Abstract
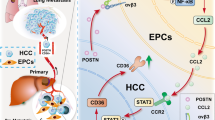
The prometastatic stroma generated through tumor cells/host cells interaction is critical for metastatic growth. To elucidate the role of ICAM-1 on the crosstalk between tumor and primary liver sinusoidal endothelial cells (LSECs) and hepatic stellate cells (HSCs), implicated in tumor adhesion and angiogenesis, we performed in vitro cocultures and an in vivo model of liver metastasis of colorectal cancer (CRC). ICAM-1 blockade in the LSECs decreased the adhesion and transmigration of tumor cells through an LSEC in vitro and vivo. Cocultures of C26 cells and LSECs contained higher amounts of IL-1β, IL-6, PGE-2, TNF-α and ICAM-1 than monocultures. C26 cells incubated with sICAM-1 secreted higher amounts of PGE-2, IL-6, VEGF, and MMPs, while enhanced the migration of LSECs and HSCs. HSCs cultures activated by media from C26 cells pretreated with sICAM-1 contained the largest amounts of VEGF and MMPs. C26 cell activation with sICAM-1 enhanced their metastasizing potential in vivo, while tumor LFA-1 blockade reduced tumor burden and LSECs and HSC-derived myofibroblasts recruitment. In vivo ICAM-1 silencing produced similar results. These findings uncover LSEC ICAM-1 as a mediator of the CRC metastatic cascade in the liver and identifies it as target for the inhibition of liver colonization and metastatic progression.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) represents one of the most prevalent malignancies worldwide1. Primary lesions are usually resectable, whereas prognosis worsens when distant metastases are detected. As many as 15% of CRC patients present hepatic metastasis at the time of diagnosis and 50% will develop liver metastasis after their primary resection2. Moreover, 30–40% of patients with advanced colorectal cancer will develop metastases to the liver only3, pointing out metastasis as a promising target for antitumor treatments to improve the survival of colorectal cancer patients.
Growing evidence supports a significant role for stromal cells of the host organ in the initiation and progression of the metastatic cascade4, and the implication of adhesion molecules in the crosstalk between tumor and host cells is currently under the spotlight5. Indeed, changes in the expression of adhesion molecules in the tumor cell surface facilitate tumor dissemination, colonization6 and metastatic growth in the liver7. However, the involvement of adhesion molecules from the host organ in the metastatic cascade needs further attention.
Formation of clinically relevant metastases depends on the generation of a favorable local microenvironment different from that of the neighboring tissues, which allows metastatic cell retention, survival, and growth8. An inflammatory response boosts tumor growth and metastasis and thus represents one of the hallmarks of cancer progression9. Tumor cells must interact with LSECs during early stages of liver colonization, in such a way that, as a result, a welcoming microenvironment for invading cells is generated. While the involvement of other liver-specific surface adhesion molecules such as E-selectin in liver metastasis has been reported10, the implications of host ICAM-1 in cancer development has remained almost unexplored. Intercellular adhesion molecule-1 (ICAM-1) is a transmembrane glycoprotein of the immunoglobulin (Ig)-like superfamily11 expressed constitutively in endothelial cells such as LSECs [Arteta et al., unpublished data]. Several inflammatory conditions enhance the expression of this molecule12. ICAM-1 interaction with its ligand, lymphocyte function associated 1 (LFA-1) mediates the adhesion and infiltration of leukocytes and immune cells into the hepatic tissue13. Furthermore, co-culture conditions induce ICAM-1 and LFA-1 upregulation in HUVECs and melanoma tumor cells, respectively14.
We have previously shown that activated LSECs release inflammatory factors after ICAM-1 ligation with tumor LFA-1, that correlates with a decreased lymphocyte cytotoxic activity15. Moreover, decreased expression of LFA-1 on tumor cells is associated with a reduction in liver metastasis of colorectal cancer in mice16. Indeed, a role for endothelial ICAM-1 on tumor transmigration could be envisioned as ICAM-1 ligation by LFA-1 receptor on bladder carcinoma cells leads to HUVEC cell retraction and transmigration17. Also, the stimulation of tumor cells with soluble ICAM-1 (sICAM-1) promotes tumor cell secretion of proangiogenic vascular endothelial growth factor (VEGF) in spheroid culture18. Besides, sICAM-1 stimulates tumor cell overexpression of prometastatic genes19. Additionally, our group has found that LSECs further contribute to the formation of a prometastatic microenvironment through their crosstalk with hepatic stellate cells (HSCs) at specific sites of circulating cancer cell arrest and transmigration across the endothelial barrier [Olaso and cols, unpublished]. An inflammatory environment promotes HSC transdifferentiation to myofibroblasts20. HSC-derived myofibroblasts contribute to the formation of a desmoplastic, proangiogenic stroma from the earliest state of micrometastasis formation through their secretion of migratory factors such as VEGF and metalloproteinases21. As a result, the interplay between tumor cells and activated LSECs and HSCs promote the transition from an early avascular micrometastatic growth to large, vascularized metastatic foci. Despite this, more studies are required to understand the mechanisms by which LSEC ICAM-1 influences the initial steps of liver metastasis while supporting and favoring disease progression. In the present study we aimed to elucidate the role of ICAM-1, produced by LSECs, on the crosstalk between tumor and host cells in early steps of liver metastasis.
