Abstract
This study aimed to compare the plasma levels of angiotensin-I converting enzyme (ACE), Angiotensin II (AngII), kallikrein (KLK1) and interleukin-6 (IL-6) in ST segment elevation myocardial infarction (STEMI) patients with different ACE Insertion/deletion (I/D) polymorphisms in a Chinese population. The ACE genotypes were determined in the 199 STEMI patients and 216 control subjects. STEMI patients were divided into three groups based on the ACE genotypes. Single polymerase chain reaction (PCR) was performed to characterize ACE I/D polymorphisms. Plasma levels of ACE, AngII, KLK1 and IL-6 were measured by enzyme-linked immunosorbent assay (ELISA). We found that the DD or ID genotype was significantly independently associated with high ACE (OR = 4.697; 95% CI = 1.927–11.339), KLK1 (3.339; 1.383–8.063) and IL-6 levels (OR = 2.10; 1.025–4.327) in STEMI patients. However, there was no statistical significance between the ACE I/D polymorphism and AngII plasma levels whether in univariate or multivariate logistic regression. Additionally, we detected a significantly positive correlation between plasma KLK1 levels and IL-6 levels in STEMI patients (r = 0.584, P < 0.001). The study showed high levels of ACE, KLK1 and IL-6 were detected when the D allele was present, but AngII plasma levels was not influenced by the ACE I/D polymorphism.
Similar content being viewed by others
Introduction
Acute myocardial infarction (AMI) is a major cause of morbidity and mortality worldwide, and it has been estimated that approximately 50% to 60% of the major risk factors for CAD and AMI are determined by heritability1. The ST segment elevation myocardial infarction (STEMI) is one of the most severe types of AMI. It primarily occurs due to the rupture of atherosclerotic plaques. A human angiotensin I-converting enzyme (ACE) gene insertion/deletion (I/D) polymorphism, due to I/D of a 287-base pair element in intron 16 of this gene, is associated with the development of AMI by modifying ACE activity and contributing to enhanced plaque vulnerability, ulceration and thrombosis2,3. Our recent case-control study has also demonstrated that the ACE DD genotype is an independent risk factor for STEMI4.
ACE, an important common regulator of the Kallikrein-Kinin system (KKs) and the rein-angiotensin system (RAs), was revealed to convert angiotensin (AngI) into angiotensin II (AngII) and inactivate bradykinin (BK). ACE plays an important role in the physiology of blood vessels and inflammatory processes and has been widely studied to observe its correlation with various cardiovascular diseases3. There is substantial evidence that the ACE I/D polymorphism determines ACE, which has been demonstrated by the mean plasma ACE concentrations in individuals with the DD genotype being approximately twice that in II individuals, with ID individuals having intermediate concentrations5.
Among the different roles of AngII, this protein enhances the levels of cytokines, such as interleukin–6(IL-6) and IL-8, thus playing a proinflammatory role6. Kallikrein (KLK1), which is responsible for the generation of BK, stimulated the proinflammatory cytokines IL-6 and IL-8, as another novel action of its contribution to neovascularization7,8. Both inflammation and neovascularization have been reported to enhance plaque vulnerability9. Animal models and clinical studies demonstrated that ACE, AngII, KLK1 and IL-6 were highly expressed in unstable plaques and were significantly increased in ACS (acute coronary artery syndrome) patients10,11. Additionally, previous studies have shown interactions between RAs, KKs and inflammation12,13. In this context, we hypothesized that changes in ACE activity through the ACE I/D polymorphism may result in an increase in vasoactive members associated with the RAs, KKs and inflammation, such as AngII, KLK1 and IL-6. Changes in AngII, KLK1 and IL-6 levels could possibly depend on the range of ACE activity differences between the ACE I/D genotypes. To date, the association of ACE genetic polymorphisms with changes in ACE, AngII, KLK1 and IL-6 plasma levels has not been investigated in patients with STEMI.
The aim of the present study was to determine the possible interplay between the ACE I/D polymorphism and the important vasoactive substance of the RAs ACE, AngII, the important regulator of the KKs KLK1, and the inflammatory mediator IL-6 in patients with STEMI in the Chinese population.
