Abstract
Technical guidelines for magnetic resonance imaging (MRI) of the small bowel (SB) in the setting of inflammatory bowel diseases (IBDs) were detailed in a 2017 consensus issued by European Society of Gastrointestinal and Abdominal Radiology (ESGAR) and European Society of Pediatric Radiology (ESPR); however, MRI for non-IBD conditions was not addressed. Hence, we performed a systematic review collecting researches on SB MRI for non-IBDs. The literatures were then divided into morphologic group and functional group. Information about the MRI techniques, gastrointestinal preparation, and details of cine-MRI protocols was extracted. We found that a 1.5 T MRI system, prone positioning, and MR enterography were frequently utilized in clinical practice. Gadolinium contrast sequences were routinely implemented, while diffusion-weighted imaging (DWI) was much less performed. The gastrointestinal preparation varied throughout the studies. No uniform protocols for cine imaging could be established. SB MRI examinations for non-IBDs are far from standardized, especially for functional studies. Recommendations for standard parameters in cine-MRI sequences are difficult to make due to lack of evidentiary support. MRI investigations in non-IBD conditions are needed and the standardization of non-IBD imaging in clinical practice is required.
Similar content being viewed by others
Introduction
Magnetic resonance enterography (MRE) or enteroclysis is an ideal technique to image the small bowel1. Cine-MRI is a helpful supplement to MRE as it provides a noninvasive way to access the global motility of small bowel (SB)2. Diffusion-weighted imaging (DWI) provides a quantitative functional evaluation of the SB without intravenous contrast, thus facilitating its use even in patients with impaired renal function3. MRE and MR enteroclysis have long been used to diagnose inflammatory bowel diseases (IBDs), especially Crohn’s disease (CD). The lack of ionizing radiation makes it preferable to CT for this purpose, particularly in patients under 35 who often require multiple scans to assess disease progression4. DWI5,6,7 and contrast-enhanced T1W sequences8,9,10 have been widely utilized to monitor the activity and remission of CD. In distinction, the role of MRE and MR enteroclysis in non–IBD conditions such as neoplasm, SB obstruction, diverticular disease, and functional disorders is far less described11.
With the transition toward quantitative imaging and greater demand for multi-center cooperation, medical image standardization has become increasingly important. In 2016, The European Society of Gastrointestinal and Abdominal Radiology (ESGAR) and European Society of Pediatric Radiology (ESPR) released a consensus statement on the technical performance of cross-sectional imaging of IBDs12. Recommendations concerning patient preparation and image acquisition protocols for MRE and MR enteroclysis in the imaging of IBD were made based on the available literature. Although the relationship between MRI image features and pathological features has been studied thoroughly7,13,14,15, further strong evidence on protocol optimization is still needed. The consensus statement highlighted that various protocols and sequences have been utilized to study IBDs with MRE and MR enteroclysis. In this paper, we review original studies on MRE and enteroclysis of non-IBD small bowel disorders in last ten years, including studies performed on healthy volunteers, with the intent of providing a reference for future standardization.
Methods
Literature search
A systematic search for studies focusing on small bowel MRI exclusive of IBDs published from January 2008 to December 2018 was performed. Published articles in English language journals were identified in electronic databases by using MeSH. The search terms were as follows: ‘small intestinal and magnetic resonance imaging not (Crohn disease and inflammatory bowel disease)’. Only original research studies written in English in the past 10 years were included. The search resulted in a total of 374 articles in PubMed Central, 344 in Web of Science and 352 in Medline.
Inclusion criteria and selection process
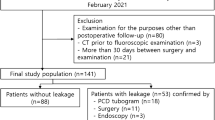
After removing duplicated papers, the remaining 568 papers were initially reviewed by two participants based on article titles and available abstracts. The exclusion criteria were as follows: research focused on Crohn disease, research focused on other IBDs, animal research, and case reports. After the exclusion of 510 papers, the full text of 58 articles was evaluated. 13 additional articles were then excluded as they were found to be clinical or basic science research using MRI as an ancillary tool. In total, 45 articles were included (Fig. 1).
Data extraction
The selected studies were divided into two groups according to the purpose of the research. The morphological group included studies investigating organic small bowel abnormalities and the functional group consisted of those focused on intestinal function. All studies were sorted according to author and year, study population, examination procedures, MR protocols, and other relevant factors.
Results
Examination procedures
The morphological group consisted of 28 articles and the functional group of 17 articles. The sample size examined in both articles was approximately around 30 for both groups (Fig. 2). In the morphological group, the pre-scan fasting time ranged from 4 hours to 8 hours; the functional group was similar, ranging from 4 hours to 9 hours. The interval between small bowel distension and MR acquisition was 0.5 to 1 hour in both groups (Table 1).