Materials and Methods
Animals
Balb/c male mice (6–8 weeks old) were obtained from Charles River (Barcelona, Spain). Housing, care, and experimental conditions were carried out in conformity with institutional guidelines and national and international laws for experimental animal care. The animals were fed ad libitum with standard chow and water. All the proceedings were approved by the Basque Country University Ethical Committee (CEID) and by institutional, national and international guidelines regarding the protection and care of animals used for scientific purposes.
Cancer cell lines
All in vitro and in vivo experiments were conducted using the murine C26 colon adenocarcinoma (C26) cell line (also known as MCA-26, CT-26) syngenic with Balb/c mice and purchased from ATCC (LGC Standards S.L.U. Barcelona, Spain). C26 cells were cultured under standard conditions in RPMI-1640 supplemented with 10% heat-inactivated fetal bovine serum (FBS), penicillin (100 U/ml), streptomycin (100 µl) and amphotericin B (25 µg/ml). The replacement of cells was done no later than ten passages to prevent any change in their properties.
In vivo ICAM-1 silencing procedure
We used small-interfering RNAs against ICAM-1 (Life Technologies Inc; MD, USA) for the reduction of ICAM-1 expression in mice. ICAM-1 siRNA (200 ng) or scramble siRNA were diluted in sterile PBS (500 µl). The siRNA was injected in a final volume of 500 µl through the tail vein at very slow flow rate to avoid spilling. The siRNA was injected 48 and 24 hours before tumor cell inoculation. We also checked the levels of endothelial ICAM-mRNA and protein expression at the time of tumor injection. The intraperitoneal doses were given to reinforce the ICAM-1 silencing procedure. To avoid the stress generated by the procedure in awaken animals, we anesthetize the mice prior to the injection of the siRNA through the tail vein.
Isolation and culture of primary LSECs and HSCs
The isolation and culture of mouse LSECs and HSCs have been described elsewhere22. Briefly, the liver was perfused with collagenase buffer from Clostridium histolyticum (Sigma-Aldrich, St. Louis, MO, USA) and the obtained cell suspension was subjected to isopycnic centrifugation through a Percoll gradient (GE Healthcare, Chicago, IL, USA). The fraction enriched in LSECs was cultured onto 1 mg/ml collagen type I (Sigma-Aldrich, St. Louis, MO, USA) coated tissue culture plates at 3′5 × 105 cell/cm2 in RPMI-1640 media supplemented with 5% FBS, antibiotics, and antimycotics. HSCs were plated on uncoated plastic dishes. LSECs and HSCs were incubated at 37 °C, 5% CO2 for at least 2 hours in low serum media before any experimental use.
Establishment of LSEC cocultures with tumor cells
Tumor cells were added on top of primary LSEC monolayers at a ratio of 1:6 and cultured with RPMI-1640 supplemented with 5% serum and antibiotics for 3 hours. Next, fresh medium supplemented with 1% serum was added, and the cells were allowed to interact for 18 hours. Then, the culture supernatant was collected. In some experiments, ICAM-1 was blocked in primary LSEC using an anti-ICAM-1 antibody for 1 hour before the addition of tumor cells. Tumor cell suspensions were incubated for 1 hour with 1 µg/ml anti-CD11a or control irrelevant antibodies (Thermo Scientific; MD, USA) before seeding them on top of LSEC monolayers.
In vitro migration of primary LSEC and HSC
LSEC and HSC migration assay were carried out using Modified Boyden chambers. 2 × 105 primary LSECs and HSC were seeded onto 8 μm-diameter pore membranes (Greiner Bio-one) (coated with type I collagen for LSEC culturing) and allowed to adhere and spread for 3 hours before treatment. We then treated the cells with C26 cell-derived medium or sICAM-1 activated C26 cell-derived medium for 18 hours, and the migrated cell numbers were quantified. To analyze the effect of the tumor-activated HSC-derived medium, LSECs were treated for 18 hours at different conditions. For quantification, cells were fixed in 4% formalin, stained with Dapi (Sigma-Aldrich, St. Louis, MO, USA) and counted in the microscope under 20 high-power ten fields per membrane. Data are expressed relative to the migration of control LSEC and HSC through membranes.
Cancer cell adhesion to LSEC monolayers
C26 cells were labeled with 25 μM CFSE probe, (Thermo Scientific; MD, USA) by a 30 min incubation at 37 °C, followed by washing in the basal culture medium. Labeled cells were then resuspended to the experimental cell concentration of 2 × 105 cells/ml. In some experiments, primary LSECs were incubated for 1 hour with the anti-ICAM-1 antibody (Thermo Fisher Scientific; MD, USA). In another set of experiments, LSECs freshly isolated from livers treated with ICAM-1 siRNA silencing or with an scramble siRNA were plated in basal media. Then, tumor cells were seeded onto the LSEC cultures. The resulting co-cultures were maintained for 30 min at 37 °C. Then, total emitted fluorescence was measured using Ascent Fluoroskan (Labsystems S.A.C.). Then, co-cultures were extensively but delicately washed with culture medium to prevent removing of adherent cells. The fluorescence emitted by adhered cells was again measured. Finally, the percentage of adhered cells was calculated by the subtraction of background fluorescence as follows:
Transendothelial tumor cell migration assay
The transmigration, an assay that implicates that tumor cells are allowed to migrate through LSEC monolayers, was carried out using modified Boyden chambers (Greiner Bio-one). LSECs were isolated from either untreated mice or mice treated with either scramble siRNA or with ICAM-1 siRNA and cultured onto type I collagen-coated membranes of eight μm-diameter pore. LSECs were allowed to adhere for ninety minutes. Then, LSEC cultures were treated with or without ICAM-1 antibody for 1 hour, and 1 × 104 tumor cells seeded on top of the LSEC monolayers. Migrated C26 cells were fixed in 4% formalin, stained with crystal violet (Sigma-Aldrich, St. Louis, MO, USA) and ten fields per membrane were counted in the microscope under 20 high-power. Data are expressed relative to the migration of C26 cells through LSECs layers from control, or scramble siRNA treated mice.