Methods
Subjects
All procedures in studies involving human participants were performed in accordance with the ethical standards of the institutional or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. This study was approved by the Ethics Committee of the Central Hospital of Zibo (approval no. ZBH05485). Informed consent for participation was obtained from all patients and their parents in an appropriate manner. A total of 260 STEMI patients admitted to the Central Hospital of Zibo from January 2014 to January 2017 and diagnosed with STEMI undergoing coronary angiography (CAG) were enrolled. All patients met the inclusion criteria, including an electrocardiography showing STEMI, detection of an increase and or decrease in troponin I with at least 1 value more than the 99th percentile upper reference limit, and at least 1 of the following: myocardial ischemic symptoms lasting longer than 30 minutes; electrocardiogram changes indicative of new ischemia (ST-segment elevation >2 mm in 2 contiguous ECG leads within 24 hours of the onset of symptoms). In addition, the CAG results for the subjects showed the presence of an acute occlusion in at least one major coronary vessel or one of its major branches. Control subjects (N = 216) had no clinical evidence of CAD, including (1) negative CAG examination results, (2) no abnormal Q wave or ST-T changes found in the resting electrocardiogram and no abnormalities found on cardiac ultrasound examinations, and (3) a negative Master exercise test. The exclusion criteria for the STEMI patients and control group were as follows: severe renal failure (serum creatinine >180 mmol/l), severe hepatic disease, peripheral angiopathy, malignant cancer and serious infections. Patients treated with ACEIs were also excluded because ACEI medication (>1 month) may affect the levels of ACE, AngII, KLK1 and IL-614,15. Finally, a total of 199 patients (51 female and 148 male) with STEMI were included in this study, and 61 patients were excluded. The control subjects constituted 96 female and 120 male.
Data collection and blood sampling
All data collection was performed with quality control. Anthropometric data on age, sex, body weight, BMI [weight (m2)/height (kg)], SBP, DBP, a smoking habit (one pack year: ≥20 cigarettes per day for more than 1 year), and comorbid conditions. The diagnosis of hypertension and diabetes mellitus was performed according to World Health Organization criteria A smoking habit was defined as a daily intake of >10 cigarettes continuing for more than 1 year. The other criteria are consistent with a previous study4. The fasting blood samples tested for routine blood, lipid profiles and coagulation tests were routinely performed in the hospital laboratory.
Fifteen milliliters of blood were taken from the arterial sheath access of all subjects during CAG prior to the injection of contrast. Blood samples were collected in tubes containing ethylene diamine tetraacetic acid (EDTA) and aprotinin and were separated by centrifugation at 4 °C for 10 minutes at 3000 rpm within one hour after collection. Then, the plasma used to measure ACE, AngII, KLK1, and IL-6 levels and leukocytes used for DNA extraction from arterial blood (during CAG). These were separated and stored at −80 °C until assayed.
Coronary angiography (CAG)
The standard Judkins technique was implemented for coronary angiography (CAG). CAG was performed on the basis of standards of clinical practice using contrast agents (iodine amine (370)). Then, we examined the left main trunk (LM), the left anterior descending artery (LAD), the left circumflex artery (LCX), and the right coronary artery (RCA) and evaluated the stenosis of coronary arteries. Two independent and experienced interventional cardiologists blinded to the clinical information for the subjects performed the angiographic assessment.
Measurements of ACE, AngII, KLK1 and IL-6
Plasma levels of ACE, AngII, KLK1 and IL-6 were measured by enzyme-linked immunosorbent assay (ELISA) using commercially available kits (Lengton Bioscience Co., Ltd., Shanghai; LOT: 201500506MY), which were based on a competitive enzyme immunoassay technique.
Human ACE, AngII, KLK1 and IL-6 levels in plasma were measured in strict accordance with the manufacturer’s instructions, as described previously4. Briefly, polyclonal antibodies specific for these three proteins were precoated onto 96-well plates and incubated for 24 hours at 4 °C. The plasma samples and horseradish peroxidase (HRP) antigen were added to each well. Standards, samples and avidin conjugated to horseradish peroxidase (HRP) were then added to the appropriate microplate wells. After rocking, the plates were covered with sealing film and incubated at 37 °C for 1 h. The plates were repeatedly washed 3 times with 1% BSA-PBS. Then, TMB substrate solution was added to each well and incubated at 37 °C for 10 min without light. After 10 min, the enzyme substrate reaction was terminated by the addition of a sulfuric acid solution. Subsequently, the optical density (OD) was measured with a Bio-Rad ELISA plate reader (Infinite M200Pro, TECAN) at a wavelength of 450 nm. The plasma levels of ACE, AngII, KLK1 and IL-6 in the samples were obtained by comparison with a calibrated standard curve.
