, 3 M). As shown in Fig. 6, seven layers of PMMA sheets (thickness = 1 mm) and double-sided tapes (thickness = 260 μm and 60 μm) were bound together to form the integrated chip. The top PMMA layer had three small holes/adaptors serving as flow inlets and outlets. The bottom two double-sided tapes ((f) and (g) in Fig. 6) provided the fluidic channel for trypsin flow-focusing and cell culture, having a total thickness of 320 μm. Cytotoxicity of PMMA substrates and double-sided tapes on cells was examined, and no significant change in cell viability was observed52.
Simulation and calculation of laminar flow and shear stress
The numerical simulation of chemical concentration and shear stress inside the microfluidic chip was performed using the commercial software COMSOL Multiphysics (ver. 5.2a, COMSOL). The “Laminar Flow” and “Transport of Dilute Species” modules were used with the following parameters and settings: the boundary condition for inlets is “velocity”: normal inflow velocity; the boundary condition for outlet is “pressure”: 101,300 Pa with normal flow and suppress backflow; diffusion coefficient = 2.1 × 10−10 m2/s for trypsin in culture medium at room temperature; central inlet flow rate = 400 μL/min; side inlet flow rate = 800 μL/min; concentration = 0.0214 mole/m3 for trypsin solution in central inlet; concentration = 0 mole/m3 for medium in side inlet. For calculation in Table 1, the shear stress (τ) within the cell culture area is related to the volume flow rate (Q), fluidic viscosity (η), and dimensions of the channel (height h and width w) as \({\rm{\tau }}=6\frac{\eta Q}{{h}^{2}w}\)53.
Cell preparation
The procedures were detailed in a previous study54. The mouse embryonic fibroblast cell line NIH/3T3 was purchased from the Bioresource Collection and Research Center (BCRC), Taiwan. A complete cell culture medium composed of Dulbecco’s modified Eagle medium (DMEM, Gibco) and 10% calf serum (CS, Invitrogen) was used for cell culture. The cells were incubated in tissue culture polystyrene flasks (Corning) in 5% CO2 at 37 °C until 90% confluence before seeding into the microfluidic chip.
Experimental system and procedure
The procedures were detailed in a previous study55. The microfluidic chip was assembled inside the laminar flow hood and then UV-sterilized for 30 min. The central inlet was connected to a syringe driven by a syringe pump (NE-300, New Era). The experimental procedure is illustrated in Fig. 7. 1× phosphate-buffered saline (PBS) buffer was flowed into the chip (see Fig. 7a) and kept within the channel under 5% CO2 at 37 °C for 2 hr. The syringe was pushed gently by hands to remove bubbles, and PBS buffer was replaced with cell culture medium (see Fig. 7b). 3 × 106 cells suspended in 1 mL culture medium was loaded into the culture area by injecting the cell solution from this inlet (Fig. 7c). The microfluidic chip with seeded cells was first incubated for 2.5 hr. It was then mounted on top of a transparent indium tin oxide (ITO) glass (Part No. 300739, Merck) for maintaining the temperature at 37 ± 0.5 °C55. Fresh culture medium was continuously pumped into the chip at a flow rate of 40 μL/hr until a cell monolayer was formed (Fig. 7d).
After a cellular monolayer was formed, the syringe was disconnected from the central inlet. Two new syringes, one filled with culture medium and the other filled with 0.0214 mole/m3 (0.05% w/w) of trypsin (Sigma) solution, were connected to side and central inlets, respectively. Flow rates of 800 μL/min and 400 μL/min were set in side and central inlets, respectively. All liquids were continuously flowed into the chip for 10 min (Fig. 7e), and then the trypsin solution was replaced with culture medium for washing off dead cells. To observe the wound-healing process, the central inlet was continuously flowed in culture medium (Fig. 7f) with or without adding the chemical β-lapachone (0.2 μM or 0.5 μM in culture medium, Sigma). Different flow rates were set to obtain desired shear stresses. Time-lapse images were taken at 0 hr, 3 hr, 6 hr, 12 hr, and 24 hr after the wound was created.
