Abstract
Junctophilin-2 (JPH2) is a part of the junctional membrane complex that facilitates calcium-handling in the cardiomyocyte. Previously, missense variants in JPH2 have been linked to hypertrophic cardiomyopathy; however, pathogenic “loss of function” (LOF) variants have not been described. Family-based genetic analysis of GME individuals with cardiomyopathic disease identified an Iranian patient with dilated cardiomyopathy (DCM) as a carrier of a novel, homozygous single nucleotide insertion in JPH2 resulting in a stop codon (JPH2-p.E641*). A second Iranian family with consanguineous parents hosting an identical heterozygous variant had 2 children die in childhood from cardiac failure. To characterize ethnicity-dependent genetic variability in JPH2 and to identify homozygous JPH2 variants associated with cardiac disease, we identified variants in JPH2 in a worldwide control cohort (gnomAD) and 2 similar cohorts from the Greater Middle East (GME Variome, Iranome). These were compared against ethnicity-matched clinical whole exome sequencing (WES) referral tests and a case cohort of individuals with hypertrophic cardiomyopathy (HCM) based on comprehensive review of the literature. Worldwide, 1.45% of healthy individuals hosted a rare JPH2 variant with a significantly higher proportion among GME individuals (4.45%); LOF variants were rare overall (0.04%) yet were most prevalent in GME (0.21%). The increased prevalence of LOF variants in GME individuals was corroborated among region-specific, clinical WES cohorts. In conclusion, we report ethnic-specific differences in JPH2 rare variants, with GME individuals being at higher risk of hosting homozygous LOF variants. This conclusion is supported by the identification of a novel JPH2 LOF variant confirmed by segregation analysis resulting in autosomal recessive pediatric DCM due to presumptive JPH2 truncation.
Similar content being viewed by others
Introduction
Dilated cardiomyopathy (DCM) is defined as a primary myocardial disorder characterized by ventricular dilation and impaired contractility not explained by abnormal loading conditions or ischemic insult1. DCM is attributable to both genetic and nongenetic causes and is found to be familial in about 25 to 50% of patients2,3,4. Of these familial cases, up to 37% have a clinically relevant genetic variant, leaving the majority of cases genetically unexplained5. DCM is a genetically heterogenous disease with disease-associated genes ranging from sarcomeric structure to metabolic etiologies to MAPK pathways. One such category includes genes encoding for proteins in calcium (Ca2+)-signaling, and -sensitive, pathways, such as JPH2-encoded junctophilin type 2 (JPH2)6.
JPH2 is a striated muscle-specific protein and a critical member of the junctional membrane complex (JMC) that regulates myocardial excitation-contraction (E-C) coupling7,8. Cardiac contraction is dependent on efficient E-C coupling which is mediated by Ca2+. Ca2+ influx through voltage-gated L-type calcium channels in the t-tubular plasma membrane triggers further Ca2+ release via the ryanodine receptor 2 in the sarcoplasmic reticulum9,10. JPH2 anchors the junction between t-tubular sarcolemma and the sarcoplasmic reticulum as well as stabilizes the ryanodine receptor 28,11,12. Early studies have suggested a role for JPH2 in the development of DCM, with loss of normal JPH2 expression during pathologic remodeling13,14,15,16. The importance of JPH2 in the structural and functional integrity of the JMC is further reinforced clinically by the observation of disease-associated variants in JPH2 found in a small number of patients with cardiomyopathy as well as atrial fibrillation11,17,18,19,20.
The clinical expansion of broad genetic sequencing, such as whole exome sequencing (WES), has allowed for rare causes of cardiomyopathy to be identified and research-based exome sequencing has identified rare variants in disease-associated genes. Despite a greater incidence of autosomal recessive disease-causing variants, regions such as the Greater Middle East (GME) remain underrepresented and understudied21,22,23. In this study, we identify two Iranian families hosting a novel loss-of-function (LOF) JPH2 variant that, when homozygous, was associated with DCM and death in early childhood from cardiac failure. We then systematically examine the background frequency of rare variants of JPH2 in regionally diverse populations as well as clinical WES sequencing referrals, including those from the GME. We conclude that there are ethnic-specific differences in rare JPH2 variants, with GME individuals being at higher risk of hosting homozygous LOF variants.
Methods
Study cohorts
This research study was approved by the Baylor College of Medicine and the Ahvaz Jundishapur University of Medical Sciences Institutional Review Boards. For genetic studies involving cohorts, informed consent was waived. For WES studies, informed consent was obtained. All experiments were performed in accordance with relevant guidelines and regulations.
Population-based control cohorts
Worldwide, population-based, control variants were derived from the Genome Aggregate Database (gnomAD) made up of 138,632 individuals as well as regionally-specific cohorts24. While the gnomAD database is comprised partly of various disease-specific cohorts in addition to population genetics studies, it excludes individuals known to have severe pediatric disease as well as severe disease in their first-degree relatives; therefore, we utilized these individuals as “control” or “reference” alleles. Furthermore, although this database includes many geographically distinct cohorts, the GME is under-represented within gnomAD and individuals from this region are not clearly delineated. Thus, variants of ostensibly healthy individuals from GME were derived from the GME Variome (N = 1,111)21 and Iranome (N = 800)25, respectively. The GME Variome includes individuals from a large collection of Arab and non-Arab Muslim countries (Morocco, Algeria, Tunisia, Libya, Egypt, Turkey, Syria, Lebanon, Israel, Saudi Arabia, Iraq, Qatar, Kuwait, Yemen, UAE, Iran, Oman, and Pakistan), and excludes individuals with a genetic kinship coefficient suggestive of a high degree of relatedness. Given overlap in the population of GME Variome and the African/African American population of gnomAD, Iranome was included to control for the population solely from Iran. For population frequency calculations of “rare variants,” a minor allele frequency (MAF) of <0.01 was utilized. In total, 140,543 individuals across these 3 cohorts were included as controls.
