Abstract
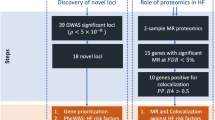
Tryptophan is an essential amino acid. Indoleamine 2,3-dioxygenase (IDO), the rate-limiting enzyme in the tryptophan-kynurenine pathway, is positively associated with cardiac events, and may be relevant to cancer. We used Mendelian Randomization to obtain unconfounded estimates of the association of IDO1 with ischemic heart disease (IHD), ischemic stroke and their risk factors, all-cancer, cancer of the prostate, lung and bronchus, and breast. We obtained genetic instruments independently and strongly (p-value < 5 × 10−8) predicting plasma IDO1 from a proteome genome-wide association study (GWAS), and applied them to consortia GWAS of the outcomes, including the UK Biobank SOFT CAD GWAS (cases < = 76 014, non-cases < = 264 785) for IHD. Estimates were obtained using inverse variance weighting; with MR-Egger, weighted median and MR-PRESSO as sensitivity analyses. IDO1 was inversely associated with IHD (odds ratio (OR) 0.96 per standard deviation, 95% confidence interval (CI) 0.93 to 1.00, p-value = 0.04), diabetes (OR 0.91, 95% CI 0.85 to 0.97) and prostate cancer (OR 0.96, 95% CI 0.93 to 0.99) with a directionally consistent estimate for stroke (OR 0.98, 95% CI 0.95 to 1.02) but not with blood pressure, or the other cancers considered. IDO1 might be a potential therapeutic target for IHD, diabetes and prostate cancer.
Similar content being viewed by others
Introduction
Tryptophan is an essential amino acid in humans that must be obtained from the diet, and is widely consumed in protein-based foods1, such as milk2, soy products and egg white3. More than 90% of dietary tryptophan, is catabolized via the kynurenine pathway4. Indoleamine 2,3-dioxygenase (IDO), one of the rate-limiting enzymes in the first step of the tryptophan-kynurenine pathway, may control the pathway under pathological conditions5 and have immunomodulatory5,6 and signaling functions7. IDO has two isoforms, IDO1 and IDO2, of which IDO1 is the major one controlling tryptophan degradation8. Kynurenine further degrades via different pathways (Supplementary Figure 1). Kynurenine--oxoglutarate transaminase (KAT), which has 4 isoforms (1–4), is responsible for degrading kynurenine to kynurenic acid9.
Despite considerable progress in the prevention of non-communicable diseases, such as cardiovascular diseases, ischemic heart disease (IHD) is still the leading cause of mortality and morbidity worldwide10. Investigating new prevention and treatment approaches is crucial. The tryptophan-kynurenine pathway is thought to be involved in the pathology of IHD and its risk factors including diabetes, obesity and immune-related diseases11. In most observational studies, IDO activity (measured as the kynurenine/tryptophan ratio) is positively associated with early atherosclerosis12 and IHD13, and correspondingly is inversely associated with prognosis in stroke patients14. However, in most animal experiments, inhibition of IDO or IDO deficiency in mice leads to early atherosclerosis and plaque instability15,16, although one study showed an inverse association of IDO1 deficiency with the risk of atherosclerosis17. IDO induction also exerts protective effects against atherosclerosis in mice18,19,20. These effects could be due to IDO1-dependent effects on lipid metabolism and inflammation16. More holistically, IHD is increasingly being considered within the well-established evolutionary theory that growth and reproduction trade-off against longevity21, gonadotropin-releasing hormone increases risk of IHD22. IDO activation might result in lower serotonin in the brain23, which may decrease gonadotropin-releasing hormone synthesis24 and secretion25. Notably, IDO1 inhibitors are under development as a cancer treatment, raising the possibility of re-purposing. However, no randomized controlled trials of IDO or IDO inhibitors to prevent or treat IHD have been conducted. Similarly, effects of KAT3 on IHD have rarely been studied, but its catabolite kynurenic acid might support the cardiovascular system by protecting the endothelium during hyperhomocysteinemia26.
Inconsistencies between observational studies and animal experiments may be due to the difficulty of eliminating confounding and distinguishing between causes and biomarkers of disease in observational studies, as well as differences in metabolism between humans and mice. In this situation, Mendelian Randomization (MR), as instrumental variable analysis with genetic instruments, may provide insight. Since the randomization of genetic makeup at conception is in some ways similar to the randomization process in randomized controlled trials27, MR provides unconfounded estimates of causal effects. Given tryptophan is a common dietary item28, we conducted an MR study to investigate the association of IDO1, and KAT3 for completeness, with IHD, ischemic stroke and their risk factors, including type 2 diabetes and blood pressure, using the largest available genetic consortia. Moreover, IDO inhibitors are being considered in cancer given their immunomodulatory property that prevents immune escape of cancer cells29 but a recent trial cast doubt on their effects on cancer30. For completeness we also assessed the association of IDO1 and KAT3 with all-cancer and common cancers including prostate, lung and bronchus, and breast cancer.
