Abstract
Fibrosis across different organs and tissues is likely to share common pathophysiological mechanisms and pathways. Recently, a polymorphism (rs12979860) near the interferon lambda gene (IFNL3) was shown to be associated with fibrosis in liver across multiple disease etiologies. We determined whether this variant is a risk factor for pulmonary fibrosis (PF) and worsening cutaneous fibrosis in systemic sclerosis (SSc). Caucasian patients with SSc (n = 733) were genotyped to test for association with the presence of PF and worsening of skin fibrosis. Serum IFN-λ3 levels from 200 SSc cases were evaluated. An association of the IFNL3 polymorphism with PF was demonstrated (OR: 1.66 (95% CI: 1.142–2.416, p = 0.008). The IFNL3 variant was not a risk factor for worsening of skin fibrosis. Functionally, IFN-λ3 serum levels were higher among subjects with PF compared to those unaffected (P < 0.0001). In conclusion, IFNL3 serum levels and the genetic variant known to be associated with liver fibrosis are similarly linked to PF, but not to worsening of skin fibrosis in SSc. These data highlight both common fibrosis pathways operating between organs, as well as differential effects within the same disease.
Similar content being viewed by others
Introduction
Despite contributing up to 45% of deaths in the developed world, fibrotic diseases have largely been overlooked from the perspective of a shared phenotype1. In this regard, organs such as lung, liver, skin, and kidney, while possessing unique tissue-specific fibrosis features, are likely to share common core and regulatory pathways. Hence, a multi-organ approach was recently suggested to identify druggable targets for generic anti-fibrotic therapies1.
Systemic sclerosis (scleroderma, SSc) is a complex autoimmune disease characterized by fibrosis in skin and internal organs, immune dysregulation, and vasculopathy that is associated with a high morbidity and mortality. A hallmark of SSc is clinical and inter-individual heterogeneity2. Though the pathogenesis of SSc remains poorly understood, there is accumulating evidence suggesting that at least in part, genetic factors are involved2.
Pulmonary fibrosis (PF) (interstitial lung disease; ILD) is a leading cause of morbidity and mortality in patients with SSc3. As new treatments become available or are developed for SSc-associated PF and other forms of PF, early identification of high-risk patients is paramount for early intervention and through this, improved clinical outcomes3. Unfortunately, reliable predictors of who will develop PF among those with scleroderma are not available. Genetic variants that might contribute to more severe fibrosis and/or progression could fill this need, as they do not fluctuate over the course of disease and are not time-dependent. Hence these variants are attractive candidates for the development of biomarkers predictive of progression and for risk stratification. The latter is also pivotal for personalization of therapy, and for improving clinical trial design for new therapies2.
We and others recently reported that single nucleotide polymorphisms (SNPs) in the interferon lambda (IFNL, a type III interferon) 3 region originally discovered through genome-wide association studies (GWAS) as a predictor of hepatitis C virus (HCV) clearance, are a strong predictor of the risk for fibrosis risk across multiple liver diseases4,5,6. IFNL receptors have restricted expression to epithelial tissues including lung and liver and thus respond to type III IFNs7. Thus, it is plausible that genetic variants in the IFNL3 locus could also affect PF risk. A key difference between idiopathic pulmonary fibrosis (IPF) and SSc-associated PF is the role of inflammation. Inflammation is thought to play a role in SSc-associated PF2 but this remains less clear for IPF. In this study, we evaluated whether there is a link between IFNL3 variants and the risk of skin and pulmonary fibrosis in a large cohort of Caucasian patients with SSc. Functionally, IFNλ-3 levels according to lung fibrosis were also evaluated in human and mice.
Results
Patient characteristics
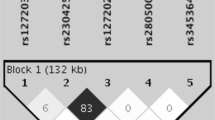
Supplementary Table 1 summarises the main features of the cohort. A total of 733 patients were eligible, of whom 24.5% had PF. Genotyping was successful for all samples except three. The genotype distribution of IFNL3 rs12979860 conformed to Hardy-Weinberg equilibrium and the minor allele frequency (MAF) was 0.316, similar to that observed in a healthy Caucasian population from the 1000 genome project (http://browser.1000genomes.org). Hence, suggestive that IFNL3 rs12979860 is not associated with SSc susceptibility.
