Abstract
Early-life experiences may fuel the emergence of obesity and type 2 diabetes among African populations. We evaluated childhood socio-economic status (SES) and childhood nutritional status as risk factors for increased waist circumference and type 2 diabetes among Ghanaian adults. In the multi-center, cross-sectional Research on Obesity and Diabetes among African Migrants (RODAM) Study, we calculated associations (adjusted for demographics and lifestyle) of parental education and anthropometric markers of childhood nutrition [leg length, leg length-to-height ratio (LHR)] with waist circumference and type 2 diabetes, respectively. Among 5,575 participants (mean age: 46.2 years; 62% female), lower education of either parent (vs. higher) was consistently associated with higher waist circumference (∆: 1.6–3.4 cm). Lower father’s education tended to increase the odds of type 2 diabetes by 50% in women (95% confidence interval (CI): 1.0, 2.4). Reduced leg length and LHR were associated with higher waist circumference. But only in men, leg length was inversely related to type 2 diabetes (OR per 1 standard deviation decrease: 1.1; 95% CI: 1.0, 1.3). In this study, markers of poor childhood SES and early-life nutritional status relate to abdominal obesity in men and women and to type 2 diabetes in men. Thus, prevention efforts should start in early childhood.
Similar content being viewed by others
Introduction
Obesity and type 2 diabetes are important public health issues globally1,2. There is accumulating evidence of the increasing burden of both obesity and type 2 diabetes in sub-Saharan Africa (SSA). Yet, the prevalence rates vary considerably between adults in SSA and among SSA migrants3. Increased life expectancy, rapid urbanization and its associated lifestyle changes are potential drivers of the upsurge of obesity and type 2 diabetes in SSA4. Still, undernutrition continues to plague both children and adults in SSA, while the co-existence with overnutrition has been described for the same settings5. In fact, the abundance of undernutrition and the rapid environmental changes in SSA and for first-generation migrants from Africa to Europe might constitute one of the underlying causes of the emergence of metabolic conditions in these populations. There is evidence from high-income countries linking early-life conditions and childhood growth patterns to the pathogenesis of chronic diseases6,7. Low childhood socioeconomic status (SES) and undernutrition during early development have been shown to be associated with an increased risk of obesity and type 2 diabetes8,9. Still, the evidence is scarce and inconsistent for African-descent populations10,11.
According to the mismatch hypothesis within the Developmental Origins of Health and Disease (DOHaD) framework, a deprived developmental environment sets up an individual’s metabolism to nutrient scarcity. This programming effect becomes detrimental when the mature environment is characterized by nutritional abundance12. Exploring the associations of childhood SES and undernutrition with obesity and type 2 diabetes could offer insights into the increasing burden of these conditions in SSA.
Therefore, we aimed to assess whether childhood SES and childhood nutritional status are associated with abdominal obesity and type 2 diabetes in adulthood, independently of adult SES in a homogenous population of Ghanaians living in different geographical locations (rural Ghana, urban Ghana and Europe). We hypothesized that adverse pre-adulthood social environments measured by parental education and anthropometric markers of childhood undernutrition (defined as leg length and leg length-to-height ratio) are associated with increased risks of abdominal obesity and type 2 diabetes, and that the associations are independent of adult lifestyle and SES.
Methods
Study design and procedures
The study protocol and procedures of the Research on Obesity and Diabetes among African Migrants (RODAM) study have previously been published13. In brief, this multi-center cross-sectional study was conducted among Ghanaian adults (25–70 years) in rural Ghana, urban Ghana, and Europe (Amsterdam, London, and Berlin) between July 2012 and September 2015 (N = 6,385). The primary objective of the RODAM study was to disentangle the relative contributions of (epi)genetic and non-genetic risk factors for type 2 diabetes and obesity. For recruitment, in Ghana, census data of 2010 were used to draw rural and urban participants in the Ashanti Region. In Amsterdam, the Municipal Register was used to randomly select Ghanaian migrants who were then invited by postal mail and home visits. In London and Berlin, Ghanaian organizations, church communities and social unions served as the sampling frame for recruitment. The response rates were 76% in rural Ghana and 74% in urban Ghana. In Amsterdam, 67% replied by response card or after a home visit. Of these, 53% agreed and participated in the study. In London, of those individuals who were invited based on their registration in Ghanaian organizations, 75% agreed and participated in the study. In Berlin, this figure was 68%3.
