Abstract
We aimed to compare the efficacy and safety of Multipulse laser vaporesection of the prostate (MPVP) versus plasmakinetic resection of the prostate (PKRP) for treatment of patients with benign prostate obstruction (BPO) in a prospective trial. From January 2016 to April 2017, a total of 144 patients were included in the cohort study, of whom 73 patients underwent MPVP and 71 underwent PKRP. All patients received pre-operative evaluation and followed up at 1, 3, 6 and 12 months postoperatively. Baseline characteristics, perioperative data and postoperative outcomes were compared. Early (within 30 days postoperatively) and late complications were also recorded. Preoperative data, including age, prostate volume, international prostate symptom score (IPSS), International Index of Erectile Function Questionnaires (IIEF-5), the rate of anticoagulants use, Charlson comorbidity index were similar in two groups. Peri-operative parameters, including the rate of transfusion, and decrease in hemoglobin level were comparable. The operative time, the duration of catheterization and length of hospital stay were significantly shorter in the MPVP group. The voiding parameters and the quality-of-life scores (QoL) improved significantly in both groups postoperatively. There was a significantly difference in QoL at 1-year in the MPVP group (p < 0.001), under mixed model analysis with random effect and Bonferroni correction. There were no significant differences in improvement of IPSS, Qmax, IIEF-5, residual prostate volume ratio and PSA level reduction at the 1-year follow-up. MPVP was significantly superior to PKRP in terms of a reduction in overall complication rate (21.9% vs 45.0%, p = 0.004). Both treatments led to comparable symptomatic improvements. MPVP demonstrates satisfactory efficiency, shorter catheterization time and shorter hospital stay. Our data revealed that MPVP may be a promising technique which is safe and favorable alternative for patients with BPO.
Similar content being viewed by others
Introduction
Benign prostate obstruction can be treated with a range of laser treatments using different laser systems and applications. Transurethral laser treatment is considered to be an alternative treatment to transurethral resection of the prostate (TURP)1. In the past decade, different kinds of laser systems are used to produce various tissue ablations, such as coagulation, vaporization or resection and/or enucleation, in the treatment of BPO2,3,4.
Previous studies have compared the outcomes between TURP and transurethral laser treatment. Compared to TURP, thulium laser prostatectomy reduced blood loss, shorten catheterization time and hospital stay, and yielded better efficacy3. The diode laser was reported to combine high tissue ablation capacity and good hemostatic properties5,6. Tan et al. indicated that diode laser was better than thulium laser for prostate vaporesection because of its shorter catheterization time7. The re-operation rate for diode laser treatment was higher compared to that for 532 nm greenlight laser, photoselective vaporization of the prostate8. Growing evidence on safety and efficacy regarding these laser treatments have been revealed, all these available laser treatments have individual advantages and disadvantages.
A recently introduced double laser combination system, the Multipulse Tm + 1470 laser system (Asclepion, Jena, Germany), has been applied for BPO treatment. The device is a combination of a Thulium:YAG laser that emits a wavelength of 1940 nm and a near infrared diode laser module that emits a wavelength of 1470 nm. The total laser power is up to 150 Watts and transmitted through end-firing optical fibers. The Multipulse laser might represent a similar resection efficacy as thulium and optimization of hemostatic efficacy deriving from the combination with the second wavelength. The data of safety and efficacy comparing Multipulse laser vaporesection of prostate (MPVP) and plasmakinetic resection of the prostate (PKRP) are still lacking.
In this study, we prospectively assessed the clinical outcome of MPVP versus PKRP with a 1-year follow-up. To our knowledge, this study is the first report on the feasibility and efficacy of Multipulse Tm + 1470 laser system for treatment of BPO.