Baylor and Iranian whole exome sequencing cohorts
Given widespread advancement in clinical WES testing, we determined the frequency of JPH2 variants in 2 clinical WES referral cohorts. The Baylor clinical WES cohort has been previously described26 and is derived from WES variant data compiled by Baylor Genetics Laboratories27. This cohort was comprised of 7,066 probands referred for WES genetic testing to the Baylor Genetics Laboratories (Houston, Texas, United States) independent of referral diagnosis or indication for genetic testing. Individuals included in this cohort were genetic testing probands. Demographic and clinical referral information was abstracted. Genetic information from samples derived for platform validation studies, or from oncological samples, was excluded. For GME-matched WES referral variants, a cohort of 823 clinical WES referrals from Iran were analyzed. Variants included in these WES cohorts were (1) identified in the coding nucleotide sequence or predicted splice junction of an HCM-associated gene locus, (2) potential splice donor or splice acceptor-effecting variants located within the first four nucleotides near the splice junction, and (3) deemed “pathogenic”, “likely pathogenic”, or “variant of uncertain significance” (VUS) at the time of genetic testing according to the American College of Medical Genetics (ACMG) criteria/interpretation guidelines28,29, and (4) included on the clinical report sent, or made available, to the referring provider. Variants excluded from this study were: (1) interpreted as “not pathogenic” at the time of genetic testing, (2) non-splice site intronic variants, (3) 5′or 3′ untranslated region variants, or (4) synonymous variants. To account for changes in evidence of pathogenicity since the initial variant identification and classification at the time of genetic testing, each variant in the Iranian and Baylor WES cohorts was subjected to further verification for pathogenicity via ClinVar aggregate records30. All variants classified as “benign” or “likely benign” as of January 23, 2019 were excluded.
Pathogenic variant cohort
To determine the prevalence of cardiomyopathy-associated JPH2 variants, previously published studies were utilized11,17,18. A combined prevalence from these cohort-based studies was created. Inclusion criteria were (1) associated with a proband/family with a clinical diagnosis of hypertrophic or dilated cardiomyopathy, (2) absence of a compound variant deemed to be a likely disease-associated variant, (3) absence of the variant in reference/control alleles, and (4) identified in a cohort-based study. Variants obtained from non-cohort-based studies that otherwise met inclusion criteria were utilized for non-prevalence analyses.
Whole exome sequencing
Clinical WES testing was conducted as previously described for the Baylor WES cohort27. Briefly, extracted DNA was subjected to an in-house exome capture platform (VCRome version 2.1) and sequenced using either an Illumina Genome Analyzer IIx platform or the Illumina HiSeq 2000 platform. Samples were additionally analyzed by an Illumina HumanExome-12 v1 cSNP array for quality-control assessment of exome data, as well as for detecting large copy-number variants and regions of absence of heterozygosity. Iranian clinical WES testing utilized commercial platforms (Beijing Genomic Institute, Shenzhen, China; Macrogen, Seoul, South Korea)30. WES performed on DNA from the proband of the first family; the second family (Family 2) had WES performed on parents due to unavailability of samples from deceased children. Haplotype analysis was performed as previously described31. Presence or absence of putatively pathogenic variants were compared against the 1000 Genomes Project32, NHLBI GO Exome Sequencing Project, gnomAD, as well as the ethnically-matched GME Variome and Iranome. Confirmation of the WES-identified JPH2-p.E641* variant was conducted in the probands of each kindred using direct Sanger sequencing. Further, variant positivity was evaluated in all kindred using Sanger sequencing.
Nomenclature
LOF variants were defined as variants that are predicted to cause a protein loss-of-function including nonsense (early termination), insertion/deletion (both in-frame and out-of-frame), and predicted canonical splice site variants. Among WES variants, designations of pathogenic, likely pathogenic, or VUS were based on the designation at the time of WES testing. Variant annotations were based on established nomenclature33.
Sequence homology and domain mapping
JPH2 consensus primary sequence (NM_020433, NP_065166) was utilized from the Ensembl browser34. Variants were mapped along the protein topology. Primary sequence conservation among 56 independent JPH2 orthologues was compared to determine degree of conservation across species using the National Center for Biotechnology Information (NCBI).
Statistics
Statistical results were expressed as mean with variance expressed as standard deviation or median and interquartile range (brackets), as appropriate. Variance of prevalence/proportion was expressed as the exact 95% confidence interval around proportion when statistical comparisons were made (brackets). Comparisons were made by Student’s t-Test, Fisher’s Exact test, Chi-Square with Yates Correction, as appropriate using OpenEpi35. Statistical significance threshold was set at P < 0.05.
