Abstract
Amino acid derangements are common in severe falciparum malaria and have been associated with endothelial dysfunction (L-arginine), metabolic acidosis (alanine and lactate), and disease severity (phenylalanine and tryptophan metabolites). Whether these amino acid perturbations reflect isolated pathogenic mechanisms or if they are part of overall changes in amino acid metabolism is unclear. To investigate this, we prospectively simultaneously quantified a broad range of plasma free amino acids (PFAA) using HPLC-MRM-Mass spectrometry in relation to presenting symptoms in adults with severe malaria (n = 88), septicaemia (n = 88), uncomplicated malaria (n = 71), and healthy controls (n = 48) from Bangladesh. The total plasma concentration of measured amino acids was significantly reduced in each of the patient groups when compared to normal levels observed in healthy local controls: uncomplicated malaria −54%, severe malaria −23%, and sepsis −32%, (p = <0.001). Inspection of amino acid profiles revealed that in each group the majority of amino acids were below normal levels, except for phenylalanine. Among patients with severe malaria, L-lactate was strongly associated with an increase of the total amino acid concentration, likely because this reflects tissue hypoxia. Our data confirm previously described amino acid abnormalities, likely resulting from overall changes in the concentration of PFAA.
Similar content being viewed by others
Introduction
Severe malaria, caused by infection with Plasmodium falciparum, remains an important contributor to premature death in endemic countries1. The World Health Organisation estimated 445,000 patients died from malaria infection in 2016, predominantly in sub-Saharan Africa2. As parenteral artesunate is now established as the best drug to treat severe falciparum malaria3,4, further gains in reducing case fatality may be achieved by the development of adjunctive therapies. To develop new adjunctive therapies for severe malaria increased understanding is required of the underlying pathophysiology of life-threatening complications.
The pathophysiology of severe falciparum malaria is linked to derangements in amino acid metabolism. Key biochemical abnormalities in falciparum malaria consist of L-arginine deficiency, associated with endothelial dysfunction5,6, elevated L-lactate and alanine, associated with metabolic acidosis7,8, elevated phenylalanine9,10,11,12 and increased tryptophan metabolites13,14, both associated with disease severity, and low glutamine, a modulation of oxidative stress15. Besides these, there are multiple other amino acid abnormalities described previously, such as low ornithine, lysine, and histidine in cases with falciparum malaria10. Prior studies have described associations between specific amino acid derangements and clinical outcomes, and new adjunctive therapies are being developed to correct amino acid disorders. However, whether these amino acid derangements are isolated pathogenic mechanisms or if they are part of overall changes in amino acid metabolism is unclear.
The plasma concentration of free amino acids reflects a balance between tissue amino acid utilisation, and intestinal absorption, protein turnover, and de novo synthesis, which are under hormonal regulation and modulated by the bioavailability of cofactors and disease16. During critical illness, the circulating concentration of PFAA may be affected by an energy deficit, hypoxia, and underlying malnutrition17,18,19,20. An acute energy deficit can develop because of reduced intake (coma) and elevated energy requirements (infection), associated with increased hepatic extraction of amino acids from the bloodstream17,19,21. Tissue hypoxia increases cellular energy requirements because of incomplete anaerobic oxidation of glucose, and increases protein breakdown to allow amino acids to be converted to sugars or other energy substrates through oxidative deamination16. Underlying malnutrition may predispose and aggravate a negative energy balance20.
During malaria infection, Plasmodium falciparum parasites adhere to the vascular endothelium of the microcirculation, where they sequester and compromise microvascular blood flow. Patterns of an obstructed microcirculation in patients with severe falciparum malaria correlate strongly with hyperlactataemia22,23. Abnormal L-lactate-to-pyruvate ratios in malaria suggest hyperlactataemia derives from anaerobic glycolysis7, and that L-lactate is a marker of underlying tissue hypoxia. In severe falciparum malaria tissue hypoxia might increase the overall concentration of PFAA.