Fasting plasma glucose (FPG; mmol/L) was measured in venous blood samples using the ABX Pentra 400 chemistry analyzer (HORIBA ABX SAS, Montpellier, France). Type 2 diabetes was defined as FPG ≥7.0 mmol/L or documented glucose-lowering medication or self-reported diabetes. Medical history, lifestyle and socio-economic factors were recorded either by ethnically matched staff in questionnaire-based interviews or by self-report. Trained study personnel performed the physical examination, including anthropometric measurements.
Ethics statement
The RODAM Study was conducted according to the guidelines laid down in the 1964 Declaration of Helsinki and its later amendments. All procedures involving human subjects were reviewed and approved by the respective ethics committees in Ghana (Committee on Human Research, Publication and Ethics, Kwame Nkrumah University of Science and Technology, Kumasi), the Netherlands (Medical Ethics Review Committee, Academic Medical Centre, University of Amsterdam), the UK (Observational/Interventions Research Ethics Committee, London School of Hygiene and Tropical Medicine), and Germany (Ethics Commission, Charité – Universitaetsmedizin Berlin). Written informed consent was obtained from all participants.
Questionnaire-based data
The educational levels of the participants and their parents were recorded according to the following categories: never been to school or elementary school, lower vocational schooling, i.e. <2 years training or lower secondary schooling, intermediate vocational schooling, i.e. 2 years training or intermediate/higher secondary schooling, and higher vocational schooling, i.e. ≥3 years training or university. Occupational class was recorded for the participants only and was classified as “high” (professionals, managers, clerical support staff, higher grade routine non-manual employees service and sales related occupations) and “low” (craft and related trades workers, elementary occupations and farmers) (International Standard Classification of Occupations scheme; ISCO-08). In addition, sociodemographic (age and sex) and lifestyle factors were obtained. Smoking status was recorded as current, former or never. Physical activity was assessed using the World Health Organization (WHO) STEPwise approach to chronic disease risk factor Surveillance (STEPS) Questionnaire and was categorized as high, moderate, or low. Energy intake was calculated from a semi-quantitative Ghana-specific Food Propensity Questionnaire (Ghana-FPQ) which queried for the usual food intake of the preceding 12 months. The latest versions of the West African Food Composition Table and the German Nutrient Database (BLS 3.01, 2010) were applied to convert food intake data into energy intake.
Anthropometric examinations
All participants underwent an anthropometric examination in light clothing and without shoes. Body weight (kg) was measured using a portable electronic scale (SECA 877) to the nearest 0.1 kg, height (cm) by a portable stadiometer (SECA 217) to the nearest 0.1 cm, and waist circumference (cm) measured at the at the midpoint between the lower rib and the upper margin of the iliac crest using a measuring tape. Body mass index (BMI) was calculated as weight/(height)2 (kg/m2). Abdominal obesity was defined as waist circumference >102 cm for men, and >88 cm for women. Adult leg length is particularly sensitive to nutrition in early childhood14. Therefore, we measured sitting height with the participant sitting upright on the base plate on a flat seat, and with the heads in the Frankfort plane position, feet on the floor and with the thighs unsupported. Leg length (cm) was calculated as (standing height − sitting height) + stool height, while leg length-to-height ratio (LHR) was calculated as leg length divided by standing height15. Fat-free mass was examined using bio-electric impedance (BODYSTAT 1500 MDD analyser) with an African-specific equation.
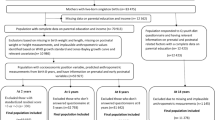
Statistical analysis
Supplemental Fig. S1 shows the flow chart of imputed raw data and excluded participants because of implausible values for composite measures yielding a final sample size of 5,575 participants. A small proportion had missing values for waist circumference (0.3%), but a considerable proportion had missings for leg length, height and parental education (24%), and for the socio-demographic and lifestyle factors (45%). Excluding these participants might have led to biased results and a loss in statistical power. Therefore, multiple imputation was applied (n = 5; discriminant fully conditional specification (FCS) method). FCS is also known as multiple imputation by chained equations (MICE) and uses separate conditional univariate imputation models specified for each incomplete variable, with other variables as predictors16. We assumed that the propensity of missing data can be explained by the observed data (missing at random, MAR), because the proportions of missingness were similar between the groups with and without type 2 diabetes (Fig. S1). This assumption was further corroborated by the good imputation efficiency (98–100%).
