Abstract
Microbial-derived short-chain fatty acids (SCFA) acetate, propionate and butyrate may provide a link between gut microbiota and whole-body insulin sensitivity (IS). In this cross-sectional study (160 participants, 64% male, BMI: 19.2–41.0 kg/m2, normal or impaired glucose metabolism), associations between SCFA (faecal and fasting circulating) and circulating metabolites, substrate oxidation and IS were investigated. In a subgroup (n = 93), IS was determined using a hyperinsulinemic-euglycemic clamp. Data were analyzed using multiple linear regression analysis adjusted for sex, age and BMI. Fasting circulating acetate, propionate and butyrate concentrations were positively associated with fasting GLP-1 concentrations. Additionally, circulating SCFA were negatively related to whole-body lipolysis (glycerol), triacylglycerols and free fatty acids levels (standardized (std) β adjusted (adj) −0.190, P = 0.023; std β adj −0.202, P = 0.010; std β adj −0.306, P = 0.001, respectively). Circulating acetate and propionate were, respectively, negatively and positively correlated with IS (M-value: std β adj −0.294, P < 0.001; std β adj 0.161, P = 0.033, respectively). We show that circulating rather than faecal SCFA were associated with GLP-1 concentrations, whole-body lipolysis and peripheral IS in humans. Therefore, circulating SCFA are more directly linked to metabolic health, which indicates the need to measure circulating SCFA in human prebiotic/probiotic intervention studies as a biomarker/mediator of effects on host metabolism.
Similar content being viewed by others
Introduction
In obesity and type 2 diabetes mellitus (T2DM), alterations in the gut microbiota composition and functionality may contribute to disease aetiology. The gut microbiota ferments indigestible carbohydrates (e.g. dietary fibres) and major end-products thereof are the short- chain fatty acids (SCFA) acetate, propionate and butyrate1. Acetate, propionate and butyrate are present in the colon in a ratio of approximately 3:1:1, respectively2,3. Most butyrate is utilized by colonocytes as energy source4. Via the portal vein, SCFA reach the liver where acetate and propionate are metabolized and partly oxidised or used as substrate in gluconeogenesis and lipogenesis5. Consequently, a small proportion of microbial-derived SCFA enters the peripheral circulation whereby acetate reaches the highest concentrations compared to propionate and butyrate6,7. SCFA are ligands to G-protein coupled receptors (GPR) 41 and 43, which are expressed on intestinal, adipose, skeletal muscle, liver and pancreatic tissues8,9,10, indicating their important role in the crosstalk between the gut and peripheral tissues. Several rodent studies showed that oral, intravenous and colonic infusion of SCFA as well as microbial-derived SCFA beneficially affect the functioning and metabolism of the aforementioned tissues and consequently improve insulin sensitivity, substrate metabolism and body weight regulation11. In humans, distal colonic acetate infusions increased fasting fat oxidation, energy expenditure, and peptide YY (PYY) secretion whilst whole-body lipolysis was decreased12,13. Other acute studies show decreased circulating free fatty acid (FFA) concentration after rectal SCFA infusion in healthy participants14,15. In addition, 24 weeks of 10 g/day inulin propionate ester protected against body weight gain as compared to inulin only in overweight individuals16. Potential mechanisms may include a SCFA-induced inhibition of energy intake possibly mediated via the stimulation of glucagon-like peptide 1 (GLP-1) and PYY secretion, increased intestinal gluconeogenesis, increased skeletal muscle fat oxidation and improved lipid buffering capacity of adipose tissue11. However, increased microbial-derived acetate formation has been associated with increased body weight gain and insulin resistance in diet-induced obese rats17. Additionally, increased faecal SCFA have been reported in overweight and obese compared to lean participants2,3,8,18,19, yet it is difficult to interpret the latter data since faecal SCFA reflect the net result of colonic production and absorption20,21. Even though faecal SCFA are commonly used as an indicator of microbial fermentation, faecal SCFA may not accurately reflect in vivo colonic fermentation since approximately 95% of colonic SCFA are absorbed and only the remaining 5% are excreted in feces22,23,24,25.
To obtain more information on the validity of faecal SCFA as biomarker for metabolic health effects, the associations between faecal and circulating SCFA concentrations and parameters of metabolic health were studied in a relatively large cohort of 160 participants with a wide range of body mass indices (BMI) and glucometabolic status. Using multiple regression analysis, we analysed the relationship between faecal and fasting circulating SCFA with fasting glucose, insulin, circulating lipids (free fatty acids (FFA), triacylglycerols (TAG), glycerol), insulin resistance index (homeostasis model assessment of insulin resistance (HOMA-IR)), gut hormone concentrations (PYY, GLP-1), fasting substrate utilization and inflammation markers including lipopolysaccharide-binding protein (LBP), tumour necrosis factor alpha (TNF-α), interleukin 6 (IL-6) and interleukin 8 (IL-8). We further investigated the relationship between faecal and fasting circulating SCFA profiles and peripheral insulin sensitivity index (M-value) as measured via the gold standard hyperinsulinaemic-euglycemic clamp technique.
Results
Mean age of the participants was 49.6 ± 14.7 years and 66.2% of participants were male with a mean BMI of 29.8 ± 4.4 kg/m2, a mean fasting glucose of 5.6 ± 0.6 mmol/L and a mean HOMA-IR of 3.7 ± 1.5 (Table 1). In the subgroup, peripheral (M-value) was measured in 93 overweight to obese, prediabetic men (n = 72) and women (n = 21) with mean age of 59.0 ± 7.1 years and a mean BMI of 31.8 ± 3.1 kg/m2, respectively.
