Abstract
Helicobacter pylori (H. pylori), an established risk factor for gastric cancer, is suggested to also play a role in the development of pancreatic cancer; however, the association remains inconclusive. We examined this association among Japanese men and women. H. pylori and atrophic gastritis (AG) status were determined serologically, using blood sample collected during health checkups. A total of 20,116 subjects enrolled in the Japan Public Health Center-based Prospective Study Cohort II with available data on H. pylori seropositivity (anti-H. pylori) and AG were followed until the end of 2010. Cox proportional hazards models were used to calculate the hazard ratios (HR) and 95% confidence intervals (CI), using the information from the baseline survey. During 320,470 person-years of follow-up, 119 cases of pancreatic cancer were identified. No statically significant increase or decrease in pancreatic cancer risk was observed for H. pylori and AG status, independently or in combination. In a multivariable-adjusted model, we observed a non-significant decrease in the risk among those who had AG but were anti-H. pylori seronegative (HR 0.57, 95% CI 0.31–1.03). In a stratified analysis, we observed a statistically significant increased risk of pancreatic cancer for AG+ (HR 3.64, 95% CI 1.37–9.66), and AG+/anti-H. pylori− or AG+/anti-H. pylori+ (HR 5.21, 95% CI 1.14–23.87) among current smokers. Non-smokers in all categories of AG and anti-H. pylori showed a non-statistical decrease in the risk. There was no statistically significant interaction between H. pylori infection, AG status, and smoking status. Our findings suggest H. pylori seropositivity and AG, individually or in combination, are not associated with the risk of pancreatic cancer in a general Japanese population. Among current smokers, pancreatic cancer risk increased with AG, regardless of H. pylori infection status.
Similar content being viewed by others
Introduction
In Japan, pancreatic cancer is the fifth most common cause of cancer death, following lung, stomach, colorectal, and liver1. Due to the location of the pancreas, early diagnosis is not easy compared to other digestive tract cancers, which might explain its poor survival rate2,3. Pancreatic cancer incidence and death rates increase with age, with a sharp rise after 652.
Age, cigarette smoking and a history of diabetes are the most known risk factors for pancreatic cancer4. Although no definite protective factors have been found, intake of fruits and vegetables, and physical exercise are possibly protective5. Some studies have shown possible etiological similarities between pancreatic and gastric cancers6,7,8. Helicobacter pylori (H. pylori) has recently been considered as another possible candidate risk factor for pancreatic cancer. This agent has been declared a group 1 carcinogen by the International Agency for Research on Cancer (IARC), and infection has been found to be strongly associated with the development of gastric-associated diseases, such as peptic ulcer disease and gastric cancer9. However, H. pylori’s role in the development of pancreatic cancer remains inconclusive10,11,12,13. One meta-analysis in 2013 including 9 studies showed a 47% increase (summary odds ratio (OR) 1.47, 95% confidence interval (CI) 1.22–1.77) among H. pylori infected individuals and pancreatic cancer risk14, while a recent meta-analysis including 10 large case-control studies found no significant association15. Some previous studies even suggested the possibility of H. pylori having a protective effect, particularly infection by cytotoxin-associated gene A (CagA) seropositive H. pylori strains, for pancreatic cancer risk16,17.
Atrophic gastritis (AG) is a chronic condition characterized by long-term inflammation of the stomach18,19. H. pylori infection, autoimmune pernicious anaemia, long-term proton pump inhibitor therapy are established etiological risk factors for AG18. It has been hypothesised that AG may also be associated with an increased risk of pancreatic cancer through a low-acid production mechanism, leading to bacterial overgrowth, enhancing the promotion of nitroso-compounds19. A previous meta-analysis conducted in 2017 could not confirm the association between AG and pancreatic cancer risk but suggested the possibility that the risk may be increasing among the population with AG but are not infected by H. pylori20.
Given that global ageing trend is likely to continue, investigation of the risk factors for pancreatic cancer is beneficial for better prevention and prediction of the disease. This study aimed to investigate the association between H. pylori infection and its related condition, AG, and the pancreatic cancer risk in a Japanese population, using a large-scale prospective study.
