Abstract
As cardiac involvement is the most important prognostic marker in light-chain amyloidosis (AL), revised Mayo staging for AL incorporated N-terminal pro-brain natriuretic peptide (NTproBNP) and troponin T (TnT). However, prognostic value of novel biomarkers, such as soluble suppression of tumorigenicity 2 (sST2), growth differentiation factor 15 (GDF15), or osteopontin (OPN) is unknown in AL amyloidosis. We aimed to investigate additive predictive effects of novel biomarkers for overall mortality rates of AL amyloidosis patients. Levels of sST2, GDF15, and OPN were quantified at diagnosis in a total of 73 AL amyloidosis patients at Samsung Medical Center from 2010 to 2016. The median follow-up duration of the censored cases was 18.0 (12.4–28.1) months. A total of 25 deaths occurred during the follow-up period. Two novel biomarkers, sST2 and GDF-15 showed satisfactory predictive performances for both one-year and overall survival from ROC analysis. Best cut-off values for predicting one-year mortality were selected. Elevated sST2 and GDF-15 levels showed significant incremental prognostic values in addition to NT-ProBNP and TnT for overall mortality. Patients were assigned 1 point for elevated sST2 or GDF-15. The mean values of NT-proBNP, TnT, mean LV wall thickness, and septal e′ velocity differed significantly according to the scores. Patients with higher scores showed significantly worse prognosis even in patients with advanced revised Mayo staging. Two novel biomarkers, sST2 and GDF-15, showed satisfactory prognostic value for overall survival of AL amyloidosis patients. Furthermore, sST2 and GDF-15 showed additive incremental values over conventional biomarkers and further discriminated prognosis of patients in advanced stages.
Similar content being viewed by others
Introduction
Cardiac involvement is the most important prognostic marker in light-chain amyloidosis (AL). Revised Mayo staging is the most widely used, well-validated prognostic system in AL amyloidosis, incorporating the cardiac biomarkers troponin T (TnT) and N-terminal pro-brain natriuretic peptide (NT-proBNP)1. According to the current staging, patients with cardiac involvement are most likely classified as advanced stage. However, recent advances in chemotherapy regimens for AL amyloidosis have improved overall survival, even in patients with cardiac involvement2,3. Furthermore, previous studies have showed that cardiac amyloid load is significantly associated with prognosis of AL amyloid patients, suggesting different prognosis according to degree of cardiac involvement4. Therefore, more detailed risk stratification of AL amyloidosis patients with cardiac involvement is needed.
Although NT-proBNP is a very sensitive marker for assessment of cardiac involvement in AL amyloidosis5, previous studies have failed to show a correlation between cardiac amyloid load and NT-proBNP in AL amyloidosis4. Considering the complex pathophysiology of cardiac involvement in AL amyloidosis, a simple combination of NT-proBNP and TnT may not provide sufficient prognostic information. Novel biomarkers with different pathophysiological targets would contribute to detailed risk stratification, which could facilitate development of risk-adapted therapies in AL amyloidosis patients, especially those with cardiac involvement.
Recently, novel biomarkers have been introduced and their prognostic values have been studied in heart failure patients. The prognostic performance of soluble suppression of tumorigenicity 2 (sST2), growth differentiation factor 15 (GDF-15), and osteopontin (OPN) has been studied in various populations with heart failure6,7,8. In this study, we sought to determine prognostic value of these three novel biomarkers in AL amyloidosis. We also investigated if prognostic values of these biomarkers had additive incremental value over the currently used biomarkers NT-proBNP and TnT.
Results
Patient characteristics
Table 1 describes the main characteristics of patients. Forty-four patients (60%) were men and mean age at baseline was 60 years. Kidney involvement was present in 41 (56%) of patients and cardiac involvement was detected in 50 (69%) patients. Thirty-four (47%) patients were classified as Revised Mayo stage IV. A total of 63 (86%) underwent chemotherapy and 10 patients did not receive chemotherapy. A total of 20 (27%) patients underwent autologous stem cell transplantation. Median follow up was 14.2 months (range 0.4–65 months). A total of 25 patients died during follow-up.
