Abstract
This study investigates the prevalence of pre-diabetes and diabetes and their associated risk factors among adults in Northeast China. A multistage stratified cluster sampling method was used to select adults from Jilin Province. Out of an initial recruitment of 23,050 individuals, 21,435 participants completed an interview and medical examination. The estimated prevalence of diabetes and pre-diabetes were 9.1% and 19.8%, respectively. The prevalence of hypertension, dyslipidemia, and obesity were the highest in participants with previously diagnosed diabetes. Participants who were previously diagnosed with diabetes were more likely to be aware of their hypertension and dyslipidemia status. Participants who were older, male, more educated, or who were widows or widowers were at greater risk for pre-diabetes. Similarly, those who were current drinkers or smokers, had higher BMI or waist circumference, had a family history of diabetes, or who reported they lived in urban areas or had low physical activity levels had increased pre-diabetes risk. The observed levels of diabetes and pre-diabetes in this study indicate that the medical authority needs to focus more attention in this area, and that health monitoring is essential to improving the health awareness of its residents.
Similar content being viewed by others
Introduction
Diabetes mellitus is one of the leading causes of death and disability worldwide1,2. In 2014, the International Diabetes Federation estimated that the number of people with diabetes will rise from 387 million to 592 million by 20353. Diabetic patients have a substantially elevated risk of cardiovascular disease and likewise cardio metabolic syndrome is associated with an increased risk of diabetes4. Diabetes has also been linked to hypertension and hyperlipidemia, with the pharmacological treatment of hypertension in diabetic patients significantly reducing macro vascular complications5,6, and highlighting the importance of managing blood pressure and blood lipids in the diabetic population.
The prevalence of diabetes has reached over 30% in some countries, most notably in the western pacific islands, such as Tokelau (37.5%), Federated States of Micronesia (35%) and the Marshall Islands (34.9%)2, although In 2013 the overall prevalence of diabetes in mainland China was 10.9%7, The prevalence of pre-diabetes in China is 35.7%8, much higher than in some other countries such as Saudi Arabia (6.8%), India (6.3%), and the southern cone of Latin America (17.8%)3,9,10. It is not clear whether pre-diabetes increases the risk of hypertension and hyperlipidemia. To provide reliable data and suggestions for prevention, this study aims (1) to estimate the prevalence of diabetes and pre-diabetes, and their influencing factors, in the adult population in the Jilin province; and (2) to describe the association between diabetes and other chronic diseases in the same population.
Method
Study design and population
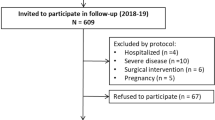
This is the first large face-to-face cross-sectional interview based study in the Jilin Province, Northeast China. This study adopted a multistage stratified cluster sampling method to select adult permanent residents in the province: Firstly, nine administrative regions were selected covering the whole province (Changchun, Jilin City, Siping, Liaoyuan, Tonghua, Baishan, Songyuan, Baicheng and Yanbian), which all have a large responsibility for health care. Secondly, from each of the nine regions, clusters of four districts, or counties, were randomly selected based on probability proportional to size (PPS) sampling. According to the National Bureau of Statistics of China, each selected district or county in this survey is divided into urban and rural areas11. Thereafter, four or five communities were randomly taken out from the urban and rural strata by PPS. Finally, one adult was randomly chosen from each household of the communities mentioned above (pregnant individuals were not included). In total, 23,050 adult subjects were recruited from 32 districts or counties, 95 towns or communities, and 45 units in the Jilin Province11. In total 21,435 participants completed the interview (response rate: 92.2%). After excluding invalid questionnaires and abnormal data (for example an indicated weight of 12 kg), 18,362 participants were included in the study. The study was approved by the Ethics Committee of Jilin University School of Public Health, and written informed consents were obtained from all the subjects in the survey. We confirm that all methods were performed in accordance with relevant guidelines and regulations.
