Abstract
This paper introduces a novel framework for fast parameter identification of personalized pharmacokinetic problems. Given one sample observation of a new subject, the framework predicts the parameters of the subject based on prior knowledge from a pharmacokinetic database. The feasibility of this framework was demonstrated by developing a new algorithm based on the Cluster Newton method, namely the constrained Cluster Newton method, where the initial points of the parameters are constrained by the database. The algorithm was tested with the compartmental model of propofol on a database of 59 subjects. The average overall absolute percentage error based on constrained Cluster Newton method is 12.10% with the threshold approach, and 13.42% with the nearest-neighbor approach. The average computation time of one estimation is 13.10 seconds. Using parallel computing, the average computation time is reduced to 1.54 seconds, achieved with 12 parallel workers. The results suggest that the proposed framework can effectively improve the prediction accuracy of the pharmacokinetic parameters with limited observations in comparison to the conventional methods. Computation cost analyses indicate that the proposed framework can take advantage of parallel computing and provide solutions within practical response times, leading to fast and accurate parameter identification of pharmacokinetic problems.
Similar content being viewed by others
Introduction
Pharmacokinetics is defined as the study of the bodily absorption, distribution, excretion, and metabolism of a drug. Pharmacokinetics is mainly concerned with the effect of the body on the drug, in contrast to pharmacodynamics, which is mainly concerned with the effect of the drug on the body. These two disciplines comprise the field of clinical pharmacology1. The rational use of a drug requires an understanding of how the drug is absorbed and what the onset of action is, as well as an understanding of how long the drug will have an effect. The duration of the effect of a drug is determined by its distribution in various body tissue, its metabolism, and its elimination from the body. No drug can be approved by the United States Food and Drug Administration without the completion of a detailed pharmacokinetic analysis.
Most tissues (such as muscle or fat) are simply inert storage depots for the drug and do not chemically alter it; they rather serve to remove the drug from the circulation but do not eliminate it from the body. This process is called distribution. However, other tissues, most notably the liver and the kidneys, can chemically alter the drug, either to metabolites that still have some effect on the body, or to inactive metabolites. In addition, the kidneys can serve to eliminate the drug via urine. This process continues as blood cycles through the vascular bed. As the drug is eliminated by metabolic processes in the liver and kidneys, the drug that was stored in inert tissues by the distribution process leaves those storage depots and is recirculated undergoing metabolism and elimination from the body. Eventually, all drug stored in the body reaches the sites of metabolism and elimination.
From this abbreviated description, one can appreciate the potential complexity of the physiological processes that determine drug disposition. This complexity is in marked contrast to the simplicity of the data from a typical pharmacokinetic study. In a typical pharmacokinetic study, the investigator administers a fixed dose of the drug to a human volunteer or a patient with the disease the drug is expected to treat. Blood samples are then drawn at fixed intervals after the administration of the drug and the investigator determines the concentration of the drug in these samples. It is seldom possible to determine the drug concentration in the various tissues of the body. Thus, the investigator is left with essentially a table of drug concentrations in the blood as a function of time.
The ultimate goal of the investigator is to predict the drug concentration that would exist at times different from the sampling times of the study and for different doses, as well as to understand the variability that might exist between different subjects. Given the complexity of drug absorption, distribution, and elimination/metabolism and the sparseness of the data, it is inevitable that mathematical modeling plays a prominent role in pharmacokinetic analysis, bridging the gap between physiology and the available data. A major challenge in using pharmacokinetic models to predict patient response to a specific drug is the lack of knowledge regarding patient-specific parameters of the pharmacokinetic model2,3. One framework that is widely used in clinical practice to assist in the titration of different drugs is population pharmacokinetics, a statistical method to predict pharmacokinetic response based on a series of demographic and pathophysiological features of the patient.
Population pharmacokinetics has been covered under various topics, such as therapeutic drug monitoring, target concentration intervention, and Bayesian forecasting4. The Bayesian forecasting has been described extensively in the literature and has been implemented in practice for many drugs, especially antibiotics5,6,7,8. A number of softwares are also available for dose individualization8,9. The general frameworks behind these softwares are based on maximum likelihood estimation and mixed-effect modeling technique.
There are multiple factors contributing to the widespread adoption of the population pharmacokinetic framework. First, population pharmacokinetics provides an easy to use framework which does not involve complicated computations. In addition, calculating the appropriate drug dose involves the utilization of a statistical model and the corresponding statistical parameters. Once the raw pharmacokinetic data, generally collected during clinical studies, has been analyzed and statistical parameters of the population pharmacokinetic model are identified, access to raw data collected from previous patients is no longer needed10.