Materials and Methods
Study population
The study was conducted using the Japan Public Health Center-based Prospective Study (JPHC Study) Cohort II. This cohort was launched in 1993–1994 including with 78,825 Japanese residents (38,740 men and 40,085 women) aged 40–69 years at the beginning of the baseline survey from 6 public health center areas all over Japan21. Details of the study design have been described elsewhere21. The study protocol was approved by the institutional review board of the National Cancer Center, Japan (Approval Number: 2001–021) and The University of Tokyo (approval number: 10508). All methods used in this study were performed by the relevant guidelines and regulations.
Baseline survey
A self-administered questionnaire regarding lifestyle factors was completed at the baseline of the cohort. The participants were informed of the objectives of the study, and those who completed the survey questionnaire were regarded as consenting to participate in the study. Figure 1 shows the study particpants selection process. Of 78,825 participants at the baseline, participants from one public health center area (Suita, n = 9,747) were excluded due to the unavailability of complete cancer data. We excluded foreign nationals (n = 22), move out of the study area before the study starting point (n = 82), missing age (n = 1), duplicates (n = 4), or those with inadequate follow-up data (n = 81). We further excluded individuals who had died, moved out of the study area, or had an unknown date of diagnosis before the starting point (n = 6,969), and non-respondents to the baseline questionnaire (n = 5,706). Among those who responded to the baseline questionnaire, 38% (n = 21,329) voluntarily provided 10 mL of blood during health checkups provided by their local government. Samples were divided into four tubes for plasma and buffy layer and stored at −80 °C until analysis. Subjects who reported a history of any cancer (n = 1,213) were excluded from the study, leaving 20,116 individuals (7,316 men and 12,800 women) for the analysis.
Laboratory analysis
H. pylori infection and AG were defined using biomarkers H. pylori seropositivity (anti-H. pylori) and pepsinogen (PG) I and II respectively. Levels of Immunoglobin G (IgG) were measured using an enzyme immunoassay (E Plate “Eiken” H. pylori Antibody II; Eiken Kagaku, Tokyo, Japan)22. An IgG titer of anti-H. pylori ≥10 U/mL was considered H. pylori seropositivy22. The latex agglutination technique was used to determine the plasma levels of PG I and II (LZ test “Eiken” Pepsinogen I, II; Eiken Kagaku, Tokyo, Japan)22. A subject was defined as AG-positive if PG I ≤70 ng/mL, and PG I/II ratio ≤3.022. Miki conducted a meta-analysis in 200623 for the sensitivity and specificity of the serum pepsinogen test method using results from 42 studies. The combined sensitivity and false-positive rates for PGI ≤70 ng/mL and PG I:II ratio ≤3.0 were 77% and 27%, respectively23. The positive predicted value ranged from 0.77% to 1.25%, while the negative predictive value varied from 99.08% and 99.90%23. CagA seropositivity was not examined due to limited availability of stored blood samples. Using these criteria, the study subjects were further divided into three groups according to a combination of AG status and anti-H. pylori; AG-negative and H. pylori seronegative (AG−/ anti-H. pylori−); AG-negative and H. pylori seropositive (AG−/anti-H. pylori+); AG-positive and H. pylori seropositive (AG+/anti-H. pylori+).
Follow-up and identification of pancreatic cancer cases
Subjects were followed from the date of the baseline survey until December 31st, 2010. Residence and survival status of the subjects was confirmed through the residential registry. The incidence of pancreatic cancer was identified through active patient notification from major local hospitals in each study area and linking with population-based cancer registries. Death certificates were used to supplement the information on cancer incidence. Cases of pancreatic cancer were classified using the International Classification of Diseases for Oncology, 3rd edition, code C2524.