Results
The F statistic for the single nucleotide polymorphisms (SNPs) available in the analyses predicting plasma IDO1 at 5 × 10−8 was 155.3, while in sensitivity analyses at 5 × 10−6 it was 72.3. The F statistic for the SNPs predicting plasma KAT3 available in the analyses at 5 × 10−8 was 68.7, while in sensitivity analyses at 5 × 10−6 it was 29.2. This study had at least 80% power at 5% α to detect an odds ratio of 0.97 for IHD per standard deviation of IDO1. The results of power calculations for all the outcomes are available in Supplementary Table 1. For the SNPs available on the GTEx Portal, we found the tissues where the instruments were expressed were consistent with IDO1 and KAT3 expression. For example, the instruments predicting IDO1 are expressed in blood, esophagus and skin (Supplementary Table 2), in which IDO1 protein is expressed.
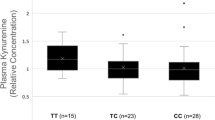
Associations of genetically predicted IDO1 and KAT3 with IHD and stroke
Table 1 shows genetically instrumented IDO1 was inversely associated with IHD but not ischemic stroke using inverse variance weighting (IVW) with directionally consistent estimates using weighted median (WM) at 5 × 10−8. MR-Egger did not show potentially pleiotropic effects. Sensitivity analyses at 5 × 10−6 gave similar results. Table 1 also shows that genetically instrumented KAT3 was not clearly associated with IHD or ischemic stroke using IVW at 5 × 10−8. However, in sensitivity analysis at 5 × 10−6 KAT3 was inversely associated with IHD but not with ischemic stroke using IVW, with a directionally consistent WM estimate. After removing 2 potentially pleiotropic SNPs related to systolic blood pressure and fat mass, identified from PhenoScanner, the association was not evident using IVW or any other method.
Associations of genetically predicted IDO1 and KAT3 with type 2 diabetes
Table 2 shows that genetically instrumented IDO1 was inversely associated with type 2 diabetes using IVW with WM giving similar results at 5 × 10−8. MR-Egger did not show potentially pleiotropic effects. Sensitivity analyses at 5 × 10−6 gave similar results. Table 2 also shows that genetically instrumented KAT3 was inversely associated with type 2 diabetes using IVW at 5 × 10−8. However, at 5 × 10−6 the associations were not evident using IVW or any other method.
Associations of genetically predicted IDO1 and KAT3 with systolic blood pressure and diastolic blood pressure
Table 3 shows genetically instrumented IDO1 was not clearly associated with systolic or diastolic blood pressure using IVW or any other method. At 5 × 10−8, KAT3 was inversely associated with systolic blood pressure but not with diastolic blood pressure using IVW, but in sensitivity analyses at 5 × 10−6 these associations were not evident.
Associations of genetically predicted IDO1 and KAT3 with cancers
Tables 4 and 5 show that genetically instrumented IDO1 was inversely associated with prostate cancer using IVW and WM with directionally consistent estimates in MR-Egger but not with all-cancer, lung and bronchus or breast cancer at 5 × 10−8. KAT3 was not clearly associated with any-cancer, prostate, lung and bronchus or breast cancer using IVW or any other method at 5 × 10−8. Sensitivity analyses at 5 × 10−6 gave similar results.
Discussion
Consistent with previous animal experiments15,16 suggesting IDO is protective against atherosclerosis, this MR study showed that plasma IDO1 protein was inversely associated with IHD. We also showed that IDO1 and KAT3 were inversely associated with type 2 diabetes which has rarely been studied previously. We could not rule out the possibility that KAT3 was inversely associated with IHD and systolic blood pressure. We also found IDO1 inversely associated with prostate cancer but not other cancers considered.
An abnormal kynurenine pathway has been observed in atherosclerosis11, which is important in the development of IHD and is also an important therapeutic target to prevent IHD. In mice IDO inhibition by 1-methyl tryptophan (an IDO inhibitor) enhanced vascular inflammation by immune dysregulation, and thus increased atherosclerotic lesions16. IDO deficiency in mice accelerated early atherosclerosis by dysregulation of cytokine IL-1015. These experiments indicate that IDO1 could be protective against atherosclerosis possibly by an immune-inflammatory response.
In this MR study, we provide genetic validation of the potential role of IDO1 in IHD, by showing that life-long increased plasma IDO1 was inversely associated with risk of developing IHD. Although the association was not significant for ischemic stroke possibly because of lack of power and selection bias, the direction of the estimate was consistent with that of IHD, which gives some validation of our findings for IHD. However, this is not consistent with most observational studies in older people12,13 or in patients with cardiac events14,31, which show IDO activity (kynurenine/tryptophan ratio) positively associated with coronary events and cardiovascular risk factors. However, the kynurenine/tryptophan ratio is not a direct measure of IDO1. On the one hand, it may mainly reflect the enzymatic function of IDO1 or the effects of its catabolite kynurenine more than the complicated function of IDO1. On the other hand, not only IDO1 but also IDO2 and tryptophan 2,3-dioxygenase can affect this ratio11. In addition, studies of a fatal disease in older people are open to selection bias, which can generate reversed estimates32, as are studies in patients, as well as to unmeasured confounding. In addition, IDO can be induced by inflammation related cytokines7,33; the associations between IDO activity and intima-media thickness did not hold after adjustment for traditional risk factors12,34. As such, IHD might increase IDO activity as a negative feedback loop to protect against over-reaction by the immune system. However, we could not conduct an adequately powered bi-directional MR study because of the relatively small sample size of the genome-wide association study (GWAS) for IDO1.