Descriptive statistics were used to present the general characteristics of the study population and the distributions of early-life factors according to sex and study site.
Paternal education and maternal education were categorized as never/low, intermediate, and high; we used high education as the reference. Relationships between parental education and the adult educational level and occupational class were calculated by partial Spearman correlations, adjusted for age and study site. For leg length and LHR, sex-specific quintiles were constructed, and the highest category was used as the reference. Among Ghanaians, multiple parenthood and child fostering are common practices17. Therefore, we did not assume that the combination of father’s and mother’s educational levels reflected the true SES during childhood.
All regression models were calculated separately for men and women owing to their differences in body fat distribution and adipose tissue function18. With regard to abdominal obesity, we modeled waist circumference as a transient phenotype and thus, as a continuous variable. The PROC MIANALYZE procedure in SAS was used to calculate sex-specific pooled ß-coefficients, 95% confidence intervals (CIs) and p-values for the associations of parental education with waist circumference by linear regressions. Also, the associations of leg length and LHR with waist circumference were evaluated per 1 standard deviation (SD) decrease using pooled effect estimates of linear regression models. Model 1 accounted for age (years) and study site (5 categories); Model 2 was additionally adjusted for the most important lifestyle risk factors of adiposity and type 2 diabetes: smoking (current or former/non-smoker), physical activity (MET-h/week), and energy intake (kcal/d). For leg length, Model 3 additionally accounted for body height (cm).
With respect to type 2 diabetes, we calculated sex-specific pooled odds ratios (ORs), 95% CIs and p-values by logistic regression models. Model 1 was adjusted for age and study site; and Model 2 additionally accounted for smoking status, physical activity, energy intake, BMI and waist circumference. The associations with type 2 diabetes were calculated per quintiles and per 1 SD decrease of leg length and LHR, respectively.
Despite the lack of statistically significant interactions with study site, we calculated multiple-adjusted associations of leg length and LHR with waist circumference and with type 2 diabetes according to study site to comment on potential effect modification. Because of sample size constrains, this was not done for parental education. Complete-case analysis was performed to examine the robustness of our results. Also, we evaluated effect mediation: Adult socio-economic status per se has been related to higher odds of type 2 diabetes in the RODAM study population19, and thus, could lie on the causal pathway from parental education in childhood to higher waist circumference and increased odds of type 2 diabetes in adulthood. Similarly, childhood nutritional status may act via fat-free mass on the adult metabolic profile, whereby fat-free mass reflects the attained metabolic capacity of muscle mass20. These proposed mediators were included in the final regression models to assess effect attenuation. Moreover, we assessed potential confounding: by diabetes family history when parental education was examined, and by hip circumference when leg length was considered. Potential changes in the effect estimates were examined by including likely confounders in the final regression models.
Results
Study population
The general characteristics of the study population according to sex and study site are presented in Supplemental Table S1. In brief, RODAM participants were mainly female (62%) and middle-aged (mean age, 46.2 ± 10.8 years). The mean waist circumference in the study population was 90.7 ± 12.6 cm, and was higher in women than in men. The crude prevalence of type 2 diabetes was 9.4%. This figure was lower in women than in men and was highest in Europe, followed by urban Ghana and rural Ghana. Men were older, had a higher educational status, had lower BMI and waist circumference, were more likely to be former or current smokers, were more physically active, and had higher daily energy intake than women. RODAM participants in Europe had the highest level of education, were more frequently former or current smokers, presented with higher BMI and waist circumference, and men in Europe had higher energy consumption than their counterparts in Ghana. The mean length of stay in Europe was 16.9 ± 9.9 years, and 99% were first-generation migrants. RODAM participants in rural Ghana had the lowest level of education, the lowest BMI and waist circumference, and were physically more active than those in urban Ghana and Europe.
With regard to the early-life factors (Table 1), the parental education was similar for men and women. Father’s and mother’s education were lowest for the participants living in rural Ghana and was highest in Europe. For leg length and LHR, men had longer legs than women. Leg length among men was lowest in rural Ghana, followed by urban Ghana and Europe, while no differences according to study site were discernible among women. For men, partial Spearman correlations of parental education with adult education ranged from +0.27 to +0.31 (p < 0.0001) and with adult occupation from −0.21 to −0.19 (p < 0.0001). For women, these figures were +0.27 to +0.34 (p < 0.0001) and −0.16 to −0.16 (p < 0.0001), respectively.