Methods and Materials
Study design and patients enrollment
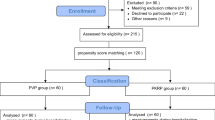
This study is a prospective, single-center, clinical observation to compare outcomes of MPVP versus PKRP. Between January 2016 and April 2017, a total of 160 patients with symptomatic BPO underwent treatment with the Multipulse Tm + 1470 laser system (80 cases) or the PKRP (80 cases). Inclusion criteria were patient age older than 50 years, maximum flow rate (Qmax) < 15 mL/second and the International Prostate Symptom Score (IPSS) ≥ 10. All subjects received quality-of-life questionnaire (QoL) and transrectal ultrasound of the prostate (TRUS) preoperatively. TRUS biopsies were performed before surgery in cases of suspicious malignancy. Patients with prostate cancer, bladder cancer, previous transurethral surgery, interstitial cystitis and neurogenic bladder were excluded. The use of anticoagulants or platelet aggregation inhibitors and urinary retention under catheterization was not a criterion for study exclusion. Patients taking anticoagulants or platelet aggregation inhibitors were requested to discontinue the use of these drugs three days before operation. The Charlson comorbidity index (CCI) was used to measure underlying comorbid disease status9. This study was approved by the institutional review board at New Taipei City Hospital (No. 105005-E). We have registered our study in WHO primary clinical trial registry on February, 21, 2019 and obtained the registration number (ChiCTR1900021449). All methods were performed in accordance with the relevant guidelines and regulations of the institution. The written informed consent forms from all subjects who met the inclusion criteria were obtained. A total of 144 patients were included in the study (73 MPVPs and 71 PKRPs), all signed an informed consent. Eight patients lost follow-up (3 MPVPs and 5 PKRPs).
Surgical technique
The MultiPulse Tm + 1470 laser system combines a Thulium:YAG laser emitting at a wavelength of 1940 nm and a near infrared diode laser module emitting at a wavelength of 1470 nm. The laser power can reach 150 Watts (120 Watts Thulium:YAG laser + 30 Watts diode laser) and is then transmitted through end-firing optical fibers.
All patients were placed in the lithotomy position under spinal or general mask anesthesia. Two experienced urologists (F.S.H. and C.W.C.) carried out all procedures in this study. Each had performed over 800 cases with transurethral resection of prostate with either laser or electrocautery. We used a 26-Fr resectoscope sheath (Olympus, Tokyo, Japan) coupled with either laserscope or resectoscope for both groups. Continuous normal saline irrigation of the operative field was brought throughout the operation. The energy setting of MPVP during surgery was within the range: Thulium:YAG laser power 80–120 Watts and diode laser power 20–30 Watts. The vaporesection procedure began with incision manner at 1 and 11 o’clock of the bladder neck, to the level of the verumontanum. The incision depth was continued to the prostate capsule. The vapoincision lines were then created at the 5 and 7 o’clock position to separate the right, median and left lobes. The three lobes were enucleated in sequence, and pushed into the bladder. Tissue was vaporized or vapoincised sufficiently so that small pieces could be removed through the laserscope by a balloon evacuator. Otherwise, intravesical morcellation by tissue morcellator was performed to remove the resected tissue.
In the PKRP group, the resection power was 160 Watts and the electric coagulation was set at 80 Watts. A reflux plasma prostate resectoscope (Olympus, Tokyo, Japan) was used. A longitudinal groove was first made at 5 and 7 o’clock, deep into the surgical capsule, from the bladder neck toward the proximal of the verumontanum. The bilateral lobes and median lobe were resected in sequence, and the procedure was finished by trimming the apex. The resected chips were washed out by an Ellick balloon evacuator. At the end of both procedures, a 22-Fr triple-lumen catheter was placed into the bladder, and continuous irrigation of the bladder with saline was set up in all patients.
Outcome measurement
The primary outcome measurement was IPSS at 12 months. The secondary outcome measurements were Qmax and QoL. The following parameters were assessed preoperatively and at 1-, 3-, 6- and 12-months intervals after operation: IPSS, International Index of Erectile Function Questionnaire (IIEF-5), Qmax, postvoid residual (PVR), QoL, PSA and prostate volume. The hemoglobin difference before surgery and the day after the surgery was documented. The operative time, catheterization time and hospital stay between two groups were compared.
The peri- and postoperative complications, classified using the Uro-Clavien-Dindo classification9,10, including blood transfusion, prolonged urinary infection, dysuria, prolonged hematuria, re-catheterization, re-operation, incontinence, urethra stricture and scrotal edema were recorded and compared. With consideration of safety issue, any adverse events (AEs) ≥ Grade III would be immediately reported and well inspected.