Statistical analysis
Study participants were censored on the date of pancreatic cancer diagnosis, move-out from the study area, death, or December 31st, 2010, whichever came first. Subjects’ characteristics at the baseline were compared independently by anti-H. pylori and AG status, and also by a combination of the two biomarkers. Differences in baseline characteristics between anti-H. pylori and AG status were analyzed using analysis of variance or χ2-test. Cox proportional hazards regression models were used to estimate the hazard ratios (HRs) and their 95% CI using attained age as the time scale due to the strong association between pancreatic cancer risk and age. Participants who tested negative to the biomarkers at the baseline of the study were used as the reference group. Covariates included were based in associations found in previous studies25. Model 1 adjusted for public health center areas (six areas treated as strata) and gender, while model 2 further adjusted for body-mass index (BMI) calculated using measured height and weight (<25.0 kg/m2, ≥25.0–<27.0 kg/m2, ≥27.0 kg/m2), self-reported history of diabetes (yes, no), self-reported physical activity (continuous, metabolic equivalent of task (METs)), self-reported alcohol consumption (never and formal, occasional, <150 g/week, ≥150 g/week), self-reported family history of pancreatic cancer (yes, no), and self-reported smoking status (never, former, current), in addition to the confounders in model 1. We conducted individual stratified analyses for each pancreatic cancer risk factors to see how H. pylori seropositivity and AG status affected the pancreatic cancer risk differently according to lifestyle habits. Interactions were considered between H. pylori infection, AG status and each of the covariates included in the analysis by running a regression model with an interaction term, then conducting a Wald test for interaction. All analyses were conducted using Stata version 13.0 (StataCorp LP).
Results
During 320,470 person-years of follow-up (mean 16 years), 119 cases (52 men and 67 women) of newly diagnosed pancreatic cancer were identified among 20,116 subjects. Table 1 shows the baseline characteristics of cohort participants by H. pylori seropositivity and AG categories. We combined never-and past- alcohol drinkers due to a small number of participants in past drinker category (n = 383, 1.9% of the total participants). Men represented 36% of the total participants. AG−/anti-H. pylori+ category had the highest percentage of men (39.1%), habitual drinkers (≥150 g of ethanol per week, 15.5%), and current smokers (18.3%). In all categories, the majority of the subjects were within normal BMI range (<25 kg/m2). At the baseline, 13,752 subjects (68%) and 8,470 (42%) were found to be anti-H. pylori seropositive and AG positive, respectively. Mean PGI value for our study was 53.4 ± 29.0 ng/mL; minimum PGI value observed was 2 ng/mL and the maximum PGI value was 606.4 ng/mL.
Table 2 shows the HR and 95% CI for anti-H. pylori and AG status and the risk of pancreatic cancer, using attained age as a time scale. Those who tested negative to each agent were used as a reference. AG is considered the endpoint of chronic gastritis caused by H. pylori infection26; therefore, AG+/anti-H. pylori− category was combined with AG+/anti-H. pylori+ category.
No statistical association was found between AG and anti-H. pylori status and pancreatic cancer risk, even when the model was adjusted for potential confounders. A borderline decrease in risk was observed among AG−/H. pylori+ subjects (HR 0.57, 95% CI 0.31–1.03).
Table 3 shows the association between H. pylori infection and the risk of pancreatic cancer by individually stratifying for smoking status, alcohol consumption, BMI, and history of diabetes. Among current smokers, we saw a statistically significant increase in the risk of pancreatic cancer for AG+ (HR 3.64, 95% CI 1.37–9.66) and AG+/anti-H. pylori− or AG+/anti-H. pylori+ subjects (HR 5.21, 95% CI 1.14–23.87). There were no statistically significant interactions between H. pylori infection, AG status, smoking status, alcohol consumption, BMI and history of diabetes.
Discussion
To best of our knowledge, this is the first prospective cohort study to investigate H. pylori infection status and the risk of pancreatic cancer incidence in a Japanese population. When stratified by smoking status, the risk of pancreatic cancer among current smokers with AG statistically increased, regardless of H. pylori infection status.
We observed a non-statistically significant decrease in the risk of pancreatic cancer for AG−/anti-H. pylori+ subjects. Although the exact mechanism of how H. pylori seropositivity lowers pancreatic cancer risk is unclear, one hypothesis proposed suggests suppression of appetite by H. pylori infection leading to a reduction of ghrelin, ultimately lowering body weight, reducing cases of pancreatic cancer caused by obesity27.