Questionnaire investigation
116 trained investigators conducted the interview in local health centers and communities using structured questionnaires. The questionnaires covered subjects’ socio-demographic characteristics and health related information. Each questionnaire was examined by the interviewer through a parallel double entry system after being completed by participants12.
Physical examination
A physical examination was conducted by trained investigators, and consisted of anthropometric measurements including height, weight, blood pressure, and fasting blood glucose (FBG & OGTT) and blood lipid levels. Blood samples were collected from participants in the morning after an overnight fast of 10 h or more. The BaiAnkang fingertip blood glucose monitor machine (Bayer, Beijing, China) was used to measure FBG levels by collecting a small drop of blood from a finger of the participant onto a strip of paper. Post-fast blood samples were also drawn by venipuncture to measure blood lipid concentration. After collection, the samples were placed in a cold chain system before being collectively transported to a central laboratory at Jilin University.
Definitions of major Variables
Diabetes: FBG ≥7.0 mmol/L, oral glucose tolerance test (OGTT-2 h) ≥11.0 mmol/L plasma glucose or self-reported use of anti-diabetic medication during the 2 weeks prior to the examination13.
Pre-diabetes: FBG from 6.1 to 6.9 mmol/l, OGTT-2 h: 7.8–10.9 mmol/l14.
Hypertension: systolic pressure >140 mmHg or diastolic pressure >90 mmHg15.
Dyslipidemia: Total cholesterol (TC) >5.18 mmol/L and/or (TG) triglyceride TG > 1.70 mmol/L and/or high-density lipoprotein cholesterol (HDL-C) <1.04 mmol/L and/or low density lipoprotein cholesterol (LDL-C) >3.37 mmol/L12. (Having a history of dyslipidemia and Hypertension disease in the past one year, and/or currently receiving treatment with lipid-lowering medications was regarded as dyslipidemia and Hypertension in this study).
Body Mass Index (BMI): For the Chinese population, obesity is defined as a BMI of ≥28 kg/m2, and overweight as a BMI of 24–27.9 kg/m2 16.
Central obesity: waist circumference (WC) >80 cm for females and WC >85 cm for males17.
Age groups: according to the criteria of age classification by WHO reported in 2012, age range is divided into three groups: young (18–44 years), middle (44–59 years) and old (≥60 years)16.
Other factors: A smoker was defined as a person who smoked at least one cigarette per day within the last 30 days, and drinker was a person who consumed more than one alcoholic drink per week. Participants were divided into those that “sometimes exercise”, with an exercise frequency of one or two times a week; those who exercised more than three times a week were defined as “exercise frequently”; while those who didn’t or seldom exercised were defined as those that “never or rarely exercise”18.
Statistical analyses
Post stratification adjustment was used to make the sample representative of the provincial population11. The adjustment was made according to the distribution of gender and age groups in the census of the adult population of Jilin Province in 2010. All the data were input into Epidata 3.0, and analyzed with SPSS (ver. 22.0; IBM Corp, Armonk, NY, USA). Continuous variables were expressed by mean and standard deviation; and categorical variables were presented as frequencies. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated by a logistic regression model. P < 0.05 was considered to be statistically significant.
Results
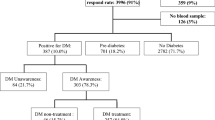
Of the 23,050 participants initially recruited, 18,362 participants aged from 18 to 79 were included in this study. The estimated prevalence of diabetes and pre-diabetes were 9.1% and 19.8% respectively. Among the diabetic participants, 68.9% were previously diagnosed diabetic patients and 31.1% were newly diagnosed in this study. Table 1 shows the socio-demographic characteristics of the study population according to glycemic status.
The newly-diagnosed group was younger, with a larger proportion of men, manual laborers, singles or widows/widowers, current drinkers or smokers, a family history of diabetes and a low frequency of physical exercise compared to the participants with previously diagnosed diabetes. In addition, the newly diagnosed participants had a higher WC, blood sugar levels (both FBG and OGTT-2 h plasma glucose), TG and DBP levels than those of the previously diagnosed group.