Statistical analysis
All data in this study are presented as mean ± standard deviation. Stata Corp Stata 15 was used for statistical analysis. The Fisher’s exact test was applied to compare categorical variables; and the Student’s t-test was used to compare quantitative variables between the two treatment groups. A mixed model with random effect and Bonferroni correction was applied to compare IPSS, QoL, Qmax, and PVR between two groups. A two-sided p-value of <0.05 was considered statistically significant.
Results
Baseline and perioperative parameters
A total of 144 patients (MPVP: 73, PKRP: 71) were included in this study. The demographic data of the patients are shown in Table 1. The mean age of the patients in the MPVP and PKRP groups was 68.8 ± 8.3 and 69.9 ± 9.2 years, respectively (p = 0.438). The mean prostate volume (57.0 vs. 60.2 mL), PSA (3.8 vs. 4.2 ng/mL), IPSS (21.7 vs. 22.5), IIEF-5 (5.1 vs. 5.9), percent of indwelling catheter (13.7% vs. 16.9%), and the Charlson comorbidity index9 (CCI, 1.47 vs. 1.44) were similar in two groups, MPVP versus PKRP (all p > 0.05).
The perioperative parameters are listed in Table 2. There were no significant differences in the rate of transfusion, and decrease of hemoglobin level between two groups. However, compared with the PKRP group, patients in the MPVP group had shorter operative time (30.9 ± 10.3 vs. 36.4 ± 13.8 minutes, p = 0.008), shorter catheterization time (21.3 ± 4.6 vs. 37.4 ± 15.9 hours, P < 0.001), and shorter hospital stay (2.6 ± 1.0 vs. 3.6 ± 1.3 days, p < 0.001). The weight of resected adenoma was heavier in PKRP group compared to those in MPVP group (11.0 ± 8.0 vs. 20.6 ± 10.5 gm, p < 0.001).
Functional outcomes
The improvement of functional outcomes is shown in Table 3 and Fig. 1. At the 12-month follow-up, the voiding parameters (IPSS, Qmax and PVR), IIEF-5 and QoL improved significantly compared with pre-operative data. Compared with PKRP group, the improvement of IPSS, QoL, Qmax and PVR in patients in MPVP group was not significantly different at 12 months post-operatively (p = 0.350, 0.096, 0.562 and 0.696, respectively). However, under mixed model analysis with random effect and Bonferroni correction, MPVP group was superior to PKRP group in IPSS and QoL (p = 0.049 and <0.001, respectively).
Outcomes following treatment with the MultiPulse laser (MPVP) or plasmakinetic resection of the prostate (PKRP). (A) International Prostate Symptom Score (IPSS), (B) quality-of-life index (QoL), (C) maximum flow rate (Qmax) and (D) postvoid residual urine (PVR). P-value of mixed model with random effect and Bonferroni correction was mentioned at the corner of each graph. Base: preoperative data, M1: 1-month, M3: 3-month, M6: 6-month, Y1: 1-year follow-up.
Adverse events
The postoperative complications were classified as early stage (within 30 days) and late stage (after one month) and summarized in Table 4. We used the Uro-Clavien-Dindo classification to evaluate treatment-related complications10,11. Overall, 78.1% of MPVP group and 55.0% of PKRP group were free of any treatment-related adverse event (AE, p = 0.004).
No statistically significance was observed between two groups in urinary tract infection (UTI), re-catheterization, clots retention, epididymo-orchitis, urinary incontinence and TUR syndrome within 30 days. The rate of late complications was comparable between two groups, including hematuria, dysuria, urethral stricture, urge incontinence, and stress incontinence. We observed a higher re-operation rate with the PKRP group (7.0% vs. 1.4%, p = 0.113). The causes of re-operation in PKRP group were two cases with bladder neck contracture, one with residual adenoma, and two with urethra stricture. There was a case undergoing MPVP developed a bladder neck stone 11 months postoperatively, and removal of the stone was done.
Discussion
In the past two decades, a wide range of innovative transurethral procedures have challenged the standard surgical treatment, monopolar TURP, in the treatment of BPO12. PKRP has efficacy similar to TURP with fewer adverse events13. Laser prostatectomy techniques such as holmium laser enucleation of the prostate (HoLEP), Green Light photoselective vaporization of the prostate (PVP) and thulium laser resection of the prostate (ThuRP), have been widely adopted in clinical practice for the comparable or improved safety and efficacy with monopolar TURP1,2,14.