ELISA assays
Tumor cells were seeded at a concentration of 1 × 105 on top of collagen type I coated plates. After 3 hours, cells were activated with sICAM-1 (200 ng/ml) for 10 hours and with a fresh basal medium for the following 18 hours. The tumor-derived media was then collected, and VEGF, IL-1β, IL-6, TNF-α, and PGE2 were quantified by ELISA (Thermo Fisher Scientific; MD, USA). HSC cultures were treated with tumor-derived conditioned media for 10 hours and with a fresh basal medium for the following 24 hours. Finally, VEGF in the media was measured by ELISA.
Gelatin and plasminogen/fibrinogen zymography
The presence of MMP-2 and MMP-9 media was determined by gelatin zymography as described previously23. In brief, culture supernatants were obtained from liver cells cultured under basal conditions or with media derived from C26 cell cultures, pretreated or not with sICAM-1. Cell culture supernatants were collected and run in 1% gelatin containing 10% bis-acrylamide gel. Gels were incubated overnight in developing buffer and stained with Coomassie Blue (BioRad, CA, USA). For uPA quantification, zymographies were carried out in gels containing gelatin and plasminogen. Images were taken through Quantity One program (BioRad, CA, USA).
Cancer cell early retention and experimental development of hepatic metastasis
Tumor cells were suspended at a concentration of 2 × 105 in PBS and were intrasplenically injected into anesthetized mice as previously described15. For retention studies, tumor cells were labeled with CFSE before the intrasplenic inoculation. After 24 hours, mice were euthanized, and the liver was removed and embedded in OCT (Tissue-Tek®, The Netherlands) before frozen in dry-ice. For hepatic metastasis, mice were sacrificed 14 days after tumor cell injection, the liver was collected and fixed in zinc-fixative solution, and paraffin embedded for histological analyses after H&E staining or embedded in OCT, frozen in dry ice, and kept at −80 °C until being processed for immunohistochemical analysis. The area of the organ occupied by the tumor cells was quantified in 10 μm thick sections. Three different regions of each liver were evaluated allowing 500 μm separation between each of them. Liver metastasis area was calculated as the area of metastatic foci per 100 mm2 of liver section. In vivo assay was performed twice with at least five mice per group.
Immunohistochemical analysis
For the recruitment of HSCs and LSECs, the quantification of the area occupied by αSMA and CD31 expressing cell within the tumors was carried out. After blocking the samples with 5% serum containing PBS and H2O2 for 10 minutes, liver samples were incubated with the primary mouse anti-human antibody against αSMA or rat anti-mouse CD31 for 2 hours (Thermo Fisher Scientific; MD, USA). Next, samples were washed, and the secondary antibody was added to the samples. Finally, HRP was utilized for the visualization of the expression of both markers.
Statistical analyses
Data are expressed as the mean ± standard deviation (SD) of three independent experiments. Statistical analysis was performed using SPSS version 13.0 (Professional statistic, Chicago, IL, USA). Individual comparisons were performed using two-tailed, unpaired Student t-test.
Ethical approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. All the proceedings were approved by the Basque Country University Ethical Committee (CEID) and by institutional, national and international guidelines regarding the protection and care of animals used for scientific purposes.
Results
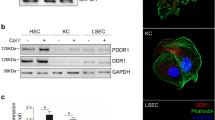
Involvement of endothelial ICAM-1 in tumor cell adhesion and transmigration
Circulating tumor cells must adhere to the vasculature of the target organ as a first step to metastasize. In the liver, LSECs represent the major interface between the portal blood and the parenchyma. Hence, adhesion and subsequent migration of blood borne tumor cells across LSECs is a crucial event to form liver metastasis. Ligation of ICAM-1 of LSECs to LFA-1 of inflammatory cells is key to allow extravasation of the latter cells across the sinusoidal lining13, but its role in the tumor transmigration to the liver tissue remains unknown. To study this, we observed the extent of C26 cell adhesion to primary monolayer cultures of LSECs pretreated or not with anti-ICAM-1 antibodies. A 40% reduction in C26 cell adherence to the LSECs caused by this treatment suggested that C26 cell-LSEC ICAM-1 adhesion is mediated by ICAM-1 on LSECs (Fig. 1A).
Tumor cell adhesion and transmigration through LSECs pretreated with anti-ICAM-1. (A) Freshly isolated mouse LSECs were treated with anti-ICAM-1 antibody or not (control) for 1 hour. Then, CFSE labeled tumor cells were added and allow to adhere for 30 minutes before total emitted fluorescence was measured. Followed by an intensive wash to remove non adherent cells, fluorescence emitted by adhered cells was measured. (B) Freshly isolated mouse LSECs were plated in 8 μm pore-membrane inserts. Then, tumor cells were seeded on top and allow to transmigrate through LSECs monolayer. Tumor cells transmigration across control and anti-ICAM-1 treated LSECs was quantified. Ten fields per membrane were counted in the microscope under 20 high-power for transmigrated C26 cell quantification. (C) Soluble ICAM-1 secretion was quantified by ELISA on the supernatants of LSECs-C26 cells cocultures. *p < 0,05.