Associations between faecal and circulating SCFA concentrations
Faecal acetate and butyrate were not associated to their respective circulating concentrations, while faecal propionate was positively associated with circulating propionate (standardized (std) std β = 0.262, P = 0.002).
Circulating, but not faecal, SCFA are associated with BMI
Faecal acetate was positively associated with BMI (std β = 0.245, P = 0.004), however, after adjustment for age and sex, the association was not significant anymore (std β adj = 0.092, P = 0.214). Faecal propionate and butyrate were not significantly associated with BMI with or without adjustment for age and sex (faecal butyrate std β = 0.162, P = 0.055, faecal propionate std β = 0.023, P = 0.746). In contrast, circulating butyrate and propionate were significantly inversely related to BMI, also after adjustment for age and sex (circulating butyrate std β = −0.599, P < 0.001, circulating propionate std β = −0.290, P < 0.001, Supplementary Figure 1 K,L). Circulating acetate was negatively associated with BMI (std β = −0.285, P < 0.001), which was not significant anymore after adjustment for age and sex (std β = −0.115, P = 0.108).
Faecal SCFA were not related to metabolic parameters
None of faecal SCFA were significantly associated with fasting GLP-1, PYY, FFA, TAG, glycerol, glucose, insulin concentrations, HOMA-IR, inflammatory markers or fasting substrate oxidation either with or without adjustment for age, sex and BMI. In the subgroup analysis faecal SCFA were not associated with peripheral insulin sensitivity (Table 2).
Fasting, circulating SCFA were related to fasting GLP-1, lipid metabolites and insulin sensitivity
All three circulating SCFA were positively associated with fasting GLP-1 concentrations (Table 3). Additionally, circulating acetate, propionate and butyrate were negatively associated with fasting glycerol, TAG and FFA, respectively. Also, circulating butyrate was negatively associated with fasting glucose. These relationships remained significant after adjustment for age, sex and BMI (Table 3, Supplementary Figure 1).
Circulating SCFA were not associated with fasting PYY, LBP, IL-6, IL-8 and TNF-α. Furthermore, circulating SCFA were not related to fat and carbohydrate oxidation, expressed as percentage of energy expenditure. In the subgroup analysis of overweight/obese, prediabetic individuals, peripheral insulin sensitivity was measured using the M-value derived from the euglycemic-hyperinsulinaemic clamp technique. We found that circulating acetate was negatively associated with peripheral insulin sensitivity (M-value) whereas circulating propionate was positively related to peripheral insulin sensitivity (Table 3, Supplementary Figure 1). The relationships between circulating SCFA and insulin sensitivity remained significant after adjustment for age, sex and BMI.
Discussion
We investigated the relationship between faecal and fasting circulating SCFA with fasting plasma metabolites, gut hormones, substrate metabolism and inflammatory markers in a cohort with a wide range of BMI and glucometabolic status. This study shows that only circulating but not faecal SCFA concentrations were related to fasting plasma glucose, FFA, TAG and glycerol, GLP-1 and insulin sensitivity, also after adjustment for age, sex and BMI. Contrary to previous human studies, faecal SCFA were not related to BMI, whereas circulating butyrate and propionate were inversely associated with BMI. Circulating plasma propionate seems to be the most reflective of its respective faecal concentrations, whilst faecal acetate and butyrate were not related to their respective circulating concentrations. In line, previous literature reports that SCFA flux into the circulation and uptake in peripheral tissues rather than microbial SCFA production per se is of importance for metabolic health26,27,28. Our data emphasize the need to measure circulating SCFA in human prebiotic/probiotic intervention studies as a biomarker/mediator of effects on host metabolism.
To our knowledge, this is the first study providing evidence that fasting circulating SCFA are positively associated with fasting plasma GLP-1 in humans. High colonic SCFA production is linked to increased GLP-1 and PYY secretion through binding of SCFA to GPR41/43 on the enteroendocrine L-cell29. Further, a one-year dietary fiber intervention (wheat bran, 24 g/d) increased circulating SCFA concentrations accompanied by increased levels of GLP-1 concentrations in hyperinsulinemic participants30. Yet, there is little known about the contribution of circulating SCFA to GLP-1 secretion during the fasted state. Circulating SCFA may stimulate GLP-1 secretion from the visceral, basolateral side of enteroendocrine L-cells as observed in isolated rat colons31. Besides enteroendocrine L-cells, pancreatic α-cells have been suggested to contribute to systemic GLP-1 concentrations in the fasted state32,33, but whether circulating SCFA act as stimuli for GLP-1 secretion warrants further investigation.
In contrast to GLP-1, we did not find an association between circulating and faecal SCFA with fasting PYY. This is in contrast to human and in vitro studies reporting a stimulatory effect of SCFA on PYY secretion12,34,35, however to what extent SCFA and/or dietary fibres contribute to fasting PYY secretion remains to be investigated. Although the mechanisms still remain to be elucidated, the present data indicate that, despite being the net result of production, uptake and tissue utilization, circulating SCFA are more directly linked to metabolic health as compared to faecal SCFA.
In our study population, only circulating, but not faecal SCFA were associated with fasting plasma metabolites. Circulating acetate was negatively associated with fasting free glycerol, an indicator of whole-body lipolysis. This is consistent with in vitro and human in vivo studies reporting that acetate has an anti-lipolytic effect13,36,37,38. This may be beneficial for metabolic health in the long term, since partial inhibition of adipose tissue lipolysis may reduce systemic lipid spillover thereby attenuating ectopic lipid accumulation39. Further, circulating propionate was negatively associated with fasting TAG, which might be explained by the activating effect of propionate on lipoprotein lipase (LPL) in adipose tissue leading to increased TAG extraction as shown in vitro40. Furthermore, circulating butyrate was negatively associated with fasting FFA concentrations. In vitro data about the lipolytic effect of butyrate are contradictive showing pro- and antilipolytic effects of butyrate in white adipose tissue models38,41. Thus, circulating SCFA may be negatively related to systemic glycerol or FFA and/or TAG suggesting that increased circulating SCFA may reduce systemic lipid overflow with a potential beneficial effect on ectopic lipid accumulation and insulin sensitivity.