Several studies demonstrated that thulium laser intrinsically possesses several advantages, such as more efficient operation, improved spatial beam quality and more precise tissue incisions7,15,16. Different thulium laser techniques have been described, including thulium vapoenucleation (ThuVEP), thulium laser vaporesection of the prostate (ThuVaRP)17, thulium laser enucleation (ThuLEP), and thulium vaporization (ThuVP)18. ThuVaRP provides efficient resection and vaporization at the same time, and thus a faster tissue ablation rate14. Several studies have described the advantages and disadvantages of various laser prostatectomy techniques such as thulium vaporesection7,15,16, thulium laser enucleation18, diode laser vaporesection19,20,21,22, and Green Light laser vasporization5.
Most investigators agreed that, the extent of thermal damage is associated with hemostasis. Several previous studies analyzed the coagulation zone for different laser prostatectomy techniques to evaluate thermal damage PKRP has a coagulation layer of 0.3–1.0 mm, while thulium laser provides a 0.5–2.0 mm coagulation zone23,24. In animal models, the application of a 980 nm 150 Watts diode laser for prostate vaporization resulted in a necrotic zone of 6.1 ± 1.2 mm25, while the 120 Watts Green Light laser showed a 1.5 ± 0.3 mm coagulation band26. In the present study, we compared tissue thermal damage with PKRP, Multipulse, thulium and diode lasers in our patients (Fig. 2). The depth of thermal damage was 0.2–0.5 mm in PKRP, 0.5–1.0 mm in thulium laser (LISA Laser Products OHG, Katlenburg-Lindau, Germany), 0.5–1.5 mm in Multipulse laser, 2–4 mm in diode laser (Limmer Laser GmbH, Berlin, Germany), respectively. The coagulation zone of Multipulse laser was between those of thulium and diode laser. Consequently, the hemostatic efficacy of Multipulse laser was relatively superior to plasmakinetic prostatectomy.
Consistently, the blood transfusion rate related to perioperative bleeding was lower in the MPVP group (0 vs. 2.8%), without statistical significance (p = 0.246). The excellent hemostatic effect of Multipulse laser resulted in shorter catheterization time and hospital stay in our study.
In our study, the operative time was shorter in MPVP group (30.9 ± 10.3 vs. 36.4 ± 13.8 minutes, p = 0.008).The excellent hemostatic efficacy of MPVP provided a nearly bloodless operation field during the procedure. Two experienced surgeons could adequately resected prostate chip to reduce the use of morcellator, allowed operative time to be shortened. In contrast, it took more time for hemostasis in PKRP procedure. Additionally, the weight of the resected prostate tissue was heavier in the PKRP group (11.0 ± 8.0 vs. 20.6 ± 10.5 gm, p < 0.001). However, there was no significant difference in residual prostate volume ratio at 12 months between the two groups. Previous study demonstrated that the thulium laser concomitantly vaporized prostate tissue during cutting27,28, which could further shorten the operative time.
Yang reported a randomized study to compare ThuLEP with PKRP18. Both procedures did not differ significantly in terms of Qmax, IPSS, PVR, and QoL through 18 months of follow-ups. A meta-analysis showed no significant difference in IPSS, QoL, PVR and Qmax between ThuVaRP and with TURP or PKRP during the 3-, 6-, and 12-month follow-ups14. Our study showed no significant difference in IPSS, Qmax, residual prostate volume ratio, IIEF-5 and PSA drop between MPVP and PKRP groups at the 12-month follow-up (Table 3). Nevertheless, after mixed model analysis with random effect and Bonferroni correction, MPVP group was superior to PKRP group in IPSS and QoL (p = 0.049 and <0.001, respectively). These finding could be explained by the significant differences between both groups in IPSS and QoL at 1 month postoperatively (Fig. 1). Similar results have been reported by Deng et al. through a systematic review and meta-analysis on ThuVaRP versus PKRP14. The better QoL may have arisen from the lower overall complication rate in the MPVP group.
Both PKRP or MPVP procedures were performed with normal saline irrigation and overcame TURP’s well-known disadvantages. Nevertheless, there was one patient (1.4%) who developed fluid overloading and respiratory distress after PKRP (grade IVa complication). There was no grade IVa complications in the MPVP group.