To determine the interrelationships between several individual amino acid disorders in patients with malaria we simultaneously quantified and profiled a broad range of amino acids in plasma by high-performance multiple-reaction-monitoring mass-spectrometry (HPLC-MRM-MS). We hypothesised that amino acid derangements in patients with malaria are not isolated disorders but that they follow overall changes in amino acid metabolism, characterised by an overall reduction of the concentration of PFAA in the context of infection. While in severe falciparum malaria, we postulated, L-lactate is related to an increase in the total concentration of PFAA. These metabolomic studies might help improve the understanding of the pathogenesis of amino acid derangements in severe malaria, with potential implications for their adjunctive treatment.
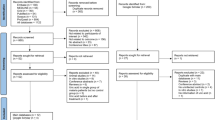
Participants
A total of 295 participants were consecutively enrolled in a prospective observational study in Chittagong Bangladesh, between 2014–2017, including adults with severe malaria (n = 88), septicaemia (n = 88), uncomplicated malaria (n = 71), and healthy controls (n = 48). The overall case fatality rate of severe falciparum malaria was 30%, and that of sepsis was 23%. Baseline characteristics of the study population are described in Table 1.
Plasma free amino acids
Using HPLC-MRM-MS, we measured a total of 30 amino acids in plasma of study participants. Amino acids were excluded from the final analysis if they were detected in only a small number of cases (n < 50). We excluded 1-methylhistidine, alpha-aminoadipic acid, threonine, homocysteine, sarcosine, thiaproline, alpha-aminopimelic acid, hydroxylysine, and γ -aminobutyric acid (GABA).
The final data set included 21 plasma free amino acids (PFAA) that could be accurately quantified in the plasma of study participants (Table 2). The total PFAA concentration was calculated for each participant and compared between patient groups. We observed a significant reduction of the median concentration of PFAA in all patient groups when compared to healthy individuals, particularly in patients with uncomplicated malaria (Table 2 and Fig. S1). The individual levels of amino acid levels are graphically displayed in Supplementary Figs S2 and S3.
Amino acid derangements in malaria and sepsis
To determine the patterns of change of individual amino acids, we profiled PFAA by calculating the fold change of each amino acid compared to healthy controls and plotting the log2 normalised changes in a radar plot (Fig. 1). With the exception of phenylalanine, we observed that in each of the study groups the majority of amino acids were below normal levels.
Radar plots of the plasma free amino acid profiles of study groups. (a) Severe falciparum malaria (n = 88). (b) SIRS/Sepsis (n = 71). (c) Uncomplicated Malaria (n = 88). The log2 normalised median fold change of each amino acid was calculated compared to the normal levels measured in healthy controls and visualised in a radar plot.
Patients with severe malaria showed an average −23% reduction of the total concentration of PFAA. This reduction was largely due to lower concentrations of amino acids in the arginine-NO pathway, aromatic amino acids (with the exception of phenylalanine), and glucogenic amino acids.
Uncomplicated malaria was associated with a −54% reduction of the total concentration of PFAA. All amino acids, except phenylalanine, were below normal levels. Particularly metabolites from the arginine-NO pathway were low, indicating a deficiency of L-arginine and L-arginine precursors in uncomplicated malaria.
Sepsis was associated with a −32% reduction in the total PFAA concentration. A widespread reduction in amino acids was observed, particularly characterised by a reduction in tryptophan, while phenylalanine was increased.
Association of amino acid profiles with coma, AKI, and hyperlactataemia
We further analysed the amino acid profiles of 88 patients with severe malaria in relation to major clinical manifestations: coma, acute kidney injury, and hyperlactataemia (Fig. 2).
Radar plots of the plasma free amino acid profiles of major clinical syndromes of severe falciparum malaria, including coma, acute kidney injury, and hyperlactataemia. The log2 normalised median fold change of each amino acid was calculated compared to the normal levels measured in healthy controls and visualised in a radar plot.