IFNL3 rs12979860 and pulmonary fibrosis
The major IFNL3 rs12979860 CC genotype previously associated with liver fibrosis was present at a significantly higher frequency in SSc patients with pulmonary fibrosis compared to those without (29% vs 21%, OR: 1.51 (95% CI: 1.077–2.119, p = 0.01). In multiple logistic regression analysis adjusting for age, gender, baseline disease duration and baseline modified Rodnan skin thickness score (mRSS), IFNL3 rs12979860 CC genotype remained independently associated with the risk of PF (OR: 1.66 (95% CI: 1.142–2.416, p = 0.008). No difference in disease duration was observed between subjects with and without PF or according to IFNL3 genotype (9.46 (3.2–17.36) vs 8.63 (2.46–18.45), p = 0.6 and (6.7 (1.93–17.6) vs 7.34 (1.72–14.09), p = 0.9) in subjects with CC and CT/TT genotype, respectively.
IFNL3 rs12979860 and worsening of skin fibrosis
Next, we evaluated the association of IFNL3 rs12979860 with worsening of skin fibrosis within ~1 year of study enrolment (follow-up time of 1.07 (0.99–1.36) years). In the overall cohort (only 632 patients had follow-up mRSS recorded). There was no significant association between rs12979860 genotype and worsening of skin fibrosis within 1 year (OR: 0.938, 95% CI: 0.543–1.619, p = 0.8). A similar result was obtained when a Cox proportional-hazards regression model was applied after adjustment for age, sex and baseline disease duration (adjusted HR for time to mRSS > 5: 0.934, 95% CI: 0.458–1.591, p = 0.8). In three further analyses, we considered only subjects with mRSS ≥ 7 (n = 316) at first visit. This cut-off was chosen based on previous reports8, that it represents the lowest value required to be considered as diffuse cutaneous systemic sclerosis (dcSSc). In this analysis, rs12979860 had no impact on the risk of worsening of skin fibrosis (OR: 1.13, 95% CI: 0.505–2.531, p = 0.7). In the second analysis conducted in subjects with diffuse SSc (n = 155), rs12979860 again demonstrated no association with the risk of worsening of skin fibrosis. Finally, in a third analysis restricted to subjects with early disease (that is, baseline disease duration shorter than 5 years) (n = 179), IFNL3 rs12979860 was again not associated with the extent of skin involvement (diffuse vs. limited) or baseline mRSS. No association was observed between IFNL3 genotype and autoantibody status, namely anti-topoisomerase antibody (anti-Scl-70), anti-centromere antibodies or anti-RNA polymerase III (data not shown).
Serum IFN-λ3 levels
We recently showed that IFN-λ3 but not IFN-λ4 mediates the IFNL3/IFNL4 haplotype dependent association with liver inflammation and fibrosis9. Hence, to further explore the functional relevance of rs12979860, we evaluated serum IFNλ-3 levels in 200 cases with SSc. As expected and consistent with our hypothesis, IFN-λ3 protein levels were 10 times as high among subjects with PF as among those unaffected by PF (P < 0.0001) (Fig. 1). Importantly, this difference remained significant even after stratification according to rs12979860 genotype (Supplementary Figure 1). Subjects who were homozygous for the major allele have higher serum IFN-λ3 levels compared to those carrying at least one copy of the minor allele in the entire ELISA sub-cohort (median 23.48 (4.28–77.5) vs. 18.35 (4.44–68.3), p = 0.2) and after stratification according to patients with and without pulmonary fibrosis), but this was not significant (Supplementary Figure 2). Notably, 62 (31%) of these patients received one or more immunosuppressive agents. Thus, we examined whether immunosuppressive agents have any effect on IFN-λ3 levels. In this analysis, there was no association between use of immunosuppressive drugs and serum IFN-λ3 levels (median 23.84 (4.29–70.26) vs. 14.2 (4.32–78), p = ns) or between type of immunosuppressive agent when assessed separately. The association between PF and IFN-λ3 levels remained significant after adjusting for the use of immunosuppressive agents (OR = 1.01, 95% CI: 1.004–1.015, p = 0.0001).