Although population pharmacokinetics has been used for decades, there are severe limitations associated with this approach. Specifically, population pharmacokinetics does not provide sufficient information to predict patient-specific pharmacokinetic response to drugs and only provides general pharmacokinetic behavior for a target patient population with limited prediction accuracy11,12. Additionally, certain assumptions regarding the statistical distribution of parameters (e.g., Gaussian), may not hold, which can affect the predictive performance of the model. Furthermore, the population pharmacokinetic approach is generally concerned with parameter identification of statistical models and fails to include validated mechanistic models which are based on the laws of physics (e.g., conservation of mass). Inclusion of mechanistic models for pharmacokinetics, which use ordinary differential equations (ODEs) that characterize drug distribution in the body, can provide a framework based on basic principles to characterize pharmacokinetic response and can increase prediction accuracy13. As the number of parameters to reproduce physiological functions tend to be large in pharmacokinetic models, efficient parameter estimation methods are essential.
Modern medicine is moving towards personalized medicine, where genetic analysis can guide personalized treatment14. Genetic analysis can also provide further insight on drug effect (i.e., pharmacodynamics) on individual patients. However, currently no framework exists for personalized pharmacokinetics to guide drug dosing. To ensure an effective personalized pharmacological treatment, we need to address interpatient and intrapatient variabilities in both pharmacokinetics and pharmacodynamics.
In this paper, we provide an approach to address the current gap in the continuum of pharmacological treatment by presenting a framework that can accurately predict pharmacokinetic response for a specific patient, which in turn can assist in personalized drug dosing. Specifically, a framework is presented that can use prior data as well as a limited number of measurements from the subject to accurately identify the parameters of a dynamical system model of drug pharmacokinetics for that subject. Such a dynamical system model with accurate parameter values can in turn be used to predict drug concentration over time, and hence, provide a framework to guide drug dosing. As discussed below, this problem involves complex computations, and hence, a numerical framework will be presented to solve the parameter identification problem in a reasonable time frame. The efficacy of the presented framework is established through analysis of pharmacokinetic data for the sedative drug propofol obtained from a dataset of 59 patients previously reported in the literature15,16.
Compartmental Dynamical Systems
In this section, we provide a brief overview of the compartmental dynamical systems framework to model pharmacokinetics (see17 for a detailed discussion). Pharmacokinetic compartmental models make the assumption that the body consists of multiple compartments. Furthermore, the drug concentration is assumed to be uniform due to ideal mixing under each compartment. There are two major types of activities, i.e., the transportation to other compartments, and elimination from the body. These two activities are controlled by the metabolic processes of the human body. In the approximation of the real activities, the transport rate is usually assumed to be proportional to drug concentration. In addition, anotherapproximation is made that the mixing of the drug is instantaneous. This has marginal effect on the accuracy of the model as long as the estimation of drug concentration is not conducted right after the administration of the drug.
To formalize the parameter identification problem, we propose to model pharmacokinetics (PK) with compartmental dynamical systems. Specifically, drug concentration dynamics for a n-compartment system are given by the state space equation
where the drug concentration in each compartment is denoted by x = [x1, …, xn]T, the drug infusion from an external source is denoted by w = [w1, …, wn]T, and the mass exchange between different compartments are characterized by f(x) = [f1(x), …, fn(x)]T, where for i = 1, …, n,
with \({\hat{a}}_{ij}\) reflecting drug exchange coefficients between compartments.
The above model is general and can be used to model any pharmacokinetic system. For instance, a special case of the above nonlinear model is the compartmental mammillary dynamical system, which is often used to model the pharmacokinetics of certain drugs (e.g., the sedative propofol). Usually, a central compartment will be defined in the nonlinear mammillary model as the site for drug administration. The drug elimination through metabolism or other means occur from this central compartment. This compartment also connects to one or several peripheral compartments for the exchange of drug. The central compartment is considered to be a combination of blood within arteries and veins and the organs that have high blood flow to weight ratios. On the other side, the peripheral compartments are assumed to be metabolically inert as far as drug is concerned.
The Parameter Identification Problem
In order to use a compartmental dynamical system to predict pharmacokinetic response, exact values of the parameters of the compartmental dynamical model (i.e., exchange coefficients between compartments, drug metabolism rate, etc.) are required. These values are unique to each individual patient and vary from patient to patient. An accurate knowledge of the compartmental model parameters can result in a more accurate prediction of the pharmacokinetic response of the patient for a given drug.
The parameter identification problem involves solving an inverse problem, where a set of measurements of drug concentration in the blood at multiple time points is given and the parameters of the compartmental dynamical system need to be identified18. This inverse problem is also referred to as system identification in the dynamical systems and controls literature. The inverse problem can be cast as an optimization problem, where a set of parameters need to be identified that minimize the error of model fit given the available data. The optimization problem associated with pharmacokinetics is generally under-determined (i.e., there are more unknowns than measurements), and hence, ill-posed (i.e., there are infinitely many solutions to the problem given the available information)19.