The prevalence of hypertension, dyslipidemia, and obesity were highest in participants with previously-diagnosed diabetes, but participants tended to be more aware of their hypertension and dyslipidemia status compared to other groups. As shown in Table 2, among participants who were aware of their respective disease condition, the previously-diagnosed diabetes group was most likely to be receiving treatment, but overall the proportion of participants receiving measures to control their blood pressure, lipid levels and obesity was not high. Figure 1 shows the status of awareness, treatment and control, in hypertension, dyslipidemia and obesity. It is worth noting that the prevalence of dyslipidemia was at a particularly high level, but the rates of awareness, treatment and control were low.
The results of Multivariable logistic regressions among the four groups are shown in Table 3. Older age, male gender, urban residents, widows or widowers, current drinkers or smokers, higher BMI and WC, with an education at undergraduate level and above, having a family history of diabetes and doing physical exercise with low frequency, were all indicators of an increased risk of pre-diabetes. Similarly, for the previously diagnosed diabetes group and the newly diagnosed diabetes group, older age, male gender, higher BMI and WC, not married, being current drinkers, and having a family history of diabetes were risk factors.
Discussion
The prevalence of diabetes in this representative population is 9.1%. According to a previous review, the prevalence of unspecified type diabetes was 10% (95%CI: 9–12%) from 42 different cohorts19, which is just slightly higher than the prevalence of diabetes in this study. In recent years, an increasing number of studies have begun to focus on pre-diabetes. An African study reported a prevalence of pre-diabetes at 13.8% in 201620,and a Norwegian study indicated that the age-standardized prevalence of pre-diabetes among men was about 3.3–3.4%, and 2.3–2.7% for women21. In this study, the level of pre-diabetes reached 19.8%, over twice the number of participants with diabetes. In a nationally representative sample of 46,239 Chinese adults in 2008, the prevalence of pre-diabetes was 15.5% (16.1% among men and 14.9% among women), which is lower than our observations22. Given the seemingly increasing rate of pre-diabetes in China, and that it is a high risk factor for the development of diabetes, the Chinese government should focus increasing attention on pre-diabetic populations.
Compared with the previously diagnosed diabetes participants, newly diagnosed diabetes participants had a higher level of blood sugar, blood fat and blood pressure, which is likely to be related to the lack of awareness and treatment. People with a clear diagnosis of diabetes tend to follow the doctor’s advice by taking regular medication, doing moderate exercise and following a low sugar diet23. People unaware of their diabetes follow their original life styles, which may not benefit their health.
Influential factors
Similar to previous research24, this study demonstrates that the male gender, increasing age, higher BMI, and a family history of diabetes are all risk factors for diabetes. In addition, our study showed that central obesity (WC) is also a significant risk factor for both diabetes and pre-diabetes. It has been previously reported that an increase in WC leads to an increased risk of death25. Furthermore, people with a normal BMI but an excess WC, are more likely to have a metabolic disease17, and as an early warning signal of some chronic diseases, central obesity is more significant than BMI26. Previous research reported that higher education is a protective factor for diabetes, which may be related to the understanding of diabetes and the inclination to keep a healthy lifestyle27,28. In this study however, higher education appeared to be a risk factor for diabetes, which may be in fact associated with the earlier detection of the disease. In line with previous studies, we also showed that both not drinking and taking exercise frequently were both protective factors for diabetes24, and confirm that diabetes is associated with a high prevalence of hypertension and dyslipidemia29,30. Although the pre-diabetes group had a blood sugar level lower than that of a diabetic, the prevalence of hypertension, dyslipidemia and obesity were larger than in the normal group.
Metabolic diseases are serious chronic diseases with multiple complications, yet the awareness by participants of these diseases is still poor12,31, which was highlighted in our study where over 30% of adults with diabetes were still not aware of their hypertension status, and an even higher number were not aware of their dyslipidemia status. However, regardless of diabetes status, the poor control rates of hypertension and dyslipidemia may partly be attributed to noncompliance with drug therapy32. This could be based on a fear of side effects including worries about their effect on sexual performance, concerns about dependency, insufficient health insurance to cover costs, or a poor knowledge of the disease risks13,31,33,34.
