Abstract
Emergence of new molecules acting directly on the hepatitic C virus (HCV) has improved treatment outcomes. However, there is a risk of selecting viral escape mutants, so a new combination is needed using different inhibitors that target different steps of the HCV infectious cycle. Novel single tablet formulations were developed: Dactavira, composed of sofosbuvir (SOF) 400 mg/daclatisvir (DCV) 60 mg/epigallocatechin gallate (EGCG) 400 mg without ribavirin (RBV); and Dactavira plus, which includes RBV 800 mg. A randomized, open-label study was carried out on treatment-naïve non-cirrhotic (Group A, n = 50) and treatment-naïve cirrhotic (Group B, n = 22) patients with genotype 4 HCV infection. Group A was randomly assigned to receive a single daily fixed-dose (Dactavira, n = 25) or the standard of care [SOF 400 mg/DCV 60 mg] (n = 25) daily for 12 weeks. Group B was randomly assigned to receive a single daily fixed-dose (Dactavira plus, n = 11) or the standard of care + RBV 800 mg (n = 11) daily for 12 weeks. Patients receiving Dactavira or Dactavira plus had a significantly more rapid rate of viral load decline as compared to patients receiving the standard of care therapy. Sustained virological response for 12 weeks for Dactavira or Dactavira plus showed no statistically significant difference when compared to the standard of care. Also, they did not affect normal hemoglobin levels (p < 0.001) versus the standard of care. The incorporated EGCG interferes with the viral entry mechanisms, as reported by several investigators, and in turn enhances efficacy and prevents relapse as compared to the standard of care. Also, its antihemeolytic and antifibrotic activities may improve the safety and tolerability of the therapy.
Similar content being viewed by others
Introduction
Hepatitis C virus (HCV) is the common cause of liver cirrhosis and hepatocellular carcinoma1. It infects more than 71 million people worldwide with a high prevalence of genotype 4 virus in Egyptian patients2. To date, there is noavailable vaccine against HCV infection3.
Discovery of new molecules that act directly on the virus itself, directly acting antivirals (DAAs), which disrupt viral translation and replication by targeting viral component(s), have completely changed chronic hepatitis C (CHC) therapeutic strategies4,5,6,7. Most of these molecules are associated with high efficacy and safety profiles for most patients with HCV8. DAA combinations in all-oral regimens have led to overall high SVR (~90%) in treated individuals compared to ~60% with treatment completion of PEG IFN-α and ribavirin (RBV), independent of the severity of liver disease and viral genotype. Although DAAs have replaced IFN-based therapy, RBV remains essential in selected cases identified by the virus’ genotype, previous treatment failure, and disease stage5,6,7,9,10.
By 2013–2014, anti-HCV therapy moved a step forward after the approval of a second generation of DAAs, e.g., sofosbuvir (SOF), nucleoside/nucleotide analogues and daclatasvir (DCV), and a nonstructural protein 5A (NS5A) inhibitor11. SOF in combination with RBV, as well as triple therapy along with PEG IFN-α/RBV, has proven its clinical efficacy against different HCV genotypes11,12. The marked simplifications for such therapeutic regimens include once-daily dosing, better tolerability, improved adverse event profile, fewer drug–drug interactions, and possibly lower contraindications13,14.
In 2015, the combination of DCV and SOF with or without RBV as an oral treatment option for patients with chronic HCV was approved by the FDA15. This combination was associated with higher SVR rates, fewer adverse events, and less antiviral resistance15. Headache and fatigue were reported as the most common adverse effects in patients treated with the combination of SOF and DCV (~10% of patients). Furthermore, the risk of adverse effects increased in patients treated with the combination of SOF, DCV, and RBV including anemia, headache, fatigue, and nausea16.