Unexpectedly, we also found that IDO1 was protective against type 2 diabetes. Type 2 diabetes causes IHD35. Preventing diabetes might be a pathway by which IDO1 lowers the risk of IHD. Previous studies of IDO1 and type 2 diabetes are limited, although some have suggested diabetes up-regulates the tryptophan-kynurenine pathway36,37. Given IDO1 has complex and multiple functionality7,38, its effects on type 2 diabetes as well as the underlying mechanism, such as via insulin given products of the kynurenine pathway inhibit the synthesis and activity of insulin39, needs further investigation. Unexpectedly, we also found KAT3 might be protective against diabetes and high systolic blood pressure but not IHD. These associations were not evident in sensitivity analysis at 5 × 10−6 so these findings need further confirmation. How these findings relate to our recent findings that other specific kynurenine related factors, i.e., aspartate but not glutamate, protect against IHD40, also needs to be considered.
Given IDO’s immunosuppressive function, IDO inhibitors have been considered for cancer treatment, and have passed phase 141 and phase 242 trials. However, recently a pivotal trial of an IDO inhibitor failed to accomplish its primary and secondary outcome in treating melanoma, casting doubt on its efficacy for treating cancer30. In this MR study, we also found that IDO1 was not associated with most cancers considered, consistent with this latest trial. However, we found IDO1 was protective against prostate cancer, which is rarely studied, although one study suggested it as a biomarker for prostate cancer43.
This MR study made full use of the largest publicly available GWAS giving adequate power, while avoided the confounding that may affect conventional observational studies. However, some limitations still exist. First, in MR studies, weak instruments could bias the association towards the null. We used genetic predictors associated with exposures at genome-wide significance (5 × 10−8), and used a less stringent cut off 5 × 10−6 for sensitivity analysis. One SNP rs7010461 (IDO1 gene) is functionally associated with IDO1 with a small p-value of 2.45 × 10−20, and was not associated with IHD, diabetes, systolic and diastolic blood pressure or cancer at genome-wide significance. Larger F statistics indicate lower probability of weak instrument bias with a conventional threshold of 1044, and the F statistics were all larger than 10 in this study. Second, we were not able to assess the association of genetic predictors with a wide range of unknown confounders, but none of the SNPs used was associated with known confounders including age of completing education, current tobacco smoking, alcohol intake frequency, walking frequency and prescription of anti-depressants at Bonferroni corrected significance. Third, we could not rule out the possibility of horizontal pleiotropy. However, we used different methods with different assumptions to detect potential horizontal pleiotropy statistically, including MR-PRESSO. We also checked for known pleiotropy and removed such SNPs in a sensitivity analysis. Fourth, although MR is less susceptible to confounding, it can be confounded by ethnicity, i.e., population stratification. We used GWAS with participants mainly of European ancestry with genomic control10,45,46,47,48,49,50,51. Fifth, we were not able to confirm whether associations varied by baseline levels of IDO1. Sixth, since IDO1 could affect the cardiovascular system via several different pathways, the associations could be non-linear but we assumed it was linear. Seventh, we did not pre-specify exhaustively what we considered pleiotropic effects, potentially adding some subjectivity to the assessment of known pleiotropy. Eighth, we did multiple testing for different outcomes here, which may increase type I error, i.e., false positives52. However, in our hypothesis IHD was the primary outcome in this study, and other outcomes such as traditional risk factors of IHD were mainly used for further investigation of potential pathways. Ninth, IDO and KAT have different isoforms, but here we only studied the effects of IDO1 and KAT3 due to data availability. However, IDO1 is the major isoform responsible for tryptophan degradation to kynurenine8, while KAT3 shares high similarity with KAT1 and may also relate to glutamine and histidine53. Finally, MR estimates are vulnerable to selection bias in the underlying GWAS, here CARDIoGRAMplusC4D and DIAGRAM. However, CARDIoGRAMplusC4D shows the expected associations for PCSK9 and HMGCR genetic variants54, while GWAS of less-fatal conditions such as diabetes are less vulnerable to selection bias.
Conclusions
Consistent with animal experiments and evolutionary biology, we obtained genetic validation of plasma IDO1 protein as protecting against IHD, with directionally consistent results for stroke. Unexpectedly, both IDO1 and KAT3 were inversely associated with type 2 diabetes, suggesting the kynurenine pathway also plays a role in development of diabetes. Consistent with evolutionary biology, we also found IDO1 was also protective against prostate cancer. Given the complex function of IDO1 and wide consumption of the essential amino acid tryptophan in our diets, IDO1 could be a potential target for IHD, diabetes and prostate cancer prevention worthy of further investigation. Intervening on IDO1 such as modifying iron intake55, might help to prevent IHD56 and diabetes.
Methods
Genetic associations with exposures: IDO1 and KAT3
SNPs strongly associated with IDO1 and KAT3 proteins (p-value < 5 × 10−8) were obtained from the most recent plasma proteome GWAS in 3301 healthy participants of European descent (mean age 43.7 years, 51.1% men), adjusted for age, sex, duration between blood draw and processing and the first three principal components of ancestry from multi-dimensional scaling45. SNPs associated with these enzymes at a less stringent significance level (5 × 10−6) were used in sensitivity analyses. We selected uncorrelated SNPs (r2 < 0.05) with a smaller p-value based on the 1000 Genomes catalog57. SNPs that were not available for an outcome were replaced by proxies. Potentially palindromic SNPs (A/T or C/G) were also replaced by proxies where available, because SNP-specific effect allele frequency was not given for the proteome study.
