Abstract
Anaesthesiologists are increasingly involved in nonoperating room anaesthesia (NORA) for fluoroscopic procedures. However, the radiation exposure of medical staff differs among NORA settings. Therefore, we aimed to investigate the radiation environment generated by fluoroscopic endoscopic retrograde cholangiopancreatography (ERCP) and the radiation exposure of anaesthesiologists. The dose area product (DAP), radiation entrance dose (RED), and fluoroscopy time (FT) according to the procedures and monthly cumulative radiation exposure were analysed at two sites (neck and wrist) from 363 procedures in 316 patients performed within 3 months. The total RED and DAP were 43643.1 mGy and 13681.1 Gy cm2, respectively. DAP and RED (r = 0.924) were strongly correlated and DAP and FT (r = 0.701) and RED and FT (r = 0.749) were moderately correlated. The radiation environment per procedure varied widely, DAP and RED per FT were the highest during stent insertion with esophagogastroduodenoscopy. Monthly cumulative deep dose equivalents at the wrist and neck ranged between 0.31–1.27 mSv and 0.33–0.59 mSv, respectively, but they were related to jaw thrust manipulation (r = 0.997, P = 0.047) and not to the radiation environment. The anaesthesiologists may be exposed to high dose of radiation in the ERCP room, which depends on the volume of procedures performed and perhaps the anaesthesiologists’ practice patterns.
Similar content being viewed by others
Introduction
An increasing number of anaesthesiologists are performing sedation during fluoroscopic procedures under nonoperating room anaesthesia (NORA) compared with that in the past1. Among these procedures involving NORA, there is a growing number of radiation-assisted procedures, especially those performed in the endoscopic retrograde cholangiopancreatography (ERCP) room2,3. A previous study reported that the radiation environment differed according to the NORA setting; it was higher for the cardiac catheterisation laboratory than for interventional radiology and higher for monitored sedation than for the general anaesthesia setting4.
Therefore, we aimed to investigate the radiation environment generated by fluoroscopic ERCP procedures and the radiation exposure of anaesthesiologists who are involved in monitored anaesthesia care during their everyday practice.
Methods
Ethics approval
This retrospective study conducted at a tertiary university hospital was approved by the Severance Hospital institutional review board (protocol number: 4–2017–0920). The need to obtain written consent from subjects was waived.
Study population
Three anaesthesiologists were involved in monitored anaesthesia care for 363 procedures in 316 patients performed by 10 endoscopists in the ERCP room over 3 months, between July and September 2017. The procedures took place from 9 AM to 4 PM in monthly shifts. All three anaesthesiologist who were involved in monitored anaesthesia care were senior residents with at least 3 years of anaesthesia experience, and they were supervised by specialist anaesthesiologists.
Conduct of the study
Various procedures were performed under fluoroscopy, such as luminal dilation, stent insertion with esophagogastroduodenoscopy, diagnosis, bile duct dilation and stent, stone removal with endoscopic retrograde cholangiopancreatography, and percutaneous transhepatic choledochoscopic stone removal. The patients were sedated using a standardised protocol of continuous propofol (Fresofol 1% MCT injection, Fresenius Kabi Korea, Seoul, South Korea) infusion with intermittent administration of fentanyl (fentanyl citrate, Hana Pharm Co., Ltd., Seoul, South Korea). Electrocardiography, pulse oximetry (blood oxygen saturation [Spo2]), non-invasive arterial blood pressure, and capnometry using a nasal prong were employed as standard monitoring methods. Oxygen was administered through a nasal prong, with a flow rate of 5 L/min. If oxygen saturation decreased (Spo2 < 90%), the anaesthesiologist reduced the rate of propofol infusion and performed jaw thrust until the patient breathed well. If oxygen saturation was not restored (Spo2 > 90%) after jaw thrust, a nasopharyngeal airway was inserted.
