Abstract
Although echocardiograms are often performed when peritoneal dialysis is started, associations between commonly reported findings and prospective changes in renal function remain understudied. Ninety-nine of 101 patients in the Trio Trial had transthoracic echocardiograms within 6 months of dialysis initiation, and measurements of residual renal function every six weeks for up to two years. Generalized mixed modelling linear regression in STATA was used to examine associations between left atrial size, left ventricular hypertrophy, left ventricular ejection fraction, right ventricular systolic pressure, and left valvular calcification with subsequent slopes in renal function. After echocardiography (performed a median of 16 days following peritoneal dialysis initiation) right ventricular systolic pressure was associated with faster, while declining left ventricular ejection fraction and valvular calcification were associated with slower declines in residual renal function. Future studies could be conducted to confirm these findings, and identify pathophysiological mechanisms.
Similar content being viewed by others
Introduction
Clinical guidelines and practice have led to widespread use of echocardiography in patients new to dialysis1. This frequently reveals abnormalities such as left atrial enlargement, left ventricular hypertrophy, impaired left ventricular function, elevated right ventricular systolic pressures, and valvular calcification that are prospectively tied to worsened survival and cardiovascular outcomes1,2,3,4,5. Links between echocardiographic findings and subsequent changes in residual renal function (RRF), particularly in patients receiving peritoneal dialysis (PD), are less clear. Most studies examining echocardiogram findings in relation to renal function were restricted to patients not yet on dialysis or to those on hemodialysis6. Those that included patients on PD were limited by cross-sectional or retrospective designs, imprecision of RRF measurements, short durations of follow-up, or examination of only some of the commonly reported echocardiographic parameters7,8.
Renal function remains very important even after PD has been initiated, and efforts to better understand factors that affect or predict its decline are warranted. Currently accepted favorable prognostic factors include use of biocompatible PD solutions as well as use of inhibitors of the renin angiotensin aldosterone system9. Given that cardiac and renal disease commonly overlap, early markers (as assessed by echocardiography) of cardiac disease might also predict progression of kidney disease. The Trio Trial was a multi-center trial in which incident patients in Toronto and Hong Kong were randomized to receive biocompatible or standard PD solutions for up to two years9. The primary outcome was slope of RRF, and all patients received transthoracic echocardiography after PD initiation according to the published study protocol. In this sub-analysis of the Trio Trial, we examined whether and how left atrial size, left ventricular hypertrophy, left ventricular ejection fraction, right ventricular systolic pressure, and left-sided valvular calcification were associated with prospective changes in RRF in patients new to peritoneal dialysis.
Methods
Selection criteria
All patients analyzed in the Trio Trial were eligible for this sub-analysis. Patients who did not have echocardiography within six months of PD initiation were excluded.
Residual renal function measurements and definitions
Residual renal function - defined as the mean of 24-hour urea and creatinine clearances - was measured every 6 weeks from dialysis initiation for 2 years, or until drop-out or study closure. Only values after echocardiography were considered for this sub-analysis.
Echocardiographic measurements, definitions, and categories
Left atrial size was defined as the anteroposterior linear dimension in the parasternal long axis view. Values were categorized as less than 30 mm, 30 to 44 mm, and 45 mm or greater. Information on left ventricular mass index was provided less consistently than commentary on the presence of left ventricular hypertrophy. Left ventricular hypertrophy was thus considered present if specifically reported, and absent if specifically reported as absent or if not mentioned. Left ventricular ejection fraction was calculated using the biplane Simpson’s method, and variously reported as a percentage (with 55% or higher considered normal) or grade (> = 55% – grade I, 45–54% - grade II, 30–44% - grade III, and <30% - grade IV). If reported as percentage it was converted to the corresponding grade. Right ventricular systolic pressure, a surrogate of systolic pulmonary artery pressure, was derived from the maximum pressure gradient difference between the right atrium and ventricle added to an estimate of right atrial pressure. It was categorized as less than 30 mmHg, 30 to 49 mmHg, and 50 mmHg or greater. Valvular calcification was assessed by number of left-sided heart valves (or respective annuli) noted to be calcified (categorized as zero, one, or two).
