Abstract
Reduced sleep quality is associated with an increased risk of sarcopenia. However, the potential effects of disturbing the regular circadian rhythm, as occurs with shift work, on the risk of sarcopenia have not been established. Data from 9105 workers from the 2008–2011 Korean National Health and Nutrition Examination Survey were analyzed. Sarcopenia, measured by dual-energy X-ray absorptiometry, was defined as one standard deviation below the mean of the appendicular skeletal muscle/body mass index value of a young reference group. Compared to the group that had never experienced shift work, the odds ratio (OR) for sarcopenia with a 95% confidence interval (95% CI) for the shift work group was 1.7 (1.5–1.9); the association remained even after adjusting for confounding variables, including age, sex, total fat mass, insulin resistance profile, smoking, alcohol intake, diet, and physical activity. The results of the subgroup analysis indicated that the highest risk of sarcopenia was among workers engaging in shift work with an irregular schedule (OR 1.8, 95% CI 1.3–2.4). Disruption of circadian rhythm by shift work was associated with increased risk of sarcopenia. Intervention strategies are needed to prevent sarcopenia in shift workers.
Similar content being viewed by others
Introduction
Sarcopenia is defined as the progressive, generalized loss of skeletal muscle mass, strength, and function1,2. Sarcopenia is divided into primary and secondary sarcopenia2. Primary sarcopenia is regarded as a normal part of the aging process with no other cause2, whereas secondary sarcopenia is related to conditions other than aging, such as chronic inflammatory disease2. Although sarcopenia is primarily a disease of the elderly, it is also seen in younger individuals.
Sarcopenia is associated with multiple adverse outcomes, including various diseases such as cardiovascular disease3,4, stroke5, liver disease6,7,8, pulmonary disease9, chronic kidney disease10,11, gastrointestinal disorders12, malignancy13, postoperative morbidity14,15, emotional disorders16, and all-cause mortality17. Therefore, it is essential to determine the prevalence and causes of sarcopenia to improve patients’ outcomes.
There are a number of known causes of sarcopenia, including aging, disuse, malnutrition, and chronic inflammatory diseases, such as osteoporosis. Several recent studies have indicated that decreased sleep quality and long or short sleep duration may also play roles in the development of sarcopenia18,19,20.
However, whether circadian rhythm disturbance is associated with sarcopenia has not been examined, even though maintaining circadian rhythm is known to be important for sleep quality. Here, we examined whether shift work21, which is known to disturb circadian rhythm, was associated with an increased risk of sarcopenia using data from a nationally representative cohort study in Korea: the Korean National Health and Nutrition Examination Survey (KNHANES).
Method
Institutional ethic review board approval of the study design
The institutional review board of Gil Medical Center reviewed the study protocol (IRB approval no: GC IRB 2018705) and approved the research. All research was performed in accordance with national guidelines and regulations. In this study, we used the data from the KNHANES which is a national surveillance system that has been assessing the health and nutritional status of Koreans since 1998, and its data is opened to public. The need for written informed consent was waived by the Ethics Committee.
Study population
The study was based on the 5th Korean National Health and Nutrition Examination Survey (KNHANES) conducted in 2008–2011 by the Korea Centers for Disease Control and Prevention, which aimed to estimate the health status of the Korean population22. All study participants provided informed consent. KNHANES enrolled representative subjects selected by stratified multistage sampling22. The variables in KNAHENS regarding socioeconomic factors, health status, and lifestyle factors including smoking, alcohol ingestion, physical activity, and dietary patterns were collected from self-administered questionnaires22.
Among 37,753 participants, subjects < 19 years old (n = 8835) and those with missing data (n = 541) were excluded from the present study. Therefore, a total study population consisting of 9,105 workers of all types was included in the final analysis.