Associations with parental education
Table 2 presents the associations of parental education with waist circumference and with type 2 diabetes, separately for men and women. In general, the educational level of the parents was inversely associated with waist circumference. For instance, in men, lower paternal education as compared to higher was associated with an increased waist circumference of 3.6 cm (95% CI: 2.1, 5.1 cm) when adjusted for age and study site. This association was also seen for maternal education and remained in the lifestyle-adjusted Model 2. For women, these inverse relationships between parental education and waist circumference were also observed (Table 2).
For type 2 diabetes, among men, neither father’s nor mother’s education were associated with this outcome. In contrast, among women, lower father’s education as compared to higher education tended to increase the odds of type 2 diabetes by 50% (1.50; 95% CI: 0.96, 2.36) in the multiple-adjusted Model 2. Otherwise, parental education was not associated with type 2 diabetes among women. Owing to sample size constraints, no further stratification by study site was performed.
Associations with leg length and leg length-to-height ratio
The sex-specific associations of leg length and LHR with waist circumference are presented per quintiles and per 1 SD decrease in Table 3. Absolute leg length was directly associated with waist circumference in Models 1 and 2 among men and women. However, these effects reversed after accounting for body height in Model 3. In men, 1 SD reduction in leg length (1 SD = 4.4 cm) increased waist circumference by 1.72 cm (95% CI: 0.89, 2.54 cm). In women (1 SD = 4.1 cm), this increment was 2.42 cm (95% CI: 1.64, 3.20 cm). Also, LHR was associated with higher waist circumference in men and women (Table 3). In men, 1 SD reduction in LHR resulted in an increase of 0.50 cm (95% CI: 0.05, 0.95 cm), while in women this effect was 0.76 cm (95% CI: 0.33, 1.18 cm). The inverse associations of leg length and LHR were strongest in urban Ghana (Supplemental Table S2).
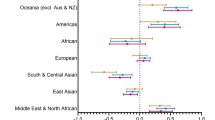
With regard to type 2 diabetes, the associations per quintiles of leg length and LHR are depicted in Fig. 1. Among men, lower quintiles tended to increase the odds of type 2 diabetes in the multiple-adjusted Model 2 (OR per 1 SD leg length decrease: 1.11; 95% CI: 0.95, 1.30; p = 0.186). However, quintile 3 showed the lowest odds of type 2 diabetes. Further, we explored the associations between absolute and relative leg lengths according to study location. The inverse tendency for the LHR-diabetes-relationship was strongest in rural Ghana (Table S2), but was neither seen for women nor for LHR (Fig. 1).
Multiple-adjusted associations of (A) leg length (cm) and (B) leg length-to-height ratio with type 2 diabetes stratified by sex. Odds ratios and 95% confidence intervals (error bars) for type 2 diabetes were calculated by logistic regression and were adjusted for age (years), study site (5 categories), smoking (current or quit/never), physical activity (MET-hours/week), energy intake (kcal/d), body mass index (kg/m2), and waist circumference (cm).
Sensitivity analyses
Compared to the results from imputed data, the associations in a complete-case analysis became stronger in men and weaker in women for waist circumference. For type 2 diabetes, there were no major changes (Supplemental Table S3). With regard to adult socio-economic variables, we evaluated whether adult education or adult occupation mediated the observed relationships with parental education (Supplemental Table S4). For waist circumference, the associations were attenuated by adult education and adult occupation. The changes in estimates were slightly stronger when accounting for adult education. Next, the inverse association between father’s education and type 2 diabetes in women attenuated from OR = 1.5 (95% CI: 1.0, 2.4) to OR = 1.4 (95% CI: 0.9, 2.2). Otherwise, the effect estimates for parental education on type 2 diabetes remained. Also, the inclusion of diabetes family history did not alter the relationships between parental education and diabetes status (data not shown). Lastly, for the associations of leg length and LHR with type 2 diabetes, we evaluated potential effect mediation by fat-free mass and adult SES as well as possible confounding by hip circumference and parental education. Yet, none of these factors changed the estimates (data not shown).