Another possibility is the infection by CagA seropositive H. pylori strains may be working as a protective factor for pancreatic cancer development. Risch et al.16 showed a statistically significant risk decrease for pancreatic cancer among H. pylori and CagA seropositive in a Chinese population (OR 0.66, 95% CI 0.53–0.81). A meta-analysis conducted based on 2,049 cases and 2,861 controls also showed a reduction in pancreatic cancer risk among those who are infected with H. pylori (summary OR 0.62, 95% CI 0.49–0.76) and CagA seropositive (summary OR 0.66, 95% CI 0.52–0.80) in Asian population28. Evidence from mouse models have suggested SHP-2, a tyrosine phosphate expressed in most embryonic and adult tissues and an intracellular target of H. pylori CagA protein, may be regulating glucose and lipid metabolism by suppressing insulin signalling in hepatocytes29, suppressing tumour proliferation in the pancreas. Eradication of CagA seronegative H. pylori among patients with duodenal ulcer returns their hyperchlorhydria to normal30,31; in contrast, eradication of CagA seropositive H. pylori among corpus AG patients returns the stomach environment to hypo- or achlorhydria to normal32. Since gastric acidity promotes secretion of bicarbonate and fluid from pancreatic ductal cells33, it allows CagA seronegative H. pylori to survive in pancreatic ductular epithelium16. An animal model has shown that excess production of pancreatic bicarbonate and fluid increased the ductular cell dysplasia and adenocarcinoma34. This suggests the possibility of difference in gastritis acidity caused by H. pylori stains may affect in the pancreatic cancer risk16. However, because we could not measure CagA seropositivity due to limited availability of stored blood samples, we were not able to test the hypothesis.
Stratified analysis by established pancreatic cancer risk factors showed a statistically significant increase in the pancreatic cancer risk among current smokers with AG. This result is inconsistent with a previous Finnish cohort study that recruited current male smokers to look at the association between AG and pancreatic cancer and found no association, whether AG was diagnosed serologically or histologically19. Serum PG levels are known to be affected depending on demographic characteristics such as gender, age, smoking, alcohol consumption, and dietary habits35, leading to various cut-off values of serum PG depending on populations. In our study, we used the threshold for defining a high-risk population in Japan36 (PGI ≤ 70 ng/mL and a ratio of PGI and PGII ≤ 3), proposed by Miki et al.23,37,38, to define AG. In European nations, the often used serum PGI cut-off value is ≤25 ng/mL, with a ratio of PGI and PGII < 339. It is possible that the differences in the findings between countries are due to the difference in PGI cut-offs used to define AG.
No epidemiological evidence has been found to clarify how AG is associated with pancreatic cancer risk. Truan et al.40 found pepsinogen expression in 38% pancreatic cancer cases, while another study found that gastrin, a gastrointestinal peptide, had a proliferative effect on pancreatic cancer cells41. AG is often caused by H. pylori infection42,43,44. The amount of H. pylori present in the stomach reduces as intestinal metaplasia develop, spreading in the presence of chronic AG45,46,47, resulting in a negative result in the antibody test48. IgG anti-H. pylori seronegative status among those who are AG positive implies prior H. pylori infection, since H. pylori cannot survive in the atrophic or intestinal metaplasia mucosa49. Previous studies have shown those with advanced gastritis with loss of H. pylori are at a higher risk of developing gastric cancer48,49. This may be the reason why the increased risk for pancreatic cancer was observed among AG positive but H. pylori negative individuals in a previous study20. AG therefore may have a causative effect on pancreatic cancer development, through the extra-gastric or systemic effect of H. pylori19.
A major strength of this study is its prospective cohort design, with subjects recruited from a large sample of the general population. The high response rate and low loss to follow-up increased the generalizability of the conclusions and reduced selection bias. We used the incidence of pancreatic cancer as an endpoint rather than death since it directly measured the risk of pancreatic cancer. Finally, because the H. pylori infection rate in the Japanese population is high for those born prior to 1950 (over 70%)50, the country provides a suitable setting for examining the association of H. pylori, AG, and pancreatic cancer.