Detection of the ACE polymorphism
Genomic DNA was extracted from arterial blood (during CAG) using a human genome extraction kit (purchased from TIANGEN Biotechnology Co., LTD). The DNA concentration was measured at 260 nm, and quality controls were conducted. ACE I/D polymorphisms were determined by polymerase chain reaction (PCR). The primers had the following sequences: 5′-CTG GAG ACC ACT CCC ATC CTT CT-3′ (forward primer) and 5′-GAT GTG GCC ATC ACA TTC GTC AGA T-3′ (reverse primer). To eliminate the potential that the D allele of the ACE gene was overestimated due to failure to amplify the I allele, all DD genotype samples were confirmed by another pair of insertion-specific primers: forward, 5′-TCG GAC CAC AGC GCC CGC CAC TAC-3′; and reverse, 5′-TCG CCA GCC CTC CCA TGC CCA TAA-3′. The DNA was amplified for 30 cycles, including denaturation at 94 °C for 1 minute, annealing at 55 °C for 30 s and extension at 72 °C for 10 min. Then, 10 μl of the amplified product was examined by 1.5% agarose gel electrophoresis. PCR amplification produced fragments of 490 bp, indicating the I allele, and 190 bp, indicating the D allele, thus yielding genotypes II, ID and DD, respectively. An additional 335 bp product, a consequence of PCR using a pair of insertion-specific primers, also indicted the I allele.
Statistical methods
The data were analyzed by SPSS version 19.0 (SPSS Co., Chicago, IL, USA) for Windows. Hardy-Weinberg equilibrium (HWE) for the distributions of ACE genotypes was performed by the chi square (χ2) test. The odds ratios (ORs) and corresponding 95% confidence intervals (CIs) for assessing the effect of the ACE I/D genotype distribution and allele frequencies on the levels of ACE, AngII, KLK1, and IL-6 in STEMI patients were calculated by logistic regression analysis. The Spearman rank test was used to define the correlation between them. For all the analyses, statistical significance was defined as P < 0.05.
Results
General characteristics and genotype distribution
As shown in Table 1, comparisons of the distributions of demographic general clinical and biochemical characteristics, genotype distribution and the estimated OR for each risk factor are listed. In the univariate logistic regression model, the ACE DD genotype, older age, a history of smoking habits and the presence of diabetes were found to be high risk factors for STEMI. The other variables including hypertension, body mass index (BMI), gender, white blood count (WBC), high-density lipoprotein (HDL) and plasma fibrinogen (FIB) were not significantly different between the two groups.
After adjusting for the other risk factors (age, BMI, Sex, hypertension, diabetes mellitus and smoking habits) the DD genotype was still significantly associated with STEMI, conferring a 5-fold higher risk (OR = 5.585; 95% CI: 2.459–12.685). A history of smoking habits was the only other independent risk factor in multivariate logistic regression, which was in accordance with other studies16.
Association of the ACE I/D Polymorphism with the plasma Levels of ACE, KLK1, AngII, IL-6 in STEMI patients
To further evaluate the etiologic effects of ACE I/D polymorphisms in STEMI, we evaluated the possible influence of ACE I/D polymorphisms on STEMI-relevant traditional risk factors, plasma ACE, AngII, KLK1, and IL-6 levels. For further statistical analysis, the above plasma indicators were divided into high vs. low levels according to the mean of the STEMI patients. As shown in Tables 2 and 3, no obvious association was observed between these clinical and biochemical characteristics (age, BMI, Gender, hypertension, diabetes, WBC, HDL-c and FIB) and the ACE I/D polymorphism. However, the ACE DD and ID genotypes were found to be statistically significant associated in STEMI patients who had smoking habits (OR: 2.635, 95% CI 1.205–5.765), high plasma ACE levels (5.222; 2.290–11.907), high KLK1 (2.847; 1.277–6.545) and high IL-6 levels (2.100; 1.025–4.327) in STEMI patients.
After adjusting for other risk factors, the DD genotype was still significantly independently associated with smoking habits (OR = 1.123, 95% CI: 1.041–1.212), high ACE levels (4.697; 1.927–11.339) and high KLK1 levels (3.339; 1.383–8.063) (Table 4). Whereas, there was no statistical significance between the ACE I/D polymorphism and the AngII plasma levels whether in univariate or multivariate logistic regression.
