Abstract
Glaucoma leads to irreversible blindness. Numerous anti-glaucoma eye drops have been developed. Unfortunately, many patients with glaucoma still suffer from progressive visual disorders. Recently, ripasudil hydrochloride hydrate, a selective Rho-associated protein kinase inhibitor, was launched for the treatment of glaucoma. However, adverse events, such as conjunctival hyperemia, are often noted in clinical trials using healthy subjects. Therefore, we investigated the onset, offset, and kinetic changes of conjunctival hyperemia induced by ripasudil ophthalmic solution in patients with open-angle glaucoma or ocular hypertension who had already been treated with anti-glaucoma eye drops other than ripasudil. Conjunctival hyperemia was evaluated by both clinical grading by 3 ophthalmic physicians and pixel coverage of conjunctival blood vessels determined by conjunctival hyperemia-analyzing software. Conjunctival hyperemia appeared within 10 min post-instillation in most of the participants. Clinical grade and pixel coverage increased significantly 10 min post-instillation and then decreased. In most of the participants, hyperemia resolved within 2 h. Median conjunctival hyperemia offset was 90 min. A tendency of monotonic increase was observed between clinical grade and pixel coverage. Taken altogether, hyperemia induced by ripasudil was transient in glaucoma patients who had already been treated with anti-glaucoma eye drops other than ripasudil.
Similar content being viewed by others
Introduction
Glaucoma can cause irreversible blindness, so numerous anti-glaucoma eye drops have been developed. Unfortunately, many patients with glaucoma still suffer from progressive visual defects and vision disorders. There are various types of glaucoma, and it is known to be a multifactorial disease. The most important risk factor for progression is intraocular pressure (IOP), followed by aging, family history, myopia, and low cerebrospinal fluid pressure. At the present, there are no effective treatments other than lowering IOP by instilling eye drops, surgery, or laser procedures.
Rho-associated protein kinase (ROCK) inhibitors lower IOP1,2,3 and are also associated with adverse events; most frequently, conjunctival hyperemia1,2,3. A phase 1 clinical trial of a selective ROCK inhibitor (K-115) found kinetic changes in conjunctival hyperemia at 0.5, 2, 4, 8, and 9 h post-instillation in 50 healthy volunteers4. Conjunctival hyperemia was observed at 30 min post-instillation at different K-115 concentrations (0.05%, 0.1%, 0.2%, 0.4% and 0.8%). IOP decreased 1–2 h after a single instillation of K-115. Slight to mild conjunctival hyperemia was found in more than half of the participants treated with K-115, after each instillation, and spontaneously resolved within 4 h. Further, conjunctival hyperemia was observed at various time-points and concentrations, and resolved spontaneously within 4 h, except for 0.8% ripasudil. However, changes in conjunctival hyperemia, observed up to 30 min post-instillation, have not been evaluated.
In December 2014, ripasudil hydrochloride hydrate, a selective ROCK inhibitor (GLANATECR, ophthalmic solution 0.4%: K-115, KOWA Company. Ltd., Nagoya, Japan) was launched as an anti-glaucoma treatment in Japan. A recent clinical trial with 51 healthy participants investigated changes in conjunctival hyperemia and reduction of IOP within 2 h (at 5, 15, 30, 60, 120 min) post-instillation of 0.4% ripasudil5. Here, conjunctival hyperemia peaked 5–15 min post-instillation and resolved within 2 h. IOP values decreased between 30 min and 2 h post-instillation, regarding healthy participants. However, ripasudil-induced changes in conjunctival hyperemia over time have not been investigated in patients with glaucoma, who were previously treated with anti-glaucoma eye drops, other than ripasudil. In the present study, we evaluated the offset of conjunctival hyperemia, induced by ripasudil, in patients with open-angle glaucoma or ocular hypertension (OHT).
Results
Study Participants
A total of 50 participants were enrolled in this trial, between September 16, 2015 and June 30, 2017. Demographic variables including sex, type of glaucoma, and prior medications are shown in Table 1.
