Abstract
Primary healthcare is the cornerstone of any healthcare system. A major health system reform to strengthen primary care has been implemented in Germany since 2008. Key components include: voluntary participation, intensive management of patients with chronic diseases, coordination of access to medical specialists, continuous quality improvement, and capitation-based reimbursement. The objective of this study was to assess the effect of this reform on survival of enrolled patients. We conducted a comparative cohorts study with 5-year follow-up, starting in the year 2012 in Baden-Wuerttemberg, Germany. Participants were 1,003,336 enrolled patients and 725,310 control patients. A Cox proportional hazards regression model was applied to compare survival of enrolled patients with a composed control cohort of non-enrolled patients, adjusted for a range of patient and physician characteristics. Average age of enrolled patients was 57.3 years and 56.1% were women. Compared to control patients, they had lower mortality (Hazard Ratio: 0.978; 95% CI: 0.968; 0.989). Participation in chronic disease management programs had independent impact on survival rate (Hazard Ratio 0.744, 95% CI: 0.734; 0.753). We concluded that strong primary care is safe and potentially beneficial in terms of patients’ survival.
Similar content being viewed by others
Introduction
Strong primary care is characterized by the provision first point of access to healthcare for most people and most health issues, high continuity over time and coordination across healthcare providers, and a strong patient-centered approach1. Although insight into the causal mechanisms is limited, epidemiological studies reported on better health outcomes and lower healthcare costs in healthcare systems with strong primary care2,3. Despite these benefits, primary care is under pressure across the world, indicated by shortages of primary care capacity and signals of suboptimal performance. Addressing these challenges is therefore high on the political agenda4,5.
In Germany, health system reforms to strengthen primary care (‘Hausarztzentrierte Versorgung’) have been implemented in the law (Social Code Book V) in the previous decade. These reforms were designed as voluntary contracts between healthcare insurers and primary care physicians, and voluntary enrollment by patients. These have effectively reformed the healthcare system as they scaled-up intensive management of chronically ill patients, coordination of access to medical specialist care, and participation of primary care physicians in continuous quality improvement activities. Studies reported that these programs increased patients’ use of primary care6, reduced number of hospital admissions7 and healthcare costs8. The aim of this study was to assess the effects of the strong primary care model on patient survival.
Results
Description of data
Data on 1,003,336 enrolled patients and 725,310 control patients were available (Table 1). In the population of enrolled patients, the mean age was 57.3 (SD 18.7) years and 56.1% were women. 83.4% had the German nationality, 36.6% were retired, and the mean Charlson-Index for co-morbidity was 1.45. Enrolled patients had been on average nearly 6 years in the program, meaning from one year before start of the observation period of this study. The cohort of non-enrolled patients had slightly different descriptive features, for instance younger average age (54.4 years) and fewer co-morbidities (mean Charlson-Index 1.14).
Healthcare utilization
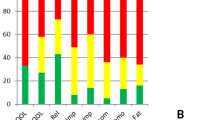
The mean number of yearly contacts in primary care was 13.65, while the number of uncoordinated contacts with medical specialists was 2.06. The average number of hospital admissions per 100 enrolled patients was 29.0 and the average yearly medication costs were 1452 euro. Control patients had partly different healthcare utilization, most particularly fewer yearly contacts in primary care (9.01 on average) and more uncoordinated contacts with medical specialists (3.37).
Survival
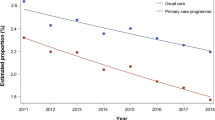
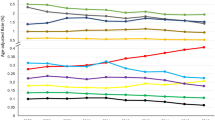
Figure 1 presents the survival rates of enrolled and non-enrolled patients. Compared to control patients, enrolled patients in the program had lower mortality (Hazard Ratio: 0.978; 95% CI: 0.968; 0.989). Table 2 presents which factors were associated with survival. Participation in disease management programs had independent positive impact on survival (Hazard Ratio 0.744, 95% CI: 0.734; 0.753). An estimated total number of 1,672 lives was saved in the strong primary care arm.