In our previous study, we stated the pharmacological potential effect of EHCV (Catvira), SOF 400 mg/RBV 1000 mg/epigallocatechin gallate (EGCG) 400 mg, which showed no statistical significant difference when compared to the standard of care (SOF 400 mg/RBV 1000 mg). In that study, we reported the faster rate of viral load decline and also the protective effect of EHCV (Catvira) on red blood cell (RBC) count and hemoglobin levels as compared to the standard of care17. These effects could be related to the incorporation of EGCG, a polyphenol component extracted from green tea that has been shown to have multiple effects on human pathological and physiological processes including anticancer, anti-oxidant, anti-inflammatory, and antifibrosis effects18,19. Recently, EGCG has been identified as an inhibitor of HCV entry as well as an antihemeolytic agent20,21. We aimed to develop a single daily fixed-dose therapy against HCV infection that would be more effective, inexpensive, better-tolerated, and safer than the standard of care therapy. The present study compared Dactavira and Dactavira plus to the standard of care treatment: Dactavira (SOF 400 mg/DCV 60 mg/EGCG 400 mg without RBV) to standard of care (SOF 400 mg/DCV 60 mg), and Dactavira plus (includes RBV 800 mg) to the standard of care with RBV 800 mg in patients with CHC genotype 4.
Methods
Patients
Patients were screened and enrolled in this phase 3 open-label study at a single center in Egypt between September, 2016 and November, 2017 (ClinicalTrials.gov Identifier NCT03186313, 14/06/2017). The study was conducted in accordance with the guidelines of Good Clinical Practice and was approved by the Independent Review Board of the Faculty of Medicine, Mansoura University. All patients provided written informed consent.
Patients were required to be at least 18 years of age with body mass index ≥18 kg/m2 and have chronic genotype 4 HCV infection with a serum HCV RNA level ≥ 4 log10 IU/ml. HCV RNA was extracted from 650 µl of serum for CAP/CTM HCV v2.0 by means of the Cobas Ampliprep automated extractor, according to the manufacturer’s instructions. The Cobas Taqman 48 analyzer was used for automated real-time PCR amplification and detection of PCR products according to the manufacturer’s instructions (Roche Molecular Systems, Pleasanton, CA, USA) with a detection limit of 15 IU/ml. HCV RNA-positive samples were genotyped using an HCV real-time genotype kit (AmpliSens HCV-genotype-FRT PCR kit) that was able to detect HCV genotypes 1a, 1b, 2, 3, and 4, following the manufacturer’s instructions. The presence of cirrhosis was determined based on Fibroscan. Cirrhosis is defined by fibroscan >12·5 kpa. Laboratory test requirements included alanine aminotransferase (ALT) and aspartate aminotransferase (AST) ≤10 times the upper limit of normal (ULN), direct bilirubin ≤1·5 times ULN, hemoglobin ≥12 g/dl for men and ≥11 g/dl for women, and creatinine clearance ≥60 ml/min (Cockcroft-Gault). Consistent with the inclusion of patients with cirrhosis, patients with platelets >50,000/µl were eligible for participation. Patients with hepatitis B or HIV were excluded. Patients were treatment-naïve. Patients who had prior treatment with an anti-HCV direct-acting antiviral were excluded. Patient characteristics are compiled in Table 1.
Randomization and masking
Patients were randomly assigned, on a 1:1 basis and in a masked fashion, to group A consisting of treatment-naïve patients with non-cirrhotic genotype 4 HCV infection (n = 50). They were randomly assigned in a 1:1 ratio to receive single (2 tablets) fixed-dose Dactavira daily for 12 weeks. Group B consisted of treatment-naïve patients with cirrhotic genotype 4 HCV infection (n = 22). They were randomly assigned in a 1:1 ratio to receive single (2 tablets) fixed-dose Dactavira plus daily for 12 weeks.
Study design
Group A consisted of treatment-naïve patients with non-cirrhotic genotype 4 HCV infection (n = 50). They were randomly assigned in a 1:1 ratio to receive single (2 tablets) fixed-dose Dactavira, each tablet containing SOF 200 mg, DCV 30 mg, and EGCG 200 mg daily for 12 weeks (n = 25) or the standard of care SOF 400 mg, DCV 60 mg (n = 25) daily for 12 weeks.