Results
Identification of a homozygous JPH2-p.E641* variant in an infant with DCM
The proband demonstrated severe left ventricular (LV) dilation with rapidly declining systolic function as an infant. He initially presented at 20 months of age after being hospitalized with fever, tachypnea, and restlessness. Imaging tests, including chest radiographs, electrocardiogram, and echocardiography, confirmed the diagnosis of DCM. By 4.5 years of age, LV systolic function was severely depressed with medically-refractory heart failure (Fig. 1A–C). A representative electrocardiogram demonstrating PR-prolongation, conduction delay, and T-wave abnormalities is depicted in Fig. 1D. The patient was referred for cardiac transplantation; however, the patient ultimately died at 5 years of age while awaiting transplant. This child was the offspring of consanguineous parents (first cousins) who had 2 affected sons. The pedigree is depicted in Fig. 2A. The mother (III-7) had 4 total pregnancies, with 1 spontaneous abortion at 8 weeks (IV-1), and 3 live births. The second affected pregnancy was an infant boy (IV-2) who presented with sudden fever, poor feeding, jaundice, and hypotonia as a neonate. He had cardiomegaly, clinical features consistent with cardiomyopathy, and died at 37 days of age after a cardiorespiratory arrest. Subsequently, the mother gave birth to the proband (IV-3).
(A–C) Transthoracic echocardiography images of the JPH2-p,E641* homozygous variant-positive proband demonstrating a severely dilated left ventricle with reduced systolic function and D, 12-lead ECG demonstrating bi-atrial dilation, PR-prolongation, interventricular conduction delay, and T wave abnormalities.
(A) Family 1 pedigree of the JPH2-p.E641* homozygous variant-positive proband and extended kindred. Arrow denotes proband; gray fill, fetal loss; black fill, dilated cardiomyopathy; diagonal line, deceased. (B) Sanger sequence chromatograms depicted wild type JPH2 as well as JPH2-p.E641* heterozygous and homozygous sequencing. (C) Linear topology with protein functional domains of JPH2 are depicted with location of p.E641* variant (red line) in the divergent region.
Genetic testing for genes canonically associated with DCM were negative for likely pathogenic variants. WES was performed and the proband was found to host a homozygous single nucleotide insertion (c.1920dupT) resulting in a premature stop codon (JPH2-p.E641*) (Fig. 2B,C; Supp. Fig. 1). The proband hosted no other pathogenic variants in currently known monogenic disease-causing genes identified on WES. This JPH2 variant is novel and absent in 299,100 reference alleles derived from healthy individuals. JPH2-p.E641* localizes to the C-terminal divergent region in an area of low sequence homology and relatively high variation. Segregation analysis was performed for the variant to determine the mode of inheritance. Although no genetic information was available for the family’s first and second children (IV-1, IV-2), both parents and their fourth child (III-6, III-7, IV-4) were found to be heterozygous for JPH2-p.E641*. Additionally, this variant was found in the heterozygous state in 8 of 32 healthy family members of the proband who were available for genetic screening. These findings suggest an autosomal recessive mode of inheritance with functional genetic truncation of JPH2 associated with neonatal cardiomyopathy.
JPH2-p.E641* variant possibly associated with rapid ventricular failure in neonatal Ebstein anomaly
Supporting the hypothesis that homozygous JPH2-p.E641* is associated with cardiac failure, we identified a second consanguineous Iranian family with this variant (Fig. 3). This family was seemingly unrelated to the previous family although they shared a similar ethnic background (Lor – a group of Iranian people found predominantly in southwest Iran). The first child of the mother and father (first cousins once-removed) presented at 6 months of age with fever, restlessness, and poor feeding following a sandstorm. His clinical status continued to decline after admission, and he eventually died from in-hospital cardiac arrest 3 days later. The second pregnancy was prenatally diagnosed with Ebstein anomaly and the child initially did well until 2 years of age when he underwent tricuspid valve annuloplasty and atrial septal defect closure. Post-operatively, he had episodes of respiratory distress and gradually developed fluid-filled blisters on his skin and had generalized edema involving hands, feet, face and abdomen. He developed progressive ventricular failure and died at 2.5 years of age due to a cardiac arrest. DNA was not obtained on either child; however, both parents were found to be heterozygous for JPH2-p.E641*. Extended segregation analysis identified 2 heterozygous carriers out of 9 additional healthy family members of the proband who did not have cardiomyopathy or history of cardiac disease and were able to undergo genetic testing. Haplotype analysis using rare variants identified in the WES data from the proband of Family 1, and the parents of Family 2 showed an identical haplotype containing the JPH2 variant, indicative of a founder effect.
