Abstract
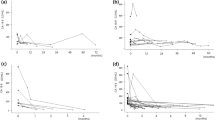
Laparoscopic hepatectomy (LH) has been accepted widely owing to its advantages as a minimally invasive surgery; however, laparoscopic right hemihepatectomy (LRH) has rarely been reported. We aimed to compare the benefits and drawbacks of LRH and open approaches. Between January 2014 and October 2017, 85 patients with tumor and hepatolithiasis who underwent LRH (n = 30) and open right hemihepatectomy (ORH) (n = 55) were enrolled in this study. For tumors, LRH showed significantly better results with respect to blood loss (P = 0.024) and duration of hospital stay (P = 0.008) than ORH, while hospital expenses (P = 0.031) and bile leakage rate (P = 0.012) were higher with LRH. However, the operative time and rate of other complications were not significantly different between the two groups. However, for hepatolithiasis, there was less blood loss (P = 0.015) and longer operative time (P = 0.036) with LRH than with ORH. There were no significant difference between LRH and ORH in terms of hospital stay, hospital expenses, and complication rate (P > 0.05). Moreover, the postoperative white blood cell count, alanine aminotransferase level, aspartate aminotransferase level, and total bilirubin were not significantly different in both types of patients (P > 0.05). Our results suggest the safety and feasibility of laparoscopy technology for right hemihepatectomy in both tumor and hepatolithiasis patients.
Similar content being viewed by others
Introduction
With the recent advances in technique and equipment in laparoscopic technology, several comparative series have suggested the feasibility and safety of laparoscopic hepatectomy (LH)1,2,3,4,5,6,7,8,9,10, including minor liver resections1,2,3,4, left hepatic lobe5,6 major hepatectomies1,2,7,8, and left hemihepatectomy9,10,11. Our previous research also showed that laparoscopic left lateral hepatic sectionectomy6 and laparoscopic left hemihepatectomy11 offered significantly more advantages than open surgery. However, thus far, few studies have explored the details of laparoscopic right hemihepatectomy (LRH). The right hemiliver exhibits a relatively complex intrahepatic tract. More importantly, the right liver is located deep in the abdominal cavity, and mobilization and exposure remain difficult due to the lack of a smooth and safe liver retractor12,13. These anatomical features of the right liver present an unfavorable condition for laparoscopy. Thus, till date, there was insufficient research to summarize the benefits and drawbacks of LRH compared with those of ORH. Moreover, there is no unified conclusion about the optimal approach, and no clear guidelines exist for the indications of the laparoscopic approach. The present study aimed to compare the clinical and economic impact of LRH and ORH in both benign and malignant lesions.
Methods
Patients and grouping
This retrospective clinical study was conducted at the Department of General Surgery and approved by the institutional review board (IRB) committee at the Second Affiliated Hospital of Nanchang University. Informed consent was obtained from all the subjects. This study was performed as per the established national and institutional ethical guidelines regarding the involvement of human subjects and the use of human tissues for research. All the patients with tumor and hepatolithiasis (Table 1) who underwent LRH (n = 30) or ORH (n = 55) were enrolled from the database between January 2014 and July 2017. The study was approved by the Second Affiliated Hospital of Nanchang University Ethics Committee, and specimens were collected after obtaining informed consent from the patients.
LRH and ORH procedure
Under general anesthesia, the patient was placed in the supine position with both the legs separated. A 12-mm trocar was placed on the right side of the umbilical cord 2 cm away for laparoscopy. The other trocars were positioned appropriately in the upper abdomen to allow optimal mobilization and dissection of the liver, as shown in Fig. 1. The two main operating 12-mm trocars were located below the xiphoid and 5 cm below the midline of the right clavicle. The other two 5 mm trocars were placed 2 cm above the umbilical cord and under the subcostal at the anterior axillary line respectively. The patient was tilted 30°–45° to the left. The pneumoperitoneum was established by maintaining an intra-peritoneal pressure of 12–14 mmHg and differential pressure with the central venous pressure (CVP) of 4–6 mmHg. The liver anatomy and the right liver were evaluated using laparoscopy. In addition, laparoscopic liver ultrasonography was used to determine the location and extent of the lesions and identify potentially hazardous intrahepatic vascular and biliary structures. The right hepatic artery were first dissected and then ligated with a Hem-o-Lok clip. The right portal vein was dissected and was ligated using Hem-o-Lok clips. We distinguish the left from the right hemiliver based on the hepatic ischemic line; however, the middle hepatic vein is occasionally damaged due to deviation. Therefore, it is crucial to determine the direction of the middle hepatic vein before dissection. We should find the branch of the middle hepatic vein first and then look for the trunk along the branch. Laparoscopic ultrasonography ensures that the middle hepatic vein is completely avoided while providing images of intrahepatic intubation14. We ligated intrahepatic vascular or biliary using Hem-o-Lok clips. The right hepatic vein was ligated using the Hem-o-Lok clips or the Endo-GIA stapler. The specific steps are shown in Fig. 2. The steps of ORH were similar to those of LRH.