Group B consisted of treatment-naïve patients with cirrhotic genotype 4 HCV infection (n = 22). They were randomly assigned in a 1:1 ratio to receive single (2 tablets) fixed-dose Dactavira plus, each tablet containing SOF 200 mg, DCV 30 mg, EGCG 200 mg, and RBV 400 mg daily for 12 weeks (n = 11) or the standard of care SOF 400 mg, DCV 60 mg with RBV 800 mg (n = 11) daily for 12 weeks. The primary efficacy endpoint was the proportion of all randomized patients who achieved SVR 12 weeks after the end of treatment (SVR12). Secondary efficacy endpoints included SVR4, on-treatment virologic failure, and virologic relapse after the end of treatment.
Efficacy assessments
Serum HCV RNA was measured using the COBAS TaqMan HCV Test v2·0 (Roche Molecular Systems; lower limit of quantitation (LLOQ) of 25 IU/ml) at baseline, at all subsequent study visits during treatment, and post-treatment weeks 4 and 12. Patients with confirmed HCV RNA <LLOQ at the end of treatment and post-treatment visits continued to the subsequent post-treatment visits, unless confirmed virologic relapse occurred. On-treatment virologic failure was defined as: breakthrough, i.e., confirmed HCV RNA ≥LLOQ after having previously had HCV RNA <LLOQ while on-treatment; rebound, i.e., confirmed > one log IU/ml increase in HCV RNA from nadir while on-treatment; or non-response, i.e., HCV RNA persistently ≥LLOQ through 8 weeks of treatment. Relapse was defined as confirmed HCV RNA ≥LLOQ during the post-treatment period having achieved HCV RNA <LLOQ at the end of treatment.
Safety assessments
Safety was evaluated by assessment of clinical laboratory tests, physical examination, vital sign measurements, and documentation of adverse events. Safety data were collected starting from the first dose of study medication through 30 days after the last dose.
Statistical assessments
The primary efficacy analysis, SVR12 rates were calculated for each treatment group, along with 2-sided 95% confidence intervals (CIs) based on the Clopper-Pearson exact method. No statistical hypothesis testing was performed.
Role of the funding source
The ELRIAH had a role in the study design, data collection, and data analysis. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Patients
Eighty patients were assessed for eligibility; 6 were excluded because they did not meet the eligibility criteria. Fifty-two patients were enrolled in group A and completed treatment for 12 weeks; 26 of them received Dactavira and the other 26 received standard of care; 2 patients were lost to follow-up. Twenty-two patients were enrolled in group B and completed treatment for 12 weeks; 11 of them received Dactavira plus and the other 11 received standard of care with RBV. The mean age of enrolled patients (male and female) was 18 years, and 63% were men. All patients had a body mass index ≥18 kg/m2, 30·6% had cirrhosis, hemoglobin level was around >12 g/dl, and the liver enzymes (ALT and AST) were around 88·5–32·8 U/L.
Efficacy
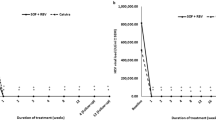
Both Dactavira or Dactavira plus and the standard of care Groups A and B yielded similar treatment outcomes in terms of viral load measured at the conclusion of the 12 week study period (Fig. 1). Patients receiving Dactavira or Dactavira plus, however, had a significantly more rapid rate of viral load decline as compared to patients receiving the standard of care therapy. Patients receiving Dactavira or Dactavira plus showed a rapid decline in HCV RNA levels upon initiation of treatment, from a mean of 1·75/1·52 log10 at baseline to 0·0/0·42 log10 in the 12 weeks after treatment. On the other hand, patients receiving standard of care therapy (SOF + DCV) or (SOF + DCV + RBV) showed a decline in HCV RNA levels upon initiation of treatment, from a mean of 1·45/1·66 log10 at baseline to 0·0/0·0 log10 in the 12 weeks after treatment. Regarding the Dactavira plus group, SVR12 was achieved by all patients (100%) receiving 12 weeks of treatment (Table 2).