MR system and protocol
In the morphological group, 22 studies were conducted using 1.5 T MR scanner, one was conducted using a combination of 1.5 T and 3.0 T and two making a comparison between 1.5 T and 7.0 T. In the functional group, 13 studies were conducted at 1.5 T and 4 studies at 3.0 T. In the group of morphological studies, 23 of the 28 studies adopted contrast-enhanced sequences. Only 5 of the 28 utilized DWI. Ten of the fifteen studies in functional group utilized cine-MRI to assess the small bowel function (Table 2).
Enteric contrast agents
In the morphological group, 96% of the studies distended the small SB before MRI acquisition with enteric contrast. In the functional group, 71% of studies mentioned the use of enteric contrast agents. The most frequently used agents were polyethylene glycol (PEG, n = 12), mannitol hydrosolution (n = 4), and methylcellulose (n = 4) in the morphological group. In functional group, mannitol hydrosolution (n = 7) was the most commonly used enteric contrast agent (Tables 1 and 3).
MR enterography and enteroclysis
In the morphological group, MR enterography was applied in 21 studies while MR enteroclysis was applied in 9 studies. MR enterography was carried out in 13 functional studies. No studies inserted a nasoduodenal catheter under fluoroscopy in the functional group (Table 2). In the morphological group, 900 ml to 2000 ml contrast material was orally administered in the studies carrying out MR enterography while 1000 ml to 3000 ml of enteric contrast agents was administered for MR enteroclysis. In the functional group, 1000 ml to 1350 ml oral administration was used to achieve small bowel distension (Table 1).
A study by Lawrance et al.16 showed equivalent distal small bowel distension and artifacts between MR enteroclysis and MR enterography. In terms of the proximal small bowel, MR enteroclysis achieved a greater degree of distension; however, the diagnostic performance of the two techniques was equal. A previous paper suggested 900 ml of oral contrast agent was sufficient to obtain duodenal distension, and 1350 ml was sufficient to distend the distal jejunum and ileum17.
Position
Prone position was adopted in 12 studies and supine position in 4 studies for the morphological group. In the functional group, 5 studies explicitly mentioned the use of a prone position, while supine position was mentioned in 5 studies (Table 2). In an MR enterography investigation by Cronin et al.18 comparing the two positions, superior small bowel distention was achieved with prone positioning, but this did not result in statistically significant differences in lesion detection. However, in the surveillance of patients with Peutz-Jeghers syndrome (PJS), Maccioni et al.19 found that a combination of supine and prone position was significantly more accurate than supine position alone for the detection of polyps smaller than 15 mm. In cine-MRI studies, prone positioning could limit anteroposterior displacement of SB loops out of the coronal slice and make quantitative motility analyses more reliable20.
Antiperistaltic agents
Four types of antiperistalic agents were mentioned in morphological group. 10–20 mg hyoscine butylbromide or anisodamine (654–2) was prescribed in 16 studies; 4 studies utilized greater than 20 mg hyoscine butylbromide (20–60 mg). Five studies administered 0.5–1.0 mg glucagon to inhibit the peristalsis of small bowel (Table 3). In one study, 0.5 mg tiemonium methylsulphate was administered in place of glucagon in nine patients. According to a review by G. Masselli et al.1, antiperistaltic agents are optimally administered intravenously just before the start of MR examination, and in patients who receive intravenous contrast, a second dose of antiperistaltic agents at the same strength should be given before contrast injection. The role of a sublingual antiperistaltic agent, hyoscyamine sulfate was investigated in one cine-MRI study but the extent of its impact on the evaluation of cine MR enterography is still uncertain21.
Though the additional value of spasmolytic administration to improve image quality of diffusion-weighted sequences has not been evaluated, Elisa et al.22 hypothesized that image quality can be increased by administrating a spasmolytic agent before the DWI MR sequence. However, in one study by Taro23, mean apparent diffusion coefficients (ADCs) before butylscopolamine administration were statistically significantly different from those after butylscopolamine administration.
As antiperistaltic agents were not routinely used for the evaluation of small bowel function, their use was not evaluated in the functional group.
The application of DWI
In the studies by Schmidt24 and Amzallag-Bellenger22, b values of 0 and 800 s/mm2 were used for DWI, while in Low et al.25 a b-value of 500 s/mm2 was utilized. In Plumb et al.26, DWI sequences were obtained with b-values of 0, 50, 150, 300, 600 s/mm2. In a study by Takahara23, DWI with b-values of 0 and 50 s/mm2 was evaluated, and low b-value DWI found useful in distinguishing strangulated from non-strangulated intestinal obstructions. The use of high b values (b >800–1000 sec/mm2) can help negate the high signal intensity of bowel contents and normal bowel mucosa27. Amzallag-Bellenger et al.22 reported significantly increased detection of small bowel tumors by junior radiologists after adding DWI sequences to traditional MRI. All studies included with DWI were performed at 1.5 T.