Primary endpoint
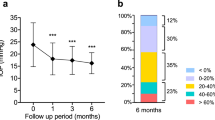
Clinical grades were used to determine the presence of, and changes in, conjunctival hyperemia. For the primary endpoint, we excluded 8 participants because were unable to induce conjunctival hyperemia by ripasudil. Therefore, data from 42 cases (16 males and 26 females) were analyzed. The mean age was 67.7 years (range: 24–86 years). The median offset time of conjunctival hyperemia, according to clinical grade, was 90 min, with a 95% confidence interval of 60 to 120 min post-instillation of ripasudil. Most frequently, conjunctival hyperemia disappeared within 60 min post-instillation (Fig. 1).
Primary endpoint of conjunctival hyperemia offset time based on clinical grade. The horizontal axis represents the offset time of conjunctival hyperemia induced post-instillation of ripasudil. The vertical axis represents the number of cases within each group. The median time conjunctival hyperemia offset, as per clinical grading, was 90 min and the 95% confidence interval was 60 to 120 min post-instillation of ripasudil.
In the group with the offset time within 60 min, the proportion of the participants that had been treated with prostaglandin analogs (PG) alone (PG Mono) was significantly higher than that with β-blocker (Table 2). On the contrary, in the group with the offset time of 180 min or over, the proportion of the participants that had been treated with β-blocker was significantly higher than that with PG Mono (Fisher’s exact test, P = 0.02) (Table 2).
Secondary endpoints
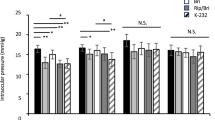
Differences compared with baseline data regarding clinical grade, the value of pixel coverage on conjunctival blood vessels, and IOP values within 180 min post-instillation are shown in Fig. 2. Clinical grade score significantly increased at 10 min, 60 min, and 90 min post-instillation compared with baseline (**P < 0.01). Then, compared to 10 min post-instillation, clinical grade score significantly decreased after 60 min, 90 min, 120 min, and 180 min (††P < 0.01). The clinical grade score was minimal at 120 min post-instillation (Fig. 2A).
The kinetic changes of clinical grade score, the value of pixel coverage on conjunctival blood vessels, and IOP measurements. The vertical axis of the upper graph shows the mean difference from baseline ± SD regarding clinical grade at each time point. The clinical grade peaked 10 min post-instillation and was at its minimum 120 min post-instillation (A). The vertical axis of the middle graph shows the mean difference from baseline ± SD regarding value of pixel coverage on conjunctival blood vessels (%). Pixel coverage values peaked 10 min post-instillation and was at its minimum 180 min post-instillation (B). The vertical axis of the lower graph shows the mean difference from baseline ± SD regarding IOP value at each time point. IOP decreased significantly at all time points after 60 min, compared to IOP values at baseline. The lowest IOP value was 90 min post-instillation (C). **P < 0.01 (Paired t-test) versus the corresponding value for before instillation as baseline, ††P < 0.01 (Paired t-test) versus the corresponding value for 10 min post-instillation.
The value of pixel coverage on conjunctival blood vessels significantly increased at 10 min post-instillation compared with baseline (**P < 0.01). Then, compared to 10 min post-instillation, the value of pixel coverage significantly decreased after 60 min, 90 min, 120 min, and 180 min (††P < 0.01). The value of pixel coverage was minimal at 180 min post-instillation (Fig. 2B).
Compared to baseline, IOP decreased after 60 min, 90 min, 120 min and 180 min, and significant differences were noted except for 10 min (**P < 0.01). Then, compared to 10 min post-instillation, IOP decreased after 60 min, 90 min, 120 min, and 180 min (††P < 0.01) (Fig. 2C).
A tendency of monotonic increase was observed between clinical grade and pixel coverage of conjunctival blood vessels (P < 0.01, Jonckheere-Terpstra Trend Test, one-tailed test) (Fig. 3).
The correlation between clinical grade and pixel coverage value on the conjunctival blood vessels. This box-whisker plot represents the correlation between clinical grades and pixel coverage values on conjunctival blood vessels (%). For both variables, there were monotonic increases, and a one-tailed test confirmed a significant difference (P < 0.01, Jonckheere-Terpstra Trend Test, one-tailed test).
IOP was lowest at 90 min post-instillation. No correlation was observed between increases in clinical grade and reductions in IOP (P = 0.896, Jonckheere-Terpstra Trend Test, two-tailed test) (Fig. 4).