We denote unknown pharmacokinetic model parameters by \(\theta \in {{\mathbb{R}}}^{n}\), where we assume that there are n unknown parameters. Furthermore, we assume that m noisy measurements y1, …, ym at time instants t1, …, tm are given, where m < n. The parameter identification problem involves solving the optimization problem
where J(y, θ) is a cost function quantifying model fit. Here, we define the cost function as
where F(θ, t1, …, tm) = [F1(θ, t1), …, Fm(θ, tm)]T denotes a mapping from model parameters θ to drug concentration at time instants t1, …, tm.
Limitations of Using Current Optimization Methods for Solving the Pharmacokinetics Parameter Identification Problem
There are certain drawbacks associated with using existing optimization frameworks such as Levenberg-Marquardt (LM) for solving the parameter identification problem discussed in this paper as explained below.
Long computation time
Each function evaluation in the optimization problem (3) (i.e., computing modeling error given a set of parameters) involves the solving a set of forward ordinary differential equations (ODEs) characterizing the compartmental pharmacokinetic model, which is computationally expensive. The optimization framework has to repeatedly solve the forward ODEs and update the set of parameters until the model error is minimized. The convergence of this process can be extremely slow. In addition, optimization methods such as the LM method are not appropriate for parallelization to reduce the computation time.
Lack of an effective mechanism to use prior knowledge
As discussed above, current optimization frameworks allow one to choose an initial set of parameters θ0 for which the desired optimum needs to be sufficiently close. Current practice involves selecting an “average” set of values for this initial parameter set (which serves as our best estimate of parameter values). This is a drawback of current frameworks, as there is no “average patient” and “average values.” For personalized pharmacokinetics, we require an effective method for selecting the initial set of parameters such that they are as close as possible to the actual pharmacokinetic parameters.
A Framework for Parameter Identification with Application to Personalized Pharmacokinetics
To address the limitations of current optimization methods, we present a framework known as the Constrained Cluster Newton (CCN) method to solve the parameter identification problem. This method has two main advantages as compared to more traditional methods for solving the inverse problem. First, it provides a mechanism to include pharmacokinetic data collected from previous patients to guide the optimization process. Second, it involves dividing the problem into a series of independent sub-problems that will allow parallel computing to reduce computation time.
The proposed Constrained Cluster Newton method is an extension to the Cluster Newton method3. The Cluster Newton method is used to find a family of solutions for an under-determined inverse problem in a way that is significantly more efficient than solving a series of independent optimization problems with different initialization values (see3). The Cluster Newton method starts with a cluster of initial points, which are generally sampled from a region defined by average pharmacokinetic values and ranges reported in the literature. It then forward-solves the ODEs for each point in the cluster. Next, it fits a hyperplane to the solutions using a least squares framework to obtain a linear approximation of the function characterizing the forward problem (which is usually nonlinear). All the initial points are collectively moved closer to the solution via an update step. By repeating the above steps, the cluster of points will move close to the solution(s) of the inverse problem. The accuracy of the estimated solutions can then be further improved using Broyden’s method until the desired accuracy is achieved3,20.
In an extension to the Cluster Newton method (CN), which we call the Constrained Cluster Newton method, we can use data from prior patients to guide the optimization process by imposing constraints on the initial cluster of points. Specifically, we assume that a dataset including blood concentrations overtime is available for a specific drug. Next, instead of randomly sampling points uniformly from a relatively large region defined by the range of values determined through population pharmacokinetics, we identify a set of patients in the archived dataset that have the most similar pharmacokinetic response to the patient under consideration to generate a more targeted cluster of points, used for initialization of the optimization framework.
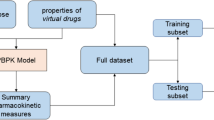
The overall architecture of the fast personalized pharmacokinetics framework is shown in Fig. 1. Initially, the parameter identification component is performed offline (and once) to compute the pharmacokinetic parameters for previously collected data from a set of patients (i.e., drug concentration over time). Next, when the pharmacokinetic response of a new patient is needed, the framework identifies the most similar patients in the archived dataset to complement the drug concentration measurement obtained from the new patient. Finally, once the pharmacokinetic parameters for the new patient are identified, they are used in conjunction with a forward-solver to compute the pharmacokinetic response of the patient to the drug (e.g., the area under the drug concentration over time curve, maximum concentration, half life, etc.). Details of these processes are discussed below.