A meta-analysis revealed that thulium vaporesection did not differ significantly from bipolar TURP in terms of complications of urethral stricture, urge incontinence, bladder neck contracture and blood transfusion14. In our study, most postoperative complications in the MPVP group were mild and occurred within first 30 days: urinary tract infection (UTI) and re-catheterization (6.8% and 9.5%, respectively). Conversely, grade II complications in the PKRP group were higher: clot retention, persistent hematuria, recurrent UTI, and dysuria or perineal pain (7.0%, 8.4%, 7.0% and 5.6%, respectively; p > 0.05). There were 5 cases (7.0%) in the PKRP group that developed bladder neck contracture, residual adenoma or urethra stricture requiring re-operation (grade IIIb complications); only one patient needed re-operation in the MPVP group. The overall complication rate was significantly higher in the PKRP group (45.0% vs. 21.9%, p = 0.004).
There were several limitations in this study. First, the case number was limited. The power analyses showed the power of the primary outcomes, IPSS and Qmax, was strong enough to detect a significant difference, instead of the other two variables, PVR and QoL. This results could be a reference for the randomized trial in the future. Second, a lack of randomization may compromise the results in view of evidence medicine; thus, patients selection bias dose exist. Third, surgeon’s experience may significantly affect the outcomes, especially the complications. The two surgeons in this study were board-certificated urologist and had more than eight years of experience in performing transurethral prostatectomies with laser or electrocauteries in over 800 cases.
Conclusion
MPVP and PKRP provided comparable symptomatic improvements. MPVP, combining thulium and diode laser energy, showed better hemostasis, shorter catheterization time, shorter hospital stay and less complications compared to PKRP. It is warranted to conduct a randomized controlled study with more case number to validate these findings limited by selection bias and statistical power.
Compliance with ethical standards
Disclosures Drs Fu-Shun Hsu, Chen-Wei Chou, Hong-Chiang Chang, Yuan-Po Tu, Shing-Jia Sha, Huang-Hsin Chung, and Kuo-How Huang have no conflict of interest or financial ties to disclose.
Change history
25 November 2019
An amendment to this paper has been published and can be accessed via a link at the top of the paper.
References
Cornu, J. N. et al. A systemic review and meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic obstruction: an update. Eur Urol 67, 1066–96 (2015).
Hermann, T. R. et al. Guidelines on lasers and technologies. EAU. (2011).
Jiang, H. J. & Zhou, Y. Safety and efficacy of Thulium laser prostatectomy versus transurethral resection of prostate for treatment of benign prostate hyperplasia: a meta-analysis. LUTS. 8, 165–70 (2016).
Netsch, C. et al. A prospective, randomized trial comparing thulium vapoenucleation with holmium laser enucleation of the prostate for the treatment of symptomatic benign prostatic obstruction: perioperative safety and efficacy. World J Urol. 35, 1913–21 (2017).
Chiang, P. H. et al. Greenlight HPS laser 120-W versus diode laser 200-W vaporization of the prostate: comparative clinical experience. Lasers in Surg and Med. 42, 624–29 (2010).
Gui, S. et al. Greenlight laser vs diode laser vaporization of the prostate: 3-year results of a prospective nonrandomized study. J Endourol. 29, 449–54 (2015).
Tan, S. et al. Transurethral vaporesection of prostate: diode laser or thulium laser? Lasers Med Sci. 33, 891–97 (2018).
Elshal, A. M. et al. GreenLight Laser (XPS) photoselective vapo-enucleation versus Holmium Laser enucleation of the prostate for the treatment of symptomatic benign prostatic hyperplasia: a randomized controlled study. J Urol. 193, 927–34 (2015).
Dindo, D., Demartines, N. & Clavien, P. A. Classification of surgical complications. Ann Surg. 240, 205–13 (2004).
Myatt, A. et al. The Uro-Clavien–Dindo system—Will the limitations of the Clavien–Dindo system for grading complications of urological surgery allow modification of the classification to encourage national adoption within the UK? Br J Med Surg Urol. 5, 54–60 (2012).
Mitropoulos, D. et al. Validation of the Clavien–Dindo Grading System in Urology by the European Association of Urology Guidelines Ad Hoc Panel. Eur Urol Focus. pii: S2405-4569(17)30062 (2017).
Ahyai, S. A. et al. Meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic enlargement. Eur Urol. 58, 384–97 (2010).