Four independent SNPs (r2 < 0.05) predicted IDO1 at p-value < 5 × 10−8 but rs8110965 was potentially palindromic and had no proxy (r2 > 0.6) (Supplementary Tables 3 and 4). Nine independent SNPs predicted IDO1 at p-value < 5 × 10−6, rs75781101 was proxied by rs17817660 (r2 = 1.0) for all outcomes but rs8110965 had no proxy (r2 > 0.6) (Supplementary Tables 3 and 4).
Only two independent SNPs predicted KAT3 at p-value < 5 × 10−8, rs9787133 was proxied by rs7539070 (r2 = 0.96) for all outcomes (Supplementary Tables 5 and 6). Sixteen independent SNPs predicted KAT3 at p-value < 5 × 10−6. Among these SNPs, three SNPs were replaced by proxies for IHD, ischemic stroke and diabetes, two for blood pressure, all-cancer, prostate cancer and breast cancer, and four for lung and bronchus cancer, but no proxy for some SNPs, such as rs12935125, was available (Supplementary Tables 5 and 6).
Genetic associations with the outcomes: IHD, its risk factors including type 2 diabetes and blood pressure, as well as cancers
Genetic associations with IHD were obtained from the most up to date and largest GWAS in the CARDIoGRAMplusC4D consortium, which is a meta-analysis of the UK Biobank SOFT CAD GWAS with studies from the CARDIoGRAMplusC4D consortium10. The UK Biobank SOFT CAD GWAS was adjusted for array and the first five principal components10. The final GWAS included up to 76 014 cases and 264 785 non-cases mainly of European descent, with double-genomic-control. Genetic associations with ischemic stroke were obtained from the MEGASTROKE consortium, which meta-analysed 29 GWASs mainly of Europeans. The final study included 60341 ischemic stroke cases and 454450 controls51. Genetic associations with type 2 diabetes were from the Stage 1 Summary statistics of the DIAGRAM 1000 Genomes GWAS meta-analysis which combined 18 GWASs. The GWAS included 26 676 cases and 132 532 controls mainly of European ancestry, adjusted for age, sex and principal components of ancestry46. Genetic associations with automated-reading systolic and diastolic blood pressure (standard deviation) were from the Neale Lab UK Biobank summary statistics (n = 340 159 for systolic blood pressure, n = 340 162 for diastolic blood pressure) mainly of people of white British ancestry, adjusted for the first 20 principal components, age, age2, sex, age*sex and age2*sex47. The UK Biobank is a large cohort comprising ~500 000 individuals from the UK, aged 40–69 years at recruitment47. Genetic associations with self-reported diagnosis of any cancer were from the same source of summary statistics similarly adjusted (cases = 28 509, controls = 331 472)47. Genetic associations with prostate cancer were obtained from the largest available meta-analyses of summary statistics in the PRACTICAL consortium. The GWAS includes 79148 prostate cancer cases and 61106 controls of European ancestry, adjusted for principal components48. Genetic associations with lung and bronchus cancer were from UK-Biobank Single Variant Association Analysis Results using SAIGE, which includes 2101 cases and 406226 controls of white British ancestry adjusted for the first four principal components, sex, and birth year49. Genetic associations with breast cancer were obtained from the BCAC consortium, which includes 122977 cases and 105974 controls of European ancestry, adjusted for principle components and sometimes additionally adjusted for country and study50. A comprehensive description of the sources of the genetic associations is presented in Supplementary Table 7.
Statistical analysis
We calculated the F statistics for all the instruments combined using an approximation, i.e., average of the estimated SNP specific F statistics (square of beta for SNP to exposure/square of its variance)58. We identified any genetic instruments associated at Bonferroni-corrected significance with potential confounders including age of completing education, current tobacco smoking, alcohol intake frequency, walking frequency and prescription of anti-depressants in the UK Biobank summary statistics47. Whether the genetic instruments are linked to the outcomes directly rather than through the exposures (pleiotropic effects) was assessed by checking their known phenotypes obtained from comprehensive curated genotype to phenotype cross-references, i.e., PhenoScanner (http://www.phenoscanner.medschl.cam.ac.uk/) and the GWAS Catalog (https://www.ebi.ac.uk/gwas/). Power was calculated for each outcome59, on the basis that the sample size for instrumental variable analysis is the sample size for regression of exposure on outcome divided by the r2 for instrument on exposure60. To further validate the SNPs we used, we checked the genotype tissue expression data using the GTEx Portal (https://gtexportal.org/home/) where available. Since IDO1 is expressed by dendritic cells61 which are present in the skin62, lungs61, stomach63, intestines61, blood and lymph nodes61, and KAT3 is expressed widely including in the skin, gastrointestinal tract and lungs64,65, we checked whether the instruments were expressed in these tissues.