Definition of sarcopenia
We defined sarcopenia in three different ways in accordance with the consensus report of the Asian Working Group for Sarcopenia, as below1,23: (1) weight-adjusted percentage muscle mass (ASM/weight squared) below the lowest quintile computed for the study population; (2) height-adjusted percentage muscle mass (ASM/height squared) below the lowest quintile computed for the study population; (3) body mass index-adjusted percentage muscle mass (ASM/body mass index) below the lowest quintile computed for the study population in
Body fat (kg) and appendicular skeletal muscle mass (ASM, kg) were measured through dual-energy X-ray absorptiometry (DISCOVERY-W fan-beam densitometer; Hologic, Inc., Bedford, MA)22. Among the total study population, subjects below the median value and subjects above the median value of the total study group were designated as the low and high total body fat mass groups, respectively. In the same manner, the low and high axial skeletal muscle mass groups were defined as subjects below the median and above the median axial skeletal muscle mass, respectively.
Definition of type of work and shift work
Type of work was categorized according to occupation: blue-collar workers (simple labor, agriculture, forestry, and fisheries), white-collar workers (professionals and office workers), and pink-collar workers (service workers)22.
Workers were divided into those who worked only in the daytime (regular daytime workers) and those with other work schedules (alternative shifts).
Other variables
Dietary patterns were assessed via single 24-h recall19,22. Individual energy and nutrient intakes were calculated using the seventh Food Composition Table prepared by the Korean National Rural Resources Development Institute19,22. Trained interviewers instructed respondents to recall and describe all foods and beverages consumed during the previous day19. Values indicating “excessive,” “appropriate,” and “lacking” in terms of nutrient status were those of the Dietary Reference Intakes for Koreans, revised in 2015. Exercise patterns were classified in accordance with exercise type and frequencies per week, such as walking exercise frequency and strength exercise frequency19,22. Smoking status was divided into nonsmoker and current smoker based on the response to the question “Do you currently smoke?19,22.” Alcohol drinking status was assigned based on the response to the question “Did you drink more than one glass of liquor during the last month?22.” Sleep duration (h/d) was self-reported as an answer to the question “How long do you usually sleep at night?”22. Household income was calculated as the sum of the monthly income of all family members and classified into groups including lowest (first quantile), middle-low (second quantile), middle-high (third quantile), and highest (4th quantile)22. Education status was divided into four classes; education for 6 years or less as elementary school; 7–9 years as middle school; 10–12 years as high school; and 13 years or over as college or university. Homeostatic model assessment for insulin resistance (HOMA-IR) was defined as below; HOMA-IR = [Fasting blood insulin (µU/mL) × [Fasting blood glucose (mmol/L)]/22.5.
Statistical analysis
Continuous and categorical variables are expressed as the mean ± standard deviation (SD) and number with percentage (±SE), respectively. General characteristics were presented according to 1) the experience of shift work among the total population, and 2) the presence of sarcopenia among the shift work group. To compare 1) the shift work group vs the non- shift work group, and 2) members of the shift work group with sarcopenia vs members of the shift work group without sarcopenia, t-test and the chi-squared test were used. Odds ratios (ORs) and 95% confidence intervals (CIs) for the associations between shift work experience and sarcopenic status were analyzed using multivariate logistic regression analyses with or without adjustment for confounding factors. Statistical analyses were performed using SPSS ver. 20 for Windows. All tests were two-sided, and P < 0.05 was taken to indicate statistical significance.
Results
Characteristics of the study population according to shift work
A total of 9105 workers were included in our analyses. There were no significant differences in education level, income status, presence of a spouse, or medical history between non-shift workers and shift workers (Table 1). Hemoglobin A1C level (HbA1C), high-density lipoprotein (HDL), BMI, and axial skeletal muscle mass index were significantly different between the two groups, whereas fat mass index and waist circumference were not significantly different between the two groups (Table 1).
Baseline health behaviors according to shift work type
Health behaviors, including diet, physical activity, smoking, alcohol ingestion, and sleep duration were examined according to the type of work schedule (Table 2). Energy excess, current smoking, current alcohol ingestion, frequency of strength exercise, and sleep duration of less than 5 hours per night were more prevalent in the shift worker group (Table 2). However, carbohydrate intake, protein intake, fat intake, and frequency of walking exercise were not significantly different between shift work and non-shift work groups (Table 2).
Characteristics of shift workers with and without sarcopenia
There were statistically significant differences in energy intake, smoking status, strength exercise frequency, BMI, total fat mass index, HbA1C, HDL, and homeostatic model assessment for insulin resistance (HOMA-IR) index between shift workers with and without sarcopenia (Table 3).