The anaesthesiologist wore a lead apron and thyroid shield for personal protection. The usual distance between the wrist of the anaesthesiologist and the central beam of the X-ray system ranged between 80 and 120 cm unless airway manipulation was required. When airway manipulation was required, the distance was reduced to between 40 and 60 cm. Thermoluminescent dosimeters (UD-802, Panasonic Communications Kyushu Co., Ltd., Ueda Usa, Oita, Japan) were used to measure the cumulative radiation exposure of the anaesthesiologists at the neck outside the thyroid shield and the dominant wrist4. These thermoluminescent badges use the tissue equivalent (Li2B4O7:Cu) and are highly sensitive (CaSO4:Tm), making it possible to precisely measure various types of radiation over a wide range of doses (10 μSv–10 Sv). A dedicated reader (UD-716, Panasonic Communications Kyushu Co., Ltd.) obtains the measurements used to determine the deep dose equivalent, Hp(10) mSv5.
Data collection and handling
During fluoroscopic procedures, radiation entrance dose (mGy), fluoroscopic time (s), and dose area product (Gy cm2) were automatically recorded by the fluoroscopy unit of the overcoach ceiling mounted system (Artis Zee Multi-Purpose, Siemens, München, Germany). The demographic data of patients, the types of procedures, and the radiation entrance dose, fluoroscopic time, and dose area product per procedure were retrospectively collected from electronic medical records.
Statistical analysis
Data for the radiation environment are expressed as mean (standard deviation), median (interquartile range), or number of patients (%). Parametric data were analysed using one-way analysis of variance, whereas nonparametric data were analysed using the Kruskal-Wallis test. Categorical variables were evaluated using the chi-squared test or Fisher’s exact test, as appropriate. Correlation analysis between the radiation exposure of the anaesthesiologists (the deep dose equivalent) and radiation environment of the endoscopic retrograde cholangiopancreatography room or other variables was performed using the Pearson or Spearman methods. A P value < 0.05 was considered statistically significant. All analyses were performed using R version 3.4.1 (R Foundation for Statistical Computing, Vienna, Austria) and SPSS 23.0 (IBM, Armonk, NY, USA).
Results
The total radiation entrance dose and dose area product of the radiation environment for the 3 months were 43643.1 mGy and 13681.1 Gy cm2, respectively. The fluoroscopy unit generated x-ray at 66–74 kV during the procedures. The most commonly performed procedure was bile duct dilation and stent insertion with endoscopic retrograde cholangiopancreatography, which accounted for 33% of all procedures. The radiation environments differed widely according to the type of procedure (Table 1). In detail, the median anaesthesia time (35 min), radiation entrance dose (107.6 mGy), fluoroscopic time (343 s), and dose area product (35.0 Gy cm2) were the highest for percutaneous transhepatic choledochoscopic stone removal. However, the radiation entrance dose per fluoroscopic time (0.59 mGy sec−1) and dose area product per fluoroscopic time (0.26 Gy cm2 sec−1) were the highest for stent insertion with esophagogastroduodenoscopy. In the correlation analysis among variables of the radiation environment, there was a strong correlation between the dose area product and radiation entrance dose (r = 0.924), but a weaker one between the dose area product and fluoroscopic time (r = 0.701) or the radiation entrance dose and fluoroscopic time (r = 0.749) (P < 0.001).
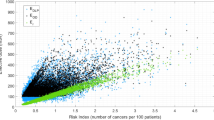
The age, height, and weight of the patients managed by the anaesthesiologists were similar across the 3 months. The number of patients with history of snoring and the fentanyl dose administered were highest in the first month. The first anaesthesiologist cared for the patients more often than the others by performing jaw thrust or nasopharyngeal airway insertion due to oxygen desaturation events (Table 2). Regarding the radiation environment for the anaesthesiologists, the cumulative dose area product, radiation entrance dose, and cumulative fluoroscopy time were in the order of the third, second, and first anaesthesiologist (Table 3). However, the personal dosimeter readings for the neck and wrist of the anaesthesiologists were not related to the cumulative radiation entrance dose and dose area product (Fig. 1). The highest radiation exposure of the neck was 0.59 mSv in the second anaesthesiologist and the highest radiation exposure of the wrist was 1.27 mSv in the first anaesthesiologist. The coefficient of correlation between radiation exposure of the wrists of the anaesthesiologists and jaw thrust manipulation was 0.997 (P = 0.047).
Total radiation entrance dose (RED) and dose area product (DAP) for the radiation exposure of each anaesthesiologist, and the effective radiation dose (neck and wrist) for each anaesthesiologist. The deep dose equivalents for the anaesthesiologists’ neck and wrist were not associated with the radiation environment variables such as total RED and DAP.