Discussion
Summary of main results
The present study investigated the mismatch hypothesis of adverse early-life factors conferring increased risks of abdominal obesity and type 2 diabetes among Ghanaian adults facing rapid environmental changes. Indeed, low childhood SES defined as low education of one parent was consistently associated with higher waist circumference among men and women. Partly, these effects were explained by the fact that low parental education was associated with lower adult educational level and lower adult occupational class, which in turn were related to higher waist circumference and type 2 diabetes risk19. Also, there was a tendency for increased odds of type 2 diabetes in women when the education of the father was lower. Moreover, childhood undernutrition defined as low absolute and relative leg lengths tended to be associated with higher odds of type 2 diabetes in men and was associated with higher waist circumference in both sexes. These relationships were more pronounced in Ghana than in Europe and were largely independent of parental education.
Associations of parental education with waist circumference and type 2 diabetes
The inverse association between parental education and waist circumference was observed in both men and women, although stronger in men. The association was partly explained by the participant’s own educational attainment and occupation. This finding is consistent with that from previous studies which have reported a higher risk of CVD and its associated factors such as obesity and type 2 diabetes in men and women with lower childhood SES21,22. In a large cohort of British children studied from birth to 36 years, men and women from lower childhood socioeconomic backgrounds were more inclined to be overweight or obese in adulthood23. Adult SES has partly explained the observed association in some but not all previous studies24,25,26. Several mechanisms underlying these observations independent of access to health care have been proposed, including physical, environmental, behavioral and psychosocial exposures21,22. Lower SES in childhood has been reportedly associated with diseases caused largely by behavioral risk factors such as smoking, physical inactivity and unhealthy diets27. Possibly, children of lower SES are more likely to live in homes and neighborhoods less conducive for engaging in physical activity, placing them at higher risk of childhood obesity which may set health-damaging trajectories that continue through adulthood21.
There was no clear association between childhood SES and type 2 diabetes in men in our study, although there was a tendency for increased odds of type 2 diabetes in women from a lower childhood SES, independent of current BMI and other risk factors. This was contrary to the inverse association reported in some28 but not all previous studies29. Lower paternal education has been reported to be more obviously associated with type 2 diabetes in women than in men in a previous study29. It remains unclear why the association between childhood SES and type 2 diabetes was not as obvious in our study, given the observed association with waist circumference.
Associations of leg length with waist circumference and type 2 diabetes
In the present study, absolute and relative leg lengths were associated with higher adult waist circumference in men and women and tended to increase the odds of type 2 diabetes in men. Among white populations living in high-income countries, shorter legs and lower LHR are consistently associated with higher measures of adiposity and diabetes-risk, including the PROMISE cohort in Canada as well as NHANES III and ARIC in the USA11,20,30,31. Still, the evidence has been scarce and inconclusive for individuals of African descent and for populations in less-developed regions, such as China and Brazil10,11,30,32,33.
Body height per se is determined by genetic and environmental factors, whereas the anthropometric measures of disproportion such as leg length and LHR sensitively indicate postnatal childhood nutritional status15. The results of the present study are therefore in accordance with the hypothesis that individuals are prone to develop cardio-metabolic diseases when a nutrient-insufficient developmental environment conflicts with nutrient surplus in the future12. Indeed, Ghana experienced three major droughts in 1971, 1977 and 198334, in addition to a period of military rule and economic crisis between 1964 and 1992. For the present study population of Ghanaian adults aged ≥35 years, this means that the majority were exposed to at least one period of famine in their childhood. After that, in the last decades, Ghana’s economy has rapidly improved. The Gross Domestic Product (GDP) has increased from US$ 4.5 billion in 1980 to US$ 42.7 billion in 2016, and more than half of Ghana’s population today lives in large cities35. Such economic boost and the sudden environmental change upon urbanization and migration to Europe might have led to a nutrition transition, as observed across the RODAM study sites. In rural Ghanaian sites, the diet relies on tuberous foods, legumes and fish, while in urban Ghana and Europe, ruminant meat, dairy products, sweet snacks and energy-containing beverages predominate36. Partially, this argues for a pronounced mismatch between the developmental and the mature environments among urban Ghanaians and migrants in Europe, corroborating the stronger inverse associations of leg length and LHR with waist circumference as compared to rural Ghana.