Odds ratio of sarcopenia according to shift work type in univariate and multivariate analyses
Sarcopenia was defined using different calculations, and all types of sarcopenia were associated with the type of shift work after adjustment for socioeconomic factors, health behaviors, fat mass, and laboratory indices (Table 4).
Discussion
In this nationally representative cohort study, we found that sarcopenia was more prevalent in shift workers than in those who had never experienced shift work. Shift workers had an increased risk of sarcopenia even after adjustment for potential confounding factors, including age, sex, low-protein diet, leisure time, physical inactivity, sleep duration, smoking, alcohol intake, insulin resistance, mental illness, and socioeconomic factors. Furthermore, among shift workers, irregularly scheduled shift work was more strongly associated with sarcopenia than regularly scheduled shift work. The results of this study suggest that the circadian rhythm disturbance associated with shift work may contribute to an increased risk of sarcopenia.
To our knowledge, this is the first study to reveal an association between shift work, which is associated with circadian rhythm disturbance, and sarcopenia in a large nationally representative population. Although previous studies have shown that sleep duration is related to sarcopenia, the effect of circadian rhythm disturbance on an increased risk of sarcopenia has not been studied in human populations, although it has been examined on an endocrinological basis in molecular studies24,25,26.
Interestingly, irregularly scheduled shift work was significantly associated with a higher prevalence of sarcopenia compared to regularly scheduled work, even after adjusting for age, sex, diet, physical activity, alcohol intake, and smoking. No previous studies have directly compared the prevalence of sarcopenia between subjects engaged in regular work and those with irregular shift work. Several preliminary reports indicated a higher prevalence of metabolic syndrome among irregularly scheduled shift workers than among regular shift workers. Sun et al. reported that irregular and unscheduled shift workers had higher rates of obesity than did those engaged in regular rotating night shift work27. Further large-scale prospective studies are needed to clarify this issue.
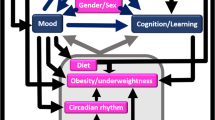
Several pathophysiological mechanisms may explain the relationship between shift work and increased risk of sarcopenia24. There is emerging evidence of crosstalk between circadian cycling and skeletal muscle metabolism24. A preliminary study suggested that the molecular clock, MyoD, and metabolic factors represent a potential system of feedback loops28,29. Beta-adrenergic signaling is considered a pathway involved in coordinating communication between circadian clocks in skeletal muscle24. Given that circadian rhythm is associated with skeletal muscle recovery and build-up and that shift work is associated with disruption of the circadian rhythm21,27,30, shift work and skeletal muscle mass index could be closely associated. However, to our knowledge, no human population-based studies have addressed this issue.
Disruption of the circadian rhythm is associated with the development of a variety of diseases in humans, including metabolic syndrome, cardiovascular disorders, and malignancy6,7,9,15,31. Circadian rhythm disruption may lead to disturbance of internal homeostasis for physiological processes and result in the development of pathologies29. Indeed, shift workers show high prevalence rates of the diseases outlined above32. Moreover, sarcopenic status is known to be closely associated with metabolic syndrome and its complications. The results of the present study indicated that shift work, which disrupts the circadian rhythm, may increase the risk of sarcopenia.
There were several reports that sleep duration <6 hours or >8 hours tended to be associated with sarcopenia. Kwon et al. reported that long sleep duration (≥9 hours) was associated with an increased risk of sarcopenia compared to 7 hours of sleep19. Lucassen et al. reported that poor sleep quality and later sleep times were risk factors for osteopenia and sarcopenia20. They reported that sleep parameters, including decreased sleep quality and later sleep times, were associated with increased risk of sarcopenia20. Kim et al. reported that sleep duration is closely associated with body composition measures26. They revealed that more than 9 hours of sleep duration is independently associated with sarcopenia, especially in women aged > 40 years. In our study, even though <5 hours or > 9 hours of sleep duration were more prevalent in the sarcopenia group compared with the non-sarcopenia group among shift workers, the relationship between sleep duration and sarcopenic status was not statistically significant.