Coma, as defined by a Glasgow Coma Scale <1124, was observed in a total of 30 (34%) patients with severe falciparum malaria. Having coma, using a binary cut-off, did not significantly alter the plasma free amino acid profile, except for a decrease in valine (Benjamini Hochberg (BH) adjusted p-value = 0.037). We did not observe any significant differences in the concentration of phenylalanine between patients with or without cerebral malaria nor was there a significant correlation between GCS and phenylalanine (Spearman’s rho = −0.17, p = 0.13).
Acute kidney injury, defined by a serum creatinine >265 µmol/L (3 mg/dL)24, was found in 29 (33%) patients. Patients with acute kidney injury had significantly higher levels of hydroxyproline (BH adj. p = 0.0037) and cysteine (BH adj. p = 6.4 × 10−4).
Hyperlactataemia, as defined by a venous L-lactate >5 mmol/L24, was diagnosed in a total of 21 (23%) of patients with severe malaria. Incremental changes in venous L-lactate were associated with an increasing total concentration of plasma free amino acids (Fig. 2). L-lactate correlated with plasma alanine (Spearman’s rho = 0.57, p = 3.5 × 10−8), as reported earlier8, and phenylalanine (Spearman’s rho = 0.37, p = 4.5 × 10−4), and proline (Spearman’s rho = 0.39, p = 2.4 × 10−4). Regardless of the degree of lactic acidosis, the overall concentrations of glutamate and tryptophan remained well below the normal levels seen in healthy controls.
Amino acid profiles associated with death
In patients with severe malaria, the amino acid profiles at study enrolment in patients who died compared to survivors generally showed an overall increase in the wide range of amino acids (Fig. 3). The altered amino acid profiles observed in patients who died resembled the patterns observed in patients with hyperlactataemia. A total of 10 out of 21 measured amino acids were significantly elevated in patients who died from severe malaria compared to those who survived their infection. These changes included a significant increase in plasma alanine (BH adj. p = 5 × 10−4), phenylalanine (BH adj. p = 5 × 10−4), and proline (BH adj. P = 0.011). In contrast, among patients with sepsis there were no significant differences between the levels of plasma amino acids between patients who survived and those who died.
Radar plot of the plasma free amino acid profiles of patients with severe falciparum malaria or sepsis who survived their infection and in patients who died. The log2 normalised median fold change of each amino acid was calculated compared to the normal levels measured in healthy controls and visualised in a radar plot.
Determinants of total plasma amino acid levels in adults with severe falciparum malaria
We modelled the effects of L-lactate on the total concentration of PFAA using multivariate regression analysis, adjusting for factors that could explain an energy deficit or malnutrition. We wanted to assess the effect of L-lactate on the total concentration of plasma free amino acids, and used a causal inference based method including directed acyclical graphs (DAGs) (Supplementary Fig. S4). To adjust for an acute energy deficit, we included duration of illness, a measure of coma depth (GCS), and blood glucose levels (to account for hypoglycaemia). We adjusted for the total parasite biomass by including log10 normalised plasma PfHRP2. Renal elimination was adjusted for by including serum creatinine. We accounted for pre-existing malnutrition by including body mass index (BMI).
Based on our multivariate linear regression model, and if our assumptions are correct, coma depth (GCS) and L-lactate are independent predictors of total PFAA (Table 3). We observed a strong effect of L-lactate on the total PFAA concentrations in patients with severe falciparum malaria, where incremental levels of L-lactate were significantly associated with increased total concentrations of PFAA. Patients who were in a deeper coma were also more likely to have higher total PFAA levels.