Data analysis
The wound-healing process was recorded using a bright-field inverted microscope (ESPA, Hsinchu, Taiwan). Time-lapse images were taken at 0 hr, 3 hr, 6 hr, 12 hr, and 24 hr after the wound was created. Under a certain condition, three images were recorded for each area (at different locations) at one time point. They were further analyzed using ImageJ, which is a free Java-based software developed by the National Institutes of Health (NIH, Bethesda, MD). As shown in Fig. 8, this software was used to draw the boundaries of the wound at different time points. The area enclosed by these boundaries could be calculated. And the wound-healing speed is calculated as \(\frac{({R}_{i}-{R}_{f})}{T},\)where Ri and Rf are the initial an final areas of the wound, respectively, and T is the time after the wound was created. For each condition, three independent runs were performed. Therefore, there were total nine (three images times three runs) data to be analyzed to get the standard errors of the mean (SEM) as the error bars in Figs. 3 and 4.
References
Friedl, P. & Gilmour, D. Collective cell migration in morphogenesis, regeneration and cancer. Nature reviews. Molecular cell biology 10, 445–457, https://doi.org/10.1038/nrm2720 (2009).
Rorth, P. Collective cell migration. Annual review of cell and developmental biology 25, 407–429, https://doi.org/10.1146/annurev.cellbio.042308.113231 (2009).
Deisboeck, T. S. & Couzin, I. D. Collective behavior in cancer cell populations. Bioessays 31, 190–197, https://doi.org/10.1002/bies.200800084 (2009).
Chen, H. C. Boyden chamber assay. Methods Mol Biol 294, 15–22 doi:1-59259-860-9:015 [pii] (2005).
Li, Y. H. & Zhu, C. A modified Boyden chamber assay for tumor cell transendothelial migration in vitro. Clin Exp Metastasis 17, 423–429 (1999).
Somersalo, K., Salo, O. P., Bjorksten, F. & Mustakallio, K. K. A simplified Boyden chamber assay for neutrophil chemotaxis based on quantitation of myeloperoxidase. Anal Biochem 185, 238–242 (1990).
Jungi, T. W. Assay of chemotaxis by a reversible Boyden chamber eliminating cell detachment. Int Arch Allergy Appl Immunol 48, 341–352 (1975).
Hasan, J. et al. Quantitative angiogenesis assays in vivo–a review. Angiogenesis 7, 1–16, https://doi.org/10.1023/B:AGEN.0000037338.51851.d1, 5271092 [pii] (2004).
Todaro, G. J., Lazar, G. K. & Green, H. The initiation of cell division in a contact-inhibited mammalian cell line. J Cell Physiol 66, 325–333 (1965).
Friedl, P., Hegerfeldt, Y. & Tusch, M. Collective cell migration in morphogenesis and cancer. Int J Dev Biol 48, 441–449 (2004).
Yarrow, J. C., Perlman, Z. E., Westwood, N. J. & Mitchison, T. J. A high-throughput cell migration assay using scratch wound healing, a comparison of image-based readout methods. BMC Biotechnol 4, 21 (2004).
Cory, G. Scratch-wound assay. Methods Mol Biol 769, 25–30, https://doi.org/10.1007/978-1-61779-207-6_2 (2011).
Riahi, R., Yang, Y., Zhang, D. D. & Wong, P. K. Advances in wound-healing assays for probing collective cell migration. J Lab Autom 17, 59–65, https://doi.org/10.1177/2211068211426550, 17/1/59 [pii] (2012).
Kroening, S. & Goppelt-Struebe, M. Analysis of matrix-dependent cell migration with a barrier migration assay. Science signaling 3, pl1, https://doi.org/10.1126/scisignal.3126pl1 (2010).