The application of DWI to intestinal neoplasms could provide useful information about TNM stage and treatment response27. In a comparative study by Wong28, DWI was found to be comparable to PET/CT in diagnosis and treatment response evaluation in patients with gastrointestinal stromal tumors (GISTs). Tang et al.29 found the non-Gaussian fractional order calculus diffusion model may be able to predict early GISTs response to second-line sunitinib targeted therapy.
Cine – MRI
The cine-MRI protocols for 13 studies are shown in Table 4. Breath-hold scanning and imaging in the coronal plane are most commonly adopted in cine-MRI studies. The parameters of slice, field of view (FOV), matrix size, and temporal resolution varied widely. Post-processing was also variably performed from manual measurements to semi-automated evaluations utilizing computer software.
Breath-hold scanning can reduce respiratory motion artifacts but limits the duration of the motility sequences. Free-breathing techniques could prolong acquisition times of the cine sequences which may prove beneficial as long duration cine-MRI is more reliable30. To observe consistent small bowel motility, a temporal resolution of at least 1 frame per second and a duration of at least 15 s is necessary in breath-hold scans31. The coronal plane is routinely used to analyze small-bowel motility as it enables adequate coverage of the entire small bowel and is optimal for assessment of peristalsis30,32,33. Regardless of the placement of coronal slices within the ventral, central, or dorsal portion of a small bowel segment, parameters reflecting SB movement did not change33. In a study of small bowel motility in 21 healthy volunteers, software-quantified measurements were repeatable and sensitive to changes in SB activity induced by pharmacologic manipulation34. However, in a study of 20 healthy volunteers, large variations in segmental motility were found within the same individual at the same time and the replicability was poor at the same location over time35. Studies by Bickelhaupt et al. in which free-breathing MRI was adopted showed that software-assisted evaluation of small bowel motility was much faster, more accurate, and reproducible than manual assessment36. Two mathematically established methods, Lomb-Scargle and Sinus-Fitting were reliable in the automated assessment of small bowel contraction frequency32. One optimized technique based on registration methods showed excellent agreement between observers for the analysis of overall gut motility in unprepared small bowel conditions37.
Clinical indications
Small-bowel neoplasms
Patients with PJS may suffer from polyp-related symptoms caused by gastrointestinal intussusception, obstruction, or infarction in addition to an increased risk of cancer38. MRE or MR enteroclysis could be used for periodic small bowel surveillance39. MR enteroclysis was found to have comparable diagnostic performance to double balloon enteroscopy (DBE) for polyps >15 mm, but DBE was better tolerated than MR enteroclysis by most patients40. A comparison between MR enterography and capsule endoscopy showed that although MR enterography was less comfortable for the patients, it was more reliable in measuring polyp size and less likely to miss large polyps41.
Neuroendocrine tumors (NETs) are common small bowel malignancies, the incidence of which is increasing42,43,44. Small bowel NETs are highly vascular tumors45. MR-enterography achieved a sensitivity of 95% for the detection of small bowel NETs. Contrast-enhanced 3D VIBE sequences were more sensitive than HASTE and True FISP for detection of NETs46.
GISTs are the most common mesenchymal tumors of the gastrointestinal tract47. MRI features and ADC measurements can be used to predict the NIH risk stratification. Obvious enhancement with intratumoral cystic change and lower ADC values may indicate a higher risk grade tumor48,49,50. GISTs could be effectively controlled by imatinib and need regular imaging follow-up. Tang et al.51 found lower baseline ADC and marked ADC increase at one week after therapy were associated with good response to imatinib mesylate.
In patients with peritoneal dissemination from appendiceal malignancy after surgical cytoreduction (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC), MRI detects tumor recurrence earlier than serum tumor makers alone and with greater accuracy25.
Amzallag-Bellenger et al.52 found that intravenous administration of gadolinium-based contrast improved sensitivity of SB tumor detection especially in patients with poor SB distension. Meanwhile, they found MR enterography achieved high negative predictive values (NPV) up to 98% on a perpatient basis, a factor conductive to excluding SB tumor when findings at capsular endoscopy are equivocal. In one MR enteroclysis study, overall sensitivity, specificity, and accuracy in identifying patients with small-bowel neoplasms were 91%, 95% and 95%, respectively53. The overall concordance between MR enteroclysis and histological examination of the surgical specimens was 62%54.
Small bowel obstruction
Computed tomography (CT) is the first-line examination for patients suspected of small bowel obstruction (SBO), but the diagnosis of strangulation or ischemia remains difficult55,56,57,58. Low b-value MRI obtainable in a short acquisition time (less than 60 s) might provide a feasible modality to detect bowel loops with compromised blood supply: the mean ADCs of the closed loop, near the site of obstruction, and distant from the obstruction site are all significantly different from each other23. Takahara et al.59 described the “peristalsis gap sign” referring to an akinetic or severely hypokinetic closed loop on cine MRI. This finding achieved higher sensitivity, specificity, positive predictive values (PPV), and NPV for strangulated small bowel than CT.