Discussion
In this prospective observational cohort of patients with malaria and sepsis we investigated the patterns and determinants of plasma free amino acid derangements during severe infection. Using HPLC-MRM-MS we quantified 21 free amino acids in the plasma of 295 study participants. All patient groups showed a general reduction in the total concentration of amino acids on enrolment compared to normal levels observed in local healthy controls. Patients with uncomplicated malaria showed the largest decrease of PFAA (−54%). We analysed the amino acid profiles in relation to clinical manifestations and outcome in patients with severe malaria. Although the total concentration of PFAAs was on average decreased compared to normal levels (on average −23%), hyperlactataemia was associated with widespread increase, likely because this reflects tissue hypoxia. We used a multivariate regression model to determine the effect of L-lactate on the plasma concentration of free amino acids in patients with severe falciparum malaria and observed that after adjusting for potential confounders, L-lactate likely caused by tissue hypoxia remained a significant predictor of an increased total concentration of PFAA.
These observations confirm previous findings of amino acid derangements in patients with severe falciparum malaria, including derangements in L-arginine, alanine, and phenylalanine metabolism, however, we show they are part of a widespread pattern of amino acid dysregulation. Concentrations of PFAA were generally decreased in patients with severe malaria, but also in sepsis and uncomplicated malaria. Previously described individual amino acid derangements are in part explained by this, and are therefore less likely to be specific for certain presenting syndromes. In cases with malaria and sepsis, we observe amino acids are depleted from plasma, which is likely due to increased hepatic amino acid extraction from blood, as has been shown before in patients with inflammation and sepsis17,19,21. Although there is on average a negative nitrogen balance in patients with severe falciparum malaria, we observe that L-lactate, as a marker for tissue hypoxia, is associated with a widespread increase in nearly all amino acids, probably due to increased muscle protein breakdown. The relationship between increased plasma L-lactate and raised PFAA may also be related to impaired liver blood flow with hepatic tissue dysoxia25,26, leading to a reduction of hepatic PFAA extracted from plasma.
Our data are consistent with previous reports of L-arginine deficiency in patients with severe and uncomplicated malaria5,6,27,28,29. Previously, L-arginine deficiency was attributed to increased metabolism of L-arginine following intravascular nitric oxide depletion30 and by arginases from host29 or parasite31,32. It has recently been proposed that L-arginine deficiency might arise from low bioavailability of its precursors33. We measured two L-arginine precursors, ornithine and citrulline, and observed both were significantly depleted in uncomplicated malaria. Our findings support the hypothesis that low-bioavailability of precursors contributes to L-arginine deficiency in malaria, early during the disease process, and probably because of a overall negative nitrogen balance.
Current data support previous findings of a correlation between L-lactate and plasma alanine in severe falciparum malaria8. Muscle protein catabolism increases nitrogen levels during tissue hypoxia and anaerobic glycolysis. Nitrogen is shuttled to the liver through the Cahill cycle in the form of alanine, where it is utilised in gluconeogenesis. However, high levels of L-lactate may reduce the hepatic disposal alanine and of other glucogenic amino acids8,34, which likely explains their strong correlation.
Our data confirm hyperphenylalaninaemia in patients with severe malaria, as described previously9,10,11,12. Similar to prior studies, we also note that patients with sepsis and uncomplicated malaria have significantly increased plasma levels of phenylalanine. Previous studies have investigated if there may be a link between hyperphenylalaninaemia and coma9,10,11,12. Hyperphenylalaninaemia has been attributed to reduced activity from phenylalanine-hydroxylase due to a deficiency of its co-factor tetrahydrobiopterin9,11,12,33 which affects the metabolism of aromatic amino acids (Arg, Trp, Phe, Tyr) and the biosynthesis of neurotransmitters from the phenylalanine/tyrosine pathways. Unfortunately we were unable to measure biopterins in this study and therefore cannot conclude a role for aromatic amino acid co-factor deficiencies in our study population. However, increased phenylalanine:tyrosine ratios among patients with malaria or sepsis were suggestive of reduced conversion of phenylalanine to tyrosine (Supplementary Fig. S5). Among patients with severe malaria, we did not observe a relationship between phenylalanine and coma depth (Spearman’s rho = −0.17, p = 0.13), as shown previously in both adult and pediatric severe malaria10. Although it is not completely clear what causes hyperphenylalaninaemia in severe falciparum malaria, it is not specific to malaria alone and also occurs in sepsis.