Our study results showed that circadian rhythm disruption is independently associated with sarcopenia even after adjusting for sleep duration. In the present study, we adjusted for sleep duration to examine the association between shift work and the risk of sarcopenia, and we found that circadian rhythm disruption was independently associated with an increased risk of sarcopenia even after adjusting for sleep duration. Sleep duration and circadian rhythm disruption may be associated with sarcopenia in different manners.
This study has several limitations. First, although our results indicated a strong relationship between shift work and sarcopenia, this study should be interpreted cautiously because of its cross-sectional nature. Further large-scale population-based prospective studies are therefore required. Second, although we assessed sleep quality with an extensive questionnaire, other factors may be associated with sleep hygiene, such as obstructive sleep apnea. Obstructive sleep apnea is known to be a determinant of sleep quality and circadian rhythm disruption. Despite these limitations, this study had a number of strengths in that sarcopenia was assessed by dual-energy X-ray absorptiometry in a large nationally representative study population, and we measured extensive potentially confounding factors at baseline, including dietary patterns, leisure time, and physical activity, which are major determinants of sarcopenia.
In conclusion, we evaluated the association between shift work, which is known to disrupt circadian rhythm, and the risk of sarcopenia. As sarcopenia is a well-known risk factor for a variety of diseases, careful examination of sarcopenic status is required among shift workers and other groups with circadian rhythm disruption. Further prospective studies are needed to clarify the causal nature of the relationship between shift work and sarcopenia.
Data Availability
The data used to support the findings of this study are available from the corresponding author upon request.
References
Beaudart, C. et al. Sarcopenia in daily practice: assessment and management. BMC Geriatr 16, 170 (2016).
Santilli, V. et al. Clinical definition of sarcopenia. Clinical Cases in Mineral and Bone. Metabolism 11, 177–180 (2014).
Sanches, I. C. et al. Combined aerobic and resistance exercise training attenuates cardiac dysfunctions in a model of diabetes and menopause. PLoS ONE 13, e0202731 (2018).
Lee, S. J., Park, Y. J. & Cartmell, K. B. Sarcopenia in cancer survivors is associated with increased cardiovascular disease risk. Support Care Cancer 26, 2313–2321 (2018).
Shiraishi, A. et al. Prevalence of stroke-related sarcopenia and its association with poor oral status in post-acute stroke patients: Implications for oral sarcopenia. Clin Nutr 37, 204–207 (2018).
Han, E. et al. Sarcopenia is associated with the risk of significant liver fibrosis in metabolically unhealthy subjects with chronic hepatitis B. Aliment Pharmacol Ther (2018).
Koo, B. K. et al. Sarcopenia is an independent risk factor for non-alcoholic steatohepatitis and significant fibrosis. J Hepatol 66, 123–131 (2017).
Lee, Y. H. et al. Sarcopaenia is associated with NAFLD independently of obesity and insulin resistance: Nationwide surveys (KNHANES 2008–2011). J Hepatol 63, 486–93. (2015).
Jones, S. E. et al. Sarcopenia in COPD: prevalence, clinical correlates and response to pulmonary rehabilitation. Thorax 70, 213–8 (2015).
Polinder-Bos, H. A. et al. Lower body mass index and mortality in older adults starting dialysis. Scientific Reports 8, 12858 (2018).
Kim, J. K. et al. Prevalence of and factors associated with sarcopenia in elderly patients with end-stage renal disease. Clin Nutr 33, 64–8 (2014).
Argeny, S. et al. Visceral fat area measured with computed tomography does not predict postoperative course in Crohn´s disease patients. PLoS ONE 13, e0202220 (2018).
Schink, K. et al. Effects of whole-body electromyostimulation combined with individualized nutritional support on body composition in patients with advanced cancer: a controlled pilot trial. BMC Cancer 18, 886 (2018).
Schreiner, A. J. et al. Periprosthetic tibial fractures in total knee arthroplasty – an outcome analysis of a challenging and underreported surgical issue. BMC Musculoskeletal Disorders 19, 323 (2018).
Park, Y. S. et al. Sarcopenia is associated with an increased risk of advanced colorectal neoplasia. Int J Colorectal Dis 32, 557–565 (2017).