In studies of chronic intestinal pseudo-obstruction (CIPO), the diagnostic value of mean luminal diameter (MLD), contraction ratio (CR), and contraction cycle (CC) extracted from cine-MRI were evaluated. Results showed that MLD and CR differed significantly between patients with CIPO and healthy volunteers60,61. CC was significantly slower in CIPO patients with impaired small intestinal peristalsis compared to those without60.
Obscure gastrointestinal bleeding
Obscure gastrointestinal bleeding (OGIB) is defined as persistent or recurrent bleeding of unknown origin after negative endoscopy62. One comparison study between MR enteroclysis and capsule endoscopy in adults found that although MRE had a low accuracy in diagnosing OGIB caused by angiodysplasia and duodenal ulcers, its diagnostic performance in detection of OGIB caused by CD, SB tumor, and Meckel’s diverticulum was satisfactory63. Casciani et al.64 found MRE to be a safe imaging modality for the evaluation of pediatric OGIB with diagnostic performance comparable to capsule endoscopy in a group of 25 pediatric patients.
Irritable bowel syndrome (IBS)
Lam et al.65 assessed small bowel and colonic regional volumes as well as gut transit with MRI and found fasting small bowel water content in IBS patients with constipation to be significantly less than those of healthy volunteers. Fasting transverse colon volumes in IBS patients with constipation were significantly greater and whole-gut transit times were prolonged compared with patients without constipation and healthy volunteers.
The clinical presentation of small intestine bacterial overgrowth (SIBO) often overlaps with that of IBS. SIBO is characterized by increased fermentation of carbohydrate substrate due to bacterial contamination of the small intestine66,67. MRI can assist in the differential diagnosis of IBS and SIBO by synchronously evaluating oral to caecal transit time (OCTT) and median small bowel gas volume (SBGV)68.
Short bowel syndrome (SBS)
SBS is characterized by the inability to maintain acceptable nutrition due to surgical resection, congenital defect, or disease-related loss of absorption69. Although it is difficult to noninvasively measure the physical length of small bowel, MRE provides us with a promising approach. Sinha et al.70 applied a vascular imaging software to estimate small bowel length on true FISP sequences and found a significant correlation with surgical measurements. Wilson et al.71 found a custom-designed algorithm to be feasible and accurate for calculation of small intestine length on true FISP images. Application of automatic software and machine learning to measure SB length may further improve these techniques, which could benefit patients with or at risk for SBS in nutritional management and surgical approach.
Other SB abnormalities
One study by Cobelli et al.72 reported that dynamic contrast-enhanced (DCE) MRI of the small bowel could be used to investigate mesenteric vascular flow finding impaired perfusion to be a reliable MRI marker in paroxysmal nocturnal hemoglobinuria (PNH) patients with abdominal pain.
MR enteroclysis and MR enterography have the ability to diagnose SB diverticulitis and diverticulosis; although, the superiority of MRI to other modalities in this regard is not clear. Focal inflammatory changes of the mesenteric fat, asymmetric wall thickening and the presence of multiple diverticula are keys to differentiate SB diverticulitis from other SB IBDs and neoplasms73.
Lymphoid nodular hyperplasia is an incidental finding and normal variant particularly in children and adolescents but can mimic CD on MR enterography. Image features including T2 signal, enhancement pattern, wall thickness, and ADC values showed no significant difference between lymphoid nodular hyperplasia of the terminal ileum and CD26.
Conclusion
MRI techniques for SB imaging differ between different institutions especially with respect to gastrointestinal preparation and cine-MRI scanning. Polyethylene glycol (PEG) and mannitol hydrosolution were the most commonly utilized enteric contrast agents. Prone positioning was more commonly used than supine; although, the balance of patient comfort versus detection rate for pathology requires further study and literature support. DWI was not routinely used for MR assessment of non-IBDs, and its role in detecting non-IBD pathology especially SB neoplasms is not yet clear. MRI protocols for cine-MRI of the small bowel vary widely, and the definition of normal and abnormal SB motility by this modality is not clear. The consensus guidelines issued by ESGAR and ESPR can be used as a reference for non-IBD small bowel MRI; however, development of standardized protocols for cine-MRI sequences will require further evidence from original research.
References
Masselli, G. & Gualdi, G. MR imaging of the small bowel. Radiology 264, 333–348, https://doi.org/10.1148/radiol.12111658 (2012).
Wnorowski, A. M., Guglielmo, F. F. & Mitchell, D. G. How to perform and interpret cine MR enterography. J. Magn. Reson. Imaging 42, 1180–1189, https://doi.org/10.1002/jmri.24981 (2015).