Discussion
In this study, we investigated the radiation environment generated by fluoroscopic ERCP procedures and the radiation exposure of anaesthesiologists who were involved in monitored anaesthesia care setting.
For the radiation environment generated during fluoroscopy, dose area product, fluoroscopy time, and radiation entrance dose are commonly-used indicators of the radiation exposure of the patient. The radiation entering the patient, dose area product, is correlated with the radiation exposure of the medical staff and used as an indirect measure of the occupational dose they receive because the largest source of occupational radiation exposure for the medical staff is the scattered radiation from the patient6,7,8. However, it is unlikely that these parameters can be used for monitoring radiation exposure of anaesthesiologists working in the ERCP room. Although our results were obtained from a single institution, the radiation environment of each procedure differed significantly according to the types of procedures and the anaesthesiologists were working in environments with high risk of radiation exposure. None of the variables of the radiation environment fit the normal distribution curve, which implies that it is difficult to predict the radiation dose based only on the type of procedure. While percutaneous transhepatic choledochoscopic stone removal required the longest fluoroscopic time and produced the largest dose area product and radiation entrance dose, the dose area product and radiation entrance dose per fluoroscopic time were the largest during stent insertion with esophagogastroduodenoscopy. The total radiation dose of the radiation environment might be affected by multiple factors unmanageable by the anaesthesiologist, which has also been shown by other studies2,9. Nevertheless, there was a correlation between fluoroscopic time and the dose area product for endoscopic retrograde cholangiopancreatography procedures in our study, as also observed in other studies2. Although Ismail et al. revealed that the radiation exposure of anaesthesiologists in the endoscopic retrograde cholangiopancreatography suite was lower than that in the cardiac catheterisation laboratory, anaesthesiologists are still exposed to a considerable amount of radiation in the ERCP room4.
Regarding the radiation exposure of anaesthesiologists in the ERCP room, we made some interesting observations. First, the radiation exposure of the anaesthesiologists was not related to the radiation environment of procedures performed in the endoscopic retrograde cholangiopancreatography room. Although the dose area product and radiation entrance dose increased in the order of the first to the third anaesthesiologist, the deep dose equivalent at the neck and wrist were the highest in the second and first anaesthesiologist, respectively. This could imply that the radiation exposure of anaesthesiologists may not be influenced by the radiation environment of the ERCP procedure because we could not find any correlation between anaesthesiologists’ radiation exposure and the radiation entrance dose or dose area product. We obtained some indication as to the reason for this from the requirement for airway manipulation for the anaesthesiologist. The first anaesthesiologist performed jaw thrust and nasopharyngeal airway insertion more often than did the others. This was confirmed by the strong correlation (r = 0.997, P = 0.047) between radiation exposure and the wrists of the anaesthesiologists. Similarly, the total number of drug boli and infusion rate changes by the anaesthesiologist was significantly related to the radiation exposure of the anaesthesiologist in other study10. However, these events were not associated with radiation exposure of the neck. Then, we inquired as to why the radiation dose measured at the necks of the anaesthesiologists did not show a pattern similar to that for the incidence of airway manipulation. This could be explained by the fact that the radiation intensity is inversely proportional to the square of distance from the source of scattered radiation (in this case, the patient).
Second, the radiation exposure of anaesthesiologists during their everyday practice did not exceed the annual radiation dose recommended by the International Commission on Radiological Protection11,12,13. However, it is important for anaesthesiologists to be aware that their radiation exposure is related to the patients’ responses to sedation methods. It is worthwhile to refine the sedation protocol used during nonoperating room anaesthesia to avoid the respiratory depression of patients, especially in the ERCP room14,15. We also recommend that anaesthesiologists should stand as far as possible from the sources of scattered radiation.
Third, in our institution, the design and working of the ERCP room was not influenced by consideration of the anaesthesiologists’ perspective. The dosimeter at our institution is only for regular staff and not for anaesthesiologists, who work in monthly shifts. However, when anaesthesiologists are requested to participate in procedures related to fluoroscopy, they must monitor their radiation exposure and wear protective shielding because the monthly radiation exposure dose is not constant10. The lead apron covers almost all active bone marrow and major organs, such as the heart, lungs, and major vessels3. The thyroid shield protects the thyroid gland and the oesophagus, vertebrae, and bone marrow12. Anaesthesiologists should wear the radiation protection equipment, including the lead apron and thyroid collar, because it protects the most radiation-sensitive areas. The lens of the eye is vulnerable to radiation and cannot be covered by routine equipment16,17,18. Protection glasses are recommended especially when the anaesthesiologists stand near the patient, regardless of the number of ERCP procedures performed10,12,19.