Identifying the parameters of patients in the archived dataset
First, an inverse problem for each patient in the archived dataset is solved such that one set of pharmacokinetic parameters is obtained for each patient. This process is performed once and offline. Specifically, if there are q patients in the archived dataset, then we identify pharmacokinetic parameters θj, j = 1, …, q, for the jth patient by minimizing J(yj, θ), where \(J(\,\cdot \,,\,\cdot \,)\) is defined by (4) and yj = [yj,1, …, yj,mq]T is the set of measurements available for the jth patient in the archived dataset. Here, we use the LM method; however, other frameworks may be used.
Initial estimate of the parameters for the new patient
Next, we solve the inverse problem (3) for the new patient under consideration to identify an initial estimate of the parameters \(\tilde{\theta }\). This is performed by solving a standard parameter identification problem by initializing the optimization parameters using average pharmacokinetic parameter values determined from the archived dataset or published in the literature. While the identified parameter \(\tilde{\theta }\) using this step is not accurate, it serves as our best estimate of the approximate region in the parameter space where the actual parameters reside.
Using prior data from the archived dataset to predict pharmacokinetic response
Finally, we select a set of patients from the archived dataset with a pharmacokinetic response that is closest to the new patient under consideration. Patients with the most similar pharmacokinetics can be selected either by selecting any patient from the archived dataset with his/her pharmacokinetic parameters being within a specific distance from the new patient (threshold-based), or by selecting the n patients from the archived dataset who are closest to the new patient (n-nearest neighbor). In the threshold-based approach, a patient from the archived dataset is considered similar to the current patient if \(\parallel \theta -\tilde{\theta }\parallel \le \alpha \), where θ is the pharmacokinetic parameters of the patient selected from the archived dataset, \(\tilde{\theta }\) is the initial estimate for the new patient, and α > 0 is a specified threshold. Alternatively, if the n-nearest neighbor is used, then n patients with the smallest distance \(\parallel \theta -\tilde{\theta }\parallel \) are selected.
Once the set of patients from the archived dataset is selected, their identified pharmacokinetic parameters are used to define a targeted region and generate a cluster of points to use with the Cluster Newton method. Note that the choice of the cluster used for initializing the optimization process has a significant impact on the results. Hence, selecting similar patients from the archived dataset can improve the results by defining a more targeted region to use for generating the initial cluster. Here, we choose a minimum bounding box to define the region from which the cluster is randomly sampled. Once the pharmacokinetic parameters of the new patient are identified, the pharmacokinetic response of the patient to a dose of drug can be computed by forward solving the ODEs using the identified parameters. A schematic of the proposed approach outlined in Sections 2 to 2 is shown in Fig. 2.
Application to Personalized Pharmacokinetics for the Sedative Drug Propofol
In this section, we model the pharmacokinetics of the sedative agent propofol21 as an example for the proposed framework. Propofol is a fast-acting intravenous hypnotic agent. It can produce anxiolysis when being used in low doses. In higher doses, it causes hypnosis. Propofol may be administered as a bolus or continuously. Propofol depresses the myocardial contractility, which leads to decreased cardiac output. Furthermore, the decrease in cardiac output affects the redistribution kinetics, which is related to the blood transportation from the central compartment to the peripheral compartments. As a consequence, the drug concentration in the central compartment may be increased, leading to more depression in myocardial contractility, and oversedation.
The pharmacokinetics of propofol are described by the three-compartment model17,22 shown in Fig. 3. As shown in Fig. 3, x1 represents the mass of drug in the central compartment. The remaining portion of the drug in the body is assumed to reside in two peripheral compartments. The masses are shown as x2 and x3, respectively. Specifically, x2 is associated with muscle and the x3 is related with fat.
A three-compartments dynamical model is defined as below
where \(c(t)=\frac{{x}_{1}(t)}{{V}_{c}}\), Vc is the volume of the central compartment (about 15 \(\ell \) for a 70-kg patient), aij(c), i ≠ j, is the rate of transfer of drug from the jth to the ith compartment, a11(c) is the rate of drug metabolism and elimination (metabolism typically occurs in the liver), and u(t), t > 0, is the infusion rate of the sedative drug propofol into the central compartment. The transfer coefficients are assumed to be functions of the drug concentration c since it is well known that the pharmacokinetics of propofol are influenced by cardiac output23 and, in turn, cardiac output is influenced by propofol plasma concentrations, both due to venodilation24 and myocardial depression25.
Experimental data indicate that the transfer coefficients aij(⋅) are nonincreasing functions of the propofol concentration24,25.
The most widely used empirical models for pharmacodynamic concentration-effect relationships are modifications of the Hill equation26. Applying this almost ubiquitous empirical model to the relationship between transfer coefficients implies that
where, for i, j ∈ {1, 2, 3}, i ≠ j, \({\tilde{C}}_{50,ij}\) is the drug concentration associated with a 50% decrease in the transfer coefficient, αij is a parameter that determines the steepness of the concentration-effect relationship, and Aij are positive constants. It is to be noted that both pharmacokinetic parameters are functions of i and j, that is, there are distinct Hill equations for each transfer coefficient. Furthermore, since for many drugs the rate of metabolism a11(c) is proportional to the rate of transport of drug to the liver, we assume that a11(c) is also proportional to the cardiac output so that a11(c) = A11Q11(c).