Discussion
This study in routine healthcare found lower 5-year mortality in patients enrolled in strong primary care as compared to a comparable cohort of non-enrolled patients. Although the small effect should be carefully interpreted, given the non-randomized study design, it was found in a large population in a naturalistic setting and adjusted for many potential confounders. The descriptive data on healthcare utilization suggest that the healthcare delivery model was successfully implemented in enrolled patients. Overall, the study shows that the strong primary care model (including a change to capitation-based reimbursement and structured management patients with chronic diseases) was safe and potentially beneficial in terms of patients’ survival.
Strengths of the study are the inclusion of the total eligible and large study population, the naturalistic setting, and extensive adjustment for potential confounders in the analysis. The influence of patient self-selection was reduced by composing a control cohort on the basis of patients from non-participating physicians; these patients did not have the option to enroll. However, the influence of physician self-selection cannot be ruled out. As the observation period started four years after initiation of the program and high numbers of physicians have joined the healthcare delivery model, it seems plausible that not only early adopters of the innovative program had joined.
Evaluation of the patient-centred medical home, a healthcare delivery model which has many features of strong primary care, found increased quality of chronic disease care and reduced overall healthcare utilization and costs3,9. It seems to comprise many components of strong primary care10. This study confirms these findings in a healthcare system, which shares several features with the healthcare system in the United States. Our study suggested that participation in disease management – one component of strong primary care - was associated with higher survival. While this subgroup effect should be interpreted carefully, it is supported by a substantial body of research in primary care11. The relatively high number of patients’ yearly number of contacts in primary care may facilitate various beneficial activities, such as screening for health problems, monitoring of diagnosed diseases, psychosocial support, and intensive care after hospital discharge. Nevertheless, further research is needed to provide insight into the working mechanisms in strong primary care.
Methods
Study design
The study is based on the total population of enrolled patients and a composed comparison cohort in Baden-Wuerttemberg, a state in South-West Germany with about 11 million inhabitants and high enrollment in the strong primary care program. The study has a longitudinal, comparative observational design with five years of follow-up. It was based on routinely recorded data from ambulatory medical practice, derived from administrative databases of the largest regional health insurer and partner of the program (AOK Baden Wuerttemberg). It provides health insurance to about 4.4 million individuals; almost 1.5 million of them and about 4.000 primary care physicians were enrolled in the strong primary care model in 2016. These patients were compared with a composed cohort of non-enrolled patients from the same state. The Heidelberg University Hospital Ethics Committee approved the study (No. S-359/2013) and the study was conducted to relevant regulations and methodological guidance. The presented data and interpretations are a very small part of a comprehensive evaluation report12 and a summary version13 in the German language. The STROBE reporting guideline for cohort studies was followed in preparing this manuscript.
Study population
Eligible were individuals aged 18 years or older, living in Baden-Wuerttemberg, at least one visit to the primary care physician in the year of enrollment, health insurance with AOK, no enrollment in other integrated care programs. Patients enter or (after one year) leave the program as they wish. They were included in the intervention arm if they were registered at start of observation (the year 2012) and remained included (without interruptions) until death or end of observation five years later (the year 2016). Patients enrolled in the program provided informed consent before participation. They were compared with a control cohort, comprising of eligible patients in the observed years in the same state and health insurer, who were linked to physicians who did not participate in the program (thus, control patients never had to opportunity to decide on participation). These control patients were linked post-hoc to the primary care physician, whom they had visited in at least 50% of their contacts in primary care. If no such linkage was possible, they were excluded from analysis.
Primary care model
Enrollment in the healthcare delivery model is a free choice for both patients and physicians. The physician receives additional secured reimbursement for each enrolled patient (capitation instead of fee-for-service). Key component of the program include: improved access to primary care for patients (shorter waiting times, absence of out-of-pocket payment for medication); more comprehensive coverage through extended medical training by physicians; gate-keeping in access to secondary care; improved information transfer between primary and secondary care; structured disease-management for diabetes, asthma/COPD, coronary heart disease run in the primary care practices; continued medical education is coordinated and independent of industry; data-drive quality improvement; and use computerized decision support for drug prescribing. Details of the program have been described elsewhere6.