Once tumor cells have adhered to LSECs, they must migrate across the endothelial layer to invade the liver parenchyma. Thus, next, we studied the implication of endothelial ICAM-1 in the ability of tumor cells to transmigrate across monolayers of primary cultured LSECs. Blockage of endothelial ICAM-1 reduced tumor transmigration by 50% (Fig. 1B). Furthermore, C26 cell attachment to LSECs stimulates the production of sICAM-1 by endothelial cells, amplifying ICAM-1 mediated response (Fig. 1C). In these experiments, we could not observe any detectable sICAM-1 on C26 cell supernatants (results not shown). This data, taken together, uncover a relevant role of host ICAM-1 in liver invasion by circulating tumor cells.
Involvement of host endothelial ICAM-1 in the inflammatory cytokine profile of tumor cell/LSEC co-cultures
Using an ELISA approach, we next examined the inflammatory cytokine profile of tumor cell/LSEC co-cultures. Media from C26 cell/LSEC co-cultures contained, on average, three-fold higher amounts of inflammatory IL-1β, IL-6, PGE2 and TNFα than media from LSEC monocultures (Fig. 2). To further analyze the implication of ICAM-1 in the inflammatory response generated by tumor cell interaction with LSEC during early stages of liver metastasis, we blocked ICAM-1 on LSEC primary cultures, co-cultured them with tumor cells and then determined the levels of soluble inflammatory factors in the resulting supernatants (Fig. 2A). Because LFA-1 is the principal canonical ligand for ICAM-1, in the second set of experimental conditions we blocked CD11a subunit of LFA-1 in the tumor cells with specific antibodies before co-culturing them with LSECs (Fig. 2B).
Secretion of inflammatory cytokines by tumor cell/LSEC cocultures following ICAM-1 or LFA-1 blockage in LSECs. Inflammatory cytokines were quatified in the supernatants of LSECs cocultured with C26 cells. (A) C26 cells were added to monolayers of LSECs either pre-treated or not with anti-CAM-1 antibody for 1 hour. (B) C26 cells were treated or not with antibody against LFA-1 before added to freshly solated LSECs. Supernatants from the resulting LSEC monocultures, LSEC/C26 cell cocultures and C26 cell monocultures were collected after 24 hours and the levels of IL-1β, PGE2, TNF-α and IL-6 were measured by ELISA. *p < 0,05.
Under both experimental conditions, disrupting endothelial ICAM-1/tumor LFA-1 interaction results in a dramatic reduction in the secretion of IL-1β, IL-6, PGE2 and TNFα into the co-culture supernatant. These findings identify tumor LFA-1 as the primary ligand for LSEC ICAM-1, and LSEC ICAM-1/tumor LFA-1 as a critical modulator of the inflammatory switch during circulating tumor cell liver colonization.
Tumor inflammatory and proangiogenic responses upon ICAM-1 activation
Given that LSECs secrete sICAM-1 as a response to C26 cell adherence (Fig. 1C), in the next set of experiments we aimed to determine whether sICAM-1 modifies tumor cell release of pro-metastatic soluble factors enabling tumor foci formation and growth. Exposure of C26 cells to sICAM-1 increased the production of VEGF, PGE2 and IL-6 in C26 cell monocultures by factors of 1.8, 2.7 and 4, respectively (Fig. 3A,C,D), compared to untreated monocultures. Moreover, sICAM-1 exposure also promoted tumor secretion of matrix remodeling factors uPA, MMP-2, and MMP-9 (Fig. 3B). As a whole, these results indicate that the activation of tumor cells by sICAM-1 enhance tumor secretion of proliferative, proangiogenic and matrix remodeling factors implicated in the metastatic development in the liver.
Secretion of angiogenic and inflammatory factors by ICAM-1-stimulated tumor cells. C26 cell cultures were treated or not (control) with soluble ICAM-1 for 10 hours. Afterwards, culture media were replaced by fresh media and cells were cultured for another 24 hours. The levels of VEGF, PGE2, and IL-6 were quantified by ELISA (A,C,D). Also, the expression of uPA, MMP-2 and MMP-9 by zymography were analyzed in sICAM-1- stimulated C26 cells (B). *p < 0,05.
Soluble factors from ICAM-1- activated tumor cells modulate the migration of primary LSECs and HSCs
Tumor growth requires the recruitment of supporting stromal cells. Thus, we studied the migratory potential of freshly isolated LSECs and HSCs in response to soluble factors secreted by sICAM-1 activated tumor cells. As illustrated in Fig. 4A, tumor-derived soluble factors promoted migration of LSECs 1.5-fold more than basal media. Migration of LSECs in response to supernatants from sICAM-1 pre-stimulated tumor cells was 2.5 fold higher than with basal media. Consistent with previous results23, HSCs cultured in the presence of tumor supernatants migrate 1.7-fold more than under basal conditions. Migration of HSCs after exposure to supernatants from sICAM-1 pre-stimulated tumor cells was 2.4 times higher than basal media (Fig. 4B). Therefore, tumor activation by sICAM-1 enhances the recruitment of LSECs and HSCs to the proximity of tumor cells invading the sinusoids.