Estimates of the associations of IDO1 and KAT3 with IHD, ischemic stroke, type 2 diabetes, blood pressure (systolic and diastolic) and cancers were obtained by meta-analysing the SNP-specific Wald estimates (ratio of SNP on outcome to SNP on exposure) using IVW with multiplicative random effects for 4+ SNPs and fixed effects for <4 SNPs66. IVW with random effects assumes balanced pleiotropy (i.e., the mean of the horizontal pleiotropic effect is zero so does not bias the estimate)67 while IVW with fixed effects assumes all SNPs are valid instruments66. We used sensitivity analyses with different assumptions to check the robustness of the IVW estimates. WM gives reliable estimates when over 50% of the weight is contributed by valid instruments68. MR-Egger and MR-PRESSO (Mendelian randomization pleiotropy residual sum and outlier) are used to test directional (unbalanced) pleiotropy. MR-Egger allows invalid instruments and is robust to pleiotropy assuming the instrument strength is independent of direct effect58. A non-null MR-Egger intercept indicates directional pleiotropy and a less reliable IVW estimate58. MR-Egger has low power and does not identify pleiotropic SNPs. MR-PRESSO detects potentially pleiotropic SNPs based on the residual sum of squares and corrects for them by removing statistically significant outliers69. We reported the corrected MR-PRESSO estimate if given otherwise the raw estimate. All statistical analyses were conducted using R version 3.5.0 (The R Foundation for Statistical Computing, Vienna, Austria). The MR-Base (TwoSampleMR) R package was used for selecting uncorrelated SNPs and aligning effect alleles, MendelianRandomization and the MRPRESSO R packages were used to obtain estimates. All the data were publicly available and thus no ethical approval was required for this study.
Ethics approval and consent to participant
All the data were publicly available and no individual data were used. Therefore, no ethical approval and consent was required for this study.
Data Availability
All data generated or analysed during this study are included in this article (and its Supplementary Files).
References
Strasser, B., Gostner, J. M. & Fuchs, D. Mood, food, and cognition: role of tryptophan and serotonin. Curr Opin Clin Nutr Metab Care. 19, 55–61, https://doi.org/10.1097/mco.0000000000000237 (2016).
Nongonierma, A. B. & FitzGerald, R. J. Milk proteins as a source of tryptophan-containing bioactive peptides. Food Funct. 6, 2115–2127, https://doi.org/10.1039/c5fo00407a (2015).
Lindseth, G., Helland, B. & Caspers, J. The effects of dietary tryptophan on affective disorders. Arch Psychiatr Nurs. 29, 102–107, https://doi.org/10.1016/j.apnu.2014.11.008 (2015).
Polyzos, K. A. & Ketelhuth, D. F. The role of the kynurenine pathway of tryptophan metabolism in cardiovascular disease. An emerging field. Hamostaseologie. 35, 128–136, https://doi.org/10.5482/hamo-14-10-0052 (2015).
Larkin, P. B. et al. Tryptophan 2,3-dioxygenase and indoleamine 2,3-dioxygenase 1 make separate, tissue-specific contributions to basal and inflammation-induced kynurenine pathway metabolism in mice. Biochim Biophys Acta. 1860, 2345–2354, https://doi.org/10.1016/j.bbagen.2016.07.002 (2016).
Munn, D. H. & Mellor, A. L. Indoleamine 2,3 dioxygenase and metabolic control of immune responses. Trends Immunol. 34, 137–143, https://doi.org/10.1016/j.it.2012.10.001 (2013).
Fallarino, F., Grohmann, U. & Puccetti, P. Indoleamine 2,3-dioxygenase: from catalyst to signaling function. Eur J Immunol. 42, 1932–1937, https://doi.org/10.1002/eji.201242572 (2012).
Lob, S. et al. IDO1 and IDO2 are expressed in human tumors: levo- but not dextro-1-methyl tryptophan inhibits tryptophan catabolism. Cancer Immunol Immunother. 58, 153–157, https://doi.org/10.1007/s00262-008-0513-6 (2009).
Maes, M., Galecki, P., Verkerk, R. & Rief, W. Somatization, but not depression, is characterized by disorders in the tryptophan catabolite (TRYCAT) pathway, indicating increased indoleamine 2,3-dioxygenase and lowered kynurenine aminotransferase activity. Neuro Endocrinol Lett. 32, 264–273 (2011).
Nelson, C. P. et al. Association analyses based on false discovery rate implicate new loci for coronary artery disease. Nat Genet. 49, 1385–1391, https://doi.org/10.1038/ng.3913 (2017).
Song, P., Ramprasath, T., Wang, H. & Zou, M. H. Abnormal kynurenine pathway of tryptophan catabolism in cardiovascular diseases. Cell Mol Life Sci. 74, 2899–2916, https://doi.org/10.1007/s00018-017-2504-2 (2017).
Niinisalo, P. et al. Indoleamine 2,3-dioxygenase activity associates with cardiovascular risk factors: the Health 2000 study. Scand J Clin Lab Invest. 68, 767–770, https://doi.org/10.1080/00365510802245685 (2008).
Sulo, G. et al. Neopterin and kynurenine-tryptophan ratio as predictors of coronary events in older adults, the Hordaland Health Study. Int J Cardiol. 168, 1435–1440, https://doi.org/10.1016/j.ijcard.2012.12.090 (2013).
Brouns, R. et al. The role of tryptophan catabolism along the kynurenine pathway in acute ischemic stroke. Neurochem Res. 35, 1315–1322, https://doi.org/10.1007/s11064-010-0187-2 (2010).
Cole, J. E. et al. Indoleamine 2,3-dioxygenase-1 is protective in atherosclerosis and its metabolites provide new opportunities for drug development. Proc Natl Acad Sci USA 112, 13033–13038, https://doi.org/10.1073/pnas.1517820112 (2015).