Outcome measure
The primary outcome was slope in residual renal function (mean of 24-hour urea and creatinine clearances measured every 6 weeks) after baseline echocardiography.
Statistical analyses
After data preparation in Excel (Version 15.14, Microsoft) all statistical analyses were conducted in STATA (Stata/IC 13.1, StataCorp, College Station, Texas). Descriptive statistics were reported as frequencies (%), means (standard deviations) or medians (ranges) as appropriate. Generalized mixed linear regression modeling assuming an autoregressive (1) covariate structure was used to examine associations between RRF and baseline echocardiographic parameters. The primary outcome was assessed in a mixed model that counted time on dialysis, study site, choice of PD solution and interaction term, and history of congestive heart failure, diabetes mellitus, or coronary artery disease in addition to the five echocardiographic parameters (examined individually and together) along with interaction terms as fixed-effects explanatory variables. Patient identification number was the only random-effect covariate included in the model. Two sensitivity analyses were conducted: the first assessed the effect of the timing of echocardiograms relative to PD initiation by adding the date of echocardiography as a fixed-effects covariate to the model. The second assessed whether similar results were obtained if urine volume was used as the primary outcome.
Ethical statements
Compliance with Ethical Standards: study procedures were conducted in accordance with the Good Clinical Practice and the Declaration of Helsinki on biomedical research involving human subjects.
Ethical approval
Written approval to conduct the Trio Trial was obtained from the ethics review boards at each of the participating hospitals - Scarborough Hospital Ethics Review Board, Credit Valley Ethics Review Board, and The Princess Margaret Hospital Ethics Review Board). The protocol was registered at controlled-trials.com/isrctn/pf/26252543 (ISRCTN26252543).
Informed consent
All participants signed written informed consent before enrolment in the study.
Results
Ninety-nine of 101 patients in the Trio Trial received protocolized echocardiograms within 6 months of starting PD. They were followed for a median of 685 days (range 84 to 795 days). Mean initial glomerular filtration rate was 6.8 ± 2.9 ml/min/1.73 m2 and overall unadjusted rate of decline was 0.154 ml/min per month (Table 1). Three patients died during the study. Echocardiograms were performed a median of 16 days after dialysis initiation (range 128 days before to 101 days after) including 22 conducted before PD initiation. The results of the echocardiograms are summarized in Table 2. Most patients had normal left ventricular ejection fractions, and for subsequent purposes this parameter was categorized as normal or reduced.
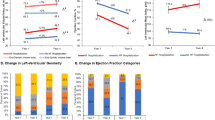
When examined independently of the other parameters, all but left atrial size significantly associated with RRF (Table 3). Figure 1(a–e) represents actual RRF values along with fitted (predicted) rates of RRF decline according to categories of baseline echocardiographic parameters. All p-values were taken from Table 3. Collectively, left ventricular ejection fraction, right ventricular systolic pressure, and left-sided valvular (or annular) calcification remained significantly associated with RRF (Table 4).
Prospective residual renal function decline stratified by echocardiograph parameter: (a) Left atrial size. (b) Left ventricular hypertrophy. (c) Left ventricular systolic function. (d) Right ventricular systolic pressure. (e) Left-sided valvular/annular calcification. The dots represent individual patient renal function measurements and the solid lines predicted slopes. P-values represent significance of the two-way interaction between parameter and time (taken from Table 3). PD = peritoneal dialysis.
The results were not altered by inclusion of the date of echocardiogram relative to dialysis initiation (data not shown), and similar results were obtained if urine volume (rather than residual renal function) was the primary outcome (see Supplements: Fig. 1a–e, and Table 1).
Discussion
In this sub-analysis of the Trio Trial, rising right ventricular systolic pressures predicted faster, while reduced left ventricular ejection fraction and left valvular calcification predicted slower subsequent rates of decline in residual renal function. These novel findings either contrast with the existing literature or have not previously been examined.
