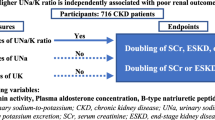
Abstract
Dietary salt restriction is essential for managing fluid retention in patients with chronic kidney disease (CKD). In this retrospective cohort study, we investigated weight loss from the perspective of fluid status in CKD patients during a 7-day hospitalization period while consuming a low-salt diet (5 g/day). Among 311 patients, the median weight loss (interquartile range, maximum) was 0.7 (0.0–1.4, 4.7) kg on Day 4 and 1.0 (0.3–1.7, 5.9) kg on Day 7. Patients were classified into quartiles based on pre-hospital urinary salt excretion (quartile [Q] 1, 1.2–5.7; Q2, 5.8–8.4; Q3, 8.5–11.3; Q4, 11.4–29.2 g/day). Weight loss was significantly greater in Q3 and Q4 than in Q1. The body mass index (BMI) and urinary salt excretion in the first 24 hours after admission were independently associated with rapid weight loss on Day 4 by multivariate logistic regression analysis. In conclusion, CKD patients with a high salt intake or high BMI exhibit rapid weight loss within a few days of consuming a low-salt diet. Dietary salt restriction is effective for reducing proteinuria in these patients, but long-term observation is needed to confirm the sustained effects.
Similar content being viewed by others
Introduction
Chronic kidney disease (CKD) can cause fluid retention, mainly due to reduced glomerular filtration of sodium and activation of the renin-angiotensin system. Many patients with stage 3–5 CKD present fluid retention, which may lead to a higher cardiovascular risk via several pathways1,2,3,4. First, fluid retention is related to hypertension in CKD patients and salt sensitivity of blood pressure increases with decreasing kidney function5. Hypertension associated with fluid retention in CKD patients often requires multiple medications6. Second, fluid retention causes endothelial oxidative stress and release of inflammatory mediators, which have been demonstrated to increase the cardiovascular risk7. In order to control fluid retention, salt restriction is essential. Therefore, the Japanese Society of Nephrology recommends restricting the salt intake to <6 g/day for CKD patients8, whereas the Kidney Diseases Improving Global Outcomes (KDIGO) guidelines recommend <5 g/day9.
In clinical settings, CKD patients with apparent fluid retention frequently experience rapid weight loss within a few days of consuming a low-salt diet during hospitalization. This decrease in body weight has been considered to occur due to reduced fluid retention. In the 1950’s, Strauss et al. reported that when salt intake was abruptly changed in healthy subjects, it took 3–4 days until a new steady state in which renal sodium excretion matched intake was achieved, and thus a negative salt balance contributed to weight loss10,11,12. Some clinical studies have reported weight loss within several weeks after dietary salt restriction13,14,15,16, whereas others did not observe significant weight loss with a longer observational period17,18. However, limited information is currently available on weight loss immediately after dietary salt restriction in CKD patients.
Therefore, we investigated the short-term effects of dietary salt restriction on weight loss from the perspective of fluid status in CKD patients. We also performed a multivariate logistic regression analysis to identify the factors related to rapid weight loss in response to dietary salt restriction.
Results
Participant characteristics
During the study period, 461 patients were assessed for eligibility. Of these, we excluded 115 patients who were missing data for body weight during hospitalization, 30 patients missing data for 24-hour urinary salt excretion, and 5 patients missing data for 24-hour proteinuria before or during hospitalization. As a result, 311 patients were included in the study. The clinical characteristics of study participants are listed in Table 1. The median age was 69 years, 74.3% were men, 47.9% had diabetes, and the median estimated glomerular filtration rate (eGFR) was 31.0 ml/min per 1.73 m2. The median pre-hospital 24-hour proteinuria was 0.50 g/day.