The biological mechanisms underlying the increased susceptibility of abdominal obesity and type 2 diabetes in this transitional society may include the accumulation of fat mass upon chronic childhood undernutrition14, possibly, because of impaired appetite control37 and reduced fat oxidation38. Also, delayed growth in childhood contributes to altered organ development and reduced skeletal muscle mass, resulting in impaired pancreatic function and reduced peripheral insulin sensitivity, respectively39,40. However, in our study, adjustment for fat-free mass as a measure of skeletal muscle mass did not contribute to the association between leg length and type 2 diabetes.
In addition, there was a lack of association for absolute and relative leg lengths with type 2 diabetes among women in our study. Smaller variations in leg length and LHR, and a lower prevalence of type 2 diabetes among females (8%) as compared to males (11%) could explain this null-finding. It is also conceivable that selective survival might have affected our results. The vicious circle of poor childhood nutritional status and infectious diseases still leads to a mortality rate of 5.9% among children <5 years of age in Ghana35, presumably attenuating the leg length-diabetes association in adulthood.
Strengths and limitations
The present analysis stems from a large, homogenous study population of SSA adults living in Ghana and in Europe. The participants originated from the same geographic region in Ghana and likely were exposed to the historic waves of famine and food crisis in the country. Still, we cannot fully exclude the positive selection of more affluent individuals migrating to Europe and the negative selection of people who experienced severe childhood undernutrition and illness. Multiple imputation was applied for an unbiased analysis of the full dataset. Under the MAR assumption, this method is useful even when 90% of the data are missing41. In our regression models, we accounted for a wide range of possible confounders and potential mediators. Still, unmeasured and residual confounding cannot be ruled out. Similar to most previous studies examining early-life factors on adult health, our study included assessment of only one SES marker. We did not take into account other components of SES that could potentially have an impact on health such as household income and living conditions during childhood, as well as SES across the entire life-course. Previously, the recollection of parental education has less likely been associated with recall bias41,42. We are aware of the genetic and the socio-economic components of attained height and leg length, and adjusted for parental education in our sensitivity analyses. Still, relative leg length represents a widely accepted and objective marker of early childhood nutritional status15. While the cross-sectional nature of our study impedes causal inference and the investigation of cumulative effects across the life-course, the exposures of interest were likely established before the onset of metabolic disturbances in adulthood.
Conclusions
Interventions to prevent abdominal obesity may have to consider targeting the early childhood period and adults who had experienced lower SES in childhood. Further studies examining the association of early-life socioeconomic and nutritional factors with waist circumference and type 2 diabetes are needed in lower- and middle-income populations. This is of particular importance in the light of the reported increasing burden of abdominal obesity and type 2 diabetes, emerging alongside an unfinished agenda of undernutrition and other poverty related diseases in these settings. Our findings emphasize that targeted improvement of early-life circumstances can have benefits not just for children but also in reducing the risks of metabolic disease in later adult life.
Data Availability
The datasets analysed during the current study are not publicly available due to the terms of consent to which the participants agreed, but are available from the corresponding author on reasonable request.
References
International Diabetes Federation (IDF). Diabetes Atlas, 7th ed, http://www.diabetesatlas.org/ (2018).
Ng, M. et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 384, 766–81 (2014).
Agyemang, C. et al. Obesity and type 2 diabetes in sub-Saharan Africans - Is the burden in today’s Africa similar to African migrants in Europe? The RODAM study. BMC Med. 14, 166 (2016).
Kengne, A. P., Echouffo-Tcheugui, J. B., Sobngwi, E. & Mbanya, J. C. New insights on diabetes mellitus and obesity in Africa-part 1: prevalence, pathogenesis and comorbidities. Heart. 99, 979–83 (2013).
Agyei-Mensah, S. & de-Graft Aikins, A. Epidemiological transition and the double burden of disease in Accra, Ghana. J Urban Health. 87, 879–97 (2010).
Eriksson, J. G. Early growth and coronary heart disease and type 2 diabetes: findings from the Helsinki Birth Cohort Study (HBCS). Am J Clin Nutr. 94, 1799s–802s (2011).
Lawlor, D. A., Ebrahim, S. & Davey Smith, G. The association between components of adult height and Type II diabetes and insulin resistance: British Women’s Heart and Health Study. Diabetologia. 45, 1097–106 (2002).
Roseboom, T. J., de Rooij, S. & Painter, R. The Dutch famine and its long-term consequences for adult health. Early Hum Develop. 82, 485–91 (2006).
van Abeelen, A. F. et al. Famine exposure in the young and the risk of type 2 diabetes in adulthood. Diabetes. 61, 2255–60 (2012).