Pasquini, L. et al. Gadolinium-Based Contrast Agent-Related Toxicities. CNS Drugs 32, 229–240, https://doi.org/10.1007/s40263-018-0500-1 (2018).
Higgins, P. D. & Fletcher, J. G. Characterization of inflammation and fibrosis in Crohn’s disease lesions by magnetic resonance imaging. Am. J. Gastroenterol. 110, 441–443, https://doi.org/10.1038/ajg.2015.26 (2015).
Buisson, A. et al. Diffusion-weighted magnetic resonance enterocolonography in predicting remission after anti-TNF induction therapy in Crohn’s disease. Dig. Liver Dis. 48, 260–266, https://doi.org/10.1016/j.dld.2015.10.019 (2016).
Dillman, J. R. et al. DWI in Pediatric Small-Bowel Crohn Disease: Are Apparent Diffusion Coefficients Surrogates for Disease Activity in Patients Receiving Infliximab Therapy? AJR Am. J. Roentgenol. 207, 1002–1008, https://doi.org/10.2214/AJR.16.16477 (2016).
Li, X. H. et al. Diffusion-weighted MRI Enables to Accurately Grade Inflammatory Activity in Patients of Ileocolonic Crohn’s Disease: Results from an Observational Study. Inflamm. Bowel Dis. 23, 244–253, https://doi.org/10.1097/MIB.0000000000001001 (2017).
Rimola, J. et al. Magnetic resonance for assessment of disease activity and severity in ileocolonic Crohn’s disease. Gut 58, 1113–1120, https://doi.org/10.1136/gut.2008.167957 (2009).
Rimola, J. et al. Magnetic resonance imaging for evaluation of Crohn’s disease: validation of parameters of severity and quantitative index of activity. Inflamm. Bowel Dis. 17, 1759–1768, https://doi.org/10.1002/ibd.21551 (2011).
Ordas, I. et al. Accuracy of magnetic resonance enterography in assessing response to therapy and mucosal healing in patients with Crohn’s disease. Gastroenterology 146, 374–382 e371, https://doi.org/10.1053/j.gastro.2013.10.055 (2014).
Amzallag-Bellenger, E. et al. Effectiveness of MR enterography for the assessment of small-bowel diseases beyond Crohn disease. Radiographics 32, 1423–1444, https://doi.org/10.1148/rg.325115088 (2012).
Taylor, S. A. et al. The first joint ESGAR/ ESPR consensus statement on the technical performance of cross-sectional small bowel and colonic imaging. Eur. Radiol. 27, 2570–2582, https://doi.org/10.1007/s00330-016-4615-9 (2017).
Pariente, B. et al. Development of the Lemann index to assess digestive tract damage in patients with Crohn’s disease. Gastroenterology 148, 52–63 e53, https://doi.org/10.1053/j.gastro.2014.09.015 (2015).
Rimola, J. et al. Characterization of inflammation and fibrosis in Crohn’s disease lesions by magnetic resonance imaging. Am. J. Gastroenterol. 110, 432–440, https://doi.org/10.1038/ajg.2014.424 (2015).
Sinha, R. et al. Diagnostic accuracy of high-resolution MR enterography in Crohn’s disease: comparison with surgical and pathological specimen. Clin. Radiol. 68, 917–927, https://doi.org/10.1016/j.crad.2013.02.012 (2013).
Lawrance, I. C., Welman, C. J., Shipman, P. & Murray, K. Small bowel MRI enteroclysis or follow through: Which is optimal? World J. Gastroenterol. 15, 5300–5306, https://doi.org/10.3748/wjg.15.5300 (2009).
Kuehle, C. A. et al. Hydro-MRI of the small bowel: effect of contrast volume, timing of contrast administration, and data acquisition on bowel distention. AJR Am. J. Roentgenol. 187, W375–385, https://doi.org/10.2214/AJR.05.1079 (2006).
Cronin, C. G. et al. MRI small-bowel follow-through: prone versus supine patient positioning for best small-bowel distention and lesion detection. AJR Am. J. Roentgenol. 191, 502–506, https://doi.org/10.2214/AJR.07.2338 (2008).
Maccioni, F., Al Ansari, N., Mazzamurro, F., Barchetti, F. & Marini, M. Surveillance of patients affected by Peutz-Jeghers syndrome: diagnostic value of MR enterography in prone and supine position. Abdom. Imaging 37, 279–287, https://doi.org/10.1007/s00261-011-9739-4 (2012).
Bickelhaupt, S., Froehlich, J. M., Wentz, K. U., von Weymarn, C. & Patak, M. A. Small-bowel dislocation during long-term MRI observation - insights in intestinal physiology. Clin. Physiol. Funct. Imaging 35, 41–48, https://doi.org/10.1111/cpf.12124 (2015).