Weight loss after admission
Patients were classified into quartiles based on pre-hospital urinary salt excretion (quartile [Q] 1, 1.2–5.7; Q2, 5.8–8.4; Q3, 8.5–11.3; and Q4, 11.4–29.2 g/day). Weight loss after admission was significantly greater in the high urinary salt excretion groups (Q3 and Q4) than in Q1 by one-way analysis of variance (ANOVA) with post-hoc Tukey’s honestly significant difference (HSD) tests (P = 0.012 and 0.015 respectively; Fig. 1). The weight loss on Day 4 and Day 7 by quartiles of pre-hospital urinary salt excretion is shown in Table 2. Among all subjects, the median weight loss (interquartile range, maximum) was 0.7 (0.0–1.4, 4.7) kg on Day 4 and 1.0 (0.3–1.7, 5.9) kg on Day 7. Weight loss on Day 4 was significantly greater in the high urinary salt excretion groups (Q3 and Q4) than in Q1 by Dunnett’s multiple comparison test (P = 0.018 and 0.004, respectively).
Urinary salt excretion and serum sodium levels after admission
The 24-hour urinary salt excretion in all quartiles markedly decreased within 48 hours after admission (Fig. 2a). The urinary salt excretion before, and in the first and second 24 hours after admission is shown in Fig. 2b. By consuming low-salt meals (5 g/day), the urinary salt excretion in all quartiles became less than 6 g/day after admission. However, 34.1% of patients in Q4 still had a urinary salt excretion of 6 g/day or more in the second 24 hours after admission, whereas only 4.2% in Q1 did (Table 3).
Changes in 24-hour urinary salt excretion after admission by quartiles of pre-hospital urinary salt excretion. (a) The 24-hour urinary salt excretion in all quartiles markedly decreased within 48 hours after admission. (b) Urinary salt excretion in all quartiles decreased to less than 6 g/day after admission. The dotted line indicates urinary salt excretion of 6 g/day. Abbreviations: Q, quartile.
Although serum sodium levels decreased significantly during hospitalization, they remained within the normal range for almost all participants (Table 4). The difference in serum sodium levels between Day 2 and Day 6 was not significant in Q2 to Q4 as compared with that in Q1.
Factors associated with rapid weight loss
To investigate factors associated with weight loss of 1 kg or more on Day 4, we conducted a multivariate logistic regression analysis (Table 5). In Model 1, which was adjusted for age and sex, body mass index (BMI) and urinary salt excretion in the first 24 hours were independently associated with rapid weight loss (adjusted odds ratio [OR], 1.11; 95% confidence interval [CI], 1.05–1.18 and adjusted OR, 1.15; 95% CI, 1.05–1.26, respectively). These factors remained significant even after adjustment for other factors: diuretic use, diabetes, proteinuria before admission, 24-hour systolic blood pressure, serum albumin, and serum creatinine (Model 2 and Model 3).
Decreases in proteinuria after admission
Decreases in proteinuria after admission, which were the secondary outcome, were compared among quartiles using Q1 as a reference group. Proteinuria decreased after admission significantly in Q2 to Q4 compared with in Q1 (Fig. 3).
Urinary salt excretion and proteinuria after discharge
Lastly, changes in 24-hour urinary salt excretion and proteinuria after discharge were examined in a subset of 263 patients with 24-hour urine samples after discharge. The urinary salt excretion in the second 24 hours after admission and 3 months after discharge is shown in Supplementary Fig. S1. In all quartiles, only 20.2% exhibited urinary salt excretion of 6 g/day or more in the second 24 hours, but this percentage increased to 58.6% at 3 months after discharge (Supplementary Table S1). Increases in proteinuria after discharge were significantly higher in patients with urinary salt excretion of 6 g/day or more at 3 months after discharge (Supplementary Fig. S2).
Discussion
This retrospective cohort study provided three important findings by investigating weight loss and decreases in proteinuria in CKD patients within 7 days of consuming a low-salt diet. First, many CKD patients exhibited rapid weight loss within a few days of consuming a low-salt diet during hospitalization. Second, weight loss with dietary salt restriction may be greater in CKD patients with a higher salt intake or higher BMI. Third, proteinuria can be decreased by dietary salt restriction in CKD patients with a high salt intake. These results were obtained using a population of CKD patients who participated in an in-hospital education program in Japan. In-hospital CKD education programs have been widely established under the public health insurance system in Japan, although the Ministry of Health recommends reducing the length of hospital stay. Each program consists of diet therapy, lectures on kidney disease, including renal replacement therapy options, and cardiovascular evaluation. Previous reports have examined the benefits of education programs19,20,21,22, but the purpose of our study was not to confirm their effects. Our subjects were selected because they underwent rapid changes in diet without additional medications, such as diuretics, which may affect weight loss. Therefore, the findings of this study can be applied to CKD patients hospitalized for any disease.