In conclusion, the concentrations of plasma free amino acid are decreased in patients with severe malaria, sepsis and uncomplicated malaria. Previously described individual amino acid derangements are in part explained by this, and less likely specific for certain presenting syndromes. Hyperlactataemia increased the total amino acid concentration in patients with severe malaria, likely because this reflects tissue hypoxia.
Methods and Materials
Ethical statement
This was a sub-study of an observational study protocol that was reviewed and approved by the local ethics review board, the Chittagong Medical College Ethics Committee, Bangladesh, and the Oxford Tropical Research Ethics Committee (OxTREC), in the United Kingdom. The trial was registered at ClinicalTrials.gov (Trial number: NCT02451904). All research staff involved with providing patient care received training according to the Guidelines for Good Clinical Practice; the studies were conducted according to the Declaration of Helsinki35,36. All participants provided written informed consent prior to enrolment. Individual written informed consent was obtained from the patient or from their attending relatives if they were unable to give consent themselves due to the severity of their illness.
Study Design
A prospective observational case-control study in Chittagong Medical College Hospital, Bangladesh. The recruitment phase of the study spanned four wet-seasons and was from May-September 2014 and May-September 2017.
Study participants and procedures
We consecutively enrolled male and female adults (>12 years) with falciparum malaria and patients with sepsis. Patients with a blood slide positive for asexual blood stages of P. falciparum (including mixed infection with non-falciparum species) were eligible to participate in the malaria study group. Severe and uncomplicated falciparum malaria were strictly defined according the WHO criteria for severe malaria24, modified by Hien et al.37. Patients who had a confirmed negative blood slide for malaria were assessed for eligibility in the sepsis study group and consecutively enrolled. A minority of patients had already received a first dose of antimalarials prior to the study, however, cases were excluded if they received antimalarial therapy >24 hours before enrolment. Healthy controls were required to have a blood slide negative for malaria, normal vital signs (no hypertension). Healthy controls were excluded if they were pregnant, had a chronic illness, took medication in the prior two months before enrolment.
On enrolment, we took a medical history, a medication history, assessed vital signs, performed a physical examination and drew blood samples for blood gas analysis and amino acid analysis. Participants were not required to be fasting at the time of blood draw. Patients were followed daily until hospital discharge or in-hospital death. Laboratory assessments included haematology, which was done in a quality controlled external laboratory (Chevron Clinical Lab, Chittagong, Bangladesh). We used iStat analysers (Abbott, Chicago, Illinois) for biochemistry (Chem8 + cartridge) and blood gas and L-lactate analysis (CG4 + cartridge).
HPLC-MRM-MS
Blood for amino acid analysis was drawn from a fresh catheter in the forearm in non-fasting adults immediately following study enrolment and usually before a first dose of antimalarials was provided. Blood samples was collected in lithium-heparin tubes that were immediately centrifuged and flash-frozen in liquid-nitrogen. Samples were shipped on dry ice and stored at −80 °C. In brief, amino acids were extracted by solid-phase extraction using sorbent tips (Phenomenex EZ:faast™), as described previously38. Plasma free amino acids (PFAA) were separated on an AAA-MS™ column (250 × 3.0 mm, Phenomenex, Torrance, California) placed in a Thermo LC system. Mass spectrometry with multiple reaction monitoring was done in positive ion mode with electrospray ionization on an ABSciex API 5000 Triple Quadrupole LC/MS/MS Mass Spectrometer. Inter-assay variation scores were determined for three amino acid standards and the individual amino acids. Concentrations were based on interpolation on a linear standard curve. We excluded amino acids if they could be measured in less than 50 cases. The final amino acid data set is publicly available on GitHub, found at: https://github.com/Stije/PFAA.