Ghobrial, P. M. et al. Cine MR enterography grading of small bowel peristalsis: evaluation of the antiperistaltic effectiveness of sublingual hyoscyamine sulfate. Acad. Radiol. 21, 86–91, https://doi.org/10.1016/j.acra.2013.09.024 (2014).
Amzallag-Bellenger, E. et al. Diffusion-weighted imaging for the detection of mesenteric small bowel tumours with Magnetic Resonance–enterography. Eur. Radiol. 24, 2916–2926, https://doi.org/10.1007/s00330-014-3303-x (2014).
Takahara, T. et al. Low b-value diffusion-weighted imaging for diagnosing strangulated small bowel obstruction: a feasibility study. J. Magn. Reson. Imaging 34, 1117–1124, https://doi.org/10.1002/jmri.22735 (2011).
Schmidt, S. A. et al. Oral distension methods for small bowel MRI: comparison of different agents to optimize bowel distension. Acta Radiol. 57, 1460–1467, https://doi.org/10.1177/0284185116631183 (2016).
Low, R. N., Barone, R. M. & Lee, M. J. Surveillance MR imaging is superior to serum tumor markers for detecting early tumor recurrence in patients with appendiceal cancer treated with surgical cytoreduction and HIPEC. Ann. Surg. Oncol. 20, 1074–1081, https://doi.org/10.1245/s10434-012-2788-2 (2013).
Plumb, A. A. et al. Lymphoid nodular hyperplasia of the terminal ileum can mimic active crohn disease on MR enterography. AJR Am. J. Roentgenol. 203, W400–407, https://doi.org/10.2214/AJR.13.12055 (2014).
Sinha, R. et al. imaging of the gastrointestinal tract: technique, indications, and imaging findings. Radiographics 33, 655–676; discussion 676–680, https://doi.org/10.1148/rg.333125042 (2013).
Wong, C. S. et al. Correlation of measurements from diffusion weighted MR imaging and FDG PET/CT in GIST patients: ADC versus SUV. Eur. J. Radiol. 81, 2122–2126, https://doi.org/10.1016/j.ejrad.2011.09.003 (2012).
Tang, L. et al. Non-Gaussian diffusion imaging with a fractional order calculus model to predict response of gastrointestinal stromal tumor to second-line sunitinib therapy. Magn. Reson. Med. 79, 1399–1406, https://doi.org/10.1002/mrm.26798 (2018).
Bickelhaupt, S. et al. Software-assisted small bowel motility analysis using free-breathing MRI: feasibility study. J. Magn. Reson. Imaging 39, 17–23, https://doi.org/10.1002/jmri.24099 (2014).
de Jonge, C. S. et al. Dynamic MRI for bowel motility imaging-how fast and how long? Br. J. Radiol. 91, 20170845, https://doi.org/10.1259/bjr.20170845 (2018).
Bickelhaupt, S. et al. Automatic detection of small bowel contraction frequencies in motility plots using lomb-scargle periodogram and sinus-fitting method–initial experience. Magn. Reson. Med. 71, 628–634, https://doi.org/10.1002/mrm.24708 (2014).
Bickelhaupt, S., Froehlich, J. M. & Patak, M. A. Automated small bowel motility measurements in MRI using 2D coronal slices - does the intrasegmental location matter? A pilot study. Clin. Imaging 39, 89–93, https://doi.org/10.1016/j.clinimag.2014.10.003 (2015).
Menys, A. et al. Global small bowel motility: assessment with dynamic MR imaging. Radiology 269, 443–450, 10.1148/radiol.13130151%/ RSNA, 2013 (2013).
Menys, A., Plumb, A., Atkinson, D. & Taylor, S. A. The challenge of segmental small bowel motility quantitation using MR enterography. Br. J. Radiol. 87, 20140330, https://doi.org/10.1259/bjr.20140330 (2014).
Bickelhaupt, S. et al. Software-assisted quantitative analysis of small bowel motility compared to manual measurements. Clin. Radiol. 69, 363–371, https://doi.org/10.1016/j.crad.2013.11.004 (2014).
Khalaf, A. et al. Cine MRI assessment of motility in the unprepared small bowel in the fasting and fed state: Beyond the breath-hold. Neurogastroenterol. Motil. 31, e13466, https://doi.org/10.1111/nmo.13466 (2019).
Beggs, A. D. et al. Peutz-Jeghers syndrome: a systematic review and recommendations for management. Gut 59, 975–986, https://doi.org/10.1136/gut.2009.198499 (2010).
Korsse, S. E., Dewint, P., Kuipers, E. J. & van Leerdam, M. E. Small bowel endoscopy and Peutz-Jeghers syndrome. Best Pract. Res. Clin. Gastroenterol. 26, 263–278, https://doi.org/10.1016/j.bpg.2012.03.009 (2012).
Goverde, A. et al. Small-bowel Surveillance in Patients With Peutz-Jeghers Syndrome: Comparing Magnetic Resonance Enteroclysis and Double Balloon Enteroscopy. J. Clin. Gastroenterol. 51, e27–e33, https://doi.org/10.1097/MCG.0000000000000592 (2017).