Surgical techniques for LRH. (A) the preoperative CT film of patient; (B) The cystic duct was dissected and ligated; (C) The right hepatic artery were dissected and then ligated. (D) The right portal vein was dissected and was ligated. (E) The hepatic ischemic line; the left intrahepatic bile ducts are interrupted and the visible stones are removed. (F,G) Intrahepatic duct isolated and ligated; (H) The right hepatic vein and the surrounding parenchymal tissues are transected using an Endo-GIA device. (I) The CT film of patient after 1 month.
Statistical analyses
Statistical analyses were performed with SPSS software, version 17.0 (SPSS Inc., Chicago, IL, USA). Continuous variables are expressed as mean ± standard deviation or median (range) values, and categorical variables are expressed as numbers. Continuous variables were compared using Student’s t-test test or the Mann–Whitney U-test, while categorical variables were compared using the χ2 test or Fisher’s exact test. P < 0.05 was considered statistically significant.
Results
Patient characteristics
Total 85 patients who underwent LRH (n = 30) or ORH (n = 55) were enrolled between January 2014 and July 2017. Their demographic and clinical/laboratory data are presented in Table 1. There were no significant inter-group differences in terms of sec, age, and liver function (P > 0.05). Of the 30 patients in the laparoscopic group, 18 had hepatolithiasis and 12 had tumor. Of the 55 patients in the open group, 38 had hepatolithiasis and 17 had tumor.
Perioperative outcome
The surgical outcomes have been shown in Table 1. LRH patients had longer operative times (P = 0.023) and higher bile leakage (P = 0.031); however, they had less blood loss (P = 0.001) and shorter hospital stay (P = 0.002) than the ORH patients. Furthermore, there were no significant differences in the frequency and intensity of other complications, postoperative white blood cell (WBC) count, aspartate aminotransferase (AST) level, and alanine aminotransferase (ALT) level (P > 0.05), suggesting no difference in the perioperative liver injury or functional outcome.
We further divided the patients into the tumor and hepatolithiasis group. Among the tumor group, 12 patients were in the LRH group, and 17 were in the ORH group. With respect to the hepatolithiasis group, 18 patients were in the LRH group, and 38 were in the ORH group. As shown in Table 2, the LRH showed significantly better results in terms of less blood loss (P = 0.024) and shorter hospital stay (P = 0.008); however, LRH patients also incurred a lower hospital cost (P = 0.031) and had a higher bile leakage rate (P = 0.012) than ORH patients. Moreover, there was less blood loss (P = 0.015) and longer operative time (P = 0.036) for LRH than for ORH, as shown in Table 3. However, there were no statistical differences between LRH and ORH in terms of the hospital stay; hospital expenses; complication rate; as well as the postoperative WBC, AST, and ALT levels (P > 0.05) in both the tumor and hepatolithiasis group.
Discussion
LH has matured and become a treatment option for benign and malignant lesions of the liver1,2,3,4,5,6,7,8,9,10, especially for left hepatectomy5,6,9,10,11. However, few studies have focused on LRH owing to the anatomical features12,13. It was difficult to mobilize and expose, and it was also difficult to control bleeding by laparoscopy. In this study, we aimed to compare the clinical and economic impact of LRH and ORH in patients with tumors and hepatolithiasis. Our results suggest that LRH offers several advantages over ORH, including reduced blood loss, lower hospital stay, and fewer complications.