Similar to our study, Ismail et al. also reported on the radiation exposure of anaesthesiologists during ERCP; the net radiation exposure of the neck was 0.25 mSv during 39 ERCP procedures (0.0064 mSv per procedure) performed over 6 months4 compared with 1.36 mSv during 363 procedures (0.0037 mSv per procedure) performed over 3 months in our study. This difference could be attributable to many factors influencing the radiation environment, such as the volume of the procedures as well as the anaesthesiologists’ practice pattern. We believe that there is a need for a guideline suggested by anaesthesiologists’ societies, such as the ones suggested by cardiologists’ societies20. For instance, considering that the radiation tolerance limit of pregnant women is 1 mSv after the pregnancy is declared, as suggested by the International Commission on Radiological Protection, the participation of a pregnant anaesthesiologist in the ERCP room should be limited3,13.
There are several limitations to our study. First, since this study was conducted at a single institute, our results may not be applicable to other institutes. Although the radiation environment related to the fluoroscopic procedure depends on many factors and the conditions differ across medical institutions, our data would be clinically meaningful considering that the radiation dose generated by each procedure was reviewed in a total of 363 cases. Second, we only measured the cumulative radiation exposure dose of anaesthesiologists over 3 months. Thus, it is difficult to identify factors affecting the radiation exposure of the anaesthesiologist. We believe that well-designed prospective studies monitoring the real-time radiation exposure of anaesthesiologists could identify the factors that influence the effective radiation dose of anaesthesiologists during fluoroscopic procedures21.
In conclusion, anaesthesiologists may be exposed to high risk of radiation exposure in ERCP room, which depends on the volume of performed procedures and perhaps the anaesthesiologists’ practice patterns. Therefore, the procedural parameters and the working environment of anaesthesiologists in fluoroscopic NORA settings must be considered to reduce radiation exposure, especially in high-volume centres, such as working in shifts, wearing protective equipment, dosimeter-based monitoring, and refining the sedation protocol. A future prospective study using real-time radiation dose monitoring is anticipated.
Data Availability
The data that support the findings of this study are available from the corresponding author on reasonable request.
References
Boggs, S. D., Barnett, S. R. & Urman, R. D. The future of nonoperating room anesthesia in the 21st century: emphasis on quality and safety. Current opinion in anaesthesiology 30, 644–651, https://doi.org/10.1097/aco.0000000000000528 (2017).
Saukko, E., Gronroos, J. M., Salminen, P., Henner, A. & Nieminen, M. T. Patient radiation dose and fluoroscopy time during ERCP: a single-center, retrospective study of influencing factors. Scandinavian journal of gastroenterology 53, 495–504, https://doi.org/10.1080/00365521.2018.1445774 (2018).
Wang, R. R., Kumar, A. H., Tanaka, P. & Macario, A. Occupational Radiation Exposure of Anesthesia Providers: A Summary of Key Learning Points and Resident-Led Radiation Safety Projects. Seminars in cardiothoracic and vascular anesthesia 21, 165–171, https://doi.org/10.1177/1089253217692110 (2017).
Ismail, S., Khan, F., Sultan, N. & Naqvi, M. Radiation exposure to anaesthetists during interventional radiology. Anaesthesia 65, 54–60, https://doi.org/10.1111/j.1365-2044.2009.06166.x (2010).
Matsubara, K. et al. Eye lens dosimetry and the study on radiation cataract in interventional cardiologists. Physica medica: PM: an international journal devoted to the applications of physics to medicine and biology: official journal of the Italian Association of Biomedical Physics (AIFB) 44, 232–235, https://doi.org/10.1016/j.ejmp.2017.10.007 (2017).
Miller, D. L. et al. Quality improvement guidelines for recording patient radiation dose in the medical record for fluoroscopically guided procedures. Journal of vascular and interventional radiology: JVIR 23, 11–18, https://doi.org/10.1016/j.jvir.2011.09.004 (2012).
Servomaa, A. & Karppinen, J. The dose-area product and assessment of the occupational dose in interventional radiology. Radiation protection dosimetry 96, 235–236 (2001).