Evaluating the Performance of the Personalized Pharmacokinetic Framework for Dosing of Propofol
In this section, we apply the presented framework to predict the pharmacokinetic response of a patient to propofol.
Identifying the parameters of patients in the archived dataset
First, we use data reported in15 and16, where plasma concentrations from arterial samples were collected from 59 adult volunteers (age 23–82 and weight 57–114 kg). Subjects received a propofol infusion of 0.5 mcg/kg/min for an average time of 8 minutes. Times at which blood sampling was performed varied across subjects. However, approximately 17 samples were collected from t = 0 to t = 100 min from all subjects. In addition, depending on the subject’s condition, between 0 to 10 extra samples were collected from subjects after t = 100 min.
As a first step, pharmacokinetic parameters for subjects in the archived dataset were identified using the Levenberg-Marquardt method. Furthermore, since there were variations in total infused propofol among different subjects in the archived dataset, the pharmacokinetic response of each subject in the archived dataset was updated using the drug dose of the new patient.
Using Prior data from the archived dataset to predict pharmacokinetic response
We compare the prediction accuracy of three frameworks: i) the Levenberg-Marquardt (LM) method, where no prior data is available and only typical ranges of pharmacokinetic parameter values are provided; ii) the Cluster Newton (CN) method, where no prior data is available and only typical ranges of pharmacokinetic parameter values are provided; and iii) the Constrained Cluster Newton (CCN) method, where data from prior patients are available.
In order to initialize the LM and CN methods, a cluster of 500 points is generated to be used by the optimization algorithms, where the cluster is chosen from the range given by typical values of the pharmacokinetic parameters reported in the literature22,27. The parameters are assumed to be distributed in a normal distribution with the mean values centered as A11Q0 = 0.119, A21Q0 = 0.112, A12Q0 = 0.055, A31Q0 = 0.0419, A13Q0 = 0.0033, and Vc = 15.96. The standard deviation of these values are std(A11Q0) = 0.0351, std(A21Q0) = 0.1051, std(A12Q0) = 0.0458, std(A31Q0) = 0.0155, std(A13Q0) = 0.0013, and std(Vc) = 12.7. In contrast, in the CCN method, the archived dataset is used to generate the cluster of 500 points to initiate the optimization process as discussed in Section 1. In addition, we use both the threshold-based approach (with the threshold set to α = 5) and the nearest neighbor-based approach (with n set to 20) to solve the parameter identification problem, namely CCN(th) and CCN(nn), respectively.
Evaluation of the proposed method
We use a leave-one-subject-out method, where data from 58 patients are assigned to the archived dataset and the remaining one patient is considered as a new patient. This process was repeated 59 times so that each subject in the dataset was considered as the new patient and all the others were assigned to the archived dataset. In the end, all results were aggregated. To solve the personalized pharmacokinetic problem, we assumed that drug concentration in plasma for the new patient is only available at one time instant (at approximately t = 3 min depending on the availability of data in the dataset). Our goal was to compare the prediction accuracy of the personalized pharmacokinetic approach with the ground truth established by the available data for each subject not included in the analysis.
In both CN and CCN methods, the optimization was performed for 10 iterations. However, Broyden’s method was not used at the end of each iteration. We used the LM implementation in the MATLAB optimization toolbox (version 2018)28. In the LM method, the optimization was terminated when the last step was smaller than the function tolerance of 10−6 or when the number of iterations was larger than 40029. To compare the pharmacokinetic prediction accuracy of each method, the following performance metrics were used: (i) peak concentration of the drug in the first 100 minutes denoted by Cmax, (ii) time to maximum concentration Cmax denoted by tmax, (iii) half-life defined as time to half Cmax denoted by thalf, and (iv) area under the curve (AUC) obtained by integration of the concentration-time curve. Here, we consider the area of a single-dose curve from time 0 to 100 minutes given by
where y(t) represents the concentration-time relationship.
All metrics are reported as absolute percentage errors (APE) by comparing the estimated values to the available ground truth. The performance metrics for LM and CN methods were compared to the proposed CCN methods (both the threshold-based and the nearest neighbor approaches).