Heo, J. E. et al. Association between appendicular skeletal muscle mass and depressive symptoms: Review of the cardiovascular and metabolic diseases etiology research center cohort. J Affect Disord 238, 8–15 (2018).
Perkisas, S. et al. Prevalence of sarcopenia and 9-year mortality in nursing home residents. Aging Clin Exp Res (2018).
Matsumoto, T. et al. Associations of obstructive sleep apnea with truncal skeletal muscle mass and density. Sci Rep 8, 6550 (2018).
Kwon, Y. J. et al. Long Sleep Duration is Associated With Sarcopenia in Korean Adults Based on Data from the 2008–2011 KNHANES. J Clin Sleep Med 13, 1097–1104 (2017).
Lucassen, E. A. et al. Poor sleep quality and later sleep timing are risk factors for osteopenia and sarcopenia in middle-aged men and women: The NEO study. PLoS ONE 12, e0176685 (2017).
Boivin, D. B. & Boudreau, P. Impacts of shift work on sleep and circadian rhythms. Pathologie Biologie 62, 292–301 (2014).
Kweon, S. et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol 43, 69–77 (2014).
Safiri, S. & Ayubi, E. Sarcopenia based on the Asian working Group for Sarcopenia criteria and all-cause mortality risk in older Japanese adults: Methodological issues. Geriatr Gerontol Int 17, 1759–1760 (2017).
Pearen, M. A. et al. Expression profiling of skeletal muscle following acute and chronic beta2-adrenergic stimulation: implications for hypertrophy, metabolism and circadian rhythm. BMC Genomics 10, 448 (2009).
Lynch, G. S. & Ryall, J. G. Role of beta-adrenoceptor signaling in skeletal muscle: implications for muscle wasting and disease. Physiol Rev 88, 729–67. (2008).
Kim, R. H. et al. Association between Sleep Duration and Body Composition Measures in Korean Adults: The Korea National Health and Nutrition Examination Survey 2010. Korean Journal of Family Medicine 39, 219–224 (2018).
Sun, M. et al. Night shift work exposure profile and obesity: Baseline results from a Chinese night shift worker cohort. PLoS One 13, e0196989 (2018).
Harfmann, B. D., Schroder, E. A. & Esser, K. A. Circadian rhythms, the molecular clock, and skeletal muscle. J Biol Rhythms 30, 84–94 (2015).
Lefta, M., Wolff, G. & Esser, K. A. Circadian rhythms, the molecular clock, and skeletal muscle. Curr Top Dev Biol 96, 231–71 (2011).
Marqueze, E. C., Ulhoa, M. A. & Moreno, C. R. Effects of irregular-shift work and physical activity on cardiovascular risk factors in truck drivers. Rev Saude Publica 47, 497–505 (2013).
Jeong, H. G. et al. Physical Activity Frequency and the Risk of Stroke: A Nationwide Cohort Study in Korea. Journal of the American Heart Association: Cardiovascular and Cerebrovascular Disease 6, e005671 (2017).
Chaudhari, A. et al. Circadian clocks, diets and aging. Nutr Healthy. Aging 4, 101–112 (2017).
Acknowledgements
Guarantor of the article: Dong Kyun Park MD, PhD.
Author information
Authors and Affiliations
Contributions
Dr. Youn I Choi, Dong Kyun Park, and Jun Won Chung contributed to the study concept and design. Dr. Youn I Choi analyzed and interpreted the data. Youn I Choi and Dong Kyun Park drafed the manuscript. Dong Kyun Park, Kyung Oh Kim, Kwang An Kwon, and Yoon Jae Kim critically revised the manuscript for important intellectual content. All authors approved the final version of the manuscript submitted.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Choi, Y.I., Park, D.K., Chung, JW. et al. Circadian rhythm disruption is associated with an increased risk of sarcopenia: a nationwide population-based study in Korea. Sci Rep 9, 12015 (2019). https://doi.org/10.1038/s41598-019-48161-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-48161-w
This article is cited by
-
Development of muscle mass and body fat reference curves for white male UK firefighters
International Archives of Occupational and Environmental Health (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.