In their analysis of 2959 patients with CKD in the Chronic Renal Insufficiency Cohort, Navaneethan et al. found no evidence for a prospective association between pulmonary hypertension (based on echocardiogram-derived right ventricular systolic pressures) and renal events10. However, in defining renal events as a 50% drop in glomerular filtration rate and/or need for renal replacement therapy, the authors may have missed more subtle changes in renal function. We speculate that a rising right ventricular systolic pressure reflects progressive right ventricular diastolic dysfunction and increasing preload dependence11. If so, the universal and sometimes aggressive pursuit of ‘dry’ weights in dialysis-dependent patients with right ventricular diastolic dysfunction would be expected to lead to disproportionately larger drops in cardiac output. Rising right ventricular systolic pressure and declining renal function may also share a common underlying cause. For example, arterial vasoconstriction in the pulmonary and renal vascular beds (on the basis of disordered circulating endothelin-1 and nitrous oxide) has been reported in CKD12. Similarly, increased pulmonary and podocyte calcium-sensing receptor activity - which induces pulmonary smooth muscle cell proliferation and increased proteinuria respectively13,14 – presents another intriguing possibility. However, whether such activation occurs in dialysis-dependent patients has not to our knowledge been studied.
The finding that worsened left ventricular function was associated with slower rates of decline in RRF was unexpected, especially given that left ventricular function was normal in 95% and only moderately impaired in the remaining five percent of patients (Table 2). It is possible that medical therapy of congestive heart failure in patients with only moderate left ventricular dysfunction favorably impacts rates of residual renal function decline. However, we were unable to show an association between a clinical history of congestive heart failure and RRF (data not shown). Left ventricular function did not associate with RRF in another cohort of 242 new PD patients with more severe left ventricular dysfunction15. It is likely that the consequences of left ventricular dysfunction, as seen in other scenarios, may depend on the degree of dysfunction. For example, unlike patients with more moderate dysfunction, only those with sustained ejection fractions under 35% suffer high enough rates of arrhythmic deaths to warrant consideration of therapy with implantable cardiac defibrillators16.
To our knowledge, no studies have looked for a prospective association between left valvular calcification and RRF. In their cross-sectional analysis of 230 prevalent PD patients, Wang et al. found an inverse association between valvular calcification and RRF. However, the direction of association could not be ascertained, and the significance of this association was lost after adjusting for the calcium/phosphorus product and C reactive protein levels7. While it is biologically implausible that the presence of valvular calcification should delay the decline in residual renal function, these observations may be explained by the presence of variables which confound the link between valvular calcification and renal function.
Left ventricular hypertrophy associated with slower rates of decline in RRF only when examined in isolation of the other echocardiographic variables, and left atrial size did not associate with RRF in this cohort of patients. Previous studies did not collectively examine these five echocardiographic variables. For example, although Kim et al. showed a positive association with left atrial size, right ventricular systolic pressure was not included in their multivariate analysis that showed an association between left atrial size and RRF8.
Limitations
The Trio Trial was designed and powered to ascertain changes in renal function following treatment with two different PD solutions, not after echocardiography. Furthermore, the lack of data concerning prospective residual renal function changes in relation to baseline echocardiographic parameters meant that sample size and power calculations could not be performed. The timing of the echocardiograms was also not standardized, with 22 performed before dialysis initiation, and the rest up to 101 days later. While it is unlikely that the echocardiographic parameters would have changed significantly within the time-frame allowed, this was addressed by restricting the analysis to residual renal function measured after echocardiography. This reduced the planned follow-up period for some patients, but extended the findings to those receiving echocardiograms up to 3 months post dialysis initiation. Details included in the reports were not standardized, and parameters such as diastolic function, indexed left ventricular mass, or the ability to grade left ventricular hypertrophy were not available. Finally, the impact of potential unexamined confounders (such as use of certain medications, serum phosphate and calcium and inflammatory markers) cannot be excluded, and this study is unable to conclude causality between echocardiographic findings and prospective changes in residual renal function.
Summary
Elevated right ventricular systolic pressure associated with faster, while reduced left ventricular ejection fraction and valvular calcification associated with slower prospective rates of decline in residual renal function in this cohort of 99 incident PD patients. If confirmed, these findings might yield further insight into the prognostic value of echocardiography and the factors that affect residual renal function in patients receiving PD.