Figure 4 illustrates the error values of the results from all methods. The values in Fig. 4(a–d) are presented in the average APE ± standard deviation. It can be seen that the errors from the CCN method are smaller than the values from the CN and LM methods for most of the metrics regardless of the specific subject selection method used in CCN (nearest neighbor or threshold-based). In addition, the conventional CN method shows better results in average APE in Cmax, thalf, and AUC0−100 compared to the conventional LM method. This result matches the observation in3 and can be explained by the fact that the CN method uses multiple sets of initial points, whereas the LM method solves the inverse problem with only one set of initial points. This improves the accuracy of the estimation from CN method.
Comparison of the leave-out validation results in (a) absolute percentage error (APE) of the maximum concentration Cmax; (b) APE of the time to the maximum concentration tmax; (c) APE of the half-life thalf; (d) APE of the area under the curve AUC0−100. (Bar: average, Error Bar: standard deviation).
Detailed results are given in Table 1. The threshold-based CCN, that is, CCN(th), gives a better performance in comparison to nearest-neighbor-based CCN method, that is, CCN(nn), regarding Cmax (7.03% in comparison to 7.71%) and thalf (7.69% compared to 16.89%). However, CCN(nn) shows better performances compared to CCN(th) in tmax and AUC0–100, reporting 8.67% versus 11.06% and 20.39% versus 22.62%, respectively. Taking the average of the four APEs, CCN(th) shows a better value of 12.10% ± 6.79% compared to 13.42% ± 7.72% from CCN(nn).
In summary, the proposed CCN method for personalized pharmacokinetics provides a more accurate prediction of pharmacokinetic response based on the performance metrics defined above. Although CCN(th) shows better overall performance in terms of the average APE of the four metrics in Table 1, it is superior to CCN(nn) only in two out of the four metrics. Therefore, we can deduce that the performances of both CCN(th) and CCN(nn) are comparable.
Reducing Computation Time through Parallel Computing
In order to utilize a personalized pharmacokinetic framework in a clinical setting, minimal computation time is critical. One limitation of using traditional methods such as Levenberg-Marquardt (LM) is that the computational structure is not well-suited for a parallel computing framework, leading to long computation times of hours and days. One attractive property of the newly-developed Constrained Cluster Newton method compared to LM is that it possesses the appropriate architecture for running the algorithm on multiple processors. Specifically, the process involves solving a number of independent forward solutions to ODEs, and then, updating the parameters. Each independent forward solution corresponds to a point randomly sampled from the initialization region. Running the program on multiple CPUs significantly reduces the computation time as discussed below.
To address the computational inefficiency of the numerical method, the computational bottleneck needs to be identified. Our analysis showed that more than 90% of the total computation time is dedicated to solve the ODEs. However, the CCN method involves independent solution to multiple ODEs, and hence, they can be solved in parallel. We used a workstation with 2 Intel Xeon CPU E5-2650 at 2.00 GHz (8 core 16 threads) running MATLAB to solve the parameter identification method using CCN. The workstation allows MATLAB to use a maximum of 12 workers in a parallel pool. A worker, defined under the MATLAB environment, is a processing thread that can be used for parallel calculation tasks. The MATLAB program manages workers by aggregating them into a pool. The workers in the pool can be used interactively and communicate with each other during the parameter identification task. The major parallel computation load is the ‘parfor’ function of the code, which is used to forward-solve the ODEs in the pharmacokinetic model.
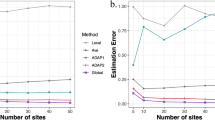
During the test, both the CCN(nn) and the CCN(th) methods are executed with 59 subjects and 10 iterations for each observation (590 iterations in total). The same test is evaluated with 1, 2, 4, 6, 8, 10, and 12 workers. The results are shown in Fig. 5. The total computation time from the CCN(th) method with one worker is 773.14 seconds. The average computation time of one subject is 13.10 seconds. The time significantly drops to 375.84 seconds in total and 6.37 seconds on average when we have two workers working in parallel. The benefit from increasing the number of workers decreases slightly as we change from 2 workers to 4, 6, 8, 10, and 12 workers with reported total times of 185.61, 159.50, 109.04, 98.60, 91.06 seconds, respectively. Furthermore, the average computation time of the estimation from one subject with 4, 6, 8, 10, and 12 workers is 3.15, 2.69, 1.85, 1.67, and 1.54 seconds.
Alternatively, the total computation time from the CCN(nn) method with one worker is 752.26 seconds with an average of 12.75 seconds per subject. The computation time decreases to 391.51 seconds and the average computation time is reduced to 6.64 seconds when 2 workers are used. The computation time continues to drop as the number of workers increases. As illustrated in Fig. 5, the total computation time is 209.96, 146.74, 104.41, 102.08, and 89.32 seconds with 4, 6, 8, 10, and 12 workers, respectively. On average, the computation time for one subject is 3.56 seconds with 4 workers, 2.49 seconds with 6 workers, 1.77 seconds with 8 workers, 1.73 seconds with 10 workers, and 1.51 seconds with 12 workers.