Nevertheless, with respect to markers of insulin sensitivity, neither fasting circulating nor faecal SCFA were related to fasting insulin or HOMA-IR in the total study population. Yet, fasting circulating butyrate, but not acetate and propionate, was negatively associated with fasting glucose. This is consistent with rodent studies showing that butyrate administration may have glucose lowering effects and may improve insulin sensitivity in the postprandial state42,43. In obesity, insulin resistance and T2DM, the abundance of butyrate-producing bacteria is reduced, which may explain to some extent the inverse association between circulating butyrate and fasting glucose in our study44,45,46.
In the subgroup analysis including prediabetic individuals with obesity, circulating acetate was negatively associated with peripheral insulin sensitivity. This is in contrast with previous rodent studies reporting a beneficial role of acetate on insulin sensitivity34 and with two small-scale human cross-sectional studies including obese women or morbidly obese individuals reported either none or a positive association of circulating acetate and insulin sensitivity measured via hyperinsulinemic-euglycemic clamp, respectively47,48. Additionally, when acetate is administered colonically, overweight participants showed increases in fasting fat oxidation, energy expenditure, and PYY secretion12,13, reflective of positive effects on metabolic health. Interestingly, a kinetic study showed that intravenously infused acetate remains longer in the circulation in individuals with T2DM suggesting a disturbed acetate tissue uptake and metabolism in the context of metabolic disorders34. Further, exogenous and endogenous acetate production but not colonic acetate absorption differed between hyperinsulinemic and normoinsulinemic individuals after rectal infusion of sodium-acetate37,49,50. Thus, our findings may reflect an altered endogenous acetate metabolism rather than an altered microbial-derived acetate production in metabolically compromised individuals. In contrast to fasting circulating acetate, fasting circulating propionate was positively associated with clamp-derived insulin sensitivity. Propionate has been reported to stimulate glucose uptake in 3T3-L1 adipocytes and C2C12 skeletal muscle cells in vitro and improve insulin sensitivity (HOMA-IR) in mice fed a high fat diet51,52. Possible mechanisms include an increase in peripheral glucose uptake via increased GPR41 stimulation, suppression of hepatic de novo lipogenesis and increase formation of beneficial odd chain fatty acids in the liver53.
The main limitation of our study is the cross-sectional design, which limits causal suppositions. Further, we cannot account for endogenous SCFA production, splanchnic and liver extraction or tissue utilization in this study54,55. Secondly, measures of GLP-1 and SCFA in the postprandial state would have been valuable. However, the study’s major strength is the availability of faecal and fasting circulating SCFA in combination with metabolic markers in a relatively large cohort with a broad range of BMI and metabolic health status. This enabled us to investigate the relationship between faecal and fasting circulating SCFA concentrations with markers of lipid and energy metabolism as well as insulin sensitivity measured by the gold standard hyperinsulinemic-euglycemic clamp. For the first time, we confirmed that fasting circulating but not faecal SCFA were related to whole-body lipolysis, fasting GLP-1 and insulin sensitivity in the fasted state. Furthermore, our study calls for urgently needed mechanistic studies in humans concerning the relationship between SCFA, GLP-1 secretion and lipid metabolism.
In conclusion, our data show that circulating but not faecal SCFA are linked to circulating GLP-1 concentrations, whole-body lipolysis and peripheral insulin sensitivity in humans. Of note, this highlights that circulating SCFA are more directly linked to metabolic health parameters. Therefore, our data indicate the need to measure circulating SCFA as a biomarker/mediator of effects on host metabolism in future human prebiotic/probiotic intervention studies. This may provide interesting leads for future research, which should aim to modulate the SCFA availability in the systemic circulation and its impact on peripheral tissue function
Methods
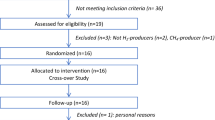
Study participants
This cross-sectional analysis included 160 Caucasian men and women aged 20–70 years with a BMI between 19.2 and 41.0 kg/m2 from the general population in the vicinity of Maastricht, The Netherlands during August 2013 and December 2016. Individuals had normoglycemia, impaired fasting glucose (IFG, ≥5.6 mmol/L) and/or impaired glucose tolerance (IGT, 2 hour plasma glucose of 7.8–11 mmol/L after 75 g oral glucose challenge) according to the diagnostic criteria of the American Diabetes Association, 201056. Eligibility of the participants was assessed via a general health questionnaire, medical history and anthropometry during an intitial screening visit. Exclusion criteria were as follows: use of antibiotics, prebiotics, or probiotics 3 months before the study, diagnosis of T2DM, gastrointestinal or cardiovascular diseases, abdominal surgery, participants with life expectancy shorter than 5 years and participants following a hypocaloric diet. Participants did not use β-blockers, lipid- or glucose-lowering drugs, anti-oxidants, or chronic corticosteroids. All protocols were reviewed and approved by the local Medical Ethical Committee (MUMC+) and conducted in accordance with the Declaration of Helsinki (revised version, October 2008, Seoul, South Korea). Written informed consent was obtained from all participants.
Study design
This cross-sectional analysis included metabolic parameters as well as faecal and fasting circulating SCFA concentrations of previously performed intervention studies12,13,57,58,59. In the present study, we collated and analyzed study data at baseline and thus prior to the respective interventions. In all studies, sample collection was performed after an overnight fast, and measurements were conducted according to the same standard operating procedures. Two days prior to the baseline investigation day, participants were asked to refrain from intense physical activity and alcohol consumption, and to collect a faecal sample. In the evening before the investigation day, the participants consumed a standardized low-fiber meal.