Migration of primary LSECs and HSCs in response to soluble factors secreted by ICAM-1- activated tumor cells (A,B). Freshly isolated mouse LSECs (A) and HSCs (B) were cultured on top of 8 μm pore membrane inserts and allowed to migrate for 24 and 36 hours, respectively towards the supernatants derived from untreated or sICAM-1 stimulated C26 cells. Migrated cells stained with DAPI were counted in 10 20x-fields per well. *p < 0,05. Secretion of angiogenic factors by HSCs activated by sICAM-1-stimulated tumor cells (C–E). Tumor cell cultures were treated or not (control) with soluble ICAM-1 for 10 hours. Primary HSCs cultures were activated with supernatants from control or ICAM-stimulated tumor cell cultures. The media was changed for fresh medium, collected after 24 hours and analyzed for uPA, MMP-2 by zymography (C) and by ELISA for VEGF content (D). (E) Primary LSECs were seeded in 8 μm poremembranes and treated with tumor-activated HSC culture supernatants. Migrated cells stained with DAPI were counted in 10 fields per well. *p < 0,05.
Effect of ICAM-1 activation of tumor cells on the angiogenic potential of HSCs
Tumor cells promote HSC activation to a proangiogenic and desmoplasic myofibroblastic phenotype characterized by increased or de novo synthesis and secretion of proangiogenic VEGF and ECM remodeling proteases21. To analyze the significance of ICAM-1 in tumor-mediated HSC activation, freshly isolated HSCs were treated with tumor supernatants. Zymography analysis showed that HSCs cultures contained a higher expression of uPA and MMP-2 when exposed to tumor supernatants, and supernatants from C26 cells activated with sICAM-1 further promoted HSCs expression of these proteases (Fig. 4C). Similarly, VEGF secretion was elevated by 33% in HSCs cultured in the presence of tumor supernatants and further increased to 60% in HSCs treated with supernatants from sICAM-1 pre-treated tumor monocultures (Fig. 4D).
Tumor-activated HSCs facilitate LSECs migration in vitro21. In concordance with this, the supernatants from tumor activated HSCs increased the number of migrated LSECs by almost 1.7-fold compared to supernatants from untreated HSCs (Fig. 4E). This promigratory effect was enhanced up to 2.4-fold by supernatants from HSCs previously activated by supernatants collected from sICAM-1 pre-treated C26 cell cultures (Fig. 4E). In summary, supernatants from ICAM-1 activated C26 cells promote a proangiogenic phenotype in HSCs.
Effect of sICAM-1 or anti-CD11a antibody pretreatment of tumor cells on their pro-metastatic properties
Our in vitro data suggests that ICAM-1 modulates tumor cell migration and release of pro-migratory factors to recruit LSECs and HSCs. Thus, we next utilized our in vivo model of liver metastasis to analyze how in vitro alteration of tumor cell response to ICAM-1 modifies tumor ability to develop liver metastasis. Tumor cells were subjected in vitro to either stimulation with sICAM-1 or blockage of LFA-1 binding capacity to ICAM-1 with anti-CD11a antibody, prior to injecting them intrasplenically to syngenic mice. Fourteen days later, we observed a significant difference in the metastatic burden in the livers between the two experimental groups. In vitro sICAM-1 pre-stimulation of tumor cell resulted in a 35% higher metastatic colonization area of the liver than what we observed in livers receiving untreated tumor cells (Fig. 5A). On the contrary, the ability of anti-CD11a treated tumor cells to metastasize to the liver was found to be reduced by 50% in metastatic area in the liver compared to livers receiving untreated tumor cells, and by 65% when compared to metastasis generated by sICAM-1 pretreated tumor cells (Fig. 5A). These differences in the metastatic growth rate between the two experimental groups correlated with altered intratumoral contents of αSMA- and CD31-expressing cells. Intratumor liver foci neovessels contained activated myofibroblastic HSCs, detected by their de novo αSMA expression, and CD31-expressing activated LSECs21. Both αSMA and CD31 expression increased by 30% and 25%, respectively, in livers collected from mice bearing sICAM-1 treated tumor cells, indicating a higher number of activated HSCs and angiogenic LSECs in tumor foci originated from sICAM-1 treated tumor cells (Fig. 5B,C). As expected from our previous in vitro data, the livers collected from mice injected with tumor cells pretreated with anti-CD11a showed both reduced area occupied by metastatic foci and a 40% decrease in foci infiltration by activated HSCs and LSECs (Fig. 5B,C). Altogether, these results indicate that endothelial ICAM-1/tumor LFA-1 interplay facilitates liver metastasis through the recruitment of a prometastatic stroma composed of activated HSCs and angiogenic LSECs.
Effect of tumor cell treatment with sICAM-1 or with anti-CD11a antibodies in liver metastasis and angiogenesis. Tumor cells were treated in vitro with sICAM-1 or with anti-CD11a antibodies or led untreated before injection. Mice were intrasplenically injected with tumor cells. Fourteen days afterwards livers were analyzed for metastatic area (A), αSMA expression (B) and CD31 (C) expression. Three liver sections per mice, each one separated by 500 μm from the other were analyzed *p < 0,05.
Effect of in vivo ICAM-1 silencing on tumor retention in the liver. In vitro tumor cell adhesion and transmigration through LSEC monolayers from ICAM-1 silenced mice
Our in vitro and in vivo data point out ICAM-1 as a mediator of the inflammatory and angiogenic host responses during the early stages of liver metastasis. To further confirm these findings in vivo, we silenced LSEC ICAM-1 by siRNAs injection and then checked for in vitro adhesion and transmigration of tumor cells to LSECs isolated from those mice (See silencing efficiency in Suppl. Fig. 1). In concordance with our previous results using ICAM-1 antibodies (Fig. 1), adhesion of tumor cells to ICAM-1 silenced LSECs was 2-fold lower than tumor adhesion to LSECs expressing ICAM-1 derived from mice injected with scramble siRNA (Fig. 6A). The involvement of ICAM-1 in tumor cell adhesion to the hepatic sinusoidal wall was confirmed by in vivo retention assays. One day after intrasplenic inoculation, tumor cells are already retained in the liver16. At this time point, ICAM-1-silenced livers contain 50% fewer tumor cells than livers from mice injected with scramble siRNA (Fig. 6B). In concordance with these results, ex vivo transendothelial migration of tumor cells through freshly isolated LSECs from mice injected with siICAM-1 was 35% less than transmigration across LSECs from mice injected scramble siRNA (Fig. 6C).