There are several limitations. The cases of pancreatic cancer found during the follow up period were relatively small (n = 119). However, we believe that with an average of 16 years of follow-up, sufficient numbers of pancreatic cancer cases were identified. Furthermore, because the development of pancreatic cancer is a rare event (Age-standardized rate per 100,000: 9.7)51, the incidence observed during this study period is believed to be acceptable. We also had to exclude 34,965 subjects from the analysis since they did not provide a blood sample, and therefore their H. pylori and AG status could not be observed. Men comprised 36% of the study population, which may have led to a gender-biased result. H. pylori infection status was defined using serum antibody-based tests, which are relatively inexpensive, rapidly performed, and cause minimal discomfort to the subjects52. However, one of the limitations of using serology test is its inability to differentiate between past and present H. pylori infections53. Although H. pylori infection is said to be associated with low socioeconomic status (SES)54, due to the unavailability of the data, we were not able to include SES into our analysis. This study also did not consider blood group antigens, a potential risk factor for pancreatic cancer incidence reported by several studies including a study conducted by Wolpin et al.55, which reported compared to those with blood type O, blood type A and B have a significantly increased risk for pancreatic cancer. Finally, the association may have been confounded by additional unmeasured or unknown risk factors.
In summary, H. pylori infection and AG was not associated with the risk of pancreatic cancer in a general Japanese population, individually or in combination; however, among current smokers with AG, a significant increase in the risk of pancreatic cancer was observed. Further investigation in larger cohorts, especially in Asian countries, will provide a more comprehensive evaluation.
Change history
28 July 2020
An amendment to this paper has been published and can be accessed via a link at the top of the paper.
References
Hori, M. et al. Cancer incidence and incidence rates in Japan in 2009: a study of 32 population-based cancer registries for the Monitoring of Cancer Incidence in Japan (MCIJ) project. Jpn J Clin Oncol 45, 884–891, https://doi.org/10.1093/jjco/hyv088 (2015).
Cancer Facts & Figures 2013. (American Cancer Society 2013).
Lowenfels, A. B. & Maisonneuve, P. Epidemiology and Prevention of Pancreatic Cancer. Japanese Journal of Clinical Oncology 34, 238–244, https://doi.org/10.1093/jjco/hyh045 (2004).
Maisonneuve, P. & Lowenfels, A. B. Epidemiology of pancreatic cancer: an update. Digestive diseases (Basel, Switzerland) 28, 645–656, https://doi.org/10.1159/000320068 (2010).
Maisonneuve, P. & Lowenfels, A. B. Risk factors for pancreatic cancer: a summary review of meta-analytical studies. International journal of epidemiology 44, 186–198, https://doi.org/10.1093/ije/dyu240 (2015).
Franceschi, F., Zuccala, G., Roccarina, D. & Gasbarrini, A. Clinical effects of Helicobacter pylori outside the stomach. Nature reviews. Gastroenterology & hepatology 11, 234–242, https://doi.org/10.1038/nrgastro.2013.243 (2014).
Luo, J. et al. Body mass index, physical activity and the risk of pancreatic cancer in relation to smoking status and history of diabetes: a large-scale population-based cohort study in Japan–the JPHC study. Cancer Causes Control 18, 603–612, https://doi.org/10.1007/s10552-007-9002-z (2007).
Sessa, F. et al. Ductal cancers of the pancreas frequently express markers of gastrointestinal epithelial cells. Gastroenterology 98, 1655–1665 (1990).
Yang, J. C., Lu, C. W. & Lin, C. J. Treatment of Helicobacter pylori infection: current status and future concepts. World journal of gastroenterology: WJG 20, 5283–5293, https://doi.org/10.3748/wjg.v20.i18.5283 (2014).
Lindkvist, B., Johansen, D., Borgstrom, A. & Manjer, J. A prospective study of Helicobacter pylori in relation to the risk for pancreatic cancer. BMC cancer 8, 321, https://doi.org/10.1186/1471-2407-8-321 (2008).
de Martel, C. et al. Helicobacter pylori infection and development of pancreatic cancer. Cancer epidemiology, biomarkers & prevention: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive. Oncology 17, 1188–1194, https://doi.org/10.1158/1055-9965.epi-08-0185 (2008).