First, many CKD patients exhibited rapid weight loss within a few days of consuming a low-salt diet during hospitalization. Hung et al. reported that 52% of patients with stage 3–5 CKD have fluid retention as assessed by bioelectrical impedance analysis (BIA)1. Fluid retention is a major cause of hypertension in CKD patients and almost all CKD patients have hypertension at the beginning of dialysis. A previous study of pre-dialysis CKD patients with a mean eGFR of 14.5 ml/min per 1.73 m2 reported the prevalence of hypertension to be 95%23. Furthermore, uncontrolled 24-hour blood pressure is a risk factor for both end-stage renal disease (ESRD) and cardiovascular disease24. We did not evaluate changes in body fluid status with dietary salt restriction by specific methods like BIA, but as remarkable weight loss occurred within a few days after admission, the weight loss likely reflected reduced fluid retention more than a decrease in muscle or fat mass. A significant decrease in serum sodium levels during hospitalization, although clinically minor, suggested that a decrease in fluid volume occurred.
In this study, CKD patients with higher urinary salt excretion before admission demonstrated significant weight loss within a few days. In addition, these patients excreted more salt than they ingested even in the second 24 hours after admission. Vogt et al. reported that weight loss was significantly greater with a low-sodium diet (50 mmol/day) than with a high-sodium diet (200 mmol/day) in 6 weeks13. Similarly, Krinkken et al. reported that in normotensive healthy subjects, significant weight loss was observed with a low-salt diet (50 mmol/day) compared with a high-salt diet (200 mmol/day) in 7 days16. In contrast, de Brito-Ashurst et al. randomly provided a tailored low-salt diet or standard low-salt advice to hypertensive CKD patients and compared outcomes after 6 months. Compared with the standard low-salt advice, the tailored diet significantly reduced urinary sodium excretion (260 mmol/day to 103 mmol/day) and mean total body water (0.50 L), as assessed by BIA, but significant weight loss was not observed in either group18. In a meta-analysis including studies of varying periods from 2 weeks to 6 months, the authors were unable to conclude whether weight loss resulted from changes in body fluid status or fat mass because many studies did not describe changes in body fluid status or energy intake17. As we examined weight loss in a shorter period than that in those previous reports, we considered the weight loss within a few days to reflect body fluid reduction more than a decrease in fat or muscle mass.
Second, weight loss with dietary salt restriction may be greater in CKD patients with a higher salt intake or higher BMI. As approximately 90% of ingested salt is excreted in the urine25,26, it is useful to measure urinary salt excretion to estimate the daily salt intake27. In this study, urinary salt excretion in the first 24 hours after admission was independently associated with rapid weight loss immediately after dietary salt restriction. Evaluation of urinary salt excretion in the first 24 hours after admission can predict patients who are likely to lose weight due to abrupt dietary salt restriction. In addition, BMI was also independently associated with rapid weight loss due to dietary salt restriction in this study. Patients with abdominal obesity have an enhanced rate of tubular sodium reabsorption28. Moreover, higher BMI was reported to be associated with fluid retention during high salt intake in 78 healthy subjects29. Therefore, in the management of CKD patients admitted to the hospital, we can predict rapid weight loss within a few days based on high urinary salt excretion or high BMI.