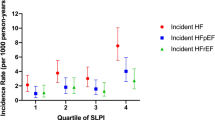
The Spearman correlation coefficient revealed a significant positive correlation between ACE and KLK1 (r = 0.430, P = 0.038), KLK1 and AngII (r = 0.256, P < 0.001), KLK1 and IL-6 (r = 0.584, P < 0.001) in patients with STEMI (Fig. 1).
Discussion
The ACE DD genotype is a great risk factor for AMI and has been extensively studied. There is substantial evidence showing that the ACE DD genotype may play a key role in the onset of AMI by altering plasma ACE levels or activity and increasing the instability of atherosclerotic plaques2,3. One study found that both Caucasian and Asian individuals as DD carriers conferred 1.21- and 2.47-fold risks of AMI, respectively, compared with ID or II genotype carriers, and Asian individuals as DD carriers appeared to be more prone to AMI than did Caucasian individuals3. This result was also similar to most studies in different populations or study cohorts17,18. One recent case-control study also demonstrated that the ACE DD genotype was an independent risk factor for AMI in a Chinese population4. A similar result was also found in the present study. After controlling for other risk factors, the DD genotype was still significantly associated with STEMI, conferring a 5-fold higher risk.
There was a significant increased risk for STEMI among individuals with DD genotypes and smoking habits. A previous study noted that The presence of the D allele also increased the risk of CAD associated with the presence of smoking habits19. Indeed, smoking and the D allele increase ACE expression, impair protective antioxidant mechanisms, causing endothelial dysfunction by accelerating superoxide anion formation and degradation of nitric oxide, leading to the onset of STEMI19,20,21. Our results showed that both the DD genotype and smoking habits were associated with an increased risk of STEMI in patients. Our study demonstrated that there may be an association between the DD or ID genotype and smoking in patients with STEMI (OR = 1.123, 95% CI: 1.041–1.212). As Kiyoshi Hibi et al. suggested that ACE gene polymorphism adds risk for the severity of coronary atherosclerosis in smokers22.
Previous studies have shown that subjects with the D polymorphism had a higher level of plasma ACE protein than did those with the I polymorphism. Intermediate levels were observed in heterozygotes (ID genotype)5. Similar results were also found in a case-control study suggesting that subjects with the DD genotype had a 2.91-fold higher risk of STEMI than those with the II genotype23. Similar results were also widely indicated by other studies24. The effects of DD genotype of the ACE I/D polymorphism on plasma ACE levels and activity may be an important mechanism for the association of the ACE I/D polymorphism with the most urgent STEMI events3. Our results suggest that STEMI patients with the ACE DD genotype showed the highest mean ACE plasma level, while patients with the ACE II genotype had the lowest mean plasma ACE level, in accordance with previous reports5.
Our present study revealed that the KLK1 plasma levels were higher in patients with STEMI carrying the D allele (ID/DD) compared to those lacking this allele (II). Although we have not obtained the exact mechanisms beyond this correlation, as we pointed out above and previous studies suggest that individuals with the D allele have significantly higher ACE plasma levels than do those with the I allele, which was validated by a substantial investigation2. The 47% phenotypic variance in ACE plasma levels was clarified by the ACE I/D gene polymorphism, and ACE plasma levels were 85% higher in DD subjects compared to II subjects, and ID subjects showed intermediate levels5. In addition, ACE is common to both RAS and KKS but plays different roles: it processes AngI to AngII and is the main BK-inactivating peptide25. KLK1 is the only member of the tissue KKS family that is responsible for the generation of BK. Subsequently, BK promotes vasodilation by the enhanced formation of nitric oxide (NO)26. H. Buikema et al. demonstrated that the arteries from DD patients with a smaller capacity for NO release in response to stimulation27. Furthermore, Kakoki et al. proposed that the D allele was associated with rapid BK degradation as a result of higher levels and activity of ACE28. It is tempting to speculate that the high KLK1 levels observed in patients with the D allele may play an important compensatory role in their increased BK degradation.