Used data sets
The data set included baseline data from the following intervention human in vivo studies. These include an intervention study in prediabetic, overweight-obese individuals on the effect of antibiotics on insulin sensitivity (Clinical trial No. NCT02241421) (3), an intervention study in prediabetic, overweight-obese individuals on the effect of dietary fiber (galacto-oligosaccharides) on insulin sensitivity (Clinical trial No. NCT02271776) (4), an intervention study in normoglycemic, normal to overweight individuals on the effect of dietary fibers on gastrointestinal transit (Clinical trial No. NCT02491125) (5), and lastly two acute studies investigating the effect of different mixtures of SCFA in normoglycemic, overweight to obese individuals on human substrate and energy metabolism (Clinical trial No. NCT01826162 (6), Clinical trial No. NCT01983046 (7)).
Baseline investigation day
After an overnight fast (>10 h), participants came to the laboratory by car or public transport. Anthropometry was measured including height, weight and waist to hip ratio. After inserting a cannula into the antecubital vein, blood samples were taken to measure plasma metabolites, hormones and inflammatory markers in the fasted state. After the blood sampling, participants were in a resting, half-supine position and fasting substrate oxidation was measured for 30 min using an open circuit ventilated hood system (Omnical, MUMC+, Maastricht, the Netherlands). Fat and carbohydrate oxidation were calculated according to the equations of Weir and Frayn60,61, assuming that protein oxidation accounted for 15% of total energy expenditure.
Hyperinsulinaemic-euglycaemic clamp
Peripheral insulin sensitivity was determined in a subgroup of overweight/obese, prediabetic individuals via hyperinsulinaemic-euglycemic clamps as previously described57,58. In short, a cannula was inserted into an antecubital vein for infusion of glucose and insulin. To measure blood glucose, a second cannula was inserted into a superficial dorsal hand vein, which was arterialized by placing the hand into a hotbox (~50 °C). A priming dose of insulin infusion (Actrapid, Novo Nordisk, Gentofte, Denmark) was administered during the first ten min (t0–t10 min) and insulin infusion was thereafter continued at 40 mU/m2/min for 2 h (t10–t120 min). By variable infusion of a 20% glucose solution, plasma concentrations were maintained at 5.0 mmol/L. Peripheral insulin sensitivity (M-value, mg*(kg*min)−1 was calculated from the mean glucose infusion rate during the steady-state of the clamp (last 30 min, stable blood glucose concentration at 5.0 mmol/L)62. A high M-value represents high insulin sensitivity (i.e., more glucose needs to be infused to maintain euglycemia during insulin infusion).
Analysis of faecal and circulating SCFA
Faecal samples were collected at home and stored in the subjects’ freezer at −20 °C maximum of two days before the baseline investigation day, transported on dry ice, and stored on arrival at the university at −80 °C. Faecal acetate, propionate, and butyrate were measured by gas chromatography-mass spectrometry (Dr. Stein and Colleague Medical Laboratory, Mönchengladbach, Germany) as previously described63. Plasma sample preparation for circulating SCFA analysis were performed as reported previously64. In short, deproteinization was performed by mixing 1 part plasma (v/v) with 2 parts methanol acidified with 1.5 mmol/l hydrochloric acid. Subsequently, samples were vortex-mixed vigorously and immediately centrifuged at 50000 × g in a model Biofuge Stratos (Hereaus, Dijkstra Vereenigde, Lelystad, the Netherlands) for 15 min. at 4 °C. 100 μl aliquots of the clear plasma supernatant were transferred into glass micro-insert vials and stored in the Combi-Pal until analysis. Samples were calibrated against external standards. The reversed phase separation was performed on a X-select ODS 2.5 µm column (150 mm × 2.1 mm I.D., Waters, Breda, the Netherlands), mounted in a Mistral Spark column oven (Separations, H.I. Ambacht, the Netherlands), set to 45 °C. Samples were completely separated from other components into the individual SCFA in a 25 min. gradient cycle between an aqueous 1 mmol/l solution of sulfuric acid and ethanol. Post-column, the solvent pH was enhanced to about 9, by mixing with 150 mmol/l ammonia in ethanol to maximize negative ionization. Samples were processed using a Combi-PAL sample processor (Interscience, Breda, the Netherlands) with Peltier chilled sample storage compartments set to 10 °C. The system was equipped with a 50 µl sample loop. Separated SCFA were detected using a model LTQ XL linear ion trap mass spectrometer (Thermo Fisher Scientific, Breda, the Netherlands), equipped with an ion-max electrospray probe. The MS was operated in MS-MS full scan negative mode.”