Polyzos, K. A. et al. Inhibition of indoleamine 2,3-dioxygenase promotes vascular inflammation and increases atherosclerosis in Apoe−/− mice. Cardiovasc Res. 106, 295–302, https://doi.org/10.1093/cvr/cvv100 (2015).
Metghalchi, S. et al. Indoleamine 2,3-Dioxygenase Fine-Tunes Immune Homeostasis in Atherosclerosis and Colitis through Repression of Interleukin-10 Production. Cell Metab. 22, 460–471, https://doi.org/10.1016/j.cmet.2015.07.004 (2015).
Forteza, M. J. et al. Activation of the Regulatory T-Cell/Indoleamine 2,3-Dioxygenase Axis Reduces Vascular Inflammation and Atherosclerosis in Hyperlipidemic Mice. Frontiers in immunology. 9, 950–950, https://doi.org/10.3389/fimmu.2018.00950 (2018).
Daissormont, I. T. et al. Plasmacytoid dendritic cells protect against atherosclerosis by tuning T-cell proliferation and activity. Circ Res. 109, 1387–1395, https://doi.org/10.1161/circresaha.111.256529 (2011).
Yun, T. J. et al. Indoleamine 2,3-Dioxygenase-Expressing Aortic Plasmacytoid Dendritic Cells Protect against Atherosclerosis by Induction of Regulatory T Cells. Cell Metab. 23, 852–866, https://doi.org/10.1016/j.cmet.2016.04.010 (2016).
Schooling, C. M. Tachykinin neurokinin 3 receptor antagonists: a new treatment for cardiovascular disease? Lancet. 390, 709–711, https://doi.org/10.1016/s0140-6736(16)31648-8 (2017).
Schooling, C. M. & Ng, J. C. M. Reproduction and longevity: A Mendelian randomization study of gonadotropin-releasing hormone and ischemic heart disease. SSM - Popul Health. in press (2019).
Elovainio, M. et al. Indoleamine 2,3-dioxygenase activation and depressive symptoms: results from the Young Finns Study. Psychosom Med. 74, 675–681, https://doi.org/10.1097/PSY.0b013e318266d0f5 (2012).
Prasad, P., Ogawa, S. & Parhar, I. S. Serotonin reuptake inhibitor citalopram inhibits GnRH synthesis and spermatogenesis in the male zebrafish. Biol Reprod. 93, 102, https://doi.org/10.1095/biolreprod.115.129965 (2015).
Kim, H. S. et al. Serotonin stimulates GnRH secretion through the c-Src-PLC gamma1 pathway in GT1-7 hypothalamic cells. J Endocrinol. 190, 581–591, https://doi.org/10.1677/joe.1.06727 (2006).
Wejksza, K., Rzeski, W. & Turski, W. A. Kynurenic acid protects against the homocysteine-induced impairment of endothelial cells. Pharmacol Rep. 61, 751–756 (2009).
Emdin, C. A., Khera, A. V. & Kathiresan, S. Mendelian Randomization. Jama. 318, 1925–1926, https://doi.org/10.1001/jama.2017.17219 (2017).
Fukushige, H. et al. Effects of tryptophan-rich breakfast and light exposure during the daytime on melatonin secretion at night. J Physiol Anthropol. 33, 33, https://doi.org/10.1186/1880-6805-33-33 (2014).
Liu, X. et al. Selective inhibition of IDO1 effectively regulates mediators of antitumor immunity. Blood. 115, 3520–3530, https://doi.org/10.1182/blood-2009-09-246124 (2010).
Genetic Engineering & Biotechnology News. Incyte, Merck & Co. Halt Phase III Trial After Epacadostat/Keytruda Combination Fails in Melanoma. Available from: https://www.genengnews.com/topics/drug-discovery/incyte-merck-co-halt-phase-iii-trial-after-epacadostat-keytruda-combination-fails-in-melanoma/ (2018).
Pedersen, E. R. et al. Urinary excretion of kynurenine and tryptophan, cardiovascular events, and mortality after elective coronary angiography. Eur Heart J. 34, 2689–2696, https://doi.org/10.1093/eurheartj/eht264 (2013).
Hernan, M. A., Alonso, A. & Logroscino, G. Cigarette smoking and dementia: potential selection bias in the elderly. Epidemiology. 19, 448–450, https://doi.org/10.1097/EDE.0b013e31816bbe14 (2008).
Baumgartner, R., Forteza M. J. & Ketelhuth D. F. J. The interplay between cytokines and the Kynurenine pathway in inflammation and atherosclerosis. Cytokine., https://doi.org/10.1016/j.cyto.2017.09.004 (2017).
Pertovaara, M. et al. Indoleamine 2,3-dioxygenase enzyme activity correlates with risk factors for atherosclerosis: the Cardiovascular Risk in Young Finns Study. Clinical and experimental immunology. 148, 106–111, https://doi.org/10.1111/j.1365-2249.2007.03325.x (2007).
Au Yeung, S. L., Luo, S. & Schooling, C. M. The Impact of Glycated Hemoglobin (HbA1c) on Cardiovascular Disease Risk: A Mendelian Randomization Study Using UK Biobank. Diabetes Care. 41, 1991–1997, https://doi.org/10.2337/dc18-0289 (2018).