Statistical analysis
Data analysis was carried out in R statistical software (V3.3.3). Baseline characteristics in the study groups and the plasma concentration of free amino acids are all presented as median with inter quartile ranges (IQR), unless stated otherwise. Categorical data were reported as number and proportions. Significance was estimated for multiple study groups (>2) using Kruskal-Wallis tests and corrected by a Benjamini-Hochberg procedure, where appropriate. Significance was estimated for two study groups by Mann-Whitney U tests. Associations were tested for using Spearman’s rank correlation. The sum of all measured amino acids (per individual) was calculated to determine the total plasma concentration of free amino acids per individual. Amino acid profiles were visualised in radar plots using the’fmsb’ package in R. Radar plots contained normalised amino acid concentrations (the log2 median fold change of patients compared to healthy controls).
We wanted to determine the potential effects of tissue hypoxia on the total concentration of PFAA, and used directed acyclic graphs (DAGs) as a causal inference framework (Supplementary Fig. S4). This method requires that the direct causal effects between variables of interest are specified based on a subjective exercise, which has the benefit of clearly displaying the assumptions underlying the results. We based our DAG on the assumption that the total concentration of PFAA reflects a balance between malnutrition, an energy deficit and tissue hypoxia. The potential mechanisms are depicted in the DAG. We used a multivariate linear regression model to characterise the relationship between tissue hypoxia and the total measured PFAA. The standard linear regression was fitted using the function glm in R.
References
Norheim, O. F. et al. Avoiding 40% of the premature deaths in each country, 2010–30: Review of national mortality trends to help quantify the un Sustainable Development Goal for health. The Lancet 385, 239–252, https://doi.org/10.1016/S0140-6736(14)61591-9 (2015).
WHO World Malaria Report 2017. Tech. Rep., World Health Organization, Geneva (2017).
Dondorp, A. M. Artesunate versus quinine for treatment of severe falciparum malaria: A randomised trial. Lancet 366, 717–725, https://doi.org/10.1016/S0140-6736(05)67176-0 (2005).
Dondorp, A. M. et al. Artesunate versus quinine in the treatment of severe falciparum malaria in African children (AQUAMAT): An open-label, randomised trial. The Lancet 376, 1647–1657, https://doi.org/10.1016/S0140-6736(10)61924-1 (2010).
Lopansri, B. K. et al. Low plasma arginine concentrations in children with cerebral malaria and decreased nitric oxide production. The Lancet 361, 676–678, https://doi.org/10.1016/S0140-6736(03)12564-0 (2003).
Yeo, T. W. et al. Recovery of Endothelial Function in Severe Falciparum Malaria: Relationship with Improvement in Plasma L-Arginine and Blood Lactate Concentrations. Journal of Infectious Diseases 198, 602–608, https://doi.org/10.1086/590209 (2008).
Day, N. P. et al. The pathophysiologic and prognostic significance of acidosis in severe adult malaria. Critical Care Medicine 28, 1833–1840, https://doi.org/10.1097/00003246-200006000-00025 (2000).
Pukrittayakamee, S. et al. Alanine metabolism in acute falciparum malaria. Tropical Medicine & International Health 7, 911–918, https://doi.org/10.1046/j.1365-3156.2002.00955.x (2002).
Enwonwu, C. O. et al. Hyperphenylalaninaemia in children with falciparum malaria. Quarterly Journal of Medicine 92, 495–503 (1999).
Lopansri, B. K. et al. Elevated plasma phenylalanine in severe malaria and implications for pathophysiology of neurological complications. Infection and Immunity 74, 3355–3359, https://doi.org/10.1128/IAI.02106-05 (2006).
Yeo, T. W. et al. Impaired Systemic Tetrahydrobiopterin Bioavailability and Increased Dihydrobiopterin in Adult Falciparum Malaria: Association with Disease Severity, Impaired Microvascular Function and Increased Endothelial Activation. PLoS Pathogens 11, 1–13, https://doi.org/10.1371/journal.ppat.1004667 (2015).