It can be observed that both the CCN(nn) and CCN(th) methods received significant benefits when the worker numbers are increased from one to two. Both methods also reveal a similar trend of receiving less significant improvements from the increased number of workers when more than two workers are involved. For instance, the average computation time from CCN(nn) with 1 worker is 13.10 seconds. This value is reduced to 1.54 seconds with 12 workers, with an improvement ratio of 8.50 (13.10/1.54). However, this ratio is lower than the worker ratio of 12 (12/1). By segmenting the computation time into detailed algorithm components, we observed that the scheduling and distribution of the parallel calculation tasks are the major reason that the benefit from parallel computing becomes less significant for a larger number of workers. The ratio of worker management time to total computation time is higher for a larger number of workers. Finally, it was also observed that the computation time of the LM method is much higher than the CCN method with the same initial points, reporting more than 7400 seconds for the LM method versus 13.10 seconds from the CCN(nn) method.
Discussion and Conclusion
In this paper, we presented a framework for fast parameter identification for personalized pharmacokinetic applications. Our numerical experiments validate the feasibility of this framework to improve the accuracy of pharmacokinetic parameter estimations with limited observations. The best overall performance is achieved with the constrained Cluster Newton method (CCN) employing a threshold strategy. Experimental results also indicate that it is beneficial to apply parallel computing to the CCN method.
In future research, we will evaluate the sensitivity of the algorithm to dosage variations and improve the robustness of the algorithm. Extensive tests with other pharmacokinetic models will also be conducted to evaluate the model-dependency of the algorithm. One limitation of this study is that the database is relatively small. In our future studies, we will evaluate the performance of the algorithm with a larger database. Another limitation is that our framework requires a high number of samplings in the archived dataset. This will ensure that the dynamics of the new patient can be adequately characterized by the proposed least-squares-based approach. In our future studies, we will investigate the effects of an increase or a decrease in the sampling density on the performance of the framework.
To achieve fast computation, more workers are needed. Implementation of the proposed framework on Graphic Processing Units (GPU) could be beneficial in this regard, as ODE implementation is reported to be 65 times faster on GPU than on CPU30. This will reduce the response time to the level of milli-seconds per estimation task, pushing forward this research to practical applications.
Data Availability
The datasets generated during and/or analysed during the current study are available in the OPENTCI repository, http://opentci.org/data/propofol.
References
Bailey, J. M. & Haddad, W. M. Drug dosing control in clinical pharamacology: Paradigms, benefits, and challenges. Contr. Sys. Mag. 25, 35–51 (2005).
Yoshida, K., Maeda, K., Kusuhara, H. & Konagaya, A. Estimation of feasible solution space using cluster newton method: Application to pharmacokinetic analysis of irinotecan with physiologically-based pharmacokinetic models. BMC Syst. Biol. 7, S3, https://doi.org/10.1186/1752-0509-7-S3-S3 (2013).
Aoki, Y., Hayami, K., Sterck, H. D. & Konagaya, A. Cluster newton method for sampling multiple solutions of underdetermined inverse problems: Application to a parameter identification problem in pharmacokinetics. SIAM J. on Sci. Comput. 36, B14–B44 (2014).
Holford, N. H. Target concentration intervention: beyond y2k. Br. journal clinical pharmacology 48, 9–13 (1999).
Maitre, P. O. & Stanski, D. R. Bayesian forecasting improves the prediction of intraoperative plasma concentrations of alfentanil. Anesthesiology 69, 652–659 (1988).
Matthews, I., Kirkpatrick, C. & Holford, N. Quantitative justification for target concentration intervention–parameter variability and predictive performance using population pharmacokinetic models for aminoglycosides. Br. journal clinical pharmacology 58, 8–19 (2004).
Wright, D. F. & Duffull, S. B. Development of a bayesian forecasting method for warfarin dose individualisation. Pharm. research 28, 1100–1111 (2011).
Hope, W. W. et al. Software for dosage individualization of voriconazole for immunocompromised patients. Antimicrob. agents chemotherapy 57, 1888–1894 (2013).
Kumar, A. A. et al. An evaluation of the user-friendliness of bayesian forecasting programs in a clinical setting. Br. journal clinical pharmacology (2019).
Prueksaritanont, T. et al. Drug–drug interaction studies: regulatory guidance and an industry perspective. The AAPS journal 15, 629–645 (2013).
Schüttler, J. & Ihmsen, H. Population pharmacokinetics of propofola multicenter study. Anesthesiol. The. J. Am. Soc. Anesthesiol. 92, 727–738 (2000).
Zhao, P. et al. Applications of physiologically based pharmacokinetic (pbpk) modeling and simulation during regulatory review. Clin Pharmacol Ther 89, https://doi.org/10.1038/clpt.2010.298 (2011).