References
Shroff, G. R. & Herzog, C. A. Echocardiography: Providing additional insights into cardiovascular structural and functional abnormalities in advanced CKD. Clin J Am Soc Nephrol. 8(3), 339–41 (2013).
Foley, R. N. et al. Clinical and echocardiographic disease in patients starting end-stage renal disease therapy. Kidney Int. 47(1), 186–92 (1995).
Wang, A. Y. et al. Heart failure in long-term peritoneal dialysis patients: a 4-year prospective analysis. Clin J Am Soc Nephrol. 6(4), 805–12 (2011).
Reque, J. et al. Pulmonary hypertension is an independent predictor of cardiovascular events and mortality in haemodialysis patients. Nephrology. 21(4), 321–6 (2016).
Wang, Z., Jiang, A., Wei, F. & Chen, H. Cardiac valve calcification and risk of cardiovascular or all-cause mortality in dialysis patients: a meta-analysis. BMC Cardiovasc Disord. 18(1), 12 (2018).
Mokoli, V. M. et al. Factors associated with residual urine volume preservation in patients undergoing hemodialysis for end-stage kidney disease in Kinshasa. BMC Nephrol. 19(1), 68 (2018).
Wang, A. Y. et al. Is valvular calcification a part of the missing link between residual kidney function and cardiac hypertrophy in peritoneal dialysis patients? Clin J Am Soc Nephrol. 4(10), 1629–36 (2009).
Kim, S. J. et al. Left atrial enlargement is associated with a rapid decline in residual renal function in ESRD patients on peritoneal dialysis. J Am Soc Echocardiogr. 25(4), 421–7 (2012).
Sikaneta, T. et al. The Trio Trial - A Randomized Controlled Clinical Trial Evaluating the Effect of a Biocompatible Peritoneal Dialysis Solution on Residual Renal Function. Perit Dial Int. 36(5), 526–32 (2016).
Navaneethan, S. D. et al. Prevalence, Predictors, and Outcomes of Pulmonary Hypertension in CKD. J Am Soc Nephrol. 27(3), 877–86 (2016).
Naeije, R. & Manes, A. The right ventricle in pulmonary arterial hypertension. Eur Respir Rev. 23(134), 476–87 (2014).
Sise, M. E., Courtwright, A. M. & Channick, R. N. Pulmonary hypertension in patients with chronic and end-stage kidney disease. Kidney Int. 84(4), 682–92 (2013).
Yamamura, A. et al. Enhanced Ca(2+)-sensing receptor function in idiopathic pulmonary arterial hypertension. Circ Res. 111(4), 469–81 (2012).
Oh, J. et al. Stimulation of the calcium-sensing receptor stabilizes the podocyte cytoskeleton, improves cell survival, and reduces toxin-induced glomerulosclerosis. Kidney Int. 80(5), 483–92 (2011).
Singhal, M. K. et al. Rate of decline of residual renal function in patients on continuous peritoneal dialysis and factors affecting it. Perit Dial Int. 20(4), 429–38 (2000).
Röger, S. et al. Therapy optimization in patients with heart failure: the role of the wearable cardioverter-defibrillator in a real-world setting. BMC Cardiovasc Disord. 18(1), 52 (2018).
Acknowledgements
The Trio Trial was partially funded by an unrestricted grant from Gambro Lundia AB, Lund, Sweden.
Author information
Authors and Affiliations
Contributions
S.M.: data analysis and substantially revised the work; K.Y.: interpreted data; G.W.: design of work; B.O.: data acquisition; D.S.: data acquisition; G.N.: interpretation of data; E.H.: interpretation of data; A.S.: data analysis; A.B.: interpretation of data; P.T.: design of work; T.S.: conception, design, analysis, interpretation and drafted work. All authors approved the final submitted version, were responsible for the integrity of their work, and acknowledged resolution of any unresolved questions regarding the integrity or accuracy of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mahdavi, S., Yared, K., Wu, G. et al. Associations between echocardiographic findings and prospective changes in residual renal function in patients new to peritoneal dialysis. Sci Rep 9, 18434 (2019). https://doi.org/10.1038/s41598-019-54851-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-54851-2
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.