Deng, Z. et al. Thulium laser vaporesection of the prostate versus traditional transurethral resection of the prostate or transurethral plasmakinetic resection of prostate for benign prostatic obstruction: a systematic review and meta-analysis. World J Urol. 36, 1355–64 (2018).
Zhang, F. et al. Thulium (Tm:YAG) laser vaporesection of prostate and bipolar transurethral resection of prostate in patients with benign prostate hyperplasia: a systematic review and meta-analysis. Urology. 79, 869–74 (2012).
Peng, B. et al. A comparative study of thulium laser resection of the prostate and bipolar transurethral plasmakinetic prostatectomy for treating benign prostatic hyperplasia. BJU Int. 111, 633–37 (2013).
Yang, Z., Wang, X. & Liu, T. Thulium laser enucleation versus plasmakinetic resection of the prostate: a randomized prospective trial with 18-month follow-up. Urology. 81, 396–400 (2013).
Lan, Y. et al. Thulium laser resection of prostate- tangerine technique in treatment of benign prostate hyperplasia. Lasers Med Sci., https://doi.org/10.1007/s10103-018-2539-0 (2018).
Barbalat, Y. et al. Evidence of the efficacy and safety of the thulium laser in the treatment of men with benign prostatic obstruction. There Adv Urol. 8, 181–91 (2016).
Xu, A. et al. A randomized trial comparing diode laser enucleation of the prostate with plasmakinetic enucleation and resection of the prostate for the treatment of benign prostatic hyperplasia. J Endourol. 27, 1254–60 (2013).
Yang, K. S., Seong, Y. K. & Kim, I. G. Initial experiences with a 980 nm diode laser for photoselective vaporization of the prostate for the treatment of benign prostatic hyperplasia. Korean J Urol. 52, 752–6 (2011).
Erol, A. et al. High power diode laser vaporization of the prostate: Preliminary results for high power diode laser vaporization of the prostate: Preliminary results for benign prostatic hyperplasia. J Urol. 192, 1078–82 (2009).
Shaker, H. S. et al. Quartz head contact laser fiber: A novel fiber for laser ablation of the prostate using the 980 nm high power diode laser. J Urol. 187, 575–9 (2012).
Zhao, C. et al. Thulium laser resection versus plasmakinetic resection of prostates in the treatment of benign prostate hyperplasia: a meta-analysis. J Laparoendo Adv Surg Tech. 26, 789–98 (2016).
Xia, S. J. et al. Thulium laser versus standard transurethral resection of the prostate: A randomized prospective trial. Eur Urol. 53, 382–9 (2008).
Rieken, M. et al. Laser vaporization of the prostate in vivo: Experience with the 150-W 980-nm diode laser in living canines. Lasers Surg Med. 42, 736–42 (2010).
Malek, R. S. et al. Greenlight photoselective 120-watt 532-nm lithium triborate laser vaporization prostatectomy in living canines. J Endourol. 23, 837–45 (2009).
DeCao, H. et al. Comparison between thulium laser resection of prostate and transurethral plasmakinetic resection of prostate or transurethral resection of prostate. Sci Rep. 7, 14542 (2015).
Fried, N. M. & Murray, K. E. High-Power thulium fiber laser ablation of urinary tissues at 1.94 nm. J Endourol. 19, 25–31 (2005).
Acknowledgements
This study is partially funded by Taiwan Maple Urological Association. This article has been proofread by Marc Anthony (The Academic Writing Education Center, National Taiwan University) and An-Chi Chen (National Chung Hsing University, Taiwan).
Author information
Authors and Affiliations
Contributions
F.S.H.: project development, data management and analysis, and manuscript writing. F.S.H., Y.P.T., H.H.C. and C.W.C.: data collection and intellectual support. C.W.C.: data management and analysis, and figures output. H.C.C.: intellectual support, revision opinions and help. S.J.S. provides technical support. K.H.H.: project development, data analysis and manuscript editing.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hsu, FS., Chou, CW., Chang, HC. et al. Comparison of Multipulse Laser Vaporesection versus Plasmakinetic Resection for Treatment of Benign Prostate Obstruction. Sci Rep 9, 6427 (2019). https://doi.org/10.1038/s41598-019-42903-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-42903-6
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.