The correlation between increased clinical grade and reduced IOP. This box-whisker plot depicts the correlation between increased clinical grade and reduced IOP (mmHg). The horizontal axis indicates clinical grade (the maximum clinical grade score observed post-instillation minus baseline clinical grade score), and the vertical axis represents the reduction of IOP (the minimum of IOP post-instillation) − (the IOP of baseline). For correlations between clinical grade and IOP, there was a non-significant trend P = 0.896 (Jonckheere-Terpstra Trend Test, two-tailed test). IOP values varied widely, and outliers at the top and bottom of the box-and-whisker plot are indicated by circles.
Discussion
Several reports have examined correlations between anti-glaucoma ophthalmic solutions and conjunctival hyperemia. Honrubia et al. reported that the incidences of hyperemia related to use of prostaglandin analog ophthalmic solutions were 3.3% to 71.4% (bimatoprost > travoprost > latanoprost)6. Using automated hyperemia analysis software7, Yanagi et al. compared the severity of hyperemia resulting from use of various types of anti-glaucoma eye drops and concluded that prostaglandin analogs were most likely to induce hyperemia.
Preclinical trials indicated a high frequency of ripasudil-related hyperemia post-instillation4,8,9. In previous clinical trials, conjunctival hyperemia was apparently induced following ripasudil instillation. Tanihara et al. performed a phase 1 clinical trial and evaluated dose-dependent adverse events and efficiency for 50 healthy volunteers (placebo, 0.05%, 0.1%, 0.2%, 0.4%, and 0.8%) at 0.5, 2, 4, 8, and 9 h post-instillation4. Hyperemia in bulbar conjunctiva was induced at 30 min post-instillation and disappeared at 4 h post-instillation of 0.4% ripasudil ophthalmic solution in all 8 healthy volunteers. The safety and the effectiveness of ripasudil were confirmed in preclinical phase 2 and 3 clinical trials of patients with glaucoma8,9. They also reported that conjunctival hyperemia was the most frequent adverse event following instillation of ripasudil in participants with glaucoma, as well as healthy participants. Conjunctival hyperemia induced by 0.4% ripasudil ophthalmic solution occurred in 65.3% (phase 2) at 1 h post-instillation and in around 60% (phase 3 studies) at 2 h post-instillation8,9.
There have been two reports of conjunctival hyperemia post-instillation of 0.4% ripasudil ophthalmic solution. According to a report from Inoue’s group, conjunctival hyperemia developed in all 40 healthy participants 15 min post-instillation of 0.4% ripasudil ophthalmic solution, and conjunctival hyperemia disappeared in 92.5% of participants by 2 h post-instillation10. Terao et al. performed a more detailed analysis5 and demonstrated that conjunctival hyperemia peaked at approximately 5–15 min after ripasudil administration in all 50 healthy participants. Hyperemia induced by ripasudil was moderately severe, and the symptoms resolved within 2 h, thus elucidating the time-course of conjunctival hyperemia induced by ripasudil in healthy volunteers. However, similar information was not previously available for patients with glaucoma. Thus, we sought to evaluate the offset of conjunctival hyperemia induced by 0.4% ripasudil ophthalmic solution in patients with glaucoma who were already receiving other (non-ripasudil) anti-glaucoma eye drops.
Clinical grades for conjunctival hyperemia were evaluated in patients with glaucoma, post-instillation of 0.4% ripasudil ophthalmic solution. Our results indicated that conjunctival hyperemia was induced in 84%, and hyperemia disappeared within 2 h in 83.3%.
Of the 50 participants, there were 8 cases where clinical grade did not increase at 10 min post-instillation of ripasudil, compared with baseline. In 7 of these 8 cases, baseline clinical scores were 2 to 3, indicating moderate hyperemia. This high baseline level of conjunctival hyperemia may be the reason that we did not observe changes in clinical grades in these participants.
In some cases, conjunctival hyperemia did not disappear over 3 h. In this study, the frequency of conjunctival hyperemia induced by ripasudil was 84%, which was less than the previously reported data from healthy participants, which showed a 100% incidence5. Previous frequencies of hyperemia were 65.3% (phase 2) and around 60% (phase 3 studies)8,9. This discrepancy may be due to differences in our experimental protocols (i.e., in the preclinical trial, where evaluations were performed 1 to 2 h post-instillation). In this clinical study, the frequency of hyperemia remaining at 1 h post-instillation was 52.4%, which is close to the data of the previous clinical trial.