Blood collection and biochemical analysis
Blood was collected in pre-chilled EDTA tubes (0.2 mol/L EDTA; Sigma, Dorset, UK) for SCFA, insulin, glucose, FFA, TAG, free glycerol, LBP, GLP-1, TNF-α, IL-6 and IL-8 analyses during fasting conditions. For GLP-1 and PYY analysis, 20 μl of dipeptidyl peptidase-IV inhibitor (Milipore Merck, Billerica, MA, USA) was added to EDTA and Aprotinin (Becton Dickinson, Eysins, Switzerland) tubes, respectively. Samples were centrifuged at 3500 g, 4 °C for 10 minutes; plasma was aliquoted and directly snap-frozen in liquid nitrogen and stored at −80 °C until analysis. Plasma glucose concentrations were determined using commercially available reagent kit (Glucose Hexokinase CP, Horiba ABX Pentra, Montpellier, France) involving a two-step enzymatic reaction with hexokinase followed by Glucose-6-phosphate-dehydrogenase resulting in D-gluconate-6-phosphate. The colorimetric reaction was measured using an automated spectrophotometer (ABX Pentra 400 autoanalyzer, Horiba ABX Pentra). Plasma FFA concentrations were measured using a commercially available kit (NEFA-HR(2) assay, Wako, Sopachem BV, Ochten, the Netherlands) with a two-step enzymatic reaction involving acylation of Coenzyme(Co) A followed by acyl-CoA oxidase resulting in the production of hydrogen peroxide as substrate that in the presence of peroxidase yields a blue purple pigment, measured with a colorimetric reaction using an automated spectrophotometer (ABX Pentra 400 autonalyzer, Horiba ABX Pentra). Plasma TAG were determined using a commercially available kit (Triglycerides CP, Horiba ABX Pentra) based on enzymatic reactions involving lipoprotein lipase, glycerolkinase and glycerol-3-phosphate oxidase resulting in the production of hydrogen peroxide as substrate of a colorimetric reaction measured using the automated spectrophotometer (ABX Pentra 400 autonalyzer, Horiba ABX Pentra). Plasma glycerol was measured after precipitation with an enzymatic assay (Enzytec TM Glycerol, Roche Biopharm, Basel, Switzerland) involving phosphorylation of glycerol to L-glycerol-3-phosphate by glycerokinase and the colorimetric reaction is measured using an automated spectrophotometer (Cobas Fara, Roche Diagnostics, Basel, Switzerland). Plasma insulin was determined with a commercially available radioimmunoassay (RIA) kit (HI-14K Human Insulin specific RIA, Millipore Merck) according to the manufacture’s protocol. Plasma IL 6, IL-8 and TNF-α were determined with an commercialy available enzyme-linked immunosorbent assay (ELISA) kit (Human Proinflammatory II 4-Plex Ultra-Sensitive kit, Meso Scale Diagnostics, MD, USA). Plasma samples were assayed for total GLP-1 immunoreactivity using an antiserum that reacts equally with intact GLP-1 and the primary (N-terminally truncated) metabolite as previously described65. PYY concentrations were determined using a commercially available RIA kit (Human PYY (3–36) Specific RIA, Millipore Merck). Plasma LBP was measured as previously described66. In short, plates (Greiner Mocrolon 600 high binding; Sigma Aldrich, St. Louis, MO) were coated with polyclonal anti-human LBP antibodies. Diluted plasma samples (1:5000) and a standard dilution series with recombinant LBP were added to the plate. Detection occurred with a biotinylated polyclonal rabbit anti-human LBP IgG, followed by peroxidase-conjugated streptavidin and substrate. The detection limit for the LBP assay was 200 pg/ml.
Statistical analysis
Normality of data was assessed with the Gaussian distribution and Kolmogorov-Smirnov procedure, and ln or Z-score transformation was used if assumption of normality was not met. HOMA-IR was calculated as previously described67. In case of missing data, the participant was excluded from the analysis. Multicollinearity was checked using variance inflation factor index <10. First, we used simple linear regression to investigate the associations between faecal and circulating concentrations of acetate, propionate and butyrate (as dependent variables) and metabolic parameters (as independent variables) i.e. insulin sensitivity (M-value), insulin resistance (HOMA-IR), circulating glucose, insulin, circulating lipids (TAG, FFA and glycerol), circulating inflammatory markers (IL-6, IL-8, TNF-α and LBP) and fasting substrate oxidation. Subsequently, we used multiple linear regression to test whether the associations between faecal and circulating SCFA and the aforementioned metabolic parameters were independent of the covariates sex, age and BMI. All data were analysed using SPSS 22.0 (IBM, Armok, U.S.) with significance set at P < 0.05.
Ethics approval
The studies summarized in this manuscript were approved by the Medical Ethics Committee of Maastricht University Medical Centre and was conducted according to the ethical standards of the Helsinki Declaration and in accordance with the Medical Research Involving Human Subjects Act (WMO). All patients provided verbal and written informed consent.
Data Availability
The used intervention study data are unsuitable for public deposition due to ethical restrictions and privacy of participant data. Data are available from these studies for any interested researcher who meets the criteria for access to confidential data. Prof. Ellen Blaak (e.blaak@ maastrichtuniversity.nl) may be contacted to request study data.
References
Macfarlane, G. T. & Macfarlane, S. Bacteria, Colonic Fermentation, and Gastrointestinal Health. Journal of AOAC International 95, 50–60, https://doi.org/10.5740/jaoacint.SGE_Macfarlane (2012).
Schwiertz, A. et al. Microbiota and SCFA in lean and overweight healthy subjects. Obesity (Silver Spring, Md.) 18, 190–195, https://doi.org/10.1038/oby.2009.167 (2010).
Fernandes, J., Su, W., Rahat-Rozenbloom, S., Wolever, T. M. S. & Comelli, E. M. Adiposity, gut microbiota and faecal short chain fatty acids are linked in adult humans. Nutrition & Diabetes 4, e121, https://doi.org/10.1038/nutd.2014.23 (2014).
Roediger, W. E. Role of anaerobic bacteria in the metabolic welfare of the colonic mucosa in man. Gut 21, 793–798 (1980).
Boets, E. et al. Systemic availability and metabolism of colonic‐derived short‐chain fatty acids in healthy subjects: a stable isotope study. The Journal of Physiology 595, 541–555, https://doi.org/10.1113/JP272613 (2017).