Gupta, A. et al. A prospective study of MR enterography versus capsule endoscopy for the surveillance of adult patients with Peutz-Jeghers syndrome. AJR Am. J. Roentgenol. 195, 108–116, https://doi.org/10.2214/AJR.09.3174 (2010).
Banck, M. S. & Beutler, A. S. Advances in small bowel neuroendocrine neoplasia. Current opinion in gastroenterology 30, 163–167, https://doi.org/10.1097/MOG.0000000000000043 (2014).
Stalberg, P., Westin, G. & Thirlwell, C. Genetics and epigenetics in small intestinal neuroendocrine tumours. J. Intern. Med. 280, 584–594, https://doi.org/10.1111/joim.12526 (2016).
Scherubl, H., Jensen, R. T., Cadiot, G., Stolzel, U. & Kloppel, G. Neuroendocrine tumors of the small bowels are on the rise: Early aspects and management. World J Gastrointest Endosc 2, 325–334, https://doi.org/10.4253/wjge.v2.i10.325 (2010).
Zhang, J. et al. Elevated expression of vascular endothelial growth factor correlates with increased angiogenesis and decreased progression-free survival among patients with low-grade neuroendocrine tumors. Cancer 109, 1478–1486, https://doi.org/10.1002/cncr.22554 (2007).
Dohan, A. et al. Neuroendocrine tumors of the small bowel: evaluation with MR-enterography. Clin. Imaging 40, 541–547, https://doi.org/10.1016/j.clinimag.2015.12.016 (2016).
Rubin, B. P., Heinrich, M. C. & Corless, C. L. Gastrointestinal stromal tumour. Lancet 369, 1731–1741, https://doi.org/10.1016/s0140-6736(07)60780-6 (2007).
Kang, T. W. et al. Gastrointestinal stromal tumours: Correlation of modified NIH risk stratification with diffusion-weighted MR imaging as an imaging biomarker. Eur. J. Radiol. 84, 33–40, https://doi.org/10.1016/j.ejrad.2014.10.020 (2015).
Zhou, H. Y., Zhang, X. M., Zeng, N. L., Jian, S. H. & Tang, W. Use of conventional MR imaging and diffusion-weighted imaging for evaluating the risk grade of gastrointestinal stromal tumors. J. Magn. Reson. Imaging 36, 1395–1401, https://doi.org/10.1002/jmri.23784 (2012).
Yu, M. H., Lee, J. M., Baek, J. H., Han, J. K. & Choi, B. I. MRI features of gastrointestinal stromal tumors. Am. J. Roentgenol. 203, 980–991, https://doi.org/10.2214/AJR.13.11667 (2014).
Tang, L. et al. Gastrointestinal stromal tumors treated with imatinib mesylate: Apparent diffusion coefficient in the evaluation of therapy response in patients. Radiology 258, 729–738, https://doi.org/10.1148/radiol.10100402 (2011).
Amzallag-Bellenger, E. et al. Prospective evaluation of magnetic resonance enterography for the detection of mesenteric small bowel tumours. Eur. Radiol. 23, 1901–1910, https://doi.org/10.1007/s00330-013-2800-7 (2013).
Van Weyenberg, S. J. et al. MR enteroclysis in the diagnosis of small-bowel neoplasms. Radiology 254, 765–773, https://doi.org/10.1148/radiol.09090828 (2010).
Pappalardo, G. et al. Impact of magnetic resonance in the preoperative staging and the surgical planning for treating small bowel neoplasms. Surg. Today 43, 613–619, https://doi.org/10.1007/s00595-012-0270-1 (2013).
Jancelewicz, T. et al. Predicting strangulated small bowel obstruction: an old problem revisited. J. Gastrointest. Surg. 13, 93–99, https://doi.org/10.1007/s11605-008-0610-z (2009).
Nicolaou, S., Kai, B., Ho, S., Su, J. & Ahamed, K. Imaging of acute small-bowel obstruction. AJR Am. J. Roentgenol. 185, 1036–1044, https://doi.org/10.2214/AJR.04.0815 (2005).
Silva, A. C., Pimenta, M. & Guimaraes, L. S. Small bowel obstruction: what to look for. Radiographics 29, 423–439, https://doi.org/10.1148/rg.292085514 (2009).
Paulson, E. K. & Thompson, W. M. Review of small-bowel obstruction: the diagnosis and when to worry. Radiology 275, 332–342, https://doi.org/10.1148/radiol.15131519 (2015).
Takahara, T. et al. Peristalsis gap sign at cine magnetic resonance imaging for diagnosing strangulated small bowel obstruction: feasibility study. Jpn J Radiol 29, 11–18, https://doi.org/10.1007/s11604-010-0508-z (2011).