Measures
The primary outcome in this study was overall survival of patients as documented in the administrative database of the health insurer in the years 2012 to 2016. Patient age, sex, urbanity, recorded morbidities, nursing need, nursing home were documented. The Charlson-Index was calculated to summarize comorbidity14. We also documented selected indicators of the fidelity of the healthcare delivery model: numbers of contacts in primary medical care, non-coordinated contacts with medical specialists, hospital admissions, and costs of ambulatory prescribed medication. All measures were based on data in administrative databases and similarly defined as in previous evaluations6,7.
Data-analysis
Differences between the two cohorts (presented in Table 1) were statistically tested. The statistical analysis focused on the comparison of survival rates between the intervention and control cohorts, using Cox proportional hazards regression models. Given the self-selection of physicians and patients into the intervention arm, we first identified predictors of physician participation (considering age, gender, urban/rural, practice size) and predictors of patient participation (considering age, gender, urban/rural, Charlson-Index, and participation in disease management programs) in (separate) logistic regression analyses. Baseline predictors with significant impact (P < 0.01, two-sided test) were included in the primary analysis as co-variables. It may be noted that statistically significant between-group differences at baseline do not necessarily imply confounding in the estimation of intervention effectiveness, because the variables may not be prognostic for outcomes15. In order to check the proportional hazards assumption16, the ASSESS-statement of SAS procedure PHREG17 was used; this showed that it was fulfilled. In the final regression models, effects were expressed with 95% confidence intervals. The Population Attributable Fraction (PAF)18 was used to calculate “saved lives” within the observation period, adjusted for confounders. PAF is the estimated fraction of all cases that would have occurred (death) if there had been no enrolment in the strong primary care program, adjusted for measured confounders. The analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, North Carolina, USA).
Ethics approval
Ethics approval was provided by the Heidelberg University Hospital Ethics Committee (No. S-359/2013).
Data Availability
AOK Baden-Wuerttemberg can be contacted for secondary analyses of their administrative data.
References
Phillips, R. L. et al. The future role of the family physician in the United States: a rigorous exercise in definition. Ann. Fam. Med. 12, 250–255 (2014).
Starfield, B., Shi, L. & Macinko, J. Contribution of primary care to health systems and health. Milbank Q. 83, 457–502 (2005).
Friedberg, M. W., Rosenthal, M. B., Werner, R. M., Volpp, K. G. & Schneider, E. C. Effects of a Medical Home and Shared Savings Intervention on quality and utilization of care. JAMA Intern. Med. 175, 1362–1368 (2015).
Ellner, A. L. & Phillips, R. S. The coming primary care revolution. J. Gen. Intern. Med. 32, 380–386 (2017).
Sessums, L. L., McHugh, S. J. & Rajkumar., R. Medicare’s vision for advanced primary care. New directions for care delivery and payment. JAMA 315, 2665–2666 (2016).
Wensing, M., Szecsenyi, J., Stock, C., Kaufmann-Kolle, P. & Laux, G. Evaluation of a program to strengthen general practice care for patients with chronic disease in Germany. BMC Health Serv. Res. 17, 62, https://doi.org/10.1186/s12913-017-2000-2 (2017).
Wensing, M., Kaufmann-Kolle, P., Szecsenyi, J., Stock, C. & Laux, G. Effects of a program to strengthen general practice care on hospitalisation rates: a comparative observational study. Scan. J. Prim. Care. 36, 109–114 (2018).
Schneider, A. et al. Costs of coordinated versus uncoordinated care in Germany: results of of a routine data analysis in Bavaria. BMJ Open 6, e011621, https://bmjopen.bmj.com/content/6/6/e011621.long (2016).