Said-Mohamed, R. et al. Rural-urban variations in age at menarche, adult height, leg-length and abdominal adiposity in black South African women in transitioning South Africa. Ann Hum Biol. 45, 123–32 (2018).
Weitzman, S., Wang, C. H., Pankow, J. S., Schmidt, M. I. & Brancati, F. L. Are measures of height and leg length related to incident diabetes mellitus? The ARIC (Atherosclerosis Risk in Communities) study. Acta Diabetol. 47, 237–42 (2010).
Barker, D. J. & Martyn, C. N. The maternal and fetal origins of cardiovascular disease. J Epidemiol Community Health. 46, 8–11 (1992).
Agyemang, C. et al. Rationale and cross-sectional study design of the Research on Obesity and type 2 Diabetes among African Migrants: the RODAM study. BMJ Open. 4, e004877 (2015).
Wadsworth, M. E., Hardy, R. J., Paul, A. A., Marshall, S. F. & Cole, T. J. Leg and trunk length at 43 years in relation to childhood health, diet and family circumstances; evidence from the 1946 national birth cohort. Int J Epidemiol. 31, 383–90 (2002).
Bogin, B. & Varela-Silva, M. I. Leg length, body proportion, and health: a review with a note on beauty. Int J Environ Res Public Health. 7, 1047–75 (2010).
Hayati Rezvan, P., Lee, K. J. & Simpson, J. A. The rise of multiple imputation: a review of the reporting and implementation of the method in medical research. BMC Med Res Methodol. 15, 30 (2015).
Cole, J. & Groes, C. Affective Circuits: African Migrations to Europe and the Pursuit of Social Regeneration. (University of Chicago Press, 2016).
Karastergiou, K., Smith, S. R., Greenberg, A. S. & Fried, S. K. Sex differences in human adipose tissues – the biology of pear shape. Biol Sex Diff. 3, 13 (2012).
Addo, J. et al. Association between socioeconomic position and the prevalence of type 2 diabetes in Ghanaians in different geographic locations: the RODAM study. J Epidemiol Community Health. 71, 633–9 (2017).
Johnston, L. W. et al. Short leg length, a marker of early childhood deprivation, is associated with metabolic disorders underlying type 2 diabetes: the PROMISE cohort study. Diabetes Care. 36, 3599–606 (2013).
Cohen, S., Janicki-Deverts, D., Chen, E. & Matthews, K. A. Childhood socioeconomic status and adult health. Ann N Y Acad Sci. 1186, 37–55 (2010).
Doom, J. R., Mason, S. M., Suglia, S. F. & Clark, C. J. Pathways between childhood/adolescent adversity, adolescent socioeconomic status, and long-term cardiovascular disease risk in young adulthood. Soc Sci Med. 188, 166–75 (2017).
Braddon, F. E., Rodgers, B., Wadsworth, M. E. & Davies, J. M. Onset of obesity in a 36 year birth cohort study. Br Med J (Clin Res Ed). 293, 299–303 (1986).
Strand, B. H. & Kunst, A. Childhood socioeconomic position and cause-specific mortality in early adulthood. Am J Epidemiol. 165, 85–93 (2007).
Galobardes, B., Lynch, J. W. & Davey Smith, G. Childhood socioeconomic circumstances and cause-specific mortality in adulthood: systematic review and interpretation. Epidemiol Rev. 26, 7–21 (2004).
Galobardes, B., Lynch, J. W. & Davey Smith, G. Is the association between childhood socioeconomic circumstances and cause-specific mortality established? Update of a systematic review. J Epidemiol Community Health. 62, 387–90 (2008).
Lawlor, D. A., Sterne, J. A., Tynelius, P., Davey Smith, G. & Rasmussen, F. Association of childhood socioeconomic position with cause-specific mortality in a prospective record linkage study of 1,839,384 individuals. Am J Epidemiol. 164, 907–15 (2006).
Derks, I. P. et al. The association of early life socioeconomic conditions with prediabetes and type 2 diabetes: results from the Maastricht study. Int J Equity Health. 16, 61 (2017).
Agardh, E. E. et al. Socio-economic position at three points in life in association with type 2 diabetes and impaired glucose tolerance in middle-aged Swedish men and women. Int J Epidemiol. 36, 84–92 (2007).