Vano, E., Gonzalez, L., Guibelalde, E., Fernandez, J. M. & Ten, J. I. Radiation exposure to medical staff in interventional and cardiac radiology. The British journal of radiology 71, 954–960, https://doi.org/10.1259/bjr.71.849.10195011 (1998).
Kim, E. et al. Retrospective analysis of radiation exposure during endoscopic retrograde cholagiopancreatography: critical determinants. Canadian journal of gastroenterology = Journal canadien de gastroenterologie 25, 555–559 (2011).
Anastasian, Z. H., Strozyk, D., Meyers, P. M., Wang, S. & Berman, M. F. Radiation exposure of the anesthesiologist in the neurointerventional suite. Anesthesiology 114, 512–520, https://doi.org/10.1097/ALN.0b013e31820c2b81 (2011).
Dumonceau, J. M. et al. Radiation protection in digestive endoscopy: European Society of Digestive Endoscopy (ESGE) guideline. Endoscopy 44, 408–421, https://doi.org/10.1055/s-0031-1291791 (2012).
Stewart, F. A. et al. ICRP publication 118: ICRP statement on tissue reactions and early and late effects of radiation in normal tissues and organs–threshold doses for tissue reactions in a radiation protection context. Annals of the ICRP 41, 1–322, https://doi.org/10.1016/j.icrp.2012.02.001 (2012).
The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Annals of the ICRP 37, 1–332, https://doi.org/10.1016/j.icrp.2007.10.003 (2007).
Yoo, Y. C. et al. A comparison of sedation protocols for gastric endoscopic submucosal dissection: moderate sedation with analgesic supplementation vs analgesia targeted light sedation. British journal of anaesthesia 115, 84–88, https://doi.org/10.1093/bja/aeu555 (2015).
Kim, N. et al. Comparison of the efficacy and safety of sedation between dexmedetomidine-remifentanil and propofol-remifentanil during endoscopic submucosal dissection. World journal of gastroenterology 21, 3671–3678, https://doi.org/10.3748/wjg.v21.i12.3671 (2015).
Ainsbury, E. A. et al. Radiation cataractogenesis: a review of recent studies. Radiation research 172, 1–9, https://doi.org/10.1667/rr1688.1 (2009).
Zagorska, A., Romanova, K., Hristova-Popova, J., Vassileva, J. & Katzarov, K. Eye lens exposure to medical staff during endoscopic retrograde cholangiopancreatography. Physica medica: PM: an international journal devoted to the applications of physics to medicine and biology: official journal of the Italian Association of Biomedical Physics (AIFB) 31, 781–784, https://doi.org/10.1016/j.ejmp.2015.03.011 (2015).
O’Connor, U., Gallagher, A., Malone, L. & O’Reilly, G. Occupational radiation dose to eyes from endoscopic retrograde cholangiopancreatography procedures in light of the revised eye lens dose limit from the International Commission on Radiological Protection. The British journal of radiology 86, 20120289, https://doi.org/10.1259/bjr.20120289 (2013).
Amis, E. S. Jr. Anesthesiologists in the neurointerventional suite: what is appropriate radiation protection? Anesthesiology 114, 477–478, https://doi.org/10.1097/ALN.0b013e31820c299d (2011).
Duran, A. et al. Recommendations for occupational radiation protection in interventional cardiology. Catheterization and cardiovascular interventions: official journal of the Society for Cardiac Angiography & Interventions 82, 29–42, https://doi.org/10.1002/ccd.24694 (2013).
Baumann, F. et al. The Effect of Realtime Monitoring on Dose Exposure to Staff Within an Interventional Radiology Setting. Cardiovascular and interventional radiology 38, 1105–1111, https://doi.org/10.1007/s00270-015-1075-6 (2015).
Author information
Authors and Affiliations
Contributions
B.L. Data collection and analysis and preparation of the first draft of the manuscript. M.-S.K. Manuscript revision. D.E. Data collection. K.T.M. Study design and preparation of the final draft of the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, B., Kim, MS., Eum, D. et al. The radiation environment of anaesthesiologists in the endoscopic retrograde cholangiopancreatography room. Sci Rep 9, 9124 (2019). https://doi.org/10.1038/s41598-019-45610-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-45610-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.