In the group with the offset time within 60 min, the proportion of patients who had been treated with PG Mono was significantly higher than that with β-blocker. In contrast, in the group with the offset time of 180 min or over, the proportion of patients who had been treated with β-blocker was significantly higher than that with PG Mono. These data may be interpreted that β-blocker instillation delays disappearance of hyperemia. However, the sample size was too small to draw such a conclusion, although the difference was statistically significant.
There were no significant trends for clinical grade increases and reduction of IOP. The correlation between the clinical grades and pixel coverage, generated by the hyperemia analysis software, showed a monotonic tendency to increase over time.
Regarding changes in hyperemia over time, in this trial baseline clinical grade values and pixel coverage values were higher than healthy subject data5. Terao et al. found an average baseline score of 0.19, in contrast to our result of 1.06 for clinical grade. Similarly, baseline pixel coverage value was 4.27 in Terao’s report5, compared to our value of 9.86. These data may be due to the fact that anti-glaucoma eye drops were previously used by our study participants. However, similar to Terao’s data5, the clinical grade and pixel coverage values were significantly decreased, compared to peak values.
In conclusion, conjunctival hyperemia, induced by 0.4% ripasudil instillation, appeared within 10 min post-instillation in patients with glaucoma who were previously treated with anti-glaucoma eye drops. Moreover, hyperemia resolved within 2 h post-instillation, indicating that the hyperemia, induced by ripasudil, was transient in this population.
Methods
This was a multicenter, prospective, interventional, non-randomized open-label study received approval from the Institutional Review Board of Kochi Medical School, Hiroshima University, and Saneikai Tsukazaki Hospital (Clinical trial registration number: 27–75, date of registration: 16/09/2015). The study conformed to Declaration of Helsinki standards. Potential participants for the clinical trial were provided with comprehensive information regarding the study protocol (Supplementary Methods), and written informed consent was obtained before entry to the study. This clinical study was registered with UMIN (code: #000019565, date of registration: 30/10/2015).
Procedures
Slit lamp photographs and IOP measures were performed between 12:00 and 14:00 before instillation as baseline and at 10, 60, 90, 120, 180 min after a single instillation of ripasudil. Binocular IOP values were compared and the eye with higher IOP value was selected at baseline. If the IOP value was the same in both eyes, the right eye was selected. The photographic method was held constant throughout this study, and the photographs were stored as JPEG images. In each participant, photographs of the bulbar conjunctiva on the temporal side were taken with a slit lamp (SL-D7; TOPCON, Tokyo, Japan). The angle between the slit lamp and the microscope arm was set at 30°. The camera flash light was adjusted to level one. The slit width was set 20 mm, and the objective magnification was set at 10. The diffuser of the slit lamp was used, and the resultant photographs were evaluated either by clinical grading or by automated hyperemia analysis software.
Clinical grade of conjunctival hyperemia
Clinical grade of conjunctival hyperemia occurred at the temporal bulbar conjunctiva was evaluated in each case. The clinical grade scores were 0 (none: no hyperemia of the bulbar conjunctiva), 1 (mild: the dilation of a few conjunctival blood vessels), 2 (moderate: the dilation of some conjunctival blood vessels), and 3 (severe: the dilation of many conjunctival blood vessels), based on Japanese guidelines for allergic conjunctival disease11. Clinical grades were evaluated by 3 medical ophthalmic physicians, using the photographs taken at each of the 6 time points. A representative photograph is presented as Fig. 5A. We selected the most frequent grade value generated by the 3 physicians. When the scores differed among the 3 physicians, we selected the maximum value.
Clinical grade and pixel coverage value of conjunctival hyperemia. Typical photograph of each clinical grade is shown (A). The software calculates the proportion of the conjunctival blood vessels as the pixel coverage. The pixel coverage value was automatically calculated for the closed square area (vertical 60% and horizontal 40%). When processing the photographs shown in (A) to the analysis software, blood vessels are drawn in the green area (B).