Urata et al. first showed in vitro two pathways for the generation of AngII in human cardiac ventricles. A serine proteinase-dependent enzyme, which was identified as a new member of the chymase family, was responsible for approximately 80% of total AngII, while ACE-dependent AngII generation only accounted for <11% of the AngII29. Despite the association of the D allele with increased levels of ACE, previous studies by varying degrees of ACEIs and computer simulations of the influence of genetically changing the levels of ACE revealed that such modest changes in ACE levels alter the levels of the substrate BK but had little effect on the active peptide AngII30. Furthermore, cellular studies stated that ACE has an even stronger affinity for BK than for AngI31. In the literature, we agree with the theory of Smithies that the decrease in the level of the active ACE substrate BK probably mediates the adverse effects of the D polymorphism but not the alteration in the level of AngII32. In the present study, we did not observe a difference in the level of active AngII regarding the ACE I/D polymorphism.
STEMI primarily occurs due to rupture of atherosclerotic plaques. In this process, inflammation is thought to play a key role along with several other risk factors33. Previous investigations have shown that a high level of IL-6 is an independent predictor of adverse events in patients with ACS34. Our data showed that the presence of the D allele is related to higher IL-6, with 18.6 ng/ml in DD and 18.0 ng/ml in ID versus 14.7 ng/ml with the II genotype15. As mentioned above, the results indicated that ACE DD has been reported to increase plasma ACE in accordance with previous studies. Increased ACE levels by the ACE I/D polymorphism may accelerate the expression of inflammatory cytokines, such as IL-6 and IL-815,35.
In this study, we detected a significant positive correlation between plasma KLK1 levels and IL-6 levels in STEMI patients (r = 0.584, P < 0.001). Previous studies have demonstrated that most of the biological functions of KLK1 are mediated by kinin receptor signaling, which can upregulate the expression of pro-inflammatory cytokines such as IL-6 and IL-826. A recent study suggests that KLK1 may also activate protease-activated receptors (PARs), leading to intracellular Ca2+ mobilization and phosphorylation of MAPK signaling and subsequent cytokine production (IL-6, CCL-2, and IL-8)36. Additionally, both inflammation and angiogenesis correlate with vulnerable plaques37. KLK1 is highly expressed in unstable plaques, implying that KLK1 contributes to angiogenesis and is involved in inflammatory activation, leading to unstable plaque formation10. Clinical studies have shown that both elevated plasma IL-6 and KLK1 levels may increase plaque vulnerability and are associated with the severity of STEMI10,34. These reports provide evidence that supports the present findings.
Controversy surrounds the effect of the ACE I/D polymorphism on CAD and AMI38. Most subsequent studies have indicated no significant influence of this polymorphism on the extent of CAD but mainly on the onset of AMI, especially in STEMI. These data imply a possible mechanism involving plaque vulnerability, ulceration and thrombosis3. In this context, it is reasonable to hypothesize that alterations in ACE activity through the ACE I/D polymorphism may result in an increase in the expression levels of IL-6 and KLK1, which increases plaque vulnerability.
Study limitations
First, the results here are preliminary due to the limitation of the small number of patients. Second, it would be of interest in future animal and clinical studies to better confirm the mechanism of the association between the ACE I/D gene polymorphism and the level of ACE, IL-6, and KLK1, although we hypothesized that alterations in ACE activity through the ACE I/D polymorphism may result in an increase in the expression levels of these factors.
Conclusion
To our knowledge, this study is the first to show that high levels of ACE, KLK1 and IL-6 are detected when D allele is present, but AngII was not influenced by ACE I/D polymorphism.
Data availability
The dataset analyzed during the current study is available from the corresponding authors on reasonable request.
References
Dai, X., Wiernek, S., Evans, J. P. & Runge, M. S. Genetics of coronary artery disease and myocardial infarction. World journal of cardiology 8, 1–23, https://doi.org/10.4330/wjc.v8.i1.1 (2016).
Cambien, F. et al. Plasma level and gene polymorphism of angiotensin-converting enzyme in relation to myocardial infarction. Circulation 90, 669–676 (1994).
Chen, Y., Dong, S., He, M., Qi, T. & Zhu, W. Angiotensin-converting enzyme insertion/deletion polymorphism and risk of myocardial infarction in an updated meta-analysis based on 34993 participants. Gene 522, 196–205, https://doi.org/10.1016/j.gene.2013.03.076 (2013).
Dai, S. H. et al. Association of serum levels of AngII, KLK1, and ACE/KLK1 polymorphisms with acute myocardial infarction induced by coronary artery stenosis. Journal of the renin-angiotensin-aldosterone system: JRAAS 17, 1470320316655037, https://doi.org/10.1177/1470320316655037 (2016).