Safety
In general, Dactavira or Dactavira plus related adverse effects were similar or less than in the standard of care groups, and they were observed to be less severe and persist for shorter duration. All these adverse events resolved and none was considered to be treatment-related.
Consistent with changes in clinical laboratory values, Dactavira or Dactavira plus did not impact hemoglobin levels or RBC count while the standard of care resulted in a significant decline in both parameters after 12 weeks of treatment (p < 0·001) (Table 3, Figs 2 and 3). Neither Dactavira or Dactavira plus, nor the standard of care was associated with significant effect on platelet count (Supplementary Table S1).
Effects on hemoglobin levels of Dactavira (SOF + DCV + EGCG) (n = 25) and Dactavira plus (SOF + DCV + EGCG + RBV) (n = 11) versus SOF + DCV (n = 25) and SOF + DCV + RBV (n = 11) in the different enrolled groups (12 weeks treatment). Values represent the changes in hemoglobin. Dactavira plus was associated with significantly less hemolysis (*p < 0·001) when compared with SOF + DCV + RBV group, and Dactavira was associated with significantly less hemolysis (*p < 0·001) when compared with SOF + DCV.
Effects on red blood cell count of Dactavira (SOF + DCV + EGCG) (n = 25) and Dactavira plus (SOF + DCV + EGCG + RBV) (n = 11) versus SOF + DCV (n = 25) and SOF + DCV + RBV (n = 11) in treatment-experienced HCV patients (12 weeks treatment). Values represent the changes in red blood cell count. Dactavira and Dactavira plus were associated with significant improvement (*p < 0·001) when compared with SOF + DCV and SOF + DCV + RBV groups.
Also, we compared the effectiveness of Dactavira, Dactavira plus, and the standard of care on liver functions including ALT, AST, bilirubin, and albumin. All treatments improved liver functions (Supplementary Table S2). Furthermore, all treatments achieved significant improvement in liver enzymes (ALT and AST) (Table 4). Regarding the diabetic status of our patients, just 6 out of 72 patients were diabetic, and we didn’t record any renal toxicity on those patients during or after the treatment.
In conclusion, there were no patients with adverse events that led to dose modification, interruption, or discontinuation of Dactavira or Dactavira plus.
Discussion
This phase 3, open-label, 12-weeks treatment study with Dactavira or Dactavira plus resulted in high rates of SVR12 in treatment-naïve non-cirrhotic and treatment-naïve cirrhotic patients with genotype 4 HCV infection. SVR12 for Dactavira or Dactavira plus showed no statistically significant difference when compared to the standard of care. Both Dactavira and Dactavira plus were well tolerated, with mostly mild adverse events. Dactavira plus did not affect hemoglobin levels as compared to the standard of care, which resulted in a significant decline.
Dactavira or Dactavira plus may be superior to EHCV (Catvira), which was reported in our previous study to be associated with rapid decline in viral load17. This may be related to combination of different DAA (DCV + SOF) that act by different targeting mechanisms: NS5A inhibitor and a nucleotide NS5B inhibitor. Furthermore, as for Catvira, Dactavira plus did not show any effect on RBC count or hemoglobin levels as compared to the standard of care that resulted in a significant decline in both parameters after 12–24 weeks of treatment17.
Incorporation of 400 mg EGCG, which is the bio-active catechin in green tea, in Dactavira and Dactavira plus may interfere with the close links between HCV and lipid metabolism. Binding of HCV particles to hepatocytes is the intial and important step in HCV infectivity. This interaction between HCV particles and the host hepatocyte is mediated mainly by heparin sulfate proteoglycan, scavenger receptor (SR-B1), apoE, and LDL receptor (LDL-r)22,23,24.