Block, E. R., Matela, A. R., SundarRaj, N., Iszkula, E. R. & Klarlund, J. K. Wounding Induces Motility in Sheets of Corneal Epithelial Cells through Loss of Spatial Constraints. Journal of Biological Chemistry 279, 24307–24312, https://doi.org/10.1074/jbc.M401058200 (2004).
Nikolić, D. L., Boettiger, A. N., Bar-Sagi, D., Carbeck, J. D. & Shvartsman, S. Y. Role of boundary conditions in an experimental model of epithelial wound healing. American Journal of Physiology - Cell Physiology 291, C68–C75, https://doi.org/10.1152/ajpcell.00411.2005 (2006).
van Horssen, R., Galjart, N., Rens, J. A. P., Eggermont, A. M. M. & ten Hagen, T. L. M. Differential effects of matrix and growth factors on endothelial and fibroblast motility: Application of a modified cell migration assay. Journal of Cellular Biochemistry 99, 1536–1552, https://doi.org/10.1002/jcb.20994 (2006).
Koller, M. R. et al. High-throughput laser-mediated in situ cell purification with high purity and yield. Cytometry A 61, 153–161, https://doi.org/10.1002/cyto.a.20079 (2004).
Zordan, M. D., Mill, C. P., Riese, D. J. 2nd. & Leary, J. F. A high throughput, interactive imaging, bright-field wound healing assay. Cytometry A 79, 227–232, https://doi.org/10.1002/cyto.a.21029 (2011).
Keese, C. R., Wegener, J., Walker, S. R. & Giaever, I. Electrical wound-healing assay for cells in vitro. Proceedings of the National Academy of Sciences of the United States of America 101, 1554–1559, https://doi.org/10.1073/pnas.0307588100 (2004).
Wu, S. Y., Sun, Y. S., Cheng, K. C. & Lo, K. Y. A Wound-Healing Assay Based on Ultraviolet Light Ablation. SLAS technology 22, 36–43, https://doi.org/10.1177/2211068216646741 (2017).
Lo, K. Y., Zhu, Y., Tsai, H. F. & Sun, Y. S. Effects of shear stresses and antioxidant concentrations on the production of reactive oxygen species in lung cancer cells. Biomicrofluidics 7, 64108, https://doi.org/10.1063/1.4836675 (2013).
Nie, F. Q. et al. On-chip cell migration assay using microfluidic channels. Biomaterials 28, 4017–4022 (2007).
Wei, Y. et al. A Tubing-Free Microfluidic Wound Healing Assay Enabling the Quantification of Vascular Smooth Muscle Cell. Migration. Scientific reports 5, 14049, https://doi.org/10.1038/srep14049 (2015).
van der Meer, A. D., Vermeul, K., Poot, A. A., Feijen, J. & Vermes, I. A microfluidic wound-healing assay for quantifying endothelial cell migration. American journal of physiology. Heart and circulatory physiology 298, H719–725, https://doi.org/10.1152/ajpheart.00933.2009 (2010).
Felder, M. et al. Microfluidic wound-healing assay to assess the regenerative effect of HGF on wounded alveolar epithelium. Lab Chip 12, 640–646, https://doi.org/10.1039/c1lc20879a (2012).
Felder, M., Stucki, A. O., Stucki, J. D., Geiser, T. & Guenat, O. T. The potential of microfluidic lung epithelial wounding: towards in vivo-like alveolar microinjuries. Integrative biology: quantitative biosciences from nano to macro 6, 1132–1140, https://doi.org/10.1039/c4ib00149d (2014).
Wang, Y. C. et al. Wound-on-a-chip: High-throughput 3D wound healing assay with a novel SU-8 mesh chip. Sensor Actuat B-Chem 280, 86–93 (2019).
Chisti, Y. Hydrodynamic damage to animal cells. Critical reviews in biotechnology 21, 67–110, https://doi.org/10.1080/20013891081692 (2001).
Davies, P. F., Remuzzi, A., Gordon, E. J., Dewey, C. F. Jr. & Gimbrone, M. A. Jr. Turbulent fluid shear stress induces vascular endothelial cell turnover in vitro. Proceedings of the National Academy of Sciences of the United States of America 83, 2114–2117 (1986).