Kroger, J. et al. Erythrocyte membrane phospholipid fatty acids, desaturase activity, and dietary fatty acids in relation to risk of type 2 diabetes in the European Prospective Investigation into Cancer and Nutrition (EPIC)-Potsdam Study. The American journal of clinical nutrition 93, 127–142, https://doi.org/10.3945/ajcn.110.005447 (2011).
Bloemen, J. G. et al. Short chain fatty acids exchange across the gut and liver in humans measured at surgery. Clinical Nutrition 28, 657–661, https://doi.org/10.1016/j.clnu.2009.05.011 (2009).
Tang, C. et al. Loss of FFA2 and FFA3 increases insulin secretion and improves glucose tolerance in type 2 diabetes. Nat Med 21, 173–177, https://doi.org/10.1038/nm.3779, http://www.nature.com/nm/journal/v21/n2/abs/nm.3779.html#supplementary-information (2015).
Koh, A., De Vadder, F., Kovatcheva-Datchary, P. & Bäckhed, F. From Dietary Fiber to Host Physiology: Short-Chain Fatty Acids as Key Bacterial Metabolites. Cell 165, 1332–1345, https://doi.org/10.1016/j.cell.2016.05.041 (2016).
Priyadarshini, M. et al. An Acetate-Specific GPCR, FFAR2, Regulates Insulin Secretion. Molecular Endocrinology 29, 1055–1066, https://doi.org/10.1210/me.2015-1007 (2015).
Canfora, E. E., Jocken, J. W. & Blaak, E. E. Short-chain fatty acids in control of body weight and insulin sensitivity. Nat Rev Endocrinol 11, 577–591, https://doi.org/10.1038/nrendo.2015.128 (2015).
van der Beek, C. M. et al. Distal, not proximal, colonic acetate infusions promote fat oxidation and improve metabolic markers in overweight/obese men. Clinical science (London, England: 1979) 130, 2073–2082, https://doi.org/10.1042/cs20160263 (2016).
Canfora, E. E. et al. Colonic infusions of short-chain fatty acid mixtures promote energy metabolism in overweight/obese men: a randomized crossover trial. Scientific Reports 7, 2360, https://doi.org/10.1038/s41598-017-02546-x (2017).
Wolever, T. M., Spadafora, P. & Eshuis, H. Interaction between colonic acetate and propionate in humans. The American journal of clinical nutrition 53, 681–687, https://doi.org/10.1093/ajcn/53.3.681 (1991).
Wolever, T. M., Brighenti, F., Royall, D., Jenkins, A. L. & Jenkins, D. J. Effect of rectal infusion of short chain fatty acids in human subjects. The American journal of gastroenterology 84, 1027–1033 (1989).
Chambers, E. S. et al. Effects of targeted delivery of propionate to the human colon on appetite regulation, body weight maintenance and adiposity in overweight adults. Gut 64, 1744–1754, https://doi.org/10.1136/gutjnl-2014-307913 (2015).
Perry, R. J. et al. Acetate mediates a microbiome-brain-β-cell axis to promote metabolic syndrome. Nature 534, 213–217, https://doi.org/10.1038/nature18309 (2016).
Rahat-Rozenbloom, S., Fernandes, J., Gloor, G. B. & Wolever, T. M. Evidence for greater production of colonic short-chain fatty acids in overweight than lean humans. International journal of obesity (2005) 38, 1525–1531, https://doi.org/10.1038/ijo.2014.46 (2014).
Teixeira, T. F. et al. Higher level of faecal SCFA in women correlates with metabolic syndrome risk factors. The British journal of nutrition 109, 914–919, https://doi.org/10.1017/s0007114512002723 (2013).
Turnbaugh, P. J. et al. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature 444, 1027–1031, https://doi.org/10.1038/nature05414 (2006).
Murphy, E. F. et al. Composition and energy harvesting capacity of the gut microbiota: relationship to diet, obesity and time in mouse models. Gut 59, 1635–1642, https://doi.org/10.1136/gut.2010.215665 (2010).
McNeil, N. I., Cummings, J. H. & James, W. P. Short chain fatty acid absorption by the human large intestine. Gut 19, 819–822 (1978).
Topping, D. L. & Clifton, P. M. Short-chain fatty acids and human colonic function: roles of resistant starch and nonstarch polysaccharides. Physiological reviews 81, 1031–1064, https://doi.org/10.1152/physrev.2001.81.3.1031 (2001).
Ruppin, H., Bar-Meir, S., Soergel, K. H., Wood, C. M. & Schmitt, M. G. Jr. Absorption of short-chain fatty acids by the colon. Gastroenterology 78, 1500–1507 (1980).
Rechkemmer, G., Rönnau, K. & Engelhardt, W. V. Fermentation of polysaccharides and absorption of short chain fatty acids in the mammalian hindgut. Comparative Biochemistry and Physiology Part A: Physiology 90, 563–568, https://doi.org/10.1016/0300-9629(88)90668-8 (1988).
de la Cuesta-Zuluaga, J. et al. Higher Fecal Short-Chain Fatty Acid Levels Are Associated with Gut Microbiome Dysbiosis, Obesity, Hypertension and Cardiometabolic Disease Risk Factors. Nutrients 11, https://doi.org/10.3390/nu11010051 (2018).
Vogt, J. A. & Wolever, T. M. Fecal acetate is inversely related to acetate absorption from the human rectum and distal colon. The Journal of nutrition 133, 3145–3148, https://doi.org/10.1093/jn/133.10.3145 (2003).
den Besten, G. et al. The short-chain fatty acid uptake fluxes by mice on a guar gum supplemented diet associate with amelioration of major biomarkers of the metabolic syndrome. PloS one 9, e107392–e107392, https://doi.org/10.1371/journal.pone.0107392 (2014).