Effect of in vivo silencing of ICAM-1 in the ex vivo tumor cell adhesion and transmigration through LSEC monolayers and in vivo tumor cell retention in the liver, liver metastasis and angiogenesis. Mice were injected with scramble siRNA or ICAM-1 siRNA through the tail vein. (A) 24 hours afterwards, LSEC were isolated and cultured for 3 hours. Then, CFSE-labeled tumor cells were added and allowed to adhered for 20 min. Then, tumor cell adhesion was quantified as shown before. (B) To quantify in vivo tumor cell retention to the liver, CFSE-labeled were i.s. injected into scramble and ICAM-1 siRNA treated mice. Livers were collected 24 hours after tumor cell injection and embedded in OCT. Retained tumor cells were quantified in 3 different 10 μm–thick liver sections/liver separated by 500 μm (n = 4 mice per group). (C) To quantify tumor cells-transmigration through LSECs, they were shed on top of LSEC monolayers cultured on top of 8 μm pore membrane inserts. Transmigrated tumor cells were stained with DAPI and count in 10 20x -fields per well. *p < 0,05, **p < 0,01. For metastasis development assay, mice were injected with scramble siRNA or ICAM-1 siRNA through the tail vein. Then, mice were injected intrasplenically with tumor cells. Fourteen days afterwards livers were analyzed for metastatic area (D), αSMA expression (E) and CD31 (F) expression. Three liver sections per mice, each one separated by 500 μm from the other were analyzed *p < 0,05.
Effect of in vivo ICAM-1 siRNA injection to mice in liver metastasis and angiogenesis
To further analyze the in vivo effect of reduced ICAM-1 expression in the liver in tumor formation, in the next set of experiments we examined metastatic tumor foci formation and growth in mice with silenced expression of LSEC ICAM-1. To do so, we injected mice with ICAM-1 siRNA 48 and 24 hours before tumor cell injection and three and six days after. Fourteen days after tumor cell-injection, histological analyses of the livers showed a drastic 75% drop in the area of liver tissue occupied by metastatic foci compared to livers from scramble siRNA treated mice (Fig. 6D). Tumor foci of ICAM-1 siRNA treated mice contained 55% less αSMA and 45% CD31 expression than control ones (Fig. 6E,F).
Discussion
ICAM-1 expression on tumor cells has been extensively studied and linked with their ability to invade adjacent and distant organs and with their increased metastatic potential in osteosarcoma, breast or colorectal cancer cells24,25,26. In this work, we report a crucial role for endothelial ICAM-1 in the in vitro C26 cell adhesion and transmigration through LSECs and the in vivo formation of a prometastatic inflammatory and angiogenic microenvironment. To our knowledge, this is the first report on the role of hepatic endothelial ICAM-1 on the early steps of liver colonization by CRC cells. We use several approaches to reinforce the strength of our findings. First, we use freshly isolated sinusoidal cells. As far as we know, this is the first report on ICAM-1 dependent tumor transmigration through freshly isolated LSECs and HSCs. The use of such cells is relevant because it resembles more closely what may happen in vivo. Second, we use several in vivo and in vitro approaches, such as in vitro blockage of ICAM-1/LFA-1 interaction by antibodies and in vivo iCAM-1 silencing, to analyze how ICAM-1 signals in LSECs. Each of them reinforced the others and allow us to conclude that host liver sinusoidal endothelial ICAM-1 is a mediator of the metastatic cascade in the liver.
Patients who suffer from colorectal cancer exhibit high serum levels of inflammatory mediators such as IL-1β, IL-6, TNF-α and PGE227,28. In our experimental model, enhanced secretion of IL-1β, PGE2, TNF-α, and IL-6 occurs following CRC cells/LSECs crosstalk in a tumor LFA-1/LSEC ICAM-1 interaction dependent fashion. C26 cells stimulation by either sICAM-1 administration or co-culture with LSECs results in tumor cell secretion of inflammatory PGE2 and IL-6, VEGF, uPA, MMP-2, MMP-9. Co-culture conditions also enhanced LSEC secretion of IL-1β, PGE2, TNF-α, and IL-6. In our hands, C26 cell cultures, treated or not with sICAM-1, do not contain detectable levels of TNFα or IL-1β, while LSECs do not secrete detectable levels of VEGF, uPA, MMP-2 or MMP-9. Enhanced PGE2 secretion in the C26 cell/LSECs co-cultures goes along with our previous studies, where we demonstrate that ligation of tumor LFA-1 with endothelial ICAM-1 drives COX-2 mediated LSECs secretion of IL-1β15. Furthermore, IL-6, and TNF-α secretion is also a COX-2 dependent event in LSECs (Arteta personal communication). In our model VEGF production is partially ICAM-1 dependent, which may explain why LSEC ICAM-1/tumor LFA-1 crosstalk modulates LSEC migration in vitro and LSEC angiogenic response inside the tumor foci.