Consistent with our results, Calland et al. reported that significant decrease of JFH1-Luc infection with recombinant HCV was observed in the presence of increasing concentrations of EGCG. EGCG at 5 μM was associated with more than 50% decrease in infectivity, while more than 90% decrease in infectivity was observed at 50 μM25.
Recent studies have reported the ability of EGCG to induce a critical structural alternation in the HCV particle itself. This structural disruption interferes with the membrane binding mediated by heparin sulfate- or sialic acid-containing glycans20.
Several reports have demonstrated the ability of EGCG to interfere with viral replication. An in vitro study using JFH1 cell line treated with 80 μM of EGCG was associated with undetecable HCV RNA and protein expression 72 hours post-infection26. Also, Lin et al. reported that HCV RNA levels were markedly eliminated (~85%) after exposure to 75 µM epicatechin isomers at 9 days using Ava5 cells27.
Calland et al. and Lin et al. reported the safety of EGCG with no effect on cell viability as measured with the MTS assay25,27. Calland et al. reported that EGCG had no toxic effect on Huh-7 cells (LD50 ~160 μM)25. Chow et al. concluded that EGCG is safe for healthy individuals even in content equivalent to the amount of EGCG in 16 cups of green tea (~800 mg EGCG) taken once a day or in divided doses twice a day for 4 weeks28.
EGCG is known as a highly efficient free radical scavenger (potent anti-oxidant). Here, we demonstrated the protective effect of Dactavira plus against hemoolytic anemia, which is associated with RBV. In our study, Dactavira plus did not affect hemoglobin levels as compared to the standard of care. Consistent with our results, Kim et al. reported that EGCG lowered the levels of hemolysis and hydrogen peroxide and malondialdehyde produced by normal human erythrocytes (RBCs) incubated with cyclosporine by about ~20%. This protective effect related mainly to a decrease in production of free radical species induced by the cyclosporine therapy21. Moses et al. investigated the effect of EGCG against paraquat-induced hemolysis. Paraquat is known to be toxic to RBCs’ membrane due to its redox activity, which produces superoxide anions. Osmotic fragility of the erythrocytes was tested after incubation of RBCs with different concentrations of EGCG (0·03–30 mg/ml) in addition to 30 mg/ml of paraquat for 10 minutes. EGCG (30 mg/ml) significantly (p < 0·05) reduced the hemolysis of erythrocytes exposed to paraquat29.
On the basis of these preliminary data, Dactavira and Dactavira plus, which consist of a combination of SOF, DCV, RBV, and EGCG might be superior to the standard of care and other IFN-containing regimens. Dactavira and Dactavira plus not only interfere with viral replication, but also inhibit virus entry and decrease the risk of anemia, sparing patients the rigors and toxicity of protracted IFN therapy. However, any such conclusions need to be established on a larger number of patients.
Limitations of this study include the small sample size, especially cirrhotics, and genotype subtypes were not done; results must be confirmed with larger studies. Although most cases now are treated with a RBV-free regimen because of RBV’s side effects, RBV has a crucial role in increasing SVR for treatment-expierenced and cirrhotic patients. Dactavira plus’ antihemolytic activity improves the tolerabiltity of the therapy.
In summary, 12 weeks’ therapy with the novel formulation Dactavira or Dactavira plus is safe and effective in both naïve non-cirrhotic and cirrhotic patients with genotype 4 HCV. Incorporation of EGCG in Dactavira and/Dactavira plus interferes with the viral entry mechanisms and may also play a role in enhancing efficacy and preventing relapse compared to the standard of care. In addition to potentially ehanced efficacy, Dactavira and Dactavira plus’ antihemoolytic activity may improve the safety and tolerability of the therapy.
Compliance with ethical requirements
The study (ClinicalTrials.gov Identifier NCT03186313, 14/06/2017) was conducted in accordance with the guidelines of Good Clinical Practice and was approved by the Independent Review Board of the Faculty of Medicine, Mansoura University. All patients provided written informed consent. Special thanks to the Egyptian Liver Research Institute and Hospital (ELRIAH) clinical trial team and Virothera LLC for supporting the manufacturing and QC for Dactavira and Dactavira plus clinical batches.