Our results show that LRH is associated with a longer operative time, but less blood loss and shorter hospital stay than ORH. For longer operative time and shorter hospital stay, our results were consistent with previous research2,12,15,16. However, bleeding control during LRH was superior to that during open hepatectomy, possibly due to improved intraoperative magnification for surgical manipulations, use of new coagulating devices unlike expected, and the pressure associated with the pneumoperitoneum that may have helped decrease bleeding during liver parenchymal transection4,12,17,18. We believe that occasional bleeding and hepatic vein injury are the most common hepatectomy risks, irrespective of which approach is selected for use. Hence, detailed preoperative evaluations, including computed tomography, magnetic resonance imaging, 3D visualization technology, and especially intraoperative ultrasonography are essential to accurately reveal the size and location of the lesion and understand the individual variations in the blood vessels and the biliary tract in order to reduce the bleeding risk. Given the use of different surgical procedures and complexity, we further divided the patients into the tumor group and the hepatolithiasis group. For tumor patients, the operative time in the LRH group was similar to that in the ORH group; however, the LRH group experienced less blood loss and shorter hospital stay with higher hospitalization costs than the ORH group. As per our understanding, the rapid developments and advances in laparoscopic equipment, such as the Endo-GIA stapler, not only greatly reduce the operative time but also effectively prevent bleeding19. Most importantly, the surgeon’s effective and professional knowledge have improved their technical skills over time and made them more confident for performing surgery, reflecting the standardization of the surgical procedures. With respect to the hospitalization costs, LRH was associated with significantly higher costs than ORH. The laparoscopic material, such as laparoscopy trocars, Hem-o-Lok clips, and staplers, along with the longer operative time contributed to the increased hospital costs of LRH13,15,20. Moreover, ultrasonic shears, vessel sealing devices (e.g., LigaSure), laparoscopic ultrasonography systems, and suturing techniques are being improved constantly, reducing the operative time while increasing the cost. The surgical procedure for hepatolithiasis is different from that for a tumor and is therefore more challenging. Severe perihepatic adhesions, deformed biliary anatomy, and fibrotic parenchyma in patients with hepatolithiasis may not only prolong the operation time, but also may increase the risk of postoperative complications, such as intraabdominal fluid collection and biliary fistula21. Considerable time is required to dissect the adhesions caused by inflammation around the liver and remove the stones from the bile duct in hepatolithiasis patients. Sometimes, choledochoscopy and hydroelectric lithotripsy need to be performed. In most cases, a T tube needs to be placed. These additional operations were not only cumbersome and complicated, but also lacked the advantages offered by laparotomy, such as operating horizon and space and tactile feedback; in addition, they require greater hand-eye coordination22. So, it was not surprising. Consistent with these reports, our results showed that the hepatolithiasis patients in our study who underwent LRH had longer operative times and less blood loss than those who underwent ORH23,24. Although LRH had no obvious superiority in terms of the operative time and hospital stay, it still had the advantage of less bleeding. Furthermore, the two groups showed no significant difference in the postoperative alanine transferase, albumin, and total bilirubin levels, suggesting no difference in the extent of perioperative liver injury or functional outcome.
With respect to the complications, our results showed that the tumor patients in our study who underwent LRH demonstrated a higher bile leakage rate than those who underwent ORH; however, no such difference was observed for the hepatolithiasis patients. Other complications were comparable between the two groups. It was partially consistent with laparoscopic left hepatectomy9,11. The most important reason was that we routinely performed water injection experiments from the cystic tube to detect the presence of bile leakage in tumor patients who underwent ORH but not in those who underwent LRH. The measure considerably reduced the probability of bile leakage. However, in case of hepatolithiasis patients, T tube drainage was performed regularly for both LRH and ORH patients25.
For LRH, we recommend that the patient be tilted to the left so that the liver is turned to the left to facilitate exposure of the right liver due to gravity. The middle hepatic vein branch and the trunk along the branch should then be identified. In addition, CVP should be maintained between 4 and 6 cm H2O, the optimal intraoperative range for reducing bleeding and hepatic vein reflux26.
In conclusion, this comparative study suggests that laparoscopy is suitable for right hepatectomy. Our results show that it is safe and feasible to perform to use laparoscopy technology for right hemihepatectomy in both tumor and hepatolithiasis patients. It is expected to be the first choice for the treatment of right hemiliver.
References
Xie, S. M. et al. Laparoscopic Versus Open Liver Resection for Colorectal Liver Metastases: A Comprehensive Systematic Review and Meta-analysis. Sci Rep 8, 6364 (2018).
Abu Hilal, M. et al. Assessment of the financial implications for laparoscopic liver surgery: a single-centre UK cost analysis for minor and major hepatectomy. Surg Endosc 27, 2542–50 (2013).
Nguyen, K. T., Gamblin, T. C. & Geller, D. A. World review of laparoscopic liver resection-2,804 patients. Ann Surg 250, 831–41 (2009).
Croome, K. P. & Yamashita, M. H. Laparoscopic vs open hepatic resection for benign and malignant tumors: An updated metaanalysis. Arch Surg 145, 1109–18 (2010).
Ratti, F. et al. Learning curve of self-taught laparoscopic liver surgeons in left lateral sectionectomy: results from an international multi-institutional analysis on 245 cases. Surg Endosc 30, 3618–29 (2015).
Liu, Z., Ding, H., Xiong, X. & Huang, Y. Laparoscopic left lateral hepatic sectionectomy was expected to be the standard for the treatment of left hepatic lobe lesions: A meta-analysis. Medicine (Baltimore) 97, e9835 (2018).
Dagher, I. et al. Laparoscopic major hepatectomy: an evolution in standard of care. Ann Surg 250, 856–60 (2009).
Kasai, M. et al. Laparoscopic versus open major hepatectomy: a systematic review and meta-analysis of individual patient data. Surgery 163, 985–95 (2018).