JPH2 demonstrates ethnic-specific variability in genetic sequence
Given our findings of a truncating LOF JPH2 variant associated with cardiac death early in childhood in two GME families, we next sought to characterize the differences in genetic variation of JPH2 amongst ethnically distinct populations. We first examined the frequency of rare JPH2 variants in several population-based genomic studies of control individuals. Among 138,632 individuals genotyped in the gnomAD cohort, there were 2,015 variants with a MAF < 0.01 that contributed to a total rare variant frequency of 1.45% [1.39–1.52]. When divided by regional subtypes, the highest prevalence of rare JPH2 variants was found in African American/African individuals (5.03% [4.65–5.43]) followed by European (Finnish) (1.74% [1.51–1.96]). Given the underrepresentation of GME individuals within gnomAD, and recent evidence of high genetic variation and autosomal recessive variants21, we next evaluated 2 additional GME-specific databases. Of the 1,111 individuals in the GME Variome cohort, there were 50 variants with a MAF < 0.01 leading to a total variant frequency of 4.50% [3.28–5.72]. Due to potential overlap between the GME Variome population and African/African American subgroup of gnomAD, the Iranome cohort was also included. The Iranome cohort demonstrated 35 variants found within 800 individuals providing a prevalence of 4.38% [2.96–5.79]. The GME Variome and Iranome cohorts each demonstrated a higher overall prevalence of JPH2 variants than any gnomAD subgroup other than African American/African (P < 0.001). There was no difference between GME Variome and Iranome JPH2 variant frequency.
Given the high prevalence of rare variants within control individuals, we next evaluated these cohorts for rare LOF variants. The incidence of LOF variants was rare within the gnomAD cohort with a prevalence of 0.04% [0.03–0.05]. In comparison, the Iranome cohort contained 3 identified LOF variants for an overall prevalence of 0.375% [0.00–0.80], nearly 10-fold the prevalence seen in gnomAD cohort. This was significantly higher than all regional groups except European (Finnish) (0.16%, [0.09–0.22]) (P < 0.001). The GME Variome hosted 1 LOF variant (0.09% [0.00–0.27]). For the purposes of comparison, both the GME Variome and Iranome were combined into a “GME Healthy Cohort” that had an overall JPH2 variant prevalence of 4.45% [3.52–5.37], with a LOF variant prevalence of 0.21% [0.01–0.41]. All LOF variants in control cohorts were heterozygous. There was a single truncating LOF variant noted in the GME Healthy Cohort. However, there were 25 total individuals in the gnomAD cohort (0.02% [0.01–0.03]) hosting heterozygous truncating variants, 18 of which were Finnish. There were no homozygous truncating variants noted in any control cohort. These results are summarized in Fig. 4A. Taken together, these results indicate a greater burden of JPH2 variation in healthy individuals from GME regions, particularly in LOF variants.
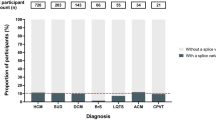
(A) Bar graph comparing the frequencies of rare JPH2 variants in ostensibly healthy individuals. The gnomAD cohort is broken down into 8 ethnic subgroups. GME Variome and Iranome represent 2 independent Middle Eastern cohorts. No fill, total frequency; tan, missense variant frequency; red, LOF variant frequency. Error bars denote 95% CI; *P < 0.05, **P < 0.001 compared to European (Non-Finnish). (B) Bar graph comparing the frequencies of JPH2 variants in a GME Healthy Cohort (GME Variome + Iranome), an ostensibly healthy population (gnomAD), a cohort of clinical WES referrals at Baylor College of Medicine (WES), a cohort of clinical WES referrals from Iran (WES-Iran), and a population of those diagnosed with HCM. Error bars denote 95% CI; *P < 0.05, **P < 0.001 compared to gnomAD.
Variants in JPH2 demonstrate ethnic-specific variability among clinical WES referrals
Due to widespread advancement in clinical WES testing, we next compared these findings to the frequency of identified variants within regionally-matched cohorts of clinical WES referrals. Among 7,066 unrelated probands undergoing clinical WES testing at Baylor College of Medicine, 167 probands hosted a JPH2 variant (2.36% [2.01–2.72]), including 10 probands with LOF variants (0.14% [0.05–0.23]). These were both modestly higher than the total variant prevalence and LOF variant prevalence observed in the gnomAD cohort (P < 0.001). Similarly, among 823 Iranian clinical WES referrals, 24 probands hosted a rare variant of JPH2 (2.92% [1.77–4.07]), 6 of which were LOF (0.73% [0.15–1.31]). Among the 6 LOF variants identified within the Iranian WES cohort, two were JPH2-p.E641* variants – one from each of the two families described above. One JPH2-p.E641* variant represents the homozygous affected proband from Family 1, whereas the second variant represents a heterozygous unaffected parent from Family 2 with evidence of two infant deaths related to cardiac failure. All LOF variants identified in clinical WES cohorts are detailed in Table 1. Between these 2 clinical WES cohorts, there was no significant difference in prevalence of total variants; however, the Iranian WES cohort demonstrated a significantly higher prevalence of LOF variants (P < 0.001). Overall, this indicates a higher incidence of JPH2 LOF variants in GME individuals referred for clinical genetic testing in independent region-specific cohorts, corroborating a similar finding in population-based, ostensibly healthy individuals. These results are summarized in Fig. 4B.