References
Cacoub, P. et al. Extrahepatic manifestations of chronic hepatitis C virus infection. Ther. Adv. Infect. Dis. 3, 3–14 (2016).
Polaris Observatory, H. C. V. et al. Global prevalence and genotype distribution of hepatitis C virus infection in 2015: a modelling study. Lancet Gastroenterol. Hepatol. 2, 161–176 (2017).
Honegger, J. R., Zhou, Y. & Walker, C. M. Will there be a vaccine to prevent HCV infection? Semin. Liver Dis. 34, 79–88 (2014).
Kwong, A. D., Kauffman, R. S., Hurter, P. & Mueller, P. Discovery and development of telaprevir: an NS3-4A protease inhibitor for treating genotype 1 chronic hepatitis C virus. Nat. Biotechnol. 29, 993–1003 (2011).
Welsch, C., Jesudian, A., Zeuzem, S. & Jacobson, I. New direct-acting antiviral agents for the treatment of hepatitis C virus infection and perspectives. Gut 61(Suppl 1), i36–46 (2012).
Shiha, G. et al. Ledipasvir/sofosbuvir with or without ribavirin for 8 or 12 weeks for the treatment of HCV genotype 4 infection: results from a randomised phase III study in Egypt. Gut 68, 721–728 (2018).
Waked, I. et al. Ombitasvir, paritaprevir, and ritonavir plus ribavirin for chronic hepatitis C virus genotype 4 infection in Egyptian patients with or without compensated cirrhosis (AGATE-II): a multicentre, phase 3, partly randomised open-label trial. Lancet Gastroenterol. Hepatol. 1, 36–44 (2016).
Gutierrez, J. A., Lawitz, E. J. & Poordad, F. Interferon-free, direct-acting antiviral therapy for chronic hepatitis C. J. Viral Hepat. 22, 861–870 (2015).
Fonseca-Coronado, S. et al. Specific detection of naturally occurring hepatitis C virus mutants with resistance to telaprevir and boceprevir (protease inhibitors) among treatment-naive infected individuals. J. Clin. Microbiol. 50, 281–287 (2012).
Elberry, M. H., Darwish, N. H. E. & Mousa, S. A. Hepatitis C virus management: potential impact of nanotechnology. Virol. J. 14, 88 (2017).
Ruane, P. J. et al. Sofosbuvir plus ribavirin for the treatment of chronic genotype 4 hepatitis C virus infection in patients of Egyptian ancestry. J. Hepatol. 62, 1040–1046 (2015).
Doss, W. et al. Sofosbuvir plus ribavirin for treating Egyptian patients with hepatitis C genotype 4. J. Hepatol. 63, 581–585 (2015).
Kayali, Z. & Schmidt, W. N. Finally sofosbuvir: an oral anti-HCV drug with wide performance capability. Pharmgenomics Pers. Med. 7, 387–398 (2014).
Bourliere, M., Oules, V., Ansaldi, C., Adhoute, X. & Castellani, P. Sofosbuvir as backbone of interferon free treatments. Dig. Liver Dis. 46(Suppl 5), S212–220 (2014).
Shiha, G., Soliman, R., ElBasiony, M., Hassan, A. A. & Mikhail, N. N. H. Sofosbuvir plus Daclatasvir with or without ribavirin for treatment of chronic HCV genotype 4 patients: real-life experience. Hepatol Int 12, 339–347 (2018).
Bristol-Myers Squibb Company, Daklinza (daclatasvir) prescribing information, https://packageinserts.bms.com/pi/pi_daklinza.pdf (2017).
Shiha, G., Soliman, R., Mousa, A. & Mousa, S. A novel single daily fixed dose combination of sofosbuvir 400 mg + ribavirin 1000 mg + EGCG 400 mg is superior to the standard of care as an anti-viral and safer causing less hemolysis in patients with chronic hepatitis C. J. Hepatol. 66, S500–S501 (2017).