Rebnord, E. W. et al. The kynurenine:tryptophan ratio as a predictor of incident type 2 diabetes mellitus in individuals with coronary artery disease. Diabetologia. 60, 1712–1721, https://doi.org/10.1007/s00125-017-4329-9 (2017).
Oxenkrug, G. F. Increased plasma levels of xanthurenic and kynurenic acids in type 2 diabetes. Molecular neurobiology. 52, 805–810, https://doi.org/10.1007/s12035-015-9232-0 (2015).
Chen, W. IDO: more than an enzyme. Nat Immunol. 12, 809–811, https://doi.org/10.1038/ni.2088 (2011).
Stone, T. W. & Darlington, L. G. Endogenous kynurenines as targets for drug discovery and development. Nat Rev Drug Discov. 1, 609–620, https://doi.org/10.1038/nrd870 (2002).
Zhao, J. V., Kwok M. K. & Schooling C. M. Effect of glutamate and aspartate on ischemic heart disease, blood pressure and diabetes: a Mendelian randomization study. American Journal of Clinical Nutrition; in press.
Soliman, H. H. et al. A phase I study of indoximod in patients with advanced malignancies. Oncotarget. 7, 22928–22938, https://doi.org/10.18632/oncotarget.8216 (2016).
Kristeleit, R. et al. A randomised, open-label, phase 2 study of the IDO1 inhibitor epacadostat (INCB024360) versus tamoxifen as therapy for biochemically recurrent (CA-125 relapse)-only epithelial ovarian cancer, primary peritoneal carcinoma, or fallopian tube cancer. Gynecol Oncol. 146, 484–490, https://doi.org/10.1016/j.ygyno.2017.07.005 (2017).
Banzola, I. et al. Expression of Indoleamine 2,3-Dioxygenase Induced by IFN-γ and TNF-α as Potential Biomarker of Prostate Cancer Progression. Frontiers in immunology. 9, 1051–1051, https://doi.org/10.3389/fimmu.2018.01051 (2018).
Burgess, S. & Thompson, S. G. Avoiding bias from weak instruments in Mendelian randomization studies. Int J Epidemiol. 40, 755–764, https://doi.org/10.1093/ije/dyr036 (2011).
Sun, B. B. et al. Genomic atlas of the human plasma proteome. Nature. 558, 73–79, https://doi.org/10.1038/s41586-018-0175-2 (2018).
Scott, R. A. et al. An Expanded Genome-Wide Association Study of Type 2 Diabetes in Europeans. Diabetes. 66, 2888–2902, https://doi.org/10.2337/db16-1253 (2017).
Neale, B. et al. UK Biobank GWAS results, Available from: http://www.nealelab.is/uk-biobank/ (2018).
Schumacher, F. R. et al. Association analyses of more than 140,000 men identify 63 new prostate cancer susceptibility loci. Nature Genetics. 50, 928–936, https://doi.org/10.1038/s41588-018-0142-8 (2018).
Zhou, W. et al. Efficiently controlling for case-control imbalance and sample relatedness in large-scale genetic association studies. Nature Genetics. 50, 1335–1341, https://doi.org/10.1038/s41588-018-0184-y (2018).
Michailidou, K. et al. Association analysis identifies 65 new breast cancer risk loci. Nature. 551, 92–94, https://doi.org/10.1038/nature24284 (2017).
Malik, R. et al. Multiancestry genome-wide association study of 520,000 subjects identifies 32 loci associated with stroke and stroke subtypes. Nat Genet. 50, 524–537, https://doi.org/10.1038/s41588-018-0058-3 (2018).
Feise, R. J. Do multiple outcome measures require p-value adjustment? BMC medical research methodology. 2, 8–8, https://doi.org/10.1186/1471-2288-2-8 (2002).
Jayawickrama, G. S. et al. Kynurenine Aminotransferases and the Prospects of Inhibitors for the Treatment of Schizophrenia. Curr Med Chem. 22, 2902–2918 (2015).
Schooling, C. M. et al. Disconnect Between Genes Associated With Ischemic Heart Disease and Targets of Ischemic Heart Disease Treatments. EBioMedicine. 28, 311–315, https://doi.org/10.1016/j.ebiom.2018.01.015 (2018).
Majewski, M., Kozlowska, A., Thoene, M., Lepiarczyk, E. & Grzegorzewski, W. J. Overview of the role of vitamins and minerals on the kynurenine pathway in health and disease. J Physiol Pharmacol. 67, 3–19 (2016).
Gill, D. et al. The Effect of Iron Status on Risk of Coronary Artery Disease: A Mendelian Randomization Study-Brief Report. Arterioscler Thromb Vasc Biol. 37, 1788–1792, https://doi.org/10.1161/atvbaha.117.309757 (2017).
Hemani, G. et al. MR-Base: a platform for systematic causal inference across the phenome using billions of genetic associations. bioRxiv, https://doi.org/10.1101/078972 (2016).
Bowden, J. et al. Assessing the suitability of summary data for two-sample Mendelian randomization analyses using MR-Egger regression: the role of the I2 statistic. International Journal of Epidemiology. 45, 1961–1974, https://doi.org/10.1093/ije/dyw220 (2016).