Friedberg, M. W., Schneider, E. C., Rosenthal, M. B., Volpp, K. G. & Werner, R. M. Association between participation in multilayer medical home intervention and changes in quality, utilization and costs of care. JAMA 311, 815–825 (2014).
Bodenheimer, T., Ghorob, A., Willard-Grace, R. & Grumbach, K. The 10 building blocks of high-performing primary care. Ann. Fam. Med. 12, 166–171 (2014).
Reynolds, R. et al. A systematic review of chronic disease management interventions in primary care. BMC Fam Pract 19, 11, https://doi.org/10.1186/s12875-017-0692-3 (2018).
Gerlach, F. M., Szecsenyi, J. & Haefeli, W. E. Evaluation der Hausarztzentrierten Versorgung (HZV) nach §73B SGB V in Baden-Württemberg (2011–2016). (Johann Wolfgang-Goethe Universität Frankfurt und Universitätsklinikum, Heidelberg 2018).
Gerlach, F. M., Szescenyi, J. & Haefeli, W. E. Evaluation der Hausarztzentrierten Versorgung (HZV) in Baden-Württemberg. Zusammenfassung der Ergebnisse 2011–2016. (Johann Wolfgang-Goethe Universität Frankfurt und Universitätsklinikum Heidelberg, 2018).
Sundararajan, V. et al. New ICD‐10 version of the Charlson comorbidity index predicted in‐hospital mortality. J. Clin. Epidemiol. 57, 1288–1294 (2004).
De Boer, M. R., Waterlander, W. E., Kuijper, L. D. J., Steenhuis, I. H. M. & Twisk, J. W. R. Testing for baseline difference in randomized controlled trials: an unhealthy research behaviour that is hard to eradicate. Int J Behav Nutr Phys Acti 12, 4, https://doi.org/10.1186/s12966-015-0162-z (2015).
Lin, D., Wei, L. J. & Ying, Z. Checking the Cox Model with Cumulative Sums of Martingale-Based Residuals. Biometrika 80, 557–572 (1993).
Donithan, M., Van Natta, M. & Tonascia, J. Cox regression analyses using SAS/PHREG. Control. Clin. Trials 13(5), 420 (1992).
Mansournia, M. A. & Altman, D. G. Population attributable fraction. BMJ 360, k757 (2018).
Acknowledgements
The study is part of a larger evaluation, which was funded by AOK Baden-Wuerttemberg, which is partner in implementation of the strong primary care model. The evaluators are scientifically independent.
Author information
Authors and Affiliations
Contributions
J.S. and G.L. designed the evaluation project and arranged funding. P.K.K. coordinated data-management and G.L. did the data-analysis. M.W. designed the presented study and wrote the manuscript. All authors provided substantial inputs and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
Joachim Szecsenyi holds stocks in the AQUA-Institute, which provides services to AOK Baden-Wuerttemberg. He also has a long and ongoing collaboration with AOK Baden-Wuerttemberg, which involved payment to Heidelberg University Hospital of scientific services. Other authors have no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wensing, M., Szecsenyi, J., Kaufmann-Kolle, P. et al. Strong primary care and patients’ survival. Sci Rep 9, 10859 (2019). https://doi.org/10.1038/s41598-019-47344-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-47344-9
This article is cited by
-
Evaluation of a collaborative ambulatory orthopedic care program for patients with hip and knee osteoarthritis: a comparative observational cohort study
BMC Musculoskeletal Disorders (2022)
-
Continuity in general practice and hospitalization patterns: an observational study
BMC Family Practice (2021)
-
Measuring care coordination in German primary care – adaptation and psychometric properties of the Medical Home Care Coordination Survey
BMC Health Services Research (2021)
-
Strong and sustainable primary healthcare is associated with a lower risk of hospitalization in high risk patients
Scientific Reports (2021)
-
Intensified ambulatory cardiology care: effects on mortality and hospitalisation—a comparative observational study
Scientific Reports (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.