Zoro, B. J. H., Owen, S., Drake, R. A. L. & Hoare, M. The impact of process stress on suspended anchorage-dependent mammalian cells as an indicator of likely challenges for regenerative medicines. Biotechnol Bioeng 99, 468–474 (2008).
Ishibazawa, A. et al. Effects of shear stress on the gene expressions of endothelial nitric oxide synthase, endothelin-1, and thrombomodulin in human retinal microvascular endothelial cells. Investigative ophthalmology & visual science 52, 8496–8504, https://doi.org/10.1167/iovs.11-7686 (2011).
Ashpole, N. E., Overby, D. R., Ethier, C. R. & Stamer, W. D. Shear Stress-Triggered Nitric Oxide Release From Schlemm’s Canal Cells. Investigative ophthalmology & visual science 55, 8067–8076 (2014).
Yamamoto, Y., Uno, T., Joko, T., Shiraishi, A. & Ohashi, Y. Effect of anterior chamber depth on shear stress exerted on corneal endothelial cells by altered aqueous flow after laser iridotomy. Investigative ophthalmology & visual science 51, 1956–1964, https://doi.org/10.1167/iovs.09-4280 (2010).
Ramsay, M. M., Walker, L. N. & Bowyer, D. E. Narrow superficial injury to rabbit aortic endothelium. The healing process as observed by scanning electron microscopy. Atherosclerosis 43, 233–243 (1982).
Albuquerque, M. L., Waters, C. M., Savla, U., Schnaper, H. W. & Flozak, A. S. Shear stress enhances human endothelial cell wound closure in vitro. American journal of physiology. Heart and circulatory physiology 279, H293–302 (2000).
Gojova, A. & Barakat, A. I. Vascular endothelial wound closure under shear stress: role of membrane fluidity and flow-sensitive ion channels. Journal of applied physiology 98, 2355–2362, https://doi.org/10.1152/japplphysiol.01136.2004 (2005).
Utsunomiya, T. et al. Transforming Growth Factor-beta Signaling Cascade Induced by Mechanical Stimulation of Fluid Shear Stress in Cultured Corneal Epithelial Cells. Investigative ophthalmology & visual science 57, 6382–6388, https://doi.org/10.1167/iovs.16-20638 (2016).
Molladavoodi, S., Robichaud, M., Wulff, D. & Gorbet, M. Corneal epithelial cells exposed to shear stress show altered cytoskeleton and migratory behaviour. PloS one 12, e0178981, https://doi.org/10.1371/journal.pone.0178981 (2017).
Yin, J., Lu, J. & Yu, F. S. Role of small GTPase Rho in regulating corneal epithelial wound healing. Investigative ophthalmology & visual science 49, 900–909, https://doi.org/10.1167/iovs.07-1122 (2008).
Yin, J. & Yu, F. S. Rho kinases regulate corneal epithelial wound healing. American journal of physiology. Cell physiology 295, C378–387, https://doi.org/10.1152/ajpcell.90624.2007 (2008).
Garanich, J. S., Mathura, R. A., Shi, Z. D. & Tarbell, J. M. Effects of fluid shear stress on adventitial fibroblast migration: implications for flow-mediated mechanisms of arterialization and intimal hyperplasia. American journal of physiology. Heart and circulatory physiology 292, H3128–3135, https://doi.org/10.1152/ajpheart.00578.2006 (2007).
Steward, R. L. Jr., Cheng, C. M., Ye, J. D., Bellin, R. M. & LeDuc, P. R. Mechanical stretch and shear flow induced reorganization and recruitment of fibronectin in fibroblasts. Scientific reports 1, 147, https://doi.org/10.1038/srep00147 (2011).
Gorin, D. R., Cordts, P. R., LaMorte, W. W. & Manzoian, J. O. The influence of wound geometry on the measurement of wound healing rates in clinical trials. Journal of vascular surgery 23, 524–528, https://doi.org/10.1016/s0741-5214(96)80021-8 (1996).