Kaji, I., Karaki, S. & Kuwahara, A. Short-chain fatty acid receptor and its contribution to glucagon-like peptide-1 release. Digestion 89, 31–36, https://doi.org/10.1159/000356211 (2014).
Freeland, K. R., Wilson, C. & Wolever, T. M. Adaptation of colonic fermentation and glucagon-like peptide-1 secretion with increased wheat fibre intake for 1 year in hyperinsulinaemic human subjects. The British journal of nutrition 103, 82–90, https://doi.org/10.1017/s0007114509991462 (2010).
Christiansen, C. B. et al. The impact of short-chain fatty acids on GLP-1 and PYY secretion from the isolated perfused rat colon. American Journal of Physiology-Gastrointestinal and Liver Physiology 315, G53–G65, https://doi.org/10.1152/ajpgi.00346.2017 (2018).
Chambers, A. P. et al. The Role of Pancreatic Preproglucagon in Glucose Homeostasis in Mice. Cell Metabolism 25, 927–934.e923, https://doi.org/10.1016/j.cmet.2017.02.008 (2017).
Gromada, J., Chabosseau, P. & Rutter, G. A. The α-cell in diabetes mellitus. Nature Reviews. Endocrinology 14, 694–704, https://doi.org/10.1038/s41574-018-0097-y (2018).
Canfora, E. E. & Blaak, E. E. Acetate: a diet-derived key metabolite in energy metabolism: good or bad in context of obesity and glucose homeostasis? Current opinion in clinical nutrition and metabolic care 20, 477–483, https://doi.org/10.1097/mco.0000000000000408 (2017).
Larraufie, P. et al. SCFAs strongly stimulate PYY production in human enteroendocrine cells. Scientific Reports 8, 74, https://doi.org/10.1038/s41598-017-18259-0 (2018).
Ge, H. et al. Activation of G Protein-Coupled Receptor 43 in Adipocytes Leads to Inhibition of Lipolysis and Suppression of Plasma Free Fatty Acids. Endocrinology 149, 4519–4526, https://doi.org/10.1210/en.2008-0059 (2008).
Fernandes, J., Vogt, J. & Wolever, T. M. Intravenous acetate elicits a greater free fatty acid rebound in normal than hyperinsulinaemic humans. Eur J Clin Nutr 66, 1029–1034, https://doi.org/10.1038/ejcn.2012.98 (2012).
Jocken, J. W. E. et al. Short-Chain Fatty Acids Differentially Affect Intracellular Lipolysis in a Human White Adipocyte Model. Frontiers in Endocrinology 8, https://doi.org/10.3389/fendo.2017.00372 (2018).
Girousse, A. et al. Partial inhibition of adipose tissue lipolysis improves glucose metabolism and insulin sensitivity without alteration of fat mass. PLoS biology 11, e1001485, https://doi.org/10.1371/journal.pbio.1001485 (2013).
Al-Lahham, S. et al. Propionic acid affects immune status and metabolism in adipose tissue from overweight subjects. European journal of clinical investigation 42, 357–364, https://doi.org/10.1111/j.1365-2362.2011.02590.x (2012).
Rumberger, J. M., Arch, J. R. S. & Green, A. Butyrate and other short-chain fatty acids increase the rate of lipolysis in 3T3-L1 adipocytes. PeerJ 2, e611–e611, https://doi.org/10.7717/peerj.611 (2014).
Khan, S. & Jena, G. Sodium butyrate reduces insulin-resistance, fat accumulation and dyslipidemia in type-2 diabetic rat: A comparative study with metformin. Chemico-biological interactions 254, 124–134, https://doi.org/10.1016/j.cbi.2016.06.007 (2016).
Khan, S. & Jena, G. B. Protective role of sodium butyrate, a HDAC inhibitor on beta-cell proliferation, function and glucose homeostasis through modulation of p38/ERK MAPK and apoptotic pathways: study in juvenile diabetic rat. Chemico-biological interactions 213, 1–12, https://doi.org/10.1016/j.cbi.2014.02.001 (2014).
Qin, J. et al. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature 490, 55, https://doi.org/10.1038/nature11450 (2012).
Karlsson, F. H. et al. Gut metagenome in European women with normal, impaired and diabetic glucose control. Nature 498, 99, https://doi.org/10.1038/nature12198 (2013).
Brahe, L. K., Astrup, A. & Larsen, L. H. Is butyrate the link between diet, intestinal microbiota and obesity-related metabolic diseases? Obesity Reviews 14, 950–959, https://doi.org/10.1111/obr.12068 (2013).
Layden, B. T., Yalamanchi, S. K., Wolever, T. M., Dunaif, A. & Lowe, W. L. Jr. Negative association of acetate with visceral adipose tissue and insulin levels. Diabetes, metabolic syndrome and obesity: targets and therapy 5, 49–55, https://doi.org/10.2147/dmso.S29244 (2012).
Moreno-Navarrete, J. M. et al. Gut Microbiota Interacts with Markers of Adipose Tissue Browning, Insulin Action and Plasma Acetate in Morbid Obesity. Molecular nutrition & food research 62, https://doi.org/10.1002/mnfr.201700721 (2018).
Fernandes, J., Vogt, J. & Wolever, T. M. S. Inulin increases short-term markers for colonic fermentation similarly in healthy and hyperinsulinaemic humans. European journal of clinical nutrition 65, 1279, https://doi.org/10.1038/ejcn.2011.116 (2011).
Fernandes, J., Vogt, J. & Wolever, T. M. S. Kinetic model of acetate metabolism in healthy and hyperinsulinaemic humans. European journal of clinical nutrition 68, 1067–1071, https://doi.org/10.1038/ejcn.2014.136 (2014).