Evaluating pixel coverage on conjunctival vessels using conjunctival hyperemia analysis software
The photographs were processed using the software program developed by our group12,13. Briefly, this software calculates the proportion of the blood vessels in the conjunctiva as the pixel percent coverage. The photographs were transferred to the software to calculate pixel coverage. To detect blood vessels, the green component of the RGB color model was used, and we adjusted the green value to accurately detect blood vessels within the region of interest (ROI). The pixel coverage was calculated by dividing the frequency of conjunctival blood vessel pixels by the total pixel frequency. For each selected region, the extent of hyperemia was determined by the percentage of pixelated blood vessels in the ROI. The ROI was depicted as the square, bordered by a blue line, with a vertical width of 60% and a horizontal width of 40%, using analysis software. Figure 5B depicts an automatically-created representative photograph. Blood vessels are displayed within the green area, and the blood vessel occupancy rate is shown in the ROI (Fig. 5B). The pixel coverage of conjunctival blood vessels was evaluated by 3 doctors using the ROIs within photographs taken at each of the 6 time points. We selected the most frequent pixel coverage value, as determined by 3 doctors. When the value differed among the 3 doctors, we selected the maximum value so as to not underestimate incidence of hyperemia.
IOP measurements using the iCare TA01i tonometer
Our method for measuring IOP was selected in order to not affect conjunctival hyperemia. Although the “gold standard” evaluation method is the Goldmann applanation tonometer; however, use of anesthesia eye drops may affect hyperemia. Therefore, we selected a technique that did not require anesthesia and measured the IOP, in the sitting position, using an iCare TA01i tonometer14.
Study population
We enrolled adult participants (older than 20y) with open-angle glaucoma or OHT, who needed additional eye drop treatment, and had never been treated with ripasudil ophthalmic solution. The inclusion and exclusion criteria for this study are outlined in Table 3.
Primary and secondary endpoints
The primary endpoint was median offset time for hyperemia, as determined by clinical grade scoring. The hyperemia offset time was determined as the time-point when clinical grade score increased by instillation of ripasudil returned to the baseline score. Our secondary endpoints were relationships among clinical grade changes over time, IOP, and pixel coverage on conjunctival blood vessels within 180 min post-instillation. The correlations between clinical grade and pixel coverage, and clinical grade and IOP reduction were statistically analyzed.
Statistical analyses
Fifty cases were selected for the purpose of exploratory data analysis and determination of feasibility. The statistical analyses were performed using the statistical package R, version 3.4.1 (R Foundation for statistical Computing, Vienna, Austria). For the primary endpoint, median offset of conjunctival hyperemia, we used a (two-tailed) 95% confidence interval, as follows. The lower bound was the [(n + 1)/2 − √n]-th value counted from the minimum value. The upper bound was the [(n + 1)/2 − √n]-th value counted from the maximum value. (The value [(n + 1)/2 − √n] was the whole number part of (n + 1)/2 − √n.) Ultimately, 42 participants were selected for final analyses. Eight participants with no increases in clinical grade post-instillation, relative to baseline, were excluded from the primary endpoint. Secondary endpoints were assessed by using repeated-measure analysis of variance (ANOVA) for all 50 participants. Paired-t test was carried out when it was judged that there was a significant difference between the two groups using ANOVA. The data were expressed as means ± SDs. P values * < 0.05 and ** < 0.01 were considered statistically significant. The correlation between the clinical grade and the value of pixel coverage of the blood vessels, and clinical grade and IOP, were subjected to statistical analyses using the Jonckheere-Terpstra Trend Test.
References
Honjo, M. et al. Effects of Rho-associated protein kinase inhibitor Y-27632 on intraocular pressure and outflow facility. Invest. Ophthalmol. Vis. Sci. 42, 137–144 (2001).
Kameda, T. et al. The effect of Rho-associated protein kinase inhibitor on monkey Schlemm’s canal endothelial cells. Invest. Ophthalmol. Vis. Sci. 53, 3092–3103 (2012).
Inoue, T. & Tanihara, H. Rho-associated kinase inhibitors: a novel glaucoma therapy. Prog. Rein. Eye Res. 37, 1–12 (2013).