Arikuma, T. et al. Drug interaction prediction using ontology-driven hypothetical assertion framework for pathway generation followed by numerical simulation. BMC bioinformatics 9, S11 (2008).
Hamburg, M. A. & Collins, F. S. The path to personalized medicine. New Engl. J. Medicine 363, 301–304 (2010).
Coetzee, J. et al. Pharmacokinetic model selection for target controlled infusions of propofolassessment of three parameter sets. Anesthesiol. The J. Am. Soc. Anesthesiol. 82, 1328–1345 (1995).
Dyck, J. & Shafer, S. Effects of age on propofol pharmacokinetics. In Seminars in anesthesia, vol. 11, 2–4 (Saunders, 1992).
Haddad, W. M., Chellaboina, V. & Hui, Q. Nonnegative and Compartmental Dynamical Systems (Princeton University Press, Princeton, NJ, 2010).
Aster, R. C., Borchers, B. & Thurber, C. H. Parameter Estimation and Inverse Problems (Elsevier, 2018).
Hanke, M. A regularizing levenberg-marquardt scheme, with applications to inverse groundwater filtration problems. Inverse problems 13, 79 (1997).
Asami, S., Kiga, D. & Konagaya, A. Constraint-based perturbation analysis with cluster newton method: A case study of personalized parameter estimations with irinotecan whole-body physiologically based pharmacokinetic model. BMC systems biology 11, 129 (2017).
Gholami, B., Haddad, W. M., Bailey, J. M. & Tannenbaum, A. R. Optimal drug dosing control for intensive care unit sedation by using a hybrid deterministic-stochastic pharmacokinetic and pharmacodynamic model. Opt. Contr. Appl. Meth. 59, 423–436 (2013).
Marsh, B., White, M., Morton, N. & Kenny, G. N. Pharmacokinetic model driven infusion of propofol in children. Brit. J. Anaesth. 67, 41–48 (1991).
Upton, R. N., Ludrook, G. I., Grant, C. & Martinez, A. Cardiac output is a determinant of the initial concentration of propofol after short-term administration. Anesth. Analg. 89, 545–552 (1999).
Muzi, M., Berens, R. A., Kampine, J. P. & Ebert, T. J. Venodilation contributes to propofol-mediated hypotension in humans. Anesth. Analg. 74, 877–883 (1992).
Ismail, E. F., Kim, S. J. & Salem, M. R. Direct effects of propofol on myocardial contractility in situ canine hearts. Anesthesiology 79, 964–972 (1992).
Hill, A. V. The possible effects of the aggregation of the molecules of haemoglobin on its dissociation curves. J. Physiol. 40, iv–vii (1910).
Eleveld, D. J., Proost, J. H., Cortínez, L. I., Absalom, A. R. & Struys, M. M. A general purpose pharmacokinetic model for propofol. Anesth. & Analg. 118, 1221–1237 (2014).
Moré, J. J. The levenberg-marquardt algorithm: implementation and theory. In Numerical analysis, 105–116 (Springer, 1978).
Shampine, L. F. & Reichelt, M. W. The matlab ode suite. SIAM journal on scientific computing 18, 1–22 (1997).
Niemeyer, K. E. & Sung, C.-J. Accelerating moderately stiff chemical kinetics in reactive-flow simulations using gpus. J. Comput. Phys. 256, 854–871 (2014).
Acknowledgements
This work was supported by the US Army Medical Research and Materiel Command under Contract No. W81XWH-18-C-0013. The views, opinions and/or findings contained in this report are those of the authors and should not be construed as an official Department of the Army position, policy or decision unless so designated by other documentation.
Author information
Authors and Affiliations
Contributions
C.Y. developed the algorithm. N.T., W.M.H., J.M.B. and B.G. conceived the framework design. All authors drafted the manuscript collaboratively. C.Y., N.T. and B.G. analyzed the results. All authors provided scientific insight and reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
C.Y., N.T., W.M.H., J.M.B., B.G. declare that they have no non-financial competing interests. B.G. and W.M.H. have stock ownership in Autonomous Healthcare, Inc. J.M.B. has stock options in Autonomous Healthcare and serves as its Chief Medical Officer.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yang, C., Tavassolian, N., Haddad, W.M. et al. A Fast Parameter Identification Framework for Personalized Pharmacokinetics. Sci Rep 9, 14143 (2019). https://doi.org/10.1038/s41598-019-50810-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-50810-z
This article is cited by
-
Transcriptomics: illuminating the molecular landscape of vegetable crops: a review
Journal of Plant Biochemistry and Biotechnology (2024)
-
A hybrid modeling approach for assessing mechanistic models of small molecule partitioning in vivo using a machine learning-integrated modeling platform
Scientific Reports (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.