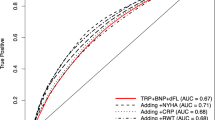
Novel biomarkers and overall survival
Median values of sST2, GDF-15, and OPN were as follows: 39.8 ng/mL (IQR 25.5, 70.8), 1.89 ng/mL (IQR 1.04, 3.79), and 107.2 ng/mL (IQR 64.0, 170.0), respectively. There were no age- or sex-related relationships among biomarkers. Receiver operating characteristic (ROC) curves were used to derive cut-off values of novel biomarkers for predicting one-year and overall mortality (Fig. 1). The best cut-off values for sST2 to predict one-year and overall mortality were 32.6 ng/mL (AUC 0.72, sensitivity 91%, specificity 52%, p = 0.003 for one-year survival; AUC 0.72, sensitivity 88%, specificity 54%, p = 0.005 for overall survival). The respective cut-off values for GDF-15 were 2.30 ng/mL (AUC 0.72, sensitivity 71%, specificity 44%, p = 0.004 for one-year mortality) and 1.71 ng/mL (AUC 0.69, sensitivity 80%, specificity 58%, p = 0.009 for overall mortality). OPN did not show significant predictive values for predicting one-year or overall mortality.
Elevated levels of sST2, GDF-15, and OPN were defined by cut-off values from previous ROC curves for predicting one-year mortality (sST2 ≥ 32.6 ng/mL, GDF-15 ≥ 2.3 ng/mL, OPN ≥ 154.7 ng/mL). Patients with elevated levels of sST2 and GDF-15 at baseline showed significantly poor overall survival compared to those with lower levels (Fig. 2). Elevated sST2 and elevated GDF-15 showed significant incremental predictive values for overall mortality over elevated traditional biomarkers (NT-proBNP ≥ 1,800 pg/mL and/or TnT ≥ 0.025 ng/mL) in a step-wise manner (Supplemental Fig. 1). From multivariate analysis, elevated sST2 and GDF-15 were independently associated with overall mortality (Table 2).
Elevated sST2 and GDF-15 in association with conventional biomarkers, LV functions, and prognosis
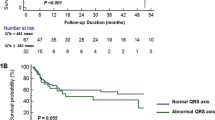
Patients were scored by assigning 1 point for each of elevated sST2 (sST2 ≥ 32.6 ng/mL) and GDF-15 (GDF-15 ≥ 2.3 ng/mL) [Score 0 (neither elevated sST2 nor GDF-15), Score 1 (elevated sST2 or GDF-15), Score 2 (both elevated sST2 and GDF-15)]. Patients were classified into 3 groups according to these scores. Mean values of NT-proBNP and TnT differed significantly among three groups (Fig. 3A,B) and they showed increasing trends with higher scores. Mean values of septal e′ and mean LV wall thickness also differed significantly among three groups (Supplemental Fig. 2A,B). Patients with higher scores had more reduced longitudinal motion of LV (reflected by septal e′ velocity) and relatively more thickened LV wall.
Patients with higher scores showed significantly worse prognosis (Fig. 4A). This trend remained to be significant in subgroups of patients with advanced revised Mayo staging (stage III and IV) (Fig. 4B) or those with cardiac involvement (Supplemental Fig. 3).
Discussion
In the current analysis, we evaluated prognostic performances of novel biomarkers in patients with AL amyloidosis. The result obtained in this cohort of patients show that (1) the novel biomarkers sST2 and GDF-15 show satisfactory prognostic values for overall survival in patients with AL amyloidosis, (2) sST2 and GDF-15 had incremental prognostic values over the conventional biomarkers NT-proBNP and TnT, and (3) sST2 and GDF-15 further discriminated prognosis of patients at advanced revised Mayo stages.
Recently, new biomarkers have been introduced and validated in heart failure patients to attempt accurate diagnosis and prognostic evaluation. As cardiac involvement is pivotal for prognosis in AL amyloidosis, parameters reflecting cardiac function or pathology are likely to be closely related to prognosis of AL amyloidosis. Almost half of AL amyloidosis patients have cardiac amyloidosis at time of the diagnosis9. As survival of AL amyloidosis patients has increased due to the introduction of novel agents and stem cell transplantation, more detailed risk stratification is needed in patients with cardiac amyloidosis, whom are often classified as advanced stages according to revised Mayo staging system. Novel biomarkers also may complement limitations of traditional biomarkers. For example, although prognostic value of NT-proBNP in AL amyloidosis has been recapitulated in previous studies, the value of NT-proBNP is greatly affected by volume status or renal function of patients5,10.
sST2 is in the IL-1 receptor family and plays an important role through IL-33 signaling11. sST2 is elevated in heart failure patients and acts as decoy receptor of IL-33 to alleviate cardio-protective effects of IL-3312,13. Many studies have reported a significant association between sST2 and outcome in chronic and acute heart failure patients14,15,16. GDF-15 is a member of the transforming growth factor-β superfamily and is highly expressed in cardiac myocytes, especially during tissue injury and inflammatory status17,18. Prognostic utility of GDF-15, as a biomarker of inflammatory stress, has been well-demonstrated in HF patients with both reduced and preserved ejection fraction19,20. OPN is a secreted phosphor-glycoprotein expressed in many cell types including cardiomyocytes21. Results from previous studies suggest that OPN is upregulated in animal models of heart failure in response to biomechanical stress. Expression of OPN is elevated and correlated with left ventricular function and diameter in patients with myocardial infarction and dilated cardiomyopathy22,23.