Asao, K. et al. Short stature and the risk of adiposity, insulin resistance, and type 2 diabetes in middle age: the Third National Health and Nutrition Examination Survey (NHANES III), 1988–1994. Diabetes Care. 29, 1632–7 (2006).
Mueller, N. T. & Pereira, M. A. Leg length and type 2 diabetes: what’s the link? Curr Opin Clin Nutr Metab Care. 18, 452–6 (2015).
Mueller, N. T. et al. Relative leg length is associated with type 2 diabetes differently according to pubertal timing: the Brazilian longitudinal study of adult health. Am J Hum Biol. 27, 219–25 (2015).
Schooling, C. M. et al. Height, its components, and cardiovascular risk among older Chinese: a cross-sectional analysis of the Guangzhou Biobank Cohort Study. Am J Public Health. 97, 1834–41 (2007).
Masi, I., Maskey, S., Mussá, F. E. F. & Trambauer, P. A review of droughts on the African continent: a geospatial and long-term perspective. Hydrol Earth Syst Sci. 18, 3635–49 (2014).
World Development Indicators Database. Country profile of Ghana 2018, http://databank.worldbank.org/data/views/reports/reportwidget.aspx?Report_Name=CountryProfile&Id=b450fd57&tbar=y&dd=y&inf=n&zm=n&country=GHA (2018).
Galbete, C. et al. Food consumption, nutrient intake, and dietary patterns in Ghanaian migrants in Europe and their compatriots in Ghana. Food Nutr Res. 61, 1341809 (2017).
Ross, M. G. & Desai, M. Developmental programming of appetite/satiety. Ann Nutr Metab. 64, 36–44 (2014).
Martins, P. A. et al. Stunted children gain less lean body mass and more fat mass than their non-stunted counterparts: a prospective study. Br J Nutr. 92, 819–25 (2004).
Hales, C. N. & Barker, D. J. Type 2 (non-insulin-dependent) diabetes mellitus: the thrifty phenotype hypothesis. Diabetologia. 35, 595–601 (1992).
Hou, W. W., Tse, M. A., Lam, T. H., Leung, G. M. & Schooling, C. M. Adolescent testosterone, muscle mass and glucose metabolism: evidence from the ‘Children of 1997’ birth cohort in Hong Kong. Diabet Med. 32, 505–12 (2015).
Mühlenbruch, K. et al. Multiple imputation was a valid approach to estimate absolute risk from a prediction model based on case–cohort data. J Clin Epidemiol. 84, 130–141 (2017).
Galobardes, B., Shaw, M., Lawlor, D. A., Lynch, J. W. & Davey Smith, G. Indicators of socioeconomic position (part 1). J Epidemiol Community Health. 60, 7–12 (2006).
Acknowledgements
The authors are very grateful to the advisory board members for their valuable support in shaping the methods, to the research assistants, interviewers and other staff of the five research locations who have taken part in gathering the data and, most of all, to the Ghanaian volunteers participating in this project. We thank the AMC Biobank for support in biobank management and storage of collected samples. This work was supported by the European Commission under the Framework Programme (Grant Number: 278901). DB was supported by the Global Health Scholarship Programme, University Medical Center Utrecht, The Netherlands. The publication of this article was funded by the Open Access Fund of the Leibniz Association. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
I.D. and J.A. analyzed the data and drafted the manuscript. I.D., C.A., K.S. and F.P.M. designed the study. D.B., K.K.G., K.M., E.B., C.G., J.S., F.P.M., C.A. and L.S. were responsible for on-site recruitment and data collection. All authors critically contributed to the writing of the manuscript. I.D. is the guarantor of this work.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Danquah, I., Addo, J., Boateng, D. et al. Early-life factors are associated with waist circumference and type 2 diabetes among Ghanaian adults: The RODAM Study. Sci Rep 9, 10848 (2019). https://doi.org/10.1038/s41598-019-47169-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-47169-6
This article is cited by
-
Subgroups of adult-onset diabetes: a data-driven cluster analysis in a Ghanaian population
Scientific Reports (2023)
-
Pathophysiology of type 2 diabetes in sub-Saharan Africans
Diabetologia (2022)
-
Estimating trunk fat in children according to sex using basic somatic readings: an opportunity for improving evaluation among girls
BMC Pediatrics (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.