Rigat, B. et al. An insertion/deletion polymorphism in the angiotensin I-converting enzyme gene accounting for half the variance of serum enzyme levels. The Journal of clinical investigation 86, 1343–1346, https://doi.org/10.1172/JCI114844 (1990).
Takahashi, T. et al. Participation of reactive oxygen intermediates in the angiotensin II-activated signaling pathways in vascular smooth muscle cells. Annals of the New York Academy of Sciences 902, 283–287 (2000).
Shao, X. et al. Inducible expression of kallikrein in renal tubular cells protects mice against spontaneous lupus nephritis. Arthritis and rheumatism 65, 780–791, https://doi.org/10.1002/art.37798 (2013).
Fu, S. S. et al. Kallikrein gene-modified EPCs induce angiogenesis in rats with ischemic hindlimb and correlate with integrin alphavbeta3 expression. PloS one 8, e73035, https://doi.org/10.1371/journal.pone.0073035 (2013).
de Vries, M. R. & Quax, P. H. Plaque angiogenesis and its relation to inflammation and atherosclerotic plaque destabilization. Current opinion in lipidology 27, 499–506, https://doi.org/10.1097/MOL.0000000000000339 (2016).
Yao, Y. Y. et al. Tissue kallikrein is related to the severity of coronary artery disease. Clinica chimica acta; international journal of clinical chemistry 423, 90–98, https://doi.org/10.1016/j.cca.2013.04.017 (2013).
Schieffer, B. et al. Expression of angiotensin II and interleukin 6 in human coronary atherosclerotic plaques: potential implications for inflammation and plaque instability. Circulation 101, 1372–1378 (2000).
Su, J. B. Different cross-talk sites between the renin-angiotensin and the kallikrein-kinin systems. Journal of the renin-angiotensin-aldosterone system: JRAAS 15, 319–328, https://doi.org/10.1177/1470320312474854 (2014).
Tang, S. C. et al. Bradykinin and high glucose promote renal tubular inflammation. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association - European Renal Association 25, 698–710, https://doi.org/10.1093/ndt/gfp599 (2010).
Fraga-Silva, R. A. et al. The angiotensin-converting enzyme 2/angiotensin-(1-7)/Mas receptor axis: a potential target for treating thrombotic diseases. Thrombosis and haemostasis 108, 1089–1096, https://doi.org/10.1160/TH12-06-0396 (2012).
Kortekaas, K. E. et al. ACE inhibitors potently reduce vascular inflammation, results of an open proof-of-concept study in the abdominal aortic aneurysm. PloS one 9, e111952, https://doi.org/10.1371/journal.pone.0111952 (2014).
The fundamental importance of smoking cessation in those with premature ST-segment elevation acute myocardial infarction.
Vaisi-Raygani, A. et al. The angiotensin converting enzyme D allele is an independent risk factor for early onset coronary artery disease. Clinical biochemistry 43, 1189–1194, https://doi.org/10.1016/j.clinbiochem.2010.07.010 (2010).
Parenica, J. et al. ACE gene insertion/deletion polymorphism has a mild influence on the acute development of left ventricular dysfunction in patients with ST elevation myocardial infarction treated with primary PCI. BMC cardiovascular disorders 10, 60, https://doi.org/10.1186/1471-2261-10-60 (2010).
Niemiec, P., Zak, I. & Wita, K. Modification of the coronary artery disease risk associated with the presence of traditional risk factors by insertion/deletion polymorphism of the ACE gene. Genetic testing 11, 353–359, https://doi.org/10.1089/gte.2007.0005 (2007).
Drexler, H. & Hornig, B. Endothelial dysfunction in human disease. Journal of molecular and cellular cardiology 31, 51–60, https://doi.org/10.1006/jmcc.1998.0843 (1999).
Zhang, S., Day, I. & Ye, S. Nicotine induced changes in gene expression by human coronary artery endothelial cells. Atherosclerosis 154, 277–283, https://doi.org/10.1016/s0021-9150(00)00475-5 (2001).
Hibi, K. et al. Angiotensin-converting enzyme gene polymorphism adds risk for the severity of coronary atherosclerosis in smokers. Hypertension 30, 574–579, https://doi.org/10.1161/01.hyp.30.3.574 (1997).
Pulla Reddy, B. et al. Angiotensin-converting enzyme gene variant and its levels: risk factors for myocardial infarction in a South Indian population. Singapore medical journal 51, 576–581 (2010).