Third, proteinuria can be decreased by dietary salt restriction in CKD patients with a high salt intake. In 95 healthy normotensive subjects, dietary salt restriction decreased urinary albumin excretion to within the normal range independent of blood pressure30. The same result was also reported for 34 CKD patients with a mean baseline proteinuria of 3.8 g/day13. Proteinuria is an independent risk factor for ESRD31 or all-cause and cardiovascular mortality32. Dietary salt restriction not only decreases blood pressure (BP), but also improves the antiproteinuric response to renin-angiotensin system inhibitors33,34,35. Furthermore, dietary salt restriction improves arterial stiffness and left ventricular diastolic function2,4. Thus, it is important to recommend dietary salt restriction for CKD patients with a high salt intake. Long-term prospective studies are required to clarify if continuation of dietary salt restriction leads to the sustained reduction of proteinuria.
There are some limitations in this study. First, as the timing of pre-hospital urine collection ranged from several weeks to several months before admission depending on the visit frequency, the pre-hospital urinary salt excretion did not reflect the salt intake just before admission. Urinary salt excretion in hypertensive patients is reported to increase in winter compared with that in summer36. Considering seasonal variations in dietary habits and physical activity, analysis using urine samples just before admission may be more ideal. As it is difficult to perform 24-hour urine collection at home in all cases, urine collection in the first 24 hours after admission may be practically useful. Second, our study lacked specific markers for fluid status such as brain natriuretic peptide (BNP) and BIA. BNP can reflect changes in body fluid status, but it is influenced by left ventricular abnormalities and accumulates in CKD patients37. Although it has been reported that fluid assessment by BIA is useful for CKD patients1,38, its utility has not been established. Even without using these expensive markers, short-term changes in body fluid status can be easily detected by daily measurement of body weight in clinical practice. Third, diuretics were discontinued in a few patients during hospitalization by decision of the attending physicians, but no patients started diuretics. Their impact on the results were considered to be limited because there was no significant difference in diuretic use or discontinuation among the quartiles of pre-hospital urinary salt excretion. Lastly, the study has the inherent limitations of a retrospective cohort study. Future randomized controlled trials comparing abrupt salt restriction with gradual salt restriction are needed for further investigation.
In conclusion, CKD patients with a high salt intake or high BMI exhibit rapid weight loss within a few days of consuming a low-salt diet during hospitalization. Dietary salt restriction is effective for reducing proteinuria in these patients, but long-term observation is needed to confirm the sustained effects.
Methods
Study design and participants
In this retrospective cohort study, we investigated weight loss in CKD patients during a 7-day hospitalization period while consuming a low-salt diet and clarified factors associated with rapid weight loss. We identified consecutive patients who participated in an in-hospital CKD education program between January 2012 and December 2014 at Omihachiman Community Medical Center, a tertiary care general hospital in Japan. We excluded patients who were missing data for body weight during hospitalization, or 24-hour urine samples before or during hospitalization. Patients with diseases unsuitable for dietary salt restriction, such as salt-wasting nephropathy or anorexia, were also excluded. The education program consisted of multidisciplinary patient education and cardiovascular evaluation for patients (Supplementary Fig. S3). During the 7-day hospitalization period, we served food that was low in salt (5 g/day) and protein (0.6–1.0 g/kg/day × ideal body weight based on individual CKD stages) according to the guidelines of the Japanese Society of Nephrology. Patients were permitted to stay out overnight from Day 4 to Day 5 to confirm nutritional therapy adherence.
This study was approved by the Ethics Committee on Human Research of Omihachiman Community Medical Center and was carried out in accordance with the Declaration of Helsinki. The requirement for informed consent was waived because of the retrospective design. Patient records/information were anonymized and de-identified prior to analysis.
Outcomes and follow-up
The primary outcome was weight loss after admission. Body weight was measured immediately after admission and every morning from Day 2 to Day 7. Weight loss (kg) was calculated as the difference between body weight on each day from Day 2 to Day 7 and that on admission.
Secondary outcomes included changes in 24-hour urinary salt excretion and proteinuria after admission. Twenty-four-hour urine collection was conducted at the outpatient visit before admission and during the first and second 24 hours after admission (Supplementary Fig. S3). We evaluated the 24-hour urinary salt excretion before admission and in the first and second 24 hours after admission. The 24-hour urinary salt excretion (g/day) was calculated as the 24-hour urinary sodium excretion (mEq/day) divided by 17. We measured serum sodium levels on Day 2 and Day 6. Decreases in proteinuria were calculated as the difference in values between before admission and at the second 24 hours after admission.