Rubach, M. P. et al. Impaired Systemic Tetrahydrobiopterin Bioavailability and Increased Oxidized Biopterins in Pediatric Falciparum Malaria: Association with Disease Severity. PLoS Pathogens 11, 1–22, https://doi.org/10.1371/journal.ppat.1004655 (2015).
Dobbie, M., Crawley, J., Waruiru, C., Marsh, K. & Surtees, R. Cerebrospinal fluid studies in children with cerebral malaria: an excitotoxic mechanism? The American Journal of Tropical Medicine and Hygiene 62, 284–90, https://doi.org/10.4269/ajtmh.2000.62.284 (2000).
Medana, I. M. et al. Metabolites of the Kynurenine Pathway of Tryptophan Metabolism in the Cerebrospinal Fluid of Malawian Children with Malaria. Journal of Infectious Diseases 188, 844–849, https://doi.org/10.1086/377583 (2003).
Planche, T. et al. Plasma glutamine and glutamate concentrations in Gabonese children with Plasmodium falciparum infection. Quarterly Journal of Medicine 95, 89–97, https://doi.org/10.1093/qjmed/95.2.89 (2002).
Nelson, D. L. & Cox, M. M. Lehninger Principles of Biochemistry 5th ed., https://doi.org/10.2307/1309148 (2008).
Druml, W., Heinzel, G. & Kleinberger, G. Amino acid kinetics in patients with sepsis. American Journal of Clinical Nutrition 73, 908–913, https://doi.org/10.1093/ajcn/73.5.908 (2001).
Askanazi, J. et al. Muscle and Plasma Amino Acids after Injury. Annals of Surgery 191, 465–472, https://doi.org/10.1097/00000658-198004000-00013 (1980).
Sprung, C. L. et al. Amino acid alterations and encephalopathy in the sepsis syndrome. Critical Care Medicine 19, 753–757, https://doi.org/10.1097/00003246-199106000-00004 (1991).
Ghisolfi, J. et al. Plasma free amino acids in normal children and in patients with proteinocaloric malnutrition: Fasting and infection. Pediatric Research 12, 912–917, https://doi.org/10.1203/00006450-197809000-00006 (1978).
Fischer, C. P., Bode, B. P., Abcouwer, S. F., Lukaszewicz, G. C. & Souba, W. W. Hepatic uptake of glutamine and other amino acids during infection and inflammation (1995).
Dondorp, A. M. et al. Direct In Vivo Assessment of Microcirculatory Dysfunction in Severe Falciparum Malaria. Journal of Infectious Diseases 197, 79–84, https://doi.org/10.1086/523762 (2008).
Hanson, J. et al. Relative contributions of macrovascular and microvascular dysfunction to disease severity in falciparum malaria. Journal of Infectious Diseases 206, 571–579, https://doi.org/10.1093/infdis/jis400 (2012).
World Health Organization. Guidelines for the treatment of Malaria, vol. 85 (Geneva, 2015).
Pukrittayakamee, S. et al. Glycerol metabolism in severe falciparum malaria. Metabolism 43, 887–892, https://doi.org/10.1016/0026-0495(94)90272-0 (1994).
Day, N. P. et al. Effects of dopamine and epinephrine infusions on renal hemodynamics in severe malaria and severe sepsis. Critical Care Medicine 28, 1353–1362, https://doi.org/10.1097/00003246-200005000-00016 (2000).
Yeo, T. W. et al. Impaired nitric oxide bioavailability and l-arginine–reversible endothelial dysfunction in adults with falciparum malaria. The Journal of Experimental Medicine 204, 2693–2704, https://doi.org/10.1084/jem.20070819 (2007).
Yeo, T. W. et al. Angiopoietin-2 is associated with decreased endothelial nitric oxide and poor clinical outcome in severe falciparum malaria. Proceedings of the National Academy of Sciences 105, 17097–17102, https://doi.org/10.1073/pnas.0805782105 (2008).