Fuyuki, A. et al. Clinical importance of cine-MRI assessment of small bowel motility in patients with chronic intestinal pseudo-obstruction: a retrospective study of 33 patients. J. Gastroenterol. 52, 577–584, https://doi.org/10.1007/s00535-016-1251-8 (2017).
Ohkubo, H. et al. Assessment of small bowel motility in patients with chronic intestinal pseudo-obstruction using cine-MRI. Am. J. Gastroenterol. 108, 1130–1139, https://doi.org/10.1038/ajg.2013.57 (2013).
Leung, W. K. et al. Capsule endoscopy or angiography in patients with acute overt obscure gastrointestinal bleeding: a prospective randomized study with long-term follow-up. Am. J. Gastroenterol. 107, 1370–1376, https://doi.org/10.1038/ajg.2012.212 (2012).
Wiarda, B. M. et al. Comparison of magnetic resonance enteroclysis and capsule endoscopy with balloon-assisted enteroscopy in patients with obscure gastrointestinal bleeding. Endoscopy 44, 668–673, https://doi.org/10.1055/s-0032-1309386 (2012).
Casciani, E. et al. MR Enterography in paediatric patients with obscure gastrointestinal bleeding. Eur. J. Radiol. 93, 209–216, https://doi.org/10.1016/j.ejrad.2017.05.044 (2017).
Lam, C. et al. Distinct Abnormalities of Small Bowel and Regional Colonic Volumes in Subtypes of Irritable Bowel Syndrome Revealed by MRI. Am. J. Gastroenterol. 112, 346–355, https://doi.org/10.1038/ajg.2016.538 (2017).
Vanner, S. The small intestinal bacterial overgrowth. Irritable bowel syndrome hypothesis: implications for treatment. Gut 57, 1315–1321, https://doi.org/10.1136/gut.2007.133629 (2008).
Pimentel, M. & Lezcano, S. Irritable Bowel Syndrome: Bacterial Overgrowth–What’s Known and What to Do. Curr Treat Options Gastroenterol 10, 328–337 (2007).
Savarino, E. et al. Measurement of oro-caecal transit time by magnetic resonance imaging. Eur. Radiol. 25, 1579–1587, https://doi.org/10.1007/s00330-014-3575-1 (2015).
O’Keefe, S. J. et al. Short bowel syndrome and intestinal failure: consensus definitions and overview. Clin. Gastroenterol. Hepatol. 4, 6–10, https://doi.org/10.1016/j.cgh.2005.10.002 (2006).
Sinha, R., Trivedi, D., Murphy, P. D. & Fallis, S. Small-intestinal length measurement on MR enterography: comparison with in vivo surgical measurement. AJR Am. J. Roentgenol. 203, W274–279, https://doi.org/10.2214/AJR.13.11944 (2014).
Wilson, N. A., Park, H. S., Lee, K. S., Barron, L. K. & Warner, B. W. A Novel Approach to Calculating Small Intestine Length Based on Magnetic Resonance Enterography. J. Am. Coll. Surg. 225, 266–273 e261, https://doi.org/10.1016/j.jamcollsurg.2017.04.009 (2017).
De Cobelli, F. et al. New Insights in Abdominal Pain in Paroxysmal Nocturnal Hemoglobinuria (PNH): A MRI Study. PLoS One 10, e0122832, https://doi.org/10.1371/journal.pone.0122832 (2015).
Mansoori, B. et al. Magnetic resonance enterography/enteroclysis in acquired small bowel diverticulitis and small bowel diverticulosis. Eur. Radiol. 26, 2881–2891, https://doi.org/10.1007/s00330-015-4098-0 (2016).
Acknowledgements
The authors thank all of the staff members in the department of Radiology, Tongji Hospital, Wuhan, Hubei, China.
Author information
Authors and Affiliations
Contributions
Y.S. and J.L. contributed to the design of the paper, Z.L. and D.H. developed and organized the paper. J.L., Z.Z. and H.Y. contributed to the literature review and data analysis. Y.L and X.H. designed the tables and figures. Y.S., J.L. and J.M. participated in drafted sections of the manuscript and helped revise the paper. All authors reviewed the manuscript and approved the final vision to be submitted.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lu, J., Zhou, Z., Morelli, J.N. et al. A Systematic Review of Technical Parameters for MR of the Small Bowel in non-IBD Conditions over the Last Ten Years. Sci Rep 9, 14100 (2019). https://doi.org/10.1038/s41598-019-50501-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-50501-9
This article is cited by
-
Mimicking conditions of intestinal Crohn’s disease: magnetic resonance enterography findings
Japanese Journal of Radiology (2022)
-
Nodular lymphoid hyperplasia of terminal ileum: how to avoid overdiagnosis of Crohn’s terminal ileitis in MR enterography?
Abdominal Radiology (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.