Brion, M. J., Shakhbazov, K. & Visscher, P. M. Calculating statistical power in Mendelian randomization studies. Int J Epidemiol. 42, 1497–1501, https://doi.org/10.1093/ije/dyt179 (2013).
Schooling, C. M., Freeman, G. & Cowling, B. J. Power and sample size calculations for Mendelian randomization studies using one genetic instrument. International Journal of Epidemiology. 42, 1157–1163, https://doi.org/10.1093/ije/dyt110 (2013).
Mellor, A. L. & Munn, D. H. IDO expression by dendritic cells: tolerance and tryptophan catabolism. Nat Rev Immunol. 4, 762–774, https://doi.org/10.1038/nri1457 (2004).
Scheler, M. et al. Indoleamine 2,3-dioxygenase (IDO): the antagonist of type I interferon-driven skin inflammation? Am J Pathol. 171, 1936–1943, https://doi.org/10.2353/ajpath.2007.070281 (2007).
Li, F. et al. The subsets of dendritic cells and memory T cells correspond to indoleamine 2,3-dioxygenase in stomach tumor microenvironment. Tumour Biol. 35, 8691–8698, https://doi.org/10.1007/s13277-014-2126-3 (2014).
Human Protein Atlas. Tissue expression of KYAT3-summary, Available from: https://www.proteinatlas.org/ENSG00000137944-KYAT3/tissue (2019).
Uhlen, M. et al. Proteomics. Tissue-based map of the human proteome. Science. 347, 1260419, https://doi.org/10.1126/science.1260419 (2015).
Burgess, S., Scott, R. A., Timpson, N. J., Davey Smith, G. & Thompson, S. G. Using published data in Mendelian randomization: a blueprint for efficient identification of causal risk factors. Eur J Epidemiol. 30, 543–552, https://doi.org/10.1007/s10654-015-0011-z (2015).
Hemani, G., Bowden, J. & Davey Smith, G. Evaluating the potential role of pleiotropy in Mendelian randomization studies. Hum Mol Genet. 27, R195–r208, https://doi.org/10.1093/hmg/ddy163 (2018).
Bowden, J., Davey Smith, G., Haycock, P. C. & Burgess, S. Consistent Estimation in Mendelian Randomization with Some Invalid Instruments Using a Weighted Median Estimator. Genet Epidemiol. 40, 304–314, https://doi.org/10.1002/gepi.21965 (2016).
Verbanck, M., Chen, C. Y., Neale, B. & Do, R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet. 50, 693–698, https://doi.org/10.1038/s41588-018-0099-7 (2018).
Acknowledgements
Data on coronary artery disease/myocardial infarction have been contributed by the CARDIoGRAMplusC4D and UK Biobank CardioMetabolic Consortium CHD working group who used the UK Biobank Resource (application number 9922). Data have been downloaded from www.CARDIOGRAMPLUSC4D.ORG. Data on ischemic stroke have been contributed by MEGASTROKE investigators. The MEGASTROKE project received funding from sources specified at http://www.megastroke.org/acknowledgments.html. Full list of MEGASTROKE authors is available in Appendix 1. Data on diabetes have been contributed by DIAGRAM investigators and have been downloaded from http://www.diagram-consortium.org. Data on blood pressure and all-cancer have been contributed by UK Biobank Ben Neale files and have been downloaded from http://www.nealelab.is/uk-biobank. Data on prostate cancer have been contributed by the PRACTICAL consortium, CRUK, BPC3, CAPS, PEGASUS. Full description is available in Appendix 1. Data on lung and bronchus cancer have been contributed by the UK Biobank SAIGE files and have been downloaded from https://www.leelabsg.org/resources. This research has been conducted using the UK Biobank Resource under application number 24460. Data on breast cancer have been contributed by the BCAC consortium. The breast cancer genome-wide association analyses were supported by the Government of Canada through Genome Canada and the Canadian Institutes of Health Research, the ‘Ministère de l’Économie, de la Science et de l’Innovation du Québec’ through Genome Québec and grant PSR-SIIRI-701, The National Institutes of Health (U19 CA148065, X01HG007492), Cancer Research UK (C1287/A10118, C1287/A16563, C1287/A10710) and The European Union (HEALTH-F2-2009-223175 and H2020 633784 and 634935). All studies and funders are listed in Michailidou et al. (2017). This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
M.L. and C.M.S. conceptualized ideas and designed the study; M.L. conducted the analysis and drafted the manuscript; C.M.S. directed the analytic strategy and supervised the study from conception to completion; M.K.K., C.M.S. and S.S.M.F. revised drafts of the manuscript. All the authors contributed to the interpretation of the data, critically revising the paper and approval of the final version.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, M., Kwok, M.K., Fong, S.S.M. et al. Indoleamine 2,3-dioxygenase and ischemic heart disease: a Mendelian Randomization study. Sci Rep 9, 8491 (2019). https://doi.org/10.1038/s41598-019-44819-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-44819-7
This article is cited by
-
Dysregulated cellular metabolism in atherosclerosis: mediators and therapeutic opportunities
Nature Metabolism (2024)
-
Comparison of moderate-intensity continuous training and high-intensity interval training effects on the Ido1-KYN-Ahr axis in the heart tissue of rats with occlusion of the left anterior descending artery
Scientific Reports (2023)
-
Systematic review of Mendelian randomization studies on risk of cancer
BMC Medicine (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.