Quantification of IFNλ3 using a highly sensitive chemiluminescent enzyme immunoassay in human serum samples. The levels of IFNλ3 were measured in 200 patients with SSc by a chemiluminescent enzyme immunoassay relative to the presence or absence of pulmonary fibrosis (PF). The x axis shows pulmonary fibrosis status dichotomized as absent (n = 100) or present (n = 100). The y axis shows serum IFNλ3 levels as pg/mL. The number of independent samples tested in each group is shown in parentheses. Each group is shown as a box plot and the median values are shown as thick dark horizontal lines. The box covers the twenty-fifth to seventy-fifth percentiles. We tested the difference in median values among genotypes using the two-tailed Mann–Whitney test and plotted the box plots using Graph pad prism 7.
Ifnl3 expression in bleomycin-induced pulmonary fibrosis
To further investigate the role of IFNL3 in lung fibrosis, we examined Ifnl3 mRNA expression in mice with lung fibrosis induced by bleomycin using ddPCR. Consistent with the human data, Ifnl3 mRNA expression in bleomycin treated mice was significantly higher than that in the control group (P < 0.05) (Fig. 2).
Discussion
In this study, we demonstrate an association of genetic variants around the IFNL3 locus with an increased risk of SSc-associated PF, but not with the extent or worsening of skin fibrosis. Furthermore, IFN-λ3 serum levels were higher in subjects with PF compared to unaffected patients, including when stratified by IFNL3 genotype and in the lungs of mice with bleomycin-induced pulmonary fibrosis. Collectively, our findings in concert with earlier reports on the risk of fibrosis across multiple liver diseases4,5, suggest that IFNL3 is a core regulatory fibrotic pathway.
The functional mechanisms for the IFNL3 association with fibrosis generally and PF in particular, remain elusive. There is mounting evidence supporting a role for IFNL in the control of inflammation in response to viral and bacterial infections of epithelial tissues, including of the liver, the gastrointestinal tract and lung7. Thus, it is conceivable that IFNL, through its contribution to tissue inflammation that is well-known to be present in the lungs of patients with SSc and PF2, modulates the progression of pulmonary disease. Support for a role for IFNL in PF can be extrapolated from other published reports. For example, a recent report showed higher serum IFNL1 levels in patients with SSc compared to healthy controls (11). Further, a variant in the interferon regulator factor-5 (IRF5) gene, a transcription factor relevant to the expression of type Ι and Ш interferons was discovered by GWAS as a susceptibility variant for SSc10. This was shown later to be associated with better preservation of lung function, milder interstitial lung involvement and longer survival11. The protective allele of this variant (rs4728142) results in reduced IRF5 transcript levels and presumably IFNL transcription. Consistently, attempts to treat patients with SSc with another IFN (IFN-α) resulted in a substantial worsening of lung disease12.
From a clinical perspective, the present findings if further independently replicated, would suggest that IFNL3 variant testing (either alone or as part of a polygenic risk score) and subsequent risk stratification, could be part of the counselling of patients with SSc who develop PF. From a translational standpoint, there are ongoing efforts to test the safety and efficacy of IFN-α blockade, such as anti-IFN-α receptor monoclonal antibody therapy for the management of SSc13. However, due to the restricted expression of IFNL receptors compared to the ubiquitous expression of IFN-α14, IFNL blockade could be a more attractive therapeutic target, especially for SSc-associated lung disease.