Grasso, S., Hernandez, J. A. & Chifflet, S. Roles of wound geometry, wound size, and extracellular matrix in the healing response of bovine corneal endothelial cells in culture. American journal of physiology. Cell physiology 293, C1327–1337, https://doi.org/10.1152/ajpcell.00001.2007 (2007).
Jin, W., Lo, K. Y., Chou, S. E., Mccue, S. W. & Simpson, M. J. The role of initial geometry in experimental models of wound closing. Chem Eng Sci 179, 221–226 (2018).
Salas, C. et al. Trypanosoma cruzi: Activities of lapachol and alpha- and beta-lapachone derivatives against epimastigote and trypomastigote forms. Bioorgan Med Chem 16, 668–674 (2008).
Kung, H. N. et al. Involvement of NO/cGMP signaling in the apoptotic and anti-angiogenic effects of beta-lapachone on endothelial cells in vitro. J Cell Physiol 211, 522–532, https://doi.org/10.1002/jcp.20963 (2007).
Fu, S. C., Chau, Y. P., Lu, K. S. & Kung, H. N. beta-lapachone accelerates the recovery of burn-wound skin. Histology and histopathology 26, 905–914, https://doi.org/10.14670/HH-26.905 (2011).
Kung, H. N., Yang, M. J., Chang, C. F., Chau, Y. P. & Lu, K. S. In vitro and in vivo wound healing-promoting activities of beta-lapachone. American journal of physiology. Cell physiology 295, C931–943, https://doi.org/10.1152/ajpcell.00266.2008 (2008).
Sun, Y. S., Peng, S. W. & Cheng, J. Y. In vitro electrical-stimulated wound-healing chip for studying electric field-assisted wound-healing process. Biomicrofluidics 6, 34117, https://doi.org/10.1063/1.4750486 (2012).
Huang, C. W., Cheng, J. Y., Yen, M. H. & Young, T. H. Electrotaxis of lung cancer cells in a multiple-electric-field chip. Biosensors & bioelectronics 24, 3510–3516, https://doi.org/10.1016/j.bios.2009.05.001 (2009).
Varma, S. & Voldman, J. A cell-based sensor of fluid shear stress for microfluidics. Lab Chip 15, 1563–1573, https://doi.org/10.1039/c4lc01369g (2015).
Lin, J. Y., Lo, K. Y. & Sun, Y. S. Effects of Substrate-Coating Materials on the Wound-Healing Process. Materials 12, https://doi.org/10.3390/ma12172775 (2019).
Huang, C. H., Hou, H. S., Lo, K. Y., Cheng, J. Y. & Sun, Y. S. Use microfluidic chips to study the effects of ultraviolet lights on human fibroblasts. Microfluid Nanofluid 21, ARTN7910.1007/s10404-017-1922-7 (2017).
Acknowledgements
This work was financially supported by the Ministry of Science and Technology of Taiwan under Contract No. MOST 108-2112-M-030-002-MY2 and MOST 107-2221-E-030-001-MY2.
Author information
Authors and Affiliations
Contributions
J.-Y.L. designed the study and the microfluidic chip; carried out the experiments and data analysis. K.-Y.L. participated in the design of the chip and cell culture. Y.-S.S. participated in the design of the study, interpreted the data, and drafted the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lin, JY., Lo, KY. & Sun, YS. A microfluidics-based wound-healing assay for studying the effects of shear stresses, wound widths, and chemicals on the wound-healing process. Sci Rep 9, 20016 (2019). https://doi.org/10.1038/s41598-019-56753-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-56753-9
This article is cited by
-
Putative mechanobiological impact of surface texture on cell activity around soft-tissue implants undergoing micromotion
Biomechanics and Modeling in Mechanobiology (2022)
-
An on-chip wound healing assay fabricated by xurography for evaluation of dermal fibroblast cell migration and wound closure
Scientific Reports (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.