From our results, sST2 and GDF-15 showed satisfactory discriminative values for overall survival in AL amyloidosis patients, while OPN did not. A combination of sST2 and GDF-15 showed significant incremental prognostic values over the traditional biomarkers TnT and NT-proBNP. Also, classifications according to levels of sST2 and GDF-15 showed good correlations with structure (mean wall thickness) and longitudinal function (septal e′ velocity) of left ventricle. Our results suggest possible utilization of sST2 and GDF-15 for further discrimination of prognosis of AL amyloid patients who were previously classified as advanced stages. Risk stratification with multi-biomarkers would facilitate selection of patients for new treatment strategies or novel agents.
There are some limitations to our study. The number of patients is relatively small from a statistical standpoint and suggested cut-off values need to be validated in further studies. We acknowledge that this was single-center cohort study and that the prognosis and baseline characteristics of our patients may not reflect the worldwide AL patient population. However, our center is one of largest referral centers for AL amyloidosis in our country. Further, because all studies were carried out in a single center, there was great consistency in blood sampling and measurement of novel biomarkers and all markers were available in all patients. Further study in a larger independent AL amyloidosis population is needed to fully validate and confirm our findings indicating that measurement of sST2 and GDF-15 provides additional prognostic value in AL patients with cardiac involvement.
In conclusion, the novel biomarkers sST 2 and GDF-15 showed satisfactory prognostic values for overall survival in patients with AL amyloidosis. Furthermore, sST2 and GDF-15 showed additive incremental values over conventional biomarkers and further discriminated prognosis of patients in advanced revised Mayo stages (stage III and IV). These new biomarkers may contribute to further detailed risk stratifications in AL amyloidosis, especially with cardiac involvement. Further studies are needed for validation of suggested cut-off values and investigation of the potential use for monitoring treatment effects.
Materials and Methods
Patient population
Levels of sST2, GDF-15, and OPN were assessed at time of diagnosis in 73 AL amyloidosis patients at Samsung Medical Center from 2010 to 2015. All patients were biopsy-proven amyloidosis confirmed by Congo red staining and immunohistochemistry of any tissue specimen using commercially available monoclonal antibodies as in previous studies4. The diagnosis of AL amyloidosis required tissue confirmation of amyloid deposits or fibrils by apple-green birefringence with Congo red staining, kappa or lamda restriction by immunohistochemistry in at least one involved organ, and evidence of monoclonal gammopathy. Cardiac involvement was defined by the presence of amyloid deposits on endomyocardial biopsy (n = 50, 69%). Patients with dialysis were excluded due to altered metabolism of biomarkers. Plasma cell dyscrasia was documented by serum/urine immunofixation electrophoresis and serum free light-chain test. All patients agreed to the use of blood samples for experimental purposes, in accordance with institutional review board guidelines.
The mortality endpoint was defined as time to death from baseline for all deceased patients or time to censor date, February 28, 2015. Date of baseline was within 1 month of diagnosis. Occurrence and date of death and ongoing survival status were regularly monitored by visits or telephone calls at Samsung Medical Center. The median follow-up duration of the censored cases was 18.0 (12.4–28.1) months.
Study procedure
Baseline assessment included standardized physical examination, history taking, 12-lead electrocardiogram, transthoracic echocardiography, and blood sampling. Modification of Diet in Renal Disease (MDRD) equation was used to calculate estimated glomerular filtration rate (eGFR).
Echocardiography
All patients underwent conventional transthoracic echocardiography at the time of diagnosis. Cardiac chamber sizes were quantified according to previous recommendations from current guidelines24. Mean left ventricular (LV) wall thickness was derived from the average of posterior left ventricular (LV) wall and interventricular wall thickness at end-diastole. The ratio of early transmitral flow to early septal mitral annular diastolic velocity (E/e′) was measured as an index of LV filling pressure25.