Risch, H. A., Yu, H., Lu, L. & Kidd, M. S. ABO blood group, Helicobacter pylori seropositivity, and risk of pancreatic cancer: a case-control study. Journal of the National Cancer Institute 102, 502–505, https://doi.org/10.1093/jnci/djq007 (2010).
Haarstad, H. & Petersen, H. Short- and long-term effects of secretin and a cholecystokinin-like peptide on pancreatic growth and synthesis of RNA and polyamines. Scandinavian journal of gastroenterology 24, 721–732 (1989).
Xiao, M., Wang, Y. & Gao, Y. Association between Helicobacter pylori infection and pancreatic cancer development: a meta-analysis. PLoS One 8, e75559 (2013).
Schulte, A. et al. Association between Helicobacter pylori and pancreatic cancer risk: a meta-analysis. Cancer Causes & Control 26, 1027–1035, https://doi.org/10.1007/s10552-015-0595-3 (2015).
Risch, H. A. et al. Helicobacter pylori seropositivities and risk of pancreatic carcinoma. Cancer Epidemiology and Prevention Biomarkers 23, 172–178 (2014).
Chen, X. Z., Wang, R., Chen, H. N. & Hu, J. K. Cytotoxin-Associated Gene A-Negative Strains of Helicobacter pylori as a Potential Risk Factor of Pancreatic Cancer: A Meta-Analysis Based on Nested Case-Control Studies. Pancreas 44, 1340–1344, https://doi.org/10.1097/mpa.0000000000000414 (2015).
Huang, J. et al. Helicobacter pylori infection, chronic corpus atrophic gastritis and pancreatic cancer risk in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort: A nested case-control study. International journal of cancer 140, 1727–1735, https://doi.org/10.1002/ijc.30590 (2017).
Laiyemo, A. O. et al. Serum Pepsinogen level, Atrophic Gastritis and the Risk of Incident Pancreatic Cancer – a Prospective Cohort Study. Cancer Epidemiol 33, 368–373, https://doi.org/10.1016/j.canep.2009.09.001 (2009).
Liu, H., Chen, Y.-T., Wang, R. & Chen, X.-Z. Helicobacter pylori infection, atrophic gastritis, and pancreatic cancer risk: A meta-analysis of prospective epidemiologic studies. Medicine 96, e7811–e7811, https://doi.org/10.1097/MD.0000000000007811 (2017).
Tsugane, S. & Sawada, N. The JPHC Study: Design and Some Findings on the Typical Japanese Diet. Japanese Journal of Clinical Oncology 44, 777–782, https://doi.org/10.1093/jjco/hyu096 (2014).
Charvat, H. et al. Prediction of the 10-year probability of gastric cancer occurrence in the Japanese population: the JPHC study cohort II. Int J Cancer, https://doi.org/10.1002/ijc.29705 (2015).
Miki, K. Gastric cancer screening using the serum pepsinogen test method. Gastric Cancer 9, 245–253, https://doi.org/10.1007/s10120-006-0397-0 (2006).
Fritz, A. International classification of diseases for oncology: ICD-O 3rd edn, (World Health Organization, 2000).
Krull Abe, S. et al. Hepatitis B and C Virus Infection and Risk of Pancreatic Cancer: A Population-Based Cohort Study (JPHC Study Cohort II). Cancer Epidemiol Biomarkers Prev 25, 555–557, https://doi.org/10.1158/1055-9965.EPI-15-1115 (2016).
Arkkila, P. E., Seppala, K., Farkkila, M. A., Veijola, L. & Sipponen, P. Helicobacter pylori eradication in the healing of atrophic gastritis: a one-year prospective study. Scandinavian journal of gastroenterology 41, 782–790, https://doi.org/10.1080/00365520500463175 (2006).
Wren, A. M. & Bloom, S. R. Gut hormones and appetite control. Gastroenterology 132, 2116–2130, https://doi.org/10.1053/j.gastro.2007.03.048 (2007).