In this study, IFNL3 genotype had no impact on the prediction of progressive skin fibrosis in the overall cohort or in the subset with diffuse SSc. As the ASCS cohort is not an inception cohort, the majority of subjects had long disease duration. Since it is well-known that skin thickening progresses more rapidly in early than late disease2, we are not able to totally exclude the possibility that inclusion of subjects with longer disease duration might have limited our ability to observe an effect of IFNL3 genotype on worsening of skin fibrosis. However, our sensitivity analysis in subjects with early disease duration did not show a trend for the association, which argues against this possibility.
The current study has strengths and limitations. The data were derived from a large well-characterised multicenter prospective cohort showing the typical features of SSc with extensive clinical data and disease characteristics. Furthermore, the ASCS-derived dataset enabled analysis of worsening skin fibrosis over a median 12 months follow-up. The latter is widely considered ideal to detect meaningful changes and is used in clinical trials8. Limitations of this study include the lack of a replication cohort for the positive association observed with PF, the number of patients with full auto-antibody profiles, and the fact that it was not an inception cohort. Nevertheless, the associations we observed are similar to those previously demonstrated for liver in large independently-replicated cohorts (>4000 and 1300 patients)4,5. Further studies will be required to address the impact of IFN-λ3, as well as IFNL3 genetic variation on ILD severity and progression in cohorts of incident patients followed prospectively with multiple HRCTs, and to clarify the functional mechanisms of this genetic association.
In conclusion, we demonstrate that the IFNL3 genetic variant and serum levels of IFNλ-3 are significantly associated with the risk of PF in a Caucasian population with SSc. The IFNL3 variant was not a risk factor for the worsening of skin fibrosis. Consistently, Ifnl3 mRNA expression was higher in lungs from mice with bleomycin-induced pulmonary fibrosis. The functional mechanisms for the pro-fibrotic effects of IFNL3 will require further investigation and if confirmed, can be exploited as a potentially more effective therapeutic target.
Methods
Patient cohort
The study comprised 733 consecutive Caucasian patients with SSc from the Australian Scleroderma Cohort Study (ASCS), a multi-center prospective study of risk factors for clinically important outcomes in SSc. All patients fulfilled either American College of Rheumatology or Leroy and Medsger criteria for SSc14. The study protocol was conformed to the ethical guidelines of the 1975 Declaration of Helsinki. Each of the participating centres obtained approval for the study from their respective ethics committees and study was performed according to the recommendations of the centers involved. The ASCS compromises 13 Australian centres and has been approved by the human research ethics committee of each of the participating hospitals (St. Vincent’s Hospital, Melbourne Royal Adelaide Hospital, Monash Medical Centre, Royal Perth Hospital, The Queen Elizabeth Hospital, Sunshine Coast Rheumatology, Prince Charles Hospital, John Hunter Hospital, Royal North Shore Hospital, Royal Prince Alfred Hospital, St George Hospital, Canberra Rheumatology and the University of Tasmania). Written informed consent for genetic testing was obtained from all participants. Details of the methods for pulmonary disease assessment, skin fibrosis progression assessment, genotyping, IFN-λ3 serum levels measurement, and the mouse model is provided in Supplementary Methods.
Statistical analysis
The Student’s t-test, Mann-Whitney test, Wilcoxon’s test and Fisher’s exact tests were used, as appropriate. Multiple logistic and Cox proportional-hazards regression models were fitted adjusting for common risk factors as covariates. The IFNL3 rs12979860 genotype was dichotomized as CC versus CT/TT, as previously reported4,15.
References
Friedman, S. L., Sheppard, D., Duffield, J. S. & Violette, S. Therapy for fibrotic diseases: nearing the starting line. Sci Transl Med 5, 167sr1 (2013).
Gabrielli, A., Avvedimento, E. V. & Krieg, T. Scleroderma. N Engl J Med 360, 1989–2003 (2009).
Elhai, M., Meune, C., Avouac, J., Kahan, A. & Allanore, Y. Trends in mortality in patients with systemic sclerosis over 40 years: a systematic review and meta-analysis of cohort studies. Rheumatology (Oxford) 51, 1017–26 (2012).