Frequency of JPH2 variants among cases of cardiomyopathy
Due to the high background rate of rare variants in JPH2, we explored the rate of pathogenic JPH2 variants found in patients clinically diagnosed with cardiomyopathy. Of the 981 individuals with cardiomyopathy in the HCM cohort, only 6 (0.61% [0.12–1.10]) hosted a JPH2 variant, all of which were heterozygous missense variants. This was significantly lower than the prevalence demonstrated in gnomAD (1.45%, P < 0.05), the GME Healthy cohort (4.45%, P < 0.001), and both of the clinical WES cohorts (WES-Iran 2.92%, WES-Baylor 2.36%, P < 0.001). No LOF variants were described. These results are summarized in Fig. 4B. Importantly, of the 6 cardiomyopathy-associated variants identified, only 1 was also found to be present in control cohorts (JPH2-A405S, gnomAD MAF = 9.69E-05). None of the 7 cardiomyopathy-associated variants were found in the GME Variome or Iranome cohorts. Taken together, these results suggest that pathogenic JPH2 variants are rare among patients with cardiomyopathy and are largely absent in population and clinical WES-based cohorts.
Comparison of genetic variability, orthologue identity, and variant topology
To characterize the genetic variation found in JPH2, amino-acid level sequence homology analysis was performed to correlate with genetic variation. The structure of JPH2 is comprised of 8 membrane occupation and recognition nexus (MORN) domains that associate with the t-tubule at the N-terminus, a C-terminal transmembrane domain that anchors into the sarcoplasmic reticulum, and an alpha-helical domain that spans the junctional space in between8. We observed the highest degree of sequence homology in the MORN domains, followed by the transmembrane and alpha-helix domains. There was markedly less sequence homology demonstrated in the linker and divergent domains. We next overlaid the prevalence of all variants in individuals from the gnomAD cohort by amino acid, including those above the MAF threshold, which revealed generally higher levels of genetic variability in regions with less sequence homology, such as the linker region. There were 2 common variants within the gnomAD cohort with MAF > 0.01 included in this analysis, JPH2-A396T (MAF = 0.179) and G505S (MAF = 0.011). Amino acid positions containing LOF variants found in ostensibly healthy individuals as well as disease-associated variants were also mapped. Both the LOF and the disease-associated variants did not appear to localize to areas of high homology nor to areas of high genetic variability. These results are summarized in Fig. 5. Overall, these findings suggest that areas of high sequence variation correspond to areas less conserved across species. However, both cardiomyopathy-associated variants and LOF variants found in ostensibly healthy individuals do not seem to localize to specific “hot spots” on the protein.
Amino-acid level genetic variability analysis of JPH2. Functional domains of JPH2 are depicted. Ortholog identity map and prevalence of variants in healthy individuals (gnomAD) by amino acid are depicted with orange lines representing rolling averages. Amino acid positions containing radical variants found in ostensibly healthy individuals and disease-causing variants found in those with cardiomyopathies are depicted, with those in red representing variants identified in individuals from the Middle East. MORN, membrane occupation and recognition nexus domain; TM, Transmembrane domain. *MAF exceeding Y-axis.
Discussion
In this study, for the first time to our knowledge, we present a novel homozygous LOF JPH2 variant, JPH2-p.E641*, associated with autosomal recessive DCM in an Iranian family, confirmed by segregation analysis. This finding was further supported by a second Iranian family where both healthy parents carry the same LOF JPH2 variant and who had 2 children who died in early childhood from cardiac failure, 1 in the context of structural heart disease. In the case of this novel truncating nonsense variant, it is possible that the homozygous loss of the C-terminal transmembrane domain in individuals hosting JPH2-p.E641* causes loss of anchoring to the sarcoplasmic reticulum, resulting in impaired Ca2+ handling and increased risk of heart failure early in life. Prior to these observations, only heterozygous missense JPH2 variants have been linked to a cardiomyopathy phenotype11,17,18,19.
In the setting of these findings, a growing body of evidence has demonstrated that alterations in JPH2 expression and function can perturb intracellular Ca2+ signaling and result in myopathic disease, including HCM and DCM12,36. JPH2-null mice demonstrate embryonic lethality due to molecular failure of the JMC and ineffective Ca2+-signaling needed to sustain EC coupling and cardiac contractility7,15. Furthermore, induction of JPH2 expression silencing in adult mice is associated with rapid deterioration into heart failure with a dilated left ventricle and loss of systolic function16,37. When combined with the striking phenotype observed in the 2 families presented here, which mimic these rodent models, our findings support the concept that loss of JPH2 expression can result in rapid progression of cardiomyopathy and heart failure. Additional studies utilizing in vitro and in vivo models are needed to fully explore this possible mechanism disease.
The investigation of pathogenic JPH2 variants in individuals with cardiomyopathies has temporally coincided with a recent increase in clinical utilization of next-generation sequencing modalities. Tools like WES not only increase the sensitivity for detecting genetic variants in atypical clinical presentations, but also have given us a window into the natural variability of human genome and how it varies by geographic and ethnic backgrounds24,38. Based on the underrepresentation of GME populations in current large-scale public genome databases, and the relatively high density of genetic disease within the GME population, we sought to examine whether significant genetic variability in JPH2 existed between GME and other ethnic populations. Remarkably, we found a high burden of genetic variation, including LOF variants, within cohorts representing the GME. The higher prevalence of LOF variants was replicated in clinical genetic testing referrals and may contribute to an overall increased risk of development of JPH2-related AR cardiomyopathy in those with GME/Iranian ethnic backgrounds. These observations highlight the critical nature of comparing disease-associated variants with ethnically-matched control alleles. This is reflected in the American College of Genetics and Genomics recommendations to include race-matched control data when interpreting sequence variants39.