Han, J.-H. et al. The effects of propionate and valerate on insulin responsiveness for glucose uptake in 3T3-L1 adipocytes and C2C12 myotubes via G protein-coupled receptor 41. PloS one 9, e95268–e95268, https://doi.org/10.1371/journal.pone.0095268 (2014).
Weitkunat, K. et al. Importance of propionate for the repression of hepatic lipogenesis and improvement of insulin sensitivity in high-fat diet-induced obesity. Mol Nutr Food Res 60, 2611–2621, https://doi.org/10.1002/mnfr.201600305 (2016).
Weitkunat, K. et al. Odd-chain fatty acids as a biomarker for dietary fiber intake: a novel pathway for endogenous production from propionate. The American journal of clinical nutrition 105, 1544–1551, https://doi.org/10.3945/ajcn.117.152702 (2017).
Knowles, S. E., Jarrett, I. G., Filsell, O. H. & Ballard, F. J. Production and utilization of acetate in mammals. Biochem J 142, 401–411 (1974).
Sun, E. W. et al. Mechanisms Controlling Glucose-Induced GLP-1 Secretion in Human Small Intestine. Diabetes 66, 2144–2149, https://doi.org/10.2337/db17-0058 (2017).
American Diabetes, A. Diagnosis and classification of diabetes mellitus. Diabetes care 33(Suppl 1), S62–S69, https://doi.org/10.2337/dc10-S062 (2010).
Canfora, E. E. et al. Supplementation of Diet With Galacto-oligosaccharides Increases Bifidobacteria, but Not Insulin Sensitivity, in Obese Prediabetic Individuals. Gastroenterology 153, 87–97.e83, https://doi.org/10.1053/j.gastro.2017.03.051 (2017).
Reijnders, D. et al. Effects of Gut Microbiota Manipulation by Antibiotics on Host Metabolism in Obese Humans: A Randomized Double-Blind Placebo-Controlled Trial. Cell Metab 24, 63–74, https://doi.org/10.1016/j.cmet.2016.06.016 (2016).
Müller, M. et al. In European Congress on Obesity Vol. 11 (Obesity Facts, Vienna, 2018).
Frayn, K. N. Calculation of substrate oxidation rates in vivo from gaseous exchange. J Appl Physiol Respir Environ Exerc Physiol 55, 628–634, https://doi.org/10.1152/jappl.1983.55.2.628 (1983).
Weir, J. B. D. V. New methods for calculating metabolic rate with special reference to protein metabolism. The Journal of Physiology 109, 1–9 (1949).
DeFronzo, R. A., Tobin, J. D. & Andres, R. Glucose clamp technique: a method for quantifying insulin secretion and resistance. The American journal of physiology 237, E214–223, https://doi.org/10.1152/ajpendo.1979.237.3.E214 (1979).
Garcia-Villalba, R. et al. Alternative method for gas chromatography-mass spectrometry analysis of short-chain fatty acids in faecal samples. Journal of separation science 35, 1906–1913, https://doi.org/10.1002/jssc.201101121 (2012).
van Eijk, H. M., Bloemen, J. G. & Dejong, C. H. Application of liquid chromatography-mass spectrometry to measure short chain fatty acids in blood. Journal of chromatography. B, Analytical technologies in the biomedical and life sciences 877, 719–724, https://doi.org/10.1016/j.jchromb.2009.01.039 (2009).
Orskov, C., Rabenhoj, L., Wettergren, A., Kofod, H. & Holst, J. J. Tissue and plasma concentrations of amidated and glycine-extended glucagon-like peptide I in humans. Diabetes 43, 535–539, https://doi.org/10.2337/diab.43.4.535 (1994).
Schols, A. M., Buurman, W. A., Staal van den Brekel, A. J., Dentener, M. A. & Wouters, E. F. Evidence for a relation between metabolic derangements and increased levels of inflammatory mediators in a subgroup of patients with chronic obstructive pulmonary disease. Thorax 51, 819–824, https://doi.org/10.1136/thx.51.8.819 (1996).
Matthews, D. R. et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28, 412–419 (1985).
Acknowledgements
We would kindly like to thank all study participants, Wendy Sluijsman, Yvonne Essers, Nicole Hoebers, Hasibe Aydeniz and Jos Stegen for their excellent technical support. The studies summarized in this manuscript were fundend by TI Food and Nutrition, a public–private partnership on precompetitive research in food and nutrition research.
Author information
Authors and Affiliations
Contributions
M.M. and M.H.G. perfomed statistical analysis and wrote the paper. M.M., E.E.C. and D.R. performed clinical research. H.E. performed analyticial measurments, E.E.B. and E.E.C. edited the paper, E.E.B., E.E.C., D.R., G.H.G., J.J.H. and J.W.E.J. read commented and E.E.B. and E.E.C. approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Müller, M., Hernández, M.A.G., Goossens, G.H. et al. Circulating but not faecal short-chain fatty acids are related to insulin sensitivity, lipolysis and GLP-1 concentrations in humans. Sci Rep 9, 12515 (2019). https://doi.org/10.1038/s41598-019-48775-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-48775-0
This article is cited by
-
Targeted metabolomics reveals plasma short-chain fatty acids are associated with metabolic dysfunction-associated steatotic liver disease
BMC Gastroenterology (2024)
-
Effects of dietary fibre on metabolic health and obesity
Nature Reviews Gastroenterology & Hepatology (2024)
-
Sodium butyrate ameliorates diabetic retinopathy in mice via the regulation of gut microbiota and related short-chain fatty acids
Journal of Translational Medicine (2023)
-
Short-chain fatty acids in diseases
Cell Communication and Signaling (2023)
-
Comparison of fecal and blood metabolome reveals inconsistent associations of the gut microbiota with cardiometabolic diseases
Nature Communications (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.