Wang, Y., Zhang, F. C. & Wang, Y. J. Helicobacter pylori and pancreatic cancer risk: a meta- analysis based on 2,049 cases and 2,861 controls. Asian Pacific journal of cancer prevention: APJCP 15, 4449–4454 (2014).
Coulombe, G. & Rivard, N. New and Unexpected Biological Functions for the Src-Homology 2 Domain-Containing Phosphatase SHP-2 in the Gastrointestinal Tract. Cellular and molecular gastroenterology and hepatology 2, 11–21, https://doi.org/10.1016/j.jcmgh.2015.11.001 (2016).
Moss, S. F. & Calam, J. Acid secretion and sensitivity to gastrin in patients with duodenal ulcer: effect of eradication of Helicobacter pylori. Gut 34, 888–892 (1993).
Parente, F. et al. Behaviour of acid secretion, gastrin release, serum pepsinogen I, and gastric emptying of liquids over six months from eradication of helicobacter pylori in duodenal ulcer patients. A controlled study. Gut 37, 210–215 (1995).
Haruma, K. et al. Eradication of Helicobacter pylori increases gastric acidity in patients with atrophic gastritis of the corpus-evaluation of 24-h pH monitoring. Alimentary pharmacology & therapeutics 13, 155–162 (1999).
Risch, H. A. Etiology of pancreatic cancer, with a hypothesis concerning the role of N-nitroso compounds and excess gastric acidity. Journal of the National Cancer Institute 95, 948–960 (2003).
Howatson, A. G. & Carter, D. C. Pancreatic carcinogenesis: effect of secretin in the hamster-nitrosamine model. JNCI: Journal of the National Cancer Institute 78, 101–105 (1987).
Kim, H. Y. et al. Clinical meaning of pepsinogen test and Helicobacter pylori serology in the health check-up population in Korea. Eur J Gastroenterol Hepatol 21, 606–612, https://doi.org/10.1097/MEG.0b013e3283086757 (2009).
Watanabe, Y. et al. Helicobacter pylori infection and gastric cancer (A nested case-control study in a rural area of Japan). Digestive diseases and sciences 42, 1383–1387 (1997).
Miki, K. Gastric cancer screening by combined assay for serum anti-Helicobacter pylori IgG antibody and serum pepsinogen levels—“ABC method”. Proceedings of the Japan Academy, Series B 87, 405–414 (2011).
Miki, K. et al. Serum pepsinogens as a screening test of extensive chronic gastritis. Gastroenterologia Japonica 22, 133–141 (1987).
Sipponen, P. & Graham, D. Y. Importance of atrophic gastritis in diagnostics and prevention of gastric cancer: application of plasma biomarkers. Scandinavian journal of gastroenterology 42, 2–10, https://doi.org/10.1080/00365520600863720 (2007).
Truan, N. et al. Expression and clinical significance of pepsinogen C in resectable pancreatic cancer. The International journal of biological markers 16, 31–36 (2001).
Smith, J. P., Fantaskey, A. P., Liu, G. & Zagon, I. S. Identification of gastrin as a growth peptide in human pancreatic cancer. The American journal of physiology 268, R135–141, https://doi.org/10.1152/ajpregu.1995.268.1.R135 (1995).
Kuipers, E. J., Pérez-Pérez, G. I., Meuwissen, S. G. M. & Blaser, M. J. Helicobacter pylori and Atrophic Gastritis: Importance of the cagA Status. JNCI: Journal of the National Cancer Institute 87, 1777–1780, https://doi.org/10.1093/jnci/87.23.1777 (1995).
Kuipers, E. J. et al. Long-term sequelae of Helicobacter pylori gastritis. Lancet (London, England) 345, 1525–1528 (1995).
Asaka, M. et al. Relationship between Helicobacter pylori infection, atrophic gastritis and gastric carcinoma in a Japanese population. Eur J Gastroenterol Hepatol 7(Suppl 1), S7–10 (1995).