The variants from WES cohorts in JPH2 are difficult to interpret, particularly in individuals with a low pre-test probability of disease. Previously there has been evidence to suggest that incidentally identified variants in channelopathies likely represent background genetic variation26,40 Both clinical WES cohorts hosted variants at a markedly higher rate than cardiomyopathy cases, which supports the hypothesis that the majority of these JPH2 variants also represent background noise. The requirement of the truncating variant JPH2-p.E641* to be homozygous in order to produce clinical disease also suggests that previously described heterozygous missense variants may result in disease through a dominant-negative effect41. However, the challenge in clinical evaluation of children who may develop a cardiomyopathy phenotype later in life must be recognized. Furthermore, the presence of variants in phenotype-negative individuals does not necessarily exclude variant pathogenicity, as is seen in TTN truncating variants that have been shown to cause DCM despite their presence in up to 1% of the general population42. This highlights the need for more research to improve identification of susceptibility alleles and the role that missense JPH2 variants play in contributing to cardiomyopathies.
Previous studies in arrhythmogenic disorders have demonstrated the value of mapping variant locations in assessing for risk of pathogenicity, suggesting that some regions of disease-causing genes may have elevated signal-to-noise ratios26,43. In an effort to characterize the genotype-phenotype mechanism of this study’s novel LOF variant, we stratified JPH2 variant analysis at the amino acid level and compared it to other previously identified variants. We found that both LOF and disease-causing variants did not cluster in areas of either increased homology or increased variance, nor did they localize to a specific protein motif. Combined with the many healthy Iranian family members that hosted a single copy of JPH2-p.E641*, this reinforces the likelihood that a heterozygous LOF variant would be insufficient to cause disease. Additionally, while the number of pathogenic and LOF variants are relatively small, these results suggest that there are no specific disease-associated “hotspot” domains in JPH2.
This study has several limitations. First, the supporting evidence that the second Iranian family provides in the potential pathogenicity of JPH2-p.E641* is limited by the lack of genotype on any of the diseased offspring noted. However, the presence of additional healthy heterozygous individuals, when combined with the incidence of multiple presumed cardiac deaths in childhood in the offspring of two heterozygous parents, warranted inclusion of the family in the study. Second, this study uses a MAF of <0.01 as an upper threshold for inclusion of rare variants in control cohorts. Though a MAF threshold of <0.0001 has previously been validated for rare cardiomyopathy-associated variants44, this upper bound was not feasible given the smaller size of the GME Variome and Iranome cohorts. The large difference in the size of these cohorts makes comparison challenging and is a result of the underrepresentation of GME individuals in larger genomic databases. This emphasizes the need for further large-scale investigation into this population.
Conclusions
Our findings add to the growing evidence that variants in JPH2 play a role in cardiomyopathy; and suggest that this novel biallelic truncating variant can give rise to severe, early-onset cardiomyopathy. Given the higher prevalence of LOF variants identified in ethnically-matched controls, as well as evidence to suggest that heterozygous LOF variants are insufficient to cause disease, it is likely that this proband’s risk of disease was exacerbated by their ethnic background.
Data Availability
JPH2-p.E641* proband information has been uploaded to PhenomeCentral45 (https://www.phenomecentral.org) under ID number P0008365.
References
Richardson, P. et al. Report of the 1995 World Health Organization/International Society and Federation of Cardiology Task Force on the Definition and Classification of cardiomyopathies. Circulation 93, 841–842 (1996).
Bozkurt, B. et al. Current Diagnostic and Treatment Strategies for Specific Dilated Cardiomyopathies: A Scientific Statement From the American Heart Association. Circulation 134, e579–e646, https://doi.org/10.1161/CIR.0000000000000455 (2016).
Elliott, P. et al. Classification of the cardiomyopathies: a position statement from the European Society Of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J 29, 270–276, https://doi.org/10.1093/eurheartj/ehm342 (2008).
Burkett, E. L. & Hershberger, R. E. Clinical and genetic issues in familial dilated cardiomyopathy. J Am Coll Cardiol 45, 969–981, https://doi.org/10.1016/j.jacc.2004.11.066 (2005).
Pugh, T. J. et al. The landscape of genetic variation in dilated cardiomyopathy as surveyed by clinical DNA sequencing. Genet Med 16, 601–608, https://doi.org/10.1038/gim.2013.204 (2014).
Vasilescu, C. et al. Genetic Basis of Severe Childhood-Onset Cardiomyopathies. J Am Coll Cardiol 72, 2324–2338, https://doi.org/10.1016/j.jacc.2018.08.2171 (2018).
Takeshima, H., Komazaki, S., Nishi, M., Iino, M. & Kangawa, K. Junctophilins: a novel family of junctional membrane complex proteins. Mol Cell 6, 11–22 (2000).
Beavers, D. L., Landstrom, A. P., Chiang, D. Y. & Wehrens, X. H. Emerging roles of junctophilin-2 in the heart and implications for cardiac diseases. Cardiovasc Res 103, 198–205, https://doi.org/10.1093/cvr/cvu151 (2014).
López-López, J. R., Shacklock, P. S., Balke, C. W. & Wier, W. G. Local calcium transients triggered by single L-type calcium channel currents in cardiac cells. Science 268, 1042–1045 (1995).