Invading tumor cells recruit stromal cells to promote tumor growth. In the liver, HSCs and LSECs contribute to the angiogenic switch from avascular metastasis to clinically relevant, angiogenic ones. HSCs are one of the first cell types arriving into the proliferating tumor cell niche23. Using a melanoma model, we have shown that the crosstalk between the tumor cell and HSCs increases the release of pro-migratory factors for LSECs such as VEGF21. In this work, we found that soluble factors released from both tumor cells and HSCs in response to sICAM-1 favor LSECs migration. It is tempting to speculate that VEGF released by both C26 cells and HSCs following C26 cell ICAM-1 activation accounts for the enhanced movement of LSECs. Furthermore, the local environment generated by LSEC ICAM-1/tumor LFA-1 binding may directly contribute to HSCs activation. To this regard, IL-6 promotes HSC expression of myofibroblastic features such as αSMA and collagen I deposition28,29. ECM remodeling accompanies tumor and host cell migration. Herein, LSEC ICAM-1 mediates ECM remodeling by C26 cells and HSC-derived myofibroblasts. Excessive degradation of the matrix is one of the hallmarks of metastasis, and uPA, MMP-2, and MMP-9 play a role in human colorectal cancer progression, invasion, and metastasis30. IL-1β and IL6 upregulate MMP-2 and uPA in lung and gastric cancer31,32,33,34,35. Thus, our in vitro observations may reveal a direct link between LSEC ICAM-1 and matrix remodeling during liver colonization of CRC.
As expected from our in vitro data, metastatic area and recruitment of LSECs and HSCs to the tumor foci was lower in C26 cell metastasized livers collected from ICAM-1 siRNA treated mice or from C26 cells pretreated with CD11a antibodies, in line with our groups previous studies disrupting the LSEC ICAM-1/C26 cell LFA-1 crosstalk through β2 integrin blocking16. On the contrary, C26 cells stimulated by sICAM-1 developed more metastasis. These results are coherent with the present ones confirming the role of the interaction between host ICAM-1 and tumor LFA-1 in the development of liver metastasis.
Altogether, our results point out host endothelial ICAM-1 as a potent inflammatory and angiogenic promoter that mediates the infiltration of tumor cells and stromal cell recruitment into the tumor mass. These hosts ICAM-1 mediated tumor/endothelial crosstalk initiates inflammatory and angiogenic responses driving to liver metastasis.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Torre, L. A. et al. Global cancer statistics, 2012. CA Cancer J Clin. 65, 87–108 (2015).
Garden, O. J. et al. Guidelines for resection of colorectal cancer liver metastases. Gut. 55, 1–8 (2006).
Donadon, M., Ribero, D., Morris-Stiff, G., Abdalla, E. K. & Vauthey, J. N. New paradigm in the management of liver-only metastases from colorectal cancer. Gastrointest Cancer Res 1, 20–7 (2007).
Taddei, M. L., Giannoni, E., Comito, G. & Chiarugi, P. Microenvironment and tumor cell plasticity: An easy way out. Cancer Letters 341, 80–96 (2013).
Van den Eynden, G. G. et al. The Multifaceted Role of the Microenvironment in Liver Metastasis: Biology and Clinical Implications. Cancer Res 73, 2031–43 (2010).
Kim, K. J. et al. STAT3 activation in endothelial cells is important for tumor metastasis via increased cell adhesion molecule expression. Oncogene 36, 5445–5459 (2017).
Benedicto, A., Romayor, I. & Arteta, B. Role of liver ICAM-1 in metastasis. Oncol Lett. 14, 3883–3892 (2017).
Nielsen, S. R. et al. Macrophage-secreted granulin supports pancreatic cancer metastasis by inducing liver fibrosis. Nature Cell Biol. 18, 549–560 (2016).
Grivennikov, S. I., Greten, F. R. & Karin, M. Immunity, inflammation, and cancer. Cell 140(6), 883–99 (2010).
Brodt, P. et al. Liver endothelial E-selectin mediates carcinoma cell adhesion and promotes liver metastasis. Int J Cancer. 71, 612–9 (1997).
Van Den Engel, N. K., Heidenthal, E., Vinke, A., Kolb, H. & Martin, S. Circulating forms of intercellular adhesion molecule (ICAM)-1 in mice lacking membranous ICAM-1. Blood. 95, 1350–1355 (2000).
Cheng, J. et al. Inhibition of the expression of alpha-smooth muscle actin in human hepatic stellate cell line, LI90, by a selective cyclooxygenase 2 inhibitor, NS-398. Biochem Biophys Res Commun. 297, 1128–34 (2002).
Wong, J. et al. A minimal role for selectins in the recruitment of leukocytes into the inflamed liver microvasculature. J Clin Invest. 99, 2782–90 (1997).
Ghislin, S. et al. LFA-1 and ICAM-1 expression induced during melanoma-endothelial cell co-culture favors the transendothelial migration of melanoma cell lines in vitro. BMC Cancer 12, 455 (2012).
Arteta, B. et al. Colon carcinoma cell interaction with liver sinusoidal endothelium inhibits organ-specific antitumor immunity through interleukin-1-induced mannose receptor in mice. Hepatology 51, 2172–82 (2010).
Benedicto, A. et al. Decreased expression of the β2 integrin on tumor cells is associated with a reduction in liver metastasis of colorectal cancer in mice. BMC Cancer 17, 827 (2017).
Gorina, R., Lyck, R., Vestweber, D. & Engelhardt, B. β2 integrin-mediated crawling on endothelial ICAM-1 and ICAM-2 is a prerequisite for transcellular neutrophil diapedesis across the inflamed blood -brain barrier. J Immunol 192, 324–337 (2014).