Eslam, M. et al. Interferon-lambda rs12979860 genotype and liver fibrosis in viral and non-viral chronic liver disease. Nat Commun 6, 6422 (2015).
Bochud, P. Y. et al. IL28B alleles associated with poor hepatitis C virus (HCV) clearance protect against inflammation and fibrosis in patients infected with non-1 HCV genotypes. Hepatology 55, 384–94 (2012).
Eslam M, et al. FibroGENE: A gene-based model for staging liver fibrosis. J Hepatol. 64(2), 390–398 (2016).
Eslam, M. & George, J. Genome-Wide Association Studies and Hepatitis C: Harvesting the Benefits of the Genomic Revolution. Semin Liver Dis 35, 402–20 (2015).
Dobrota, R. et al. Prediction of improvement in skin fibrosis in diffuse cutaneous systemic sclerosis: a EUSTAR analysis. Ann Rheum Dis 75, 1743–8 (2016).
Eslam, M. et al. IFN-lambda3, not IFN-lambda4, likely mediates IFNL3-IFNL4 haplotype-dependent hepatic inflammation and fibrosis. Nat Genet 49, 795–800 (2017).
Radstake, T. R. D. J. et al. Genome-wide association study of systemic sclerosis identifies CD247 as a new susceptibility locus. Nature Genetics 42, 426–U71 (2010).
Sharif, R. et al. IRF5 polymorphism predicts prognosis in patients with systemic sclerosis. Ann Rheum Dis 71, 1197–202 (2012).
Spagnolo, P. et al. Non-steroid agents for idiopathic pulmonary fibrosis. Cochrane Database Syst Rev, CD003134 (2010).
Goldberg, A. et al. Dose-escalation of human anti-interferon-alpha receptor monoclonal antibody MEDI-546 in subjects with systemic sclerosis: a phase 1, multicenter, open label study. Arthritis Res Ther 16, R57 (2014).
Preliminary criteria for the classification of systemic sclerosis (scleroderma). Subcommittee for scleroderma criteria of the American Rheumatism Association Diagnostic and Therapeutic Criteria Committee. Arthritis Rheum 23, 581–90 (1980).
Bochud, P. Y. et al. IL28B polymorphisms predict reduction of HCV RNA from the first day of therapy in chronic hepatitis C. Journal of Hepatology 55, 980–988 (2011).
Acknowledgements
We would like to thank all the patients for their participation in this study. ME and JG are supported by the Robert W. Storr Bequest to the Sydney Medical Foundation, University of Sydney, a National Health and Medical Research Council of Australia (NHMRC) Program Grant (1053206), Project grants (APP1107178 and APP1108422). MN is supported by an NHMRC Fellowship (APP1071735).
Author information
Authors and Affiliations
Contributions
M.M., M.E., J.G. conceived the research. Enrolling of patients, clinical phenotype, data collation and sample acquisition/DNA preparation, genotyping, IFNL3 ELISA, RNA Extraction, ddPCR and critical analysis was performed by M.M., K.T., A.B., M.N., W.S., J.S., J.Z., J.R., K.T., G.S., S.L., M.R., G.S.N., J.W., P.H., O.S., C.L., N.M., L.B., S.M.P., J.G., M.E. The manuscript was principally written and revised by M.M., M.E and J.G. All authors critically reviewed the manuscript for important intellectual content and approved the final submitted manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Metwally, M., Thabet, K., Bayoumi, A. et al. IFNL3 genotype is associated with pulmonary fibrosis in patients with systemic sclerosis. Sci Rep 9, 14834 (2019). https://doi.org/10.1038/s41598-019-50709-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-50709-9
This article is cited by
-
Association between endothelin-1 and systemic lupus erythematosus: insights from a case–control study
Scientific Reports (2023)
-
The role of IFNL4 in liver inflammation and progression of fibrosis
Genes & Immunity (2022)
-
Interferon lambda in inflammation and autoimmune rheumatic diseases
Nature Reviews Rheumatology (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.