Sipponen, P., Kosunen, T., Valle, J., Riihelä, M. & Seppälä, K. Helicobacter pylori infection and chronic gastritis in gastric cancer. Journal of clinical pathology 45, 319–323 (1992).
Karnes, W. et al. Positive serum antibody and negative tissue staining for Helicobacter pylori in subjects with atrophic body gastritis. Gastroenterology 101, 167–174 (1991).
Farinati, F. et al. Prevalence of Helicobacter pylori infection in patients with precancerous changes and gastric cancer. European journal of cancer prevention: the official journal of the European Cancer Prevention Organisation (ECP) 2, 321–326 (1993).
Ohata, H. et al. Progression of chronic atrophic gastritis associated with Helicobacter pylori infection increases risk of gastric cancer. International Journal of Cancer 109, 138–143, https://doi.org/10.1002/ijc.11680 (2004).
Mizuno, S. et al. Prescreening of a high-risk group for gastric cancer by serologically determined Helicobacter pylori infection and atrophic gastritis. Digestive diseases and sciences 55, 3132–3137 (2010).
Shiota, S., Murakawi, K., Suzuki, R., Fujioka, T. & Yamaoka, Y. Helicobacter pylori infection in Japan. Expert review of gastroenterology &. hepatology 7, 35–40, https://doi.org/10.1586/egh.12.67 (2013).
Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians 68, 394–424, https://doi.org/10.3322/caac.21492 (2018).
Raj, P., Thompson, J. F. & Pan, D. H. Helicobacter pylori serology testing is a useful diagnostic screening tool for symptomatic inner city children. Acta paediatrica (Oslo, Norway: 1992) 106, 470–477, https://doi.org/10.1111/apa.13724 (2017).
Oderda, G. et al. Eighteen month follow up of Helicobacter pylori positive children treated with amoxycillin and tinidazole. Gut 33, 1328–1330 (1992).
Brown, L. M. Helicobacter pylori: epidemiology and routes of transmission. Epidemiologic reviews 22, 283–297 (2000).
Wolpin, B. M. et al. ABO blood group and the risk of pancreatic cancer. J Natl Cancer Inst 101, 424–431, https://doi.org/10.1093/jnci/djp020 (2009).
Acknowledgements
This paper is a part of Japan Public Health Center-based Prospective Study. The full JPHC Study Group members are listed at the following: https://epi.ncc.go.jp/en/jphc/781/7951.html. We would like to thank the Ibaraki, Niigata, Kochi, Nagasaki, Okinawa and Osaka Cancer Registries for providing their incidence data. This work was funded by the National Cancer Center Research and Development Fund [23-A-31(toku), 26-A-2. 29-A-4] and Kiban A: Burden of Disease Fund [25253051].
Author information
Authors and Affiliations
Contributions
M.I. designed the research. M.H. performed the analysis, prepared the tables and drafted the paper. M.I., E.S. and S.K.A. supported analysis and finalization the paper. N.S., E.S., S.K.A., A.H., M.Iw., T.Y., T.S., S.T. and M.I. substantially contributed to the discussion and interpretation of the findings. All authors read and approved the final manuscript. Mayo Hirabayashi is a fellow of Ministry of Education, Culture, Sports, Science and Technology’s Leading Graduate Schools Program, Global Leader Program for Social Design and Management (GSDM). GSDM played no role in the design, data collection, analysis, interpretation or manuscript drafting, or in the decision to submit the manuscript for publication.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
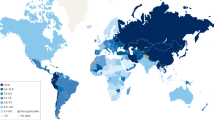
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hirabayashi, M., Inoue, M., Sawada, N. et al. Helicobacter pylori infection, atrophic gastritis, and risk of pancreatic cancer: A population-based cohort study in a large Japanese population: the JPHC Study. Sci Rep 9, 6099 (2019). https://doi.org/10.1038/s41598-019-42365-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-42365-w
This article is cited by
-
The impact of the human microbiome in tumorigenesis, cancer progression, and biotherapeutic development
BMC Microbiology (2022)
-
Association Between Helicobacter pylori and Periampullary and Pancreatic Cancer: a Case–Control Study
Journal of Gastrointestinal Cancer (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.