Valcárcel, M. et al. Three-dimensional growth as multicellular spheroid activates the proangiogenic phenotype of colorectal carcinoma cells via LFA-1-dependent VEGF: implications on hepatic micrometastasis. J Transl Med. 6, 57–12 (2008).
Benedicto, A., Romayor, I. & Arteta, B. CXCR4 receptor blockage reduces the contribution of tumor and stromal cells to the metastatic growth in the liver. Oncol. Rep. 39, 2022–2030 (2018).
Olaso, E. & Friedman, S. L. Molecular regulation of hepatic fibrogenesis. J Hepatol. 29, 836–47 (1998).
Olaso, E. et al. Proangiogenic Role of Tumor-Activated Hepatic Stellate Cells in Experimental Melanoma Metastasis. Hepatology 37, 674–685 (2003).
Smedsrød, B. & Pertoft, H. Preparation of pure hepatocytes and reticuloendothelial cells in high yield from a single rat liver by means of Percoll centrifugation and selective adherence. J Leukoc Biol. 38, 213–30 (1985).
Olaso, E. et al. Tumor-dependent activation of rodent hepatic stellate cells during experimental melanoma metastasis. Hepatology 26, 634–42 (1997).
Itoh, H. et al. TET2-dependent IL-6 induction mediated by the tumor microenvironment promotes tumor metastasis in osteosarcoma. Oncogene 37, 2903–2920 (2018).
Wee, H., Oh, H. M., Jo, J. H. & Jun, C. D. ICAM-1/LFA-1 interaction contributes to the induction of endothelial cell-cell separation: implication for enhanced leukocyte diapedesis. Exp Mol Med. 41, 341–348 (2009).
Han, Y. H., Kee, J. Y. & Hong, S. H. Rosmarinic Acid Activates AMPK to Inhibit Metastasis of Colorectal Cancer. Front Pharmacol 9, 68 (2018).
Szkaradkiewicz, A. et al. Proinflammatory cytokines and IL-10 in inflammatory bowel disease and colorectal cancer patients. Arch Immunol Ther Exp (Warsz) 57, 291–4 (2009).
Yaqub, S. et al. Regulatory T cells in colorectal cancer patients suppress anti-tumor immune activity in a COX-2 dependent manner. Cancer Immunol Immunother. 57, 813–21 (2008).
Kagan, P., Sultan, M., Tachlytski, I., Safran, M. & Ben-Ari, Z. Both MAPK and STAT3 signal transduction pathways are necessary for IL-6-dependent hepatic stellate cells activation. PLoS One 12, e0176173 (2017).
Seetoo, D. Q., Crowe, P. J., Russell, P. J. & Yang, J. L. Quantitative expression of protein markers of plasminogen activation system in prognosis of colorectal cancer. J Surg Oncol 82, 184–193 (2003).
Mook, O. R. F., Frederiks, W. M. & Van Noorden, C. J. F. The role of gelatinases in colorectal cancer progression and metastasis. Bio Chem Biophys Acta 1705, 69–89 (2004).
Cheng, C. Y. et al. IL-1 beta induces urokinase-plasminogen activator expression and cell migration through PKC alpha, JNK1/2, and NF-kappaB in A549 cells. J Cell Physiol. 219, 183–93 (2009).
Lee, K. H. et al. IL-1β-stimulated urokinase plasminogen activator expression through NF-κB in gastric cancer after HGF treatment. Oncol Rep. 31, 2123–30 (2014).
Roomi, M. W., Kalinovsky, T., Rath, M. & Niedzwiecki, A. Modulation of MMP-2 and MMP-9 secretion by cytokines, inducers, and inhibitors in human glioblastoma T-98G cells. Oncol Rep. 37, 1907–1913 (2017).
Wang, L. et al. Cancer-associated fibroblasts enhance metastatic potential of lung cancer cells through IL-6/STAT3 signaling pathway. Oncotarget. 8, 76116–76128 (2017).
Acknowledgements
This work has been supported by a predoctoral grant from the University of the Basque Country to the principal author and from the Department of Industry and Research of the Basque Government SAIOTEK S-PE12UN075 and S-PE11UN043 to BA, and IT-487-09 to EO.
Author information
Authors and Affiliations
Contributions
A.B. wrote the manuscript and performed the majority of the experiments. A.H., I.R. and J.M. carried out different experiments and participated in data analisys. E.O., B.S. and B.A. designed the project and prepared the paper. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Benedicto, A., Herrero, A., Romayor, I. et al. Liver sinusoidal endothelial cell ICAM-1 mediated tumor/endothelial crosstalk drives the development of liver metastasis by initiating inflammatory and angiogenic responses. Sci Rep 9, 13111 (2019). https://doi.org/10.1038/s41598-019-49473-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-49473-7
This article is cited by
-
Neutrophil extracellular traps facilitate cancer metastasis: cellular mechanisms and therapeutic strategies
Journal of Cancer Research and Clinical Oncology (2023)
-
Constitutively active Lyn kinase causes a cutaneous small vessel vasculitis and liver fibrosis syndrome
Nature Communications (2023)
-
iMAP: integration of multiple single-cell datasets by adversarial paired transfer networks
Genome Biology (2021)
-
Role of liver sinusoidal endothelial cells in liver diseases
Nature Reviews Gastroenterology & Hepatology (2021)
-
Silencing of sinusoidal DDR1 reduces murine liver metastasis by colon carcinoma
Scientific Reports (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.