Yeo, T. W. et al. Increased Asymmetric Dimethylarginine in Severe Falciparum Malaria: Association with Impaired Nitric Oxide Bioavailability and Fatal Outcome. PLoS Pathogens 6, e1000868, https://doi.org/10.1371/journal.ppat.1000868 (2010).
Weinberg, J. B., Lopansri, B. K., Mwaikambo, E. & Granger, D. L. Arginine, nitric oxide, carbon monoxide, and endothelial function in severe malaria. Current Opinion in Infectious Diseases 21, 468–475, https://doi.org/10.1097/QCO.0b013e32830ef5cf (2008).
Olszewski, K. L. et al. Host-Parasite Interactions Revealed by Plasmodium falciparum Metabolomics. Cell Host & Microbe 5, 191–199, https://doi.org/10.1016/j.chom.2009.01.004 (2009).
Cobbold, S. A., Llinás, M. & Kirk, K. Sequestration and metabolism of host cell arginine by the intraerythrocytic malaria parasite Plasmodium falciparum. Cellular Microbiology 18, 820–830, https://doi.org/10.1111/cmi.12552 (2016).
Alkaitis, M. S. et al. Decreased rate of plasma arginine appearance in murine malaria may explain hypoargininemia in children with cerebral malaria. Journal of Infectious Diseases 214, 1840–1849, https://doi.org/10.1093/infdis/jiw452 (2016).
Marliss, E. B. et al. Amino acid metabolism in lactic acidosis. The American Journal of Medicine 52, 474–481, https://doi.org/10.1016/0002-9343(72)90038-1 (1972).
ICH Expert Working Group ICH Harmonised Tripartite Guideline: Guideline for Good Clinical Practice. Tech. Rep. June, International conference on harmonisation of technical requirements for registration of pharmaceuticals for human use (1996).
CIOMS International Ethical Guidelines for Health-related Research Involving Humans (The World Health Organization, Geneva, 2016).
Hien, T. T. et al. A Controlled Trial of Artemether or Quinine in Vietnamese Adults with Severe Falciparum Malaria. New England Journal of Medicine 335, 76–83, https://doi.org/10.1056/NEJM199607113350202 (1996).
Badawy, A. A. B., Morgan, C. J. & Turner, J. A. Application of the Phenomenex EZ:faast amino acid analysis kit for rapid gas-chromatographic determination of concentrations of plasma tryptophan and its brain uptake competitors. Amino Acids 34, 587–596, https://doi.org/10.1007/s00726-007-0012-7 (2008).
Acknowledgements
We are grateful for all patients and their families who participated in the study. We thank Sanjib Kanti Paul and Sumon Sharma for their support with screening patients, and Benjamach Intharabut and Ketsanee Srinamon for malaria microscopy and laboratory support. We thank Md Safiqul Mostafa Chowdhury for his administrative support and Marja Schilstra for data management. This work was supported by the Wellcome Trust [106698/B14/Z].
Author information
Authors and Affiliations
Contributions
M.W., A.M.D., S.J.L. and H.W.K. conceived the study, S.J.L., H.W.K., and A.G., K.P. collected clinical data and samples, S.J.L., A.P. and M.W. conducted the LCMS experiments, S.J.L. analysed the results. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Leopold, S.J., Apinan, S., Ghose, A. et al. Amino acid derangements in adults with severe falciparum malaria. Sci Rep 9, 6602 (2019). https://doi.org/10.1038/s41598-019-43044-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-43044-6
This article is cited by
-
Host metabolomic responses in recurrent P. vivax malaria
Scientific Reports (2024)
-
Starvation induces changes in abundance and small RNA cargo of extracellular vesicles released from Plasmodium falciparum infected red blood cells
Scientific Reports (2023)
-
The Metabolomic Profiles of Sera of Mice Infected with Plasmodium berghei and Treated by Effective Fraction of Naja naja oxiana Using 1H Nuclear Magnetic Resonance Spectroscopy
Acta Parasitologica (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.