Sheng, R., Gu, Z. L. & Xie, M. L. Epigallocatechin gallate, the major component of polyphenols in green tea, inhibits telomere attrition mediated cardiomyocyte apoptosis in cardiac hypertrophy. Int. J. Cardiol. 162, 199–209 (2013).
Ikeda, I. et al. Tea catechins with a galloyl moiety suppress postprandial hypertriacylglycerolemia by delaying lymphatic transport of dietary fat in rats. J. Nutr. 135, 155–159 (2005).
Calland, N. et al. Polyphenols inhibit hepatitis C virus entry by a new mechanism of action. J. Virol. 89, 10053–10063 (2015).
Kim, H. C., Chang, E. J. & Mun, K. C. Effects of epigallocatechin gallate on the hemolysis induced by cyclosporine. Transplant. Proc. 37, 2385–2386 (2005).
Dao Thi, V. L. et al. Characterization of hepatitis C virus particle subpopulations reveals multiple usage of the scavenger receptor BI for entry steps. J. Biol. Chem. 287, 31242–31257 (2012).
Barth, H. et al. Cellular binding of hepatitis C virus envelope glycoprotein E2 requires cell surface heparan sulfate. J. Biol. Chem. 278, 41003–41012 (2003).
Jiang, J., Wu, X., Tang, H. & Luo, G. Apolipoprotein E mediates attachment of clinical hepatitis C virus to hepatocytes by binding to cell surface heparan sulfate proteoglycan receptors. PLoS One 8, e67982 (2013).
Calland, N. et al. (-)-Epigallocatechin-3-gallate is a new inhibitor of hepatitis C virus entry. Hepatology 55, 720–729 (2012).
Chen, C. et al. (-)-Epigallocatechin-3-gallate inhibits the replication cycle of hepatitis C virus. Arch. Virol. 157, 1301–1312 (2012).
Lin, Y. T. et al. Green tea phenolic epicatechins inhibit hepatitis C virus replication via cycloxygenase-2 and attenuate virus-induced inflammation. PLoS One 8, e54466 (2013).
Chow, H. H. et al. Pharmacokinetics and safety of green tea polyphenols after multiple-dose administration of epigallocatechin gallate and polyphenon E in healthy individuals. Clin. Cancer Res. 9, 3312–3319 (2003).
Moses, K., Pepple, D. & Singh, P. The protective effect of epigallocatechin-3-gallate on paraquat-induced haemolysis. West Indian Med. J. 64, 186–188 (2015).
Acknowledgements
We appreciate Dr. Kelly Keating, Pharmaceutical Research Institute, for her excellent editing of this manuscript.
Author information
Authors and Affiliations
Contributions
G.S. designed the clinical trial and is the Principal Investigator. R.S. and M.E. conducted the clinical trial and did the patient enrollment and randomization. N.H.E.D. did the data analysis. S.A.M. contributed to the single tablet design and manufacturing and the design of the study and with G.S. contributed to the manuscript write up and data interpretation. All authors have approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
Gamal Shiha has been a Principal Investigator for Gilead and Abbvie. Reham Soliman has been an Investigator for Gilead and Abbvie. Mohamed Elbasiony has been an Investigator for Gilead. Shaker A Mousa has no conflict of interest other than helping HCV patients in underdeveloped countries have access to treatment at low to no cost. Noureldien H.E. Darwish declares no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shiha, G., Soliman, R., Elbasiony, M. et al. Addition of Epigallocatechin Gallate 400 mg to Sofosbuvir 400 mg + Daclatisvir 60 mg With or Without Ribavirin in Treatment of Patients with Chronic Hepatitis C Improves the Safety Profile: A Pilot Study. Sci Rep 9, 13593 (2019). https://doi.org/10.1038/s41598-019-49973-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-49973-6
This article is cited by
-
Novel combined single dose anti-hepatitis C therapy: a pilot study
Scientific Reports (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.