In addition, 24-hour urinary salt excretion and proteinuria after discharge were assessed in a subset of patients who had 24-hour urine samples 3 months after discharge. Increases in proteinuria were calculated between the second 24 hours after admission and 3 months after discharge.
Baseline assessment
Baseline characteristics of patients were extracted from electronic medical records as follows: age, sex, history of diabetes, and diuretic use. BMI was calculated as body weight (kg) divided by the height squared (m2). We collected baseline blood samples, and measured serum creatinine, serum albumin, and hemoglobin on Day 2. We used the following formula for Japanese patients with CKD to calculate the eGFR by gender: eGFR (ml/min per 1.73 m2) = 194 × serum creatinine−1.094 × age−0.287 (×0.739 if female)39. Patients wore a 24-hour ambulatory BP monitor (FB-270; Fukuda Denshi Co., Ltd., Tokyo, Japan) from Day 1 to Day 2. Ambulatory BP values were recorded every 30 minutes from 6:00 a.m. to 10:00 p.m. and every 60 minutes from 10:00 p.m. to 6:00 a.m., and the average was calculated as the 24-hour systolic and diastolic BP.
Statistical analysis
Data are shown as numbers (percentage) for categorical variables and the median (interquartile range) for continuous variables. Patients were classified into quartiles based on pre-hospital urinary salt excretion. Weight loss after admission was compared among the groups by one-way ANOVA with post-hoc Tukey’s HSD tests. We compared weight loss among the groups on Day 4 and Day 7 by Dunnett’s multiple comparison test using the smallest quartile as a reference group. We compared the urinary salt excretion before and after admission in each group, and evaluated the proportion of patients with urinary salt excretion of 6 g/day or more in the first and second 24 hours after admission. We compared serum sodium levels on Day 2 and Day 6 using the Wilcoxon signed-rank test. We compared the difference in serum sodium levels between Day 2 and Day 6 by Dunnett’s multiple comparison test using the smallest quartile as a reference group.
We conducted a multivariate logistic regression analysis to clarify the effects of BMI and urinary salt excretion on weight loss in response to dietary salt restriction. In order to minimize the effects of changes in muscle and fat mass, and to more precisely evaluate changes in fluid status, we analyzed weight loss of 1 kg or more on Day 4. We also considered the subjects who stayed out overnight from Day 4 to Day 5. We used three logistic regression models because the model should be evaluated by several combinations of confounders for the sensitivity analysis. Model 1 was adjusted for age and sex, and Model 2 was adjusted for variables in Model 1 plus diuretic use, diabetes, and proteinuria before admission. Model 3 was adjusted for variables in Model 2 plus 24-hour systolic blood pressure, serum albumin, and serum creatinine. The results were expressed as an OR and its 95% CI.
We compared decreases in proteinuria after admission among the quartiles of pre-hospital urinary salt excretion by Dunnett’s multiple comparison test using the smallest quartile as a reference group.
In patients with 24-hour urine samples 3 months after discharge, we compared 24-hour urinary salt excretion before and after discharge in each group, and evaluated the proportion of patients with urinary salt excretion of 6 g/day or more in the second 24 hours after admission and at 3 months after discharge. We compared increases in proteinuria after discharge between patients with urinary salt excretion of 6 g/day or more and those with less than 6 g/day at 3 months after discharge by the Mann-Whitney test.
Differences were considered significant when the two-sided P-value was less than 0.05. Statistical analyses were performed using JMP software, Version 13 (SAS Institute Inc., Cary, NC).
Data Availability
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
References
Hung, S.-C. et al. Volume overload correlates with cardiovascular risk factors in patients with chronic kidney disease. Kidney Int. 85, 703–709 (2014).
Oberleithner, H. et al. Plasma sodium stiffens vascular endothelium and reduces nitric oxide release. Proc Natl Acad Sci. 104, 16281–16286 (2007).