Mehri, S. et al. Angiotensin-converting enzyme insertion/deletion gene polymorphism in a Tunisian healthy and acute myocardial infarction population. Genetic testing and molecular biomarkers 14, 85–91, https://doi.org/10.1089/gtmb.2009.0105 (2010).
Rhaleb, N. E., Yang, X. P. & Carretero, O. A. The kallikrein-kinin system as a regulator of cardiovascular and renal function. Comprehensive Physiology 1, 971–993, https://doi.org/10.1002/cphy.c100053 (2011).
Tang, S. C., Leung, J. C. & Lai, K. N. The kallikrein-kinin system. Contributions to nephrology 170, 145–155, https://doi.org/10.1159/000325650 (2011).
Buikema, H. et al. The deletion polymorphism of the angiotensin-converting enzyme gene is related to phenotypic differences in human arteries. European heart journal 17, 787–794 (1996).
Kakoki, M. & Smithies, O. The kallikrein-kinin system in health and in diseases of the kidney. Kidney international 75, 1019–1030, https://doi.org/10.1038/ki.2008.647 (2009).
Urata, H., Healy, B., Stewart, R. W., Bumpus, F. M. & Husain, A. Angiotensin II-forming pathways in normal and failing human hearts. Circulation research 66, 883–890 (1990).
Campbell, D. J., Kladis, A. & Duncan, A. M. Effects of converting enzyme inhibitors on angiotensin and bradykinin peptides. Hypertension 23, 439–449 (1994).
Sasaguri, M. et al. Purification and characterization of a kinin- and angiotensin II-forming enzyme in the dog heart. Journal of hypertension 15, 675–682 (1997).
Smithies, O., Kim, H. S., Takahashi, N. & Edgell, M. H. Importance of quantitative genetic variations in the etiology of hypertension. Kidney Int 58, 2265–2280, https://doi.org/10.1046/j.1523-1755.2000.00411.x (2000).
Libby, P., Tabas, I., Fredman, G. & Fisher, E. A. Inflammation and its resolution as determinants of acute coronary syndromes. Circulation research 114, 1867–1879, https://doi.org/10.1161/CIRCRESAHA.114.302699 (2014).
Garcia-Salas, J. M. et al. Interleukin-6 as a predictor of cardiovascular events in troponin-negative non-ST elevation acute coronary syndrome patients. International journal of clinical practice 68, 294–303, https://doi.org/10.1111/ijcp.12245 (2014).
Apavaloaie, M. C. et al. Inflammatory and Genetic Markers (APO B100 and Angiotensin-Converting Enzyme Gene) in the Coronary Artery Disease. Revista medico-chirurgicala a Societatii de Medici si Naturalisti din Iasi 120, 530–536 (2016).
Yiu, W. H. et al. Tissue kallikrein mediates pro-inflammatory pathways and activation of protease-activated receptor-4 in proximal tubular epithelial cells. PloS one 9, e88894, https://doi.org/10.1371/journal.pone.0088894 (2014).
Davies, M. J. Stability and instability: two faces of coronary atherosclerosis. The Paul Dudley White Lecture 1995. Circulation 94, 2013-2020 (1996).
Zintzaras, E., Raman, G., Kitsios, G. & Lau, J. Angiotensin-converting enzyme insertion/deletion gene polymorphic variant as a marker of coronary artery disease: a meta-analysis. Archives of internal medicine 168, 1077–1089, https://doi.org/10.1001/archinte.168.10.1077 (2008).
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: S.H.D., L.Y.G., H.Y.L., M.D. and D.Q.L. Performed the experiments: S.H.D., L.Y.G., H.Y.L. and N.L. Analyzed the data: S.H.D., L.Y.G., H.Y.L., M.D., Z.L. and D.Q.L. Contributed reagents/materials/analysis tools: S.H.D., L.Y.G., H.Y.L., M.D., N.L., Z.L. and D.Q.L. Wrote the paper: S.H.D., L.Y.G., H.Y.L., M.D. and N.L.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dai, S., Ding, M., Liang, N. et al. Associations of ACE I/D polymorphism with the levels of ACE, kallikrein, angiotensin II and interleukin-6 in STEMI patients. Sci Rep 9, 19719 (2019). https://doi.org/10.1038/s41598-019-56263-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-56263-8
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.