Bers, D. M. Cardiac excitation-contraction coupling. Nature 415, 198–205, https://doi.org/10.1038/415198a (2002).
Beavers, D. L. et al. Mutation E169K in junctophilin-2 causes atrial fibrillation due to impaired RyR2 stabilization. J Am Coll Cardiol 62, 2010–2019, https://doi.org/10.1016/j.jacc.2013.06.052 (2013).
Landstrom, A. P., Beavers, D. L. & Wehrens, X. H. The junctophilin family of proteins: from bench to bedside. Trends Mol Med. 20(6), 353–362, https://doi.org/10.1016/j.molmed.2014.02.004 (2014).
Xu, M. et al. Intermolecular failure of L-type Ca2+ channel and ryanodine receptor signaling in hypertrophy. PLoS Biol 5, e21, https://doi.org/10.1371/journal.pbio.0050021 (2007).
Wei, S. et al. T-tubule remodeling during transition from hypertrophy to heart failure. Circ Res 107, 520–531, https://doi.org/10.1161/CIRCRESAHA.109.212324 (2010).
Minamisawa, S. et al. Junctophilin type 2 is associated with caveolin-3 and is down-regulated in the hypertrophic and dilated cardiomyopathies. Biochem Biophys Res Commun 325, 852–856, https://doi.org/10.1016/j.bbrc.2004.10.107 (2004).
Landstrom, A. P. et al. Junctophilin-2 expression silencing causes cardiocyte hypertrophy and abnormal intracellular calcium-handling. Circ Heart Fail 4, 214–223, https://doi.org/10.1161/CIRCHEARTFAILURE.110.958694 (2011).
Landstrom, A. P. et al. Mutations in JPH2-encoded junctophilin-2 associated with hypertrophic cardiomyopathy in humans. J Mol Cell Cardiol 42, 1026–1035, https://doi.org/10.1016/j.yjmcc.2007.04.006 (2007).
Quick, A. P. et al. Novel junctophilin-2 mutation A405S is associated with basal septal hypertrophy and diastolic dysfunction. JACC Basic Transl Sci 2, 56–67, https://doi.org/10.1016/j.jacbts.2016.11.004 (2017).
Sabater-Molina, M. et al. Mutation in JPH2 cause dilated cardiomyopathy. Clin Genet 90, 468–469, https://doi.org/10.1111/cge.12825 (2016).
Vanninen, S. U. M. et al. Heterozygous junctophilin-2 (JPH2) p.(Thr161Lys) is a monogenic cause for HCM with heart failure. PLoS One 13, e0203422, https://doi.org/10.1371/journal.pone.0203422 (2018).
Scott, E. M. et al. Characterization of Greater Middle Eastern genetic variation for enhanced disease gene discovery. Nat Genet 48, 1071–1076, https://doi.org/10.1038/ng.3592 (2016).
Al-Gazali, L., Hamamy, H. & Al-Arrayad, S. Genetic disorders in the Arab world. BMJ 333, 831–834, https://doi.org/10.1136/bmj.38982.704931.AE (2006).
Sheffield, V. C., Stone, E. M. & Carmi, R. Use of isolated inbred human populations for identification of disease genes. Trends Genet 14, 391–396 (1998).
Lek, M. et al. Analysis of protein-coding genetic variation in 60,706 humans. Nature 536, 285–291, https://doi.org/10.1038/nature19057 (2016).
Akbari, M. et al. In ASHG Annual Meeting (Orlando, FL, USA, 2017).
Landstrom, A. P. et al. Interpreting Incidentally Identified Variants in Genes Associated With Catecholaminergic Polymorphic Ventricular Tachycardia in a Large Cohort of Clinical Whole-Exome Genetic Test Referrals. Circulation. Arrhythmia and electrophysiology 10, https://doi.org/10.1161/CIRCEP.116.004742 (2017).
Yang, Y. et al. Molecular findings among patients referred for clinical whole-exome sequencing. JAMA 312, 1870–1879, https://doi.org/10.1001/jama.2014.14601 (2014).
Green, R. C. et al. ACMG recommendations for reporting of incidental findings in clinical exome and genome sequencing. Genet Med 15, 565–574, https://doi.org/10.1038/gim.2013.73 (2013).
Directors, A. B. O. ACMG policy statement: updated recommendations regarding analysis and reporting of secondary findings in clinical genome-scale sequencing. Genet Med 17, 68–69, https://doi.org/10.1038/gim.2014.151 (2015).
Landrum, M. J. et al. ClinVar: improving access to variant interpretations and supporting evidence. Nucleic Acids Res 46, D1062–D1067, https://doi.org/10.1093/nar/gkx1153 (2018).
Schaffer, A. E. et al. CLP1 founder mutation links tRNA splicing and maturation to cerebellar development and neurodegeneration. Cell 157, 651–663, https://doi.org/10.1016/j.cell.2014.03.049 (2014).
Auton, A. et al. A global reference for human genetic variation. Nature 526, 68–74, https://doi.org/10.1038/nature15393 (2015).
den Dunnen, J. T. et al. HGVS Recommendations for the Description of Sequence Variants: 2016 Update. Hum Mutat 37, 564–569, https://doi.org/10.1002/humu.22981 (2016).