Biomarkers
NT-proBNP was measured with an electrochemiluminescence sandwich immunoassay (Elecsys system 2010®, Roche Diagnostics, Mannheim, Germany). TnT assay was performed with a fourth generation assay (Elecsys 2010®, Roche Diagnostics, Mannheim, Germany).
Blood samples were frozen immediately and stored at −70 °C before measurement of sST2, GDF-15, and OPN. Plasma OPN levels were measured with a sandwich immunoassay by use of a commercially available kit (Quantikine®; R&D Systems, Inc., Minneapolis, MN, USA). Plasma levels of soluble suppression of tumorigenicity 2 (sST2) were determined using a novel high-sensitivity sandwich immunoassay (Presage ST2®; Critical Diagnostics, San Diego, CA, USA). Plasma levels of growth differentiation factor 15 (GDF15) were determined by a sandwich enzyme immunoassay technique (Quantikine®; R&D Systems, Inc., Minneapolis, MN, USA).
Statistical analysis
Continuous data were expressed as mean ± standard deviation and categorical variables were expressed as absolute number (percent). Receiver operating characteristics (ROC) curves were used to assess the predictive accuracy of biomarkers on 1-year all-cause mortality. The incremental prognostic utility of sST2 and GDF-15 was assessed by comparing the global chi square values. For comparison among three groups, which were classified according to sST2 and GDF-15 levels, one way ANOVA (parametric) and Kruskal-Wallis test (non-parametric) were used. Difference in overall survival was assessed using log-rank analysis with right censoring and displayed by Kaplan-Meier survival curve. Cox regression analysis was performed to investigate independent parameters to predict overall survival rates. All analyses were performed using IBM SPSS Statistics version 24 (SPSS Inc., Chicago, IL, USA).
Statement
Informed consent was obtained from all subjects, and all methods were carried out in accordance with the relevant guidelines and regulations according to the principles expressed in the Declaration of Helsinki. All study protocols were approved by Institutional Review Board at Samsung Medical Center.
Disclosures
This research was supported by a grant (code: 2016E6300502) from the Research of Korea Centers for Disease Control and Prevention
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Kumar, S. et al. Revised prognostic staging system for light chain amyloidosis incorporating cardiac biomarkers and serum free light chain measurements. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 30, 989–995, https://doi.org/10.1200/JCO.2011.38.5724 (2012).
Gatt, M. E. & Palladini, G. Light chain amyloidosis 2012: a new era. British journal of haematology 160, 582–598, https://doi.org/10.1111/bjh.12191 (2013).
Skinner, M. et al. High-dose melphalan and autologous stem-cell transplantation in patients with AL amyloidosis: an 8-year study. Annals of internal medicine 140, 85–93 (2004).
Kristen, A. V. et al. Cardiac Amyloid Load: A Prognostic and Predictive Biomarker in Patients With Light-Chain Amyloidosis. Journal of the American College of Cardiology 68, 13–24, https://doi.org/10.1016/j.jacc.2016.04.035 (2016).
Palladini, G. et al. Serum N-terminal pro-brain natriuretic peptide is a sensitive marker of myocardial dysfunction in AL amyloidosis. Circulation 107, 2440–2445, https://doi.org/10.1161/01.CIR.0000068314.02595.B2 (2003).
Lassus, J. et al. Incremental value of biomarkers to clinical variables for mortality prediction in acutely decompensated heart failure: the Multinational Observational Cohort on Acute Heart Failure (MOCA) study. International journal of cardiology 168, 2186–2194, https://doi.org/10.1016/j.ijcard.2013.01.228 (2013).
Cotter, G. et al. Growth differentiation factor 15 (GDF-15) in patients admitted for acute heart failure: results from the RELAX-AHF study. European journal of heart failure 17, 1133–1143, https://doi.org/10.1002/ejhf.331 (2015).
Rosenberg, M. et al. Osteopontin, a new prognostic biomarker in patients with chronic heart failure. Circulation. Heart failure 1, 43–49, https://doi.org/10.1161/CIRCHEARTFAILURE.107.746172 (2008).
Sidiqi, M. H. et al. Stem Cell Transplantation for Light Chain Amyloidosis: Decreased Early Mortality Over Time. Journal of clinical oncology: official journal of the American Society of Clinical Oncology, JCO2017769554, https://doi.org/10.1200/JCO.2017.76.9554 (2018).
Dispenzieri, A. et al. Serum cardiac troponins and N-terminal pro-brain natriuretic peptide: a staging system for primary systemic amyloidosis. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 22, 3751–3757, https://doi.org/10.1200/JCO.2004.03.029 (2004).