Tanihara, H. et al. K-115 Clinical Study Group. Phase 1 clinical trials of a selective Rho-kinase inhibitor, K-115. JAMA Ophthalmol. 131, 1288–1295 Erratum in: JAMA Ophthalmol. 132, 787 (2014) (2013).
Terao, E. et al. Time course of conjunctival hyperemia induced by a Rho-kinase inhibitor anti-glaucoma eye drop: Ripasudil 0.4%. Curr. Eye Res. 42, 738–742 (2017).
Honrubia, F., García-Sánchez, J., Polo, V., de la Casa, J. M. & Soto, J. Conjunctival hyperaemia with the use of latanoprost versus other prostaglandin analogues in patients with ocular hypertension or glaucoma: a meta-analysis of randomised clinical trials. Br. J. Ophthalmol. 93, 316–321 (2009).
Yanagi, M. et al. Association between glaucoma eye drops and hyperemia. Jpn. J. Ophthalmol. 60, 72–77 (2016).
Tanihara, H. et al. K-115 Clinical Study Group. Phase 2 randomaized clinical study of a Rho kinase inhibitor, K-115, in primary open-angle glaucoma and ocular hypertension. Am. J. Ophthalmol. 156, 731–736 (2013).
Tanihara, H. et al. K-115 Clinical study group additive intraocular pressure-lowering effects of the Rho Kinase Inhibitor Ripasudil (K-115) combined with Timolol or Latanoprost: A report of 2 randomized clinical trials. JAMA Ophthalmol. 133, 755–761 (2015).
Inoue, K. et al. Conjunctival hyperemia post-instillation of one drop of ripasudil ophthalmic solution in volunteers. Jpn. J. Ophthalmol. 71, 103–108 (2017).
Japanese Ocular Allergology Society [Guidelines for the clinical management of allergic conjunctival disease (2nd edition)]. Jpn. Ophthalmol. 114, 831–870 (2010).
Yoneda, T. et al. Automated hyperemia analysis software: reliability and reproducibility in healthy subjects. Jpn. J. Ophthalmol. 56, 1–7 (2012).
Sumi, T. et al. Development of automated conjunctival hyperemia analysis software. Cornea. 32, 52–5 (2013).
Pakrou, N., Gray, T., Mills, R., Landers, J. & Craig, J. Clinical comparison of the Icare tonometer and Goldmann applanation tonometry. J. Glaucoma. 17, 43–47 (2008).
Author information
Authors and Affiliations
Contributions
S.N., Y.K. and A.F. designed the study, E.S. and W.I. wrote the main manuscript text in consultation with S.N., Y.K. and A.F. E.S., E.T., Y.F., S.N., K.J., H.O. and Y.K. conducted the study, W.I., T.S., T.K., K.T., K.F. T.Y. and H.K. analysed the data. All authors reviewed the manuscript. All authors have contributed to interpretation, and critically reviewed the manuscript. All authors approved the final version of the manuscript, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing Interests
This study was funded by Kowa Company, Ltd. under contract. The funder had no control over the interpretation, writing, or publication of this work. E.S., T.S., K.F., S.N., Y.K. and A.F. report grants and personal fee from Kowa. W.I., T.K., K.T., H.K., E.T., Y.F., K.J., and H.O. report grants from Kowa. T.Y. declares no potential conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sakamoto, E., Ishida, W., Sumi, T. et al. Evaluation of offset of conjunctival hyperemia induced by a Rho-kinase inhibitor; 0.4% Ripasudil ophthalmic solution clinical trial. Sci Rep 9, 3755 (2019). https://doi.org/10.1038/s41598-019-40255-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-40255-9
This article is cited by
-
Role of mechanically-sensitive cation channels Piezo1 and TRPV4 in trabecular meshwork cell mechanotransduction
Human Cell (2024)
-
Crossover Randomized Study of Pharmacologic Effects of Ripasudil–Brimonidine Fixed-Dose Combination Versus Ripasudil or Brimonidine
Advances in Therapy (2023)
-
Safety and efficacy of ripasudil in Japanese patients with glaucoma or ocular hypertension: 12-month interim analysis of ROCK-J, a post-marketing surveillance study
BMC Ophthalmology (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.