Akdam, H. et al. Assessment of volume status and arterial stiffness in chronic kidney disease. Ren Fail. 36, 28–34 (2014).
Hummel, S. L., Seymour, E. M., Brook, R. D., Sheth, S. S. & Ghosh, E. Low-Sodium DASH Diet Improves Diastolic Function and Ventricular-Arterial Coupling in Hypertensive Heart Failure with Preserved Ejection Fraction. Circ Hear Fail. 2013 6, 1165–1171 (2013).
Koomans, H. A., Roos, J. C., Boer, P., Geyskes, G. G. & Mees, E. J. Salt sensitivity of blood pressure in chronic renal failure. Evidence for renal control of body fluid distribution in man. Hypertension. 4, 190–7 (1982).
Tanner, R. M. et al. Prevalence of Apparent Treatment-Resistant Hypertension among Individuals with CKD. Clin J Am Soc Nephrol. 8, 1583–1590 (2013).
Colombo, P. C. et al. Peripheral venous congestion causes inflammation, neurohormonal, and endothelial cell activation. Eur Heart J. 35, 448–454 (2014).
Japanese Society of Nephrology. Evidence-based practice guideline for the treatment of CKD. Clin Exp Nephrol. 13, 537–66 (2009).
Kidney Disease. Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 3, 1–150 (2013).
Simpson, F. O. Sodium intake, body sodium, and sodium excretion. Lancet. 2, 25–9 (1988).
Rose, B. D. & Post, T. Syntax of referencing in Clinical physiology of acid-base and electrolyte disorders 260–263 (McGraw-Hill Education, 2001).
Strauss, M. B., Lamdin, E., Smith, W. P. & Bleifer, D. J. Surfeit and deficit of sodium; a kinetic concept of sodium excretion. AMA Arch Intern Med. 102, 527–36 (1958).
Vogt, L., Waanders, F., Boomsma, F., de Zeeuw, D. & Navis, G. Effects of Dietary Sodium and Hydrochlorothiazide on the Antiproteinuric Efficacy of Losartan. J Am Soc Nephrol. 19, 999–1007 (2008).
McMahon, E. J. et al. A Randomized Trial of Dietary Sodium Restriction in CKD. J Am Soc Nephrol. 24, 2096–2103 (2013).
Meuleman, Y. et al. Sodium Restriction in Patients With CKD: A Randomized Controlled Trial of Self-management Support. Am J Kidney Dis. 69, 576–586 (2017).
Krikken, J. A., Dallinga-Thie, G. M., Navis, G. & Dullaart, R. P. F. Short term dietary sodium restriction decreases HDL cholesterol, apolipoprotein A-I and high molecular weight adiponectin in healthy young men: Relationships with renal hemodynamics and RAAS activation. Nutr Metab Cardiovasc Dis. 22, 35–41 (2012).
Mcmahon, E. J., Campbell, K. L., Bauer, J. D. & Mudge, D. W. Altered dietary salt intake for people with chronic kidney disease. Cochrane Database Syst Rev. 18, https://doi.org/10.1002/14651858.CD010070.pub2 (2015).
de Brito-Ashurst, I. et al. The role of salt intake and salt sensitivity in the management of hypertension in South Asian people with chronic kidney disease: a randomised controlled trial. Heart. 99, 1256–1260 (2013).
Yamaji, K. et al. Effect of educational hospitalization on chronic kidney disease (CKD) patients. Clin Nephrol. 68, 401–4 (2007).
Kusaba, T. et al. Sodium restriction improves the gustatory threshold for salty taste in patients with chronic kidney disease. Kidney Int. 76, 638–643 (2009).
Rioux, J. P., Cheema, H., Bargman, J. M., Watson, D. & Chan, C. T. Effect of an in-hospital chronic kidney disease education program among patients with unplanned urgent-start dialysis. Clin J Am Soc Nephrol. 6, 799–804 (2011).
Machida, S., Shibagaki, Y. & Sakurada, T. An inpatient educational program for chronic kidney disease. Clin Exp Nephrol. https://doi.org/10.1007/s10157-018-1660-5 (2018).