Seki, K. et al. Interleukin-33 prevents apoptosis and improves survival after experimental myocardial infarction through ST2 signaling. Circulation. Heart failure 2, 684–691, https://doi.org/10.1161/CIRCHEARTFAILURE.109.873240 (2009).
Weinberg, E. O. et al. Expression and regulation of ST2, an interleukin-1 receptor family member, in cardiomyocytes and myocardial infarction. Circulation 106, 2961–2966 (2002).
Sanada, S. et al. IL-33 and ST2 comprise a critical biomechanically induced and cardioprotective signaling system. The Journal of clinical investigation 117, 1538–1549, https://doi.org/10.1172/JCI30634 (2007).
Januzzi, J. L. Jr. et al. Measurement of the interleukin family member ST2 in patients with acute dyspnea: results from the PRIDE (Pro-Brain Natriuretic Peptide Investigation of Dyspnea in the Emergency Department) study. Journal of the American College of Cardiology 50, 607–613, https://doi.org/10.1016/j.jacc.2007.05.014 (2007).
Broch, K. et al. Soluble ST2 is associated with adverse outcome in patients with heart failure of ischaemic aetiology. European journal of heart failure 14, 268–277, https://doi.org/10.1093/eurjhf/hfs006 (2012).
Gruson, D., Lepoutre, T., Ahn, S. A. & Rousseau, M. F. Increased soluble ST2 is a stronger predictor of long-term cardiovascular death than natriuretic peptides in heart failure patients with reduced ejection fraction. International journal of cardiology 172, E250–E252, https://doi.org/10.1016/j.ijcard.2013.12.101 (2014).
Xu, J. et al. GDF15/MIC-1 functions as a protective and antihypertrophic factor released from the myocardium in association with SMAD protein activation. Circ Res 98, 342–350, https://doi.org/10.1161/01.Res.0000202804.84885.D0 (2006).
Kempf, T. et al. The transforming growth factor-beta superfamily member growth-differentiation factor-15 protects the heart from ischemia/reperfusion injury. Circ Res 98, 351–360, https://doi.org/10.1161/01.Res.0000202805.73038.48 (2006).
Stahrenberg, R. et al. The novel biomarker growth differentiation factor 15 in heart failure with normal ejection fraction. European journal of heart failure 12, 1309–1316, https://doi.org/10.1093/eurjhf/hfq151 (2010).
Santhanakrishnan, R. et al. Growth differentiation factor 15, ST2, high-sensitivity troponin T, and N-terminal pro brain natriuretic peptide in heart failure with preserved vs. reduced ejection fraction. European journal of heart failure 14, 1338–1347, https://doi.org/10.1093/eurjhf/hfs130 (2012).
Denhardt, D. T. & Guo, X. Osteopontin: a protein with diverse functions. FASEB journal: official publication of the Federation of American Societies for Experimental Biology 7, 1475–1482 (1993).
Stawowy, P. et al. Increased myocardial expression of osteopontin in patients with advanced heart failure. European journal of heart failure 4, 139–146 (2002).
Satoh, M. et al. Myocardial osteopontin expression is associated with collagen fibrillogenesis in human dilated cardiomyopathy. Eur Heart J 26, 755–755 (2005).
Lang, R. M. et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. European heart journal cardiovascular Imaging 16, 233–270, https://doi.org/10.1093/ehjci/jev014 (2015).
Yu, C. M., Sanderson, J. E., Marwick, T. H. & Oh, J. K. Tissue Doppler imaging a new prognosticator for cardiovascular diseases. Journal of the American College of Cardiology 49, 1903–1914, https://doi.org/10.1016/j.jacc.2007.01.078 (2007).
Author information
Authors and Affiliations
Contributions
D.K., G.Y.L. and E.S.J. designed the study. J.C., K.K. and S.J.K. participated in data collection. E.S.J. and D.K. participated in data analysis and interpretation. D.K. participated in the writing of the paper. E.S.J. critically revised the article for important intellectual content.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, D., Lee, G.Y., Choi, JO. et al. Prognostic values of novel biomarkers in patients with AL amyloidosis. Sci Rep 9, 12200 (2019). https://doi.org/10.1038/s41598-019-48513-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-48513-6
This article is cited by
-
An observational, non-interventional study for the follow-up of patients with amyloidosis who received miridesap followed by dezamizumab in a phase 1 study
Orphanet Journal of Rare Diseases (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.