Zerbino, D. R. et al. Ensembl 2018. Nucleic Acids Res 46, D754–D761, https://doi.org/10.1093/nar/gkx1098 (2018).
Dean, A., Sullivan, K. & Soe, M. OpenEpi: Open Source Epidemiologic Statistics for Public Health, version 3.01, www.OpenEpi.com (2006).
Zhang, H. B. et al. Ultrastructural uncoupling between T-tubules and sarcoplasmic reticulum in human heart failure. Cardiovasc Res 98, 269–276, https://doi.org/10.1093/cvr/cvt030 (2013).
van Oort, R. J. et al. Disrupted junctional membrane complexes and hyperactive ryanodine receptors after acute junctophilin knockdown in mice. Circulation 123, 979–988, https://doi.org/10.1161/CIRCULATIONAHA.110.006437 (2011).
Yang, Y. et al. Clinical whole-exome sequencing for the diagnosis of mendelian disorders. The New England journal of medicine 369, 1502–1511, https://doi.org/10.1056/NEJMoa1306555 (2013).
Richards, S. et al. Standards and guidelines for the interpretation of sequence variants: A joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 17, 405–424, https://doi.org/10.1038/gim.2015.30 (2015).
Landstrom, A. P. et al. Amino acid-level signal-to-noise analysis of incidentally identified variants in genes associated with long QT syndrome during pediatric whole exome sequencing reflects background genetic noise. Heart Rhythm. https://doi.org/10.1016/j.hrthm.2018.02.031 (2018).
Walsh, R. et al. Defining the genetic architecture of hypertrophic cardiomyopathy: re-evaluating the role of non-sarcomeric genes. Eur Heart J 38, 3461–3468, https://doi.org/10.1093/eurheartj/ehw603 (2017).
Schafer, S. et al. Titin-truncating variants affect heart function in disease cohorts and the general population. Nat Genet 49, 46–53, https://doi.org/10.1038/ng.3719 (2017).
Giudicessi, J. R. et al. Phylogenetic and physicochemical analyses enhance the classification of rare nonsynonymous single nucleotide variants in type 1 and 2 long-QT syndrome. Circulation. Cardiovascular genetics 5, 519–528, https://doi.org/10.1161/CIRCGENETICS.112.963785 (2012).
Walsh, R. et al. Reassessment of Mendelian gene pathogenicity using 7,855 cardiomyopathy cases and 60,706 reference samples. Genet Med 19, 192–203, https://doi.org/10.1038/gim.2016.90 (2017).
Buske, O. J. et al. PhenomeCentral: a portal for phenotypic and genotypic matchmaking of patients with rare genetic diseases. Hum Mutat 36, 931–940, https://doi.org/10.1002/humu.22851 (2015).
Acknowledgements
APL is supported by the National Institutes of Health K08-HL136839 and L40-HL129273, the Pediatric and Congenital Electrophysiology Society Paul C. Gillette Award, pilot grant funding from the Baylor College of Medicine Department of Pediatrics, and the McCrae Foundation. XHTW is supported by NIH grants R01-HL089598, R01-HL091947, and R01-HL117641, and American Heart Association grant 13EIA14560061.
Author information
Authors and Affiliations
Contributions
E.G.J. and A.P.L. conducted the cohort-based genetic studies. N.M., R.M., M.Z., T.S., A.S., G.S., Y.J. and H.G. conduct genetic analyses of the G.M.E. cohort and families and abstracted clinical data. N.M., R.M., H.D.A., H.G. and A.P.L. were responsible for acquiring respective institutional IRB approval and obtaining informed consent when not waived. H.D.A. and X.H.T.W. provided expert contextualization of findings and advice on analysis. E.G.J., N.M. and R.M. drafted the paper and prepared the figures. E.G.J., N.M., R.M., M.Z., T.S., A.S., G.S., Y.J., H.D.A., X.H.T.W., H.G. and A.P.L. revised and approved the paper. H.G. and A.P.L. assumed responsibility for (1) ensuring that original data upon which the submission is based is preserved and retrievable for reanalysis; (2) approving data presentation as representative of the original data; and (3) foreseeing and minimizing obstacles to the sharing of data, materials, algorithms or reagents described in the work.
Corresponding authors
Ethics declarations
Competing Interests
XHTW is a founding partner of Elex Biotech, a start-up company that developed drug molecules that target ryanodine receptors for the treatment of cardiac arrhythmia disorders. All other offers declare no potential conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jones, E.G., Mazaheri, N., Maroofian, R. et al. Analysis of enriched rare variants in JPH2-encoded junctophilin-2 among Greater Middle Eastern individuals reveals a novel homozygous variant associated with neonatal dilated cardiomyopathy. Sci Rep 9, 9038 (2019). https://doi.org/10.1038/s41598-019-44987-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-44987-6
This article is cited by
-
Exploring the complex spectrum of dominance and recessiveness in genetic cardiomyopathies
Nature Cardiovascular Research (2023)
-
Biallelic loss of LDB3 leads to a lethal pediatric dilated cardiomyopathy
European Journal of Human Genetics (2023)
-
T-tubule remodeling in human hypertrophic cardiomyopathy
Journal of Muscle Research and Cell Motility (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.