Cho, H. D. et al. Comparison of pure laparoscopic versus open left hemihepatectomy by multivariate analysis: a retrospective cohort study. Surg Endosc 32, 643–50 (2018).
Peng, L. et al. Laparoscopic left-sided hepatectomy for the treatment of hepatolithiasis: A comparative study with open approach. Int J Surg 40, 117–23 (2017).
Yin, X., Luo, D., Huang, Y. & Huang, M. Advantages of laparoscopic left hemihepatectomy: A meta-analysis. Medicine (Baltimore) 98, e15929 (2019).
Dagher, I. et al. Laparoscopic versus open right hepatectomy: a comparative study. Am J Surg 198, 173–7 (2009).
Dagher, I. et al. Laparoscopic right hepatectomy: original technique and results. J Am Coll Surg 206, 756–60 (2008).
Araki, Z. et al. Intraoperative ultrasonography of laparoscopic hepatectomy: key technique for safe liver transection. J Am Coll Surg 218, e37–41 (2014).
Medbery, R. L. et al. Laparoscopic vs open right hepatectomy: a value-based analysis. J Am Coll Surg 218, 929–39 (2014).
Belli, G. et al. Laparoscopic versus open liver resection for hepatocellular carcinoma in patients with histologically proven cirrhosis: short- and middle-term results. Surg Endosc 21, 2004–11 (2007).
Morino, M., Morra, I., Rosso, E., Miglietta, C. & Garrone, C. Laparoscopic vs open hepatic resection: a comparative study. Surg Endosc 17, 1914–8 (2003).
Morise, Z. et al. Pure laparoscopic hepatectomy for hepatocellular carcinoma with chronic liver disease. World J Hepatol 5, 487 (2013).
Schemmer, P. et al. The use of endo-GIA vascular staplers in liver surgery and their potential benefit: a review. Dig Surg 24, 300–5 (2007).
Polignano, F. M. et al. Laparoscopic versus open liver segmentectomy: prospective, case-matched, intention-to-treat analysis of clinical outcomes and cost effectiveness. Surg Endosc 22, 2564–70 (2008).
Ye, X., Ni, K., Zhou, X., Xie, K. & Hong, X. Laparoscopic versus open left hemihepatectomy for hepatolithiasis. J Surg Res 199, 402–6 (2015).
Wang, X., Li, Y., Zhou, J., Wu, Z. & Peng, B. Hand-assisted laparoscopic splenectomy is a better choice for patients with supramassive splenomegaly due to liver cirrhosis. J Laparoendosc Adv Surg Tech A 22, 962–7 (2012).
Liu, X., Min, X., Ma, Z., He, X. & Du, Z. Laparoscopic hepatectomy produces better outcomes for hepatolithiasis than open hepatectomy: An updated systematic review and meta-analysis. Int J Surg 51, 151–63 (2018).
Namgoong, J. M. et al. Comparison of laparoscopic versus open left hemihepatectomy for left-sided hepatolithiasis. Int J Med Sci 11, 127–33 (2014).
Wills, V. L., Gibson, K., Karihaloot, C. & Jorgensen, J. O. Complications of biliary T-tubes after choledochotomy. ANZ J Surg 72, 177–80 (2002).
Montorsi, M. et al. Perspectives and draw backs of minimally invasive surgery for hepatocellular carcinoma. Hepatogastroenterology 49, 56–61 (2002).
Acknowledgements
This work was supported by National Natural Science Foundation of China (No. 81760514; No.81360338).
Author information
Authors and Affiliations
Contributions
The research was designed by Yong Huang, Xin Yu; Yong Huang, Yupeng Tang, Xin Yu performed the research and provided analytic tools; Yong Huang, Yupeng Tang, Xin Yu analyzed the data; Yong Huang, Dilai Luo, Mingwen Huang, Yupeng Tang, Xin Yu wrote the paper, Yong Huang, Dilai Luo, Mingwen Huang, Xin Yu revised critically, final approval.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yu, X., Luo, D., Tang, Y. et al. Safety and feasibility of laparoscopy technology in right hemihepatectomy. Sci Rep 9, 18809 (2019). https://doi.org/10.1038/s41598-019-52694-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-52694-5
This article is cited by
-
Laparoscopic versus open in right posterior sectionectomy: a systematic review and meta-analysis
Langenbeck's Archives of Surgery (2023)
-
Laparoscopic middle-hepatic-vein-guided anatomical hemihepatectomy in the treatment of hepatolithiasis: a 10-year case study
Surgical Endoscopy (2022)
-
Safety and feasibility for laparoscopic versus open caudate lobe resection: a meta-analysis
Langenbeck's Archives of Surgery (2021)
-
Comparative analysis of the safety and feasibility of laparoscopic versus open caudate lobe resection
Langenbeck's Archives of Surgery (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.