Sarafidis, P. A. et al. Prevalence, Patterns of Treatment, and Control of Hypertension in Predialysis Patients with Chronic Kidney Disease. Nephron Clin Pract. 120, 147–155 (2012).
Minutolo, R. et al. Assessment of achieved clinic and ambulatory blood pressure recordings and outcomes during treatment in hypertensive patients with CKD: a multicenter prospective cohort study. Am J Kidney Dis. 64, 744–52 (2014).
Pietinen, P. Estimating Sodium Intake from Food Consumption Data. Ann Nutr Metab. 26, 90–99 (1982).
Holbrook, J. T. et al. Sodium and potassium intake and balance in adults consuming self-selected diets. Am J Clin Nutr. 40, 786–93 (1984).
Brown, I. J., Tzoulaki, I., Candeias, V. & Elliott, P. Salt intakes around the world: Implications for public health. Int J Epidemiol. 38, 791–813 (2009).
Strazzullo, P. et al. Altered renal sodium handling in men with abdominal adiposity: a link to hypertension. J Hypertens. 19, 2157–64 (2001).
Visser, F. W., Krikken, J. A., Muntinga, J. H. J., Dierckx, R. A. & Navis, G. J. Rise in extracellular fluid volume during high sodium depends on bmi in healthy men. Obesity. 17, 1684–1688 (2009).
Krikken, J. A., Lely, A. T., Bakker, S. J. & Navis, G. The effect of a shift in sodium intake on renal hemodynamics is determined by body mass index in healthy young men. Kidney Int. 71, 260–265 (2007).
Matsushita, K., van der Velde, M., Astor, B. C., Woodward, M. & Levey, A. S. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality: a collaborative meta-analysis of general population cohorts. Lancet. 375, 2073–2081 (2014).
Iseki, K., Ikemiya, Y., Iseki, C. & Takishita, S. Proteinuria and the risk of developing end-stage renal disease. Kidney Int. 63, 1468–1474 (2003).
Heeg, J. E., De Jong, P. E., Van der Hem, G. K. & De Zeeuw, D. Efficacy and variability of the antiproteinuric effect of ACE inhibition by lisinopril. Kidney Int. 36, 272–279 (1989).
Esnault, V. L. M., Amr, E., Catherine, D., Marie-Genevieve, M. & Jean-Michel, N. Diuretic and Enhanced Sodium Restriction Results in Improved Antiproteinuric Response to RAS Blocking Agents. J Am Soc Nephrol. 16, 474–481 (2005).
Houlihan, C. A. et al. A low-sodium diet potentiates the effects of losartan in type 2 diabetes. Diabetes Care. 25, 663–671 (2002).
Hata, T. et al. The seasonal variation of blood pressure in patients with essential hypertension. Clin Exp Hypertens. A 4, 341–54 (1982).
Wang, A. Y.-M. & Lai, K.-N. Use of Cardiac Biomarkers in End-Stage Renal Disease. J Am Soc Nephrol. 19, 1643–1652 (2008).
Davies, S. J. & Davenport, A. The role of bioimpedance and biomarkers in helping to aid clinical decision-making of volume assessments in dialysis patients. Kidney Int. 86, 489–496 (2014).
Matsuo, S. et al. Revised Equations for Estimated GFR From Serum Creatinine in Japan. Am J Kidney Dis. 53, 982–992 (2009).
Acknowledgements
The authors would like to thank Medical English Service for English language revision.
Author information
Authors and Affiliations
Contributions
Y.M. and K.T. designed the study. H.K., K.S. and T.H. carried out data acquisition. Y.I. was responsible for statistical analysis. Y.S., T.K., T.H. and S.M. assisted in revising the article. All authors approved the submitted version of this study.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mihara, Y., Kado, H., Yokota, I. et al. Rapid weight loss with dietary salt restriction in hospitalized patients with chronic kidney disease. Sci Rep 9, 8787 (2019). https://doi.org/10.1038/s41598-019-45341-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-45341-6
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.