In spite of increased vigilance in the detection of diabetes, the attention afforded to pre-diabetes is insufficient. To enhance the quality of general health and reduce the morbidity of diabetes, the Chinese government should actively encourage regular blood sugar monitoring.
Study strengths and limitations
This study is the largest sample of diabetic and pre-diabetic patients in northeast China. The response rate was high, and the study was actually beneficial to the participants in that it included a medical exam. Limitations included the use of self-reported information, such as drinking, smoking and taking exercise, which may lead to recall bias. In addition, the study didn’t discriminate between diabetes type I and type 2, although most participants did have diabetes type 2. Moreover, all the participants were only recruited from the Jilin Province and therefore might not be comparable to other areas of China. Finally, blood lipids were measured from venous blood and not all participants had their blood lipids measured, notably those who clearly knew about their blood lipid status (such as those who had been diagnosed with dyslipidemia by doctors) and non-fasting subjects.
Conclusion
The levels of pre-diabetes and diabetes in Northeast China that we show in this study indicate that the medical authority needs to increase their focus in this area. Given that the link between increases in blood sugar levels and the incidence of cardio-metabolic disorders, we highly recommended that participants with pre-diabetes and diabetes monitor their health regularly.
References
Murray, C. J. et al. Global, regional, and national incidence and mortality for HIV, tuberculosis, and malaria during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet (London, England) 384, 1005–1070, https://doi.org/10.1016/s0140-6736(14)60844-8 (2014).
Naeem, Z. Burden of Diabetes Mellitus in Saudi Arabia. International journal of healthsciences 9, V–vi (2015).
Shen, J. et al. A Multiethnic Study of Pre-Diabetes and Diabetes in LMIC. Global heart 11, 61–70, https://doi.org/10.1016/j.gheart.2015.12.015 (2016).
Ogihara, T. & Mita, T. Relationships between lifestyle patterns and cardio-renal-metabolic parameters in patients with type 2 diabetes mellitus: A cross-sectional study. 12, e0173540, https://doi.org/10.1371/journal.pone.0173540 (2017).
Arauz-Pacheco, C., Parrott, M. A. & Raskin, P. The treatment of hypertension in adult patients with diabetes. Diabetes care 25, 134–147 (2002).
Bakris, G. L. & Sowers, J. R. ASH position paper: treatment of hypertension in patients with diabetes-an update. Journal of clinical hypertension (Greenwich, Conn.) 10, 707–713; discussion 714–705, https://doi.org/10.1111/j.1751-7176.2008.00012.x (2008).
Liu, X. et al. The prevalence and long-term variation of hospital readmission for patients with diabetes in Tianjin, China: A cross-sectional study. Medicine 96, e7953, https://doi.org/10.1097/md.0000000000007953 (2017).
Wang, L. et al. Prevalence and Ethnic Pattern of Diabetes and Prediabetes in China in 2013. Jama 317, 2515–2523, https://doi.org/10.1001/jama.2017.7596 (2017).
Alanazi, N. H. et al. Prevalence of diabetes and its relation with age and sex in Turaif city, northern Saudi Arabia in 2016–2017. Electronic physician 9, 5294–5297, https://doi.org/10.19082/5294 (2017).
Tripathy, J. P. et al. Prevalence and risk factors of diabetes in a large community-based study in North India: results from a STEPS survey in Punjab, India. Diabetology & metabolic syndrome 9, 8, https://doi.org/10.1186/s13098-017-0207-3 (2017).
Wang, S. et al. Rural-urban differences in the prevalence of chronic disease in Northeast China. Asia-Pacific journal of publichealth 27, 394–406, https://doi.org/10.1177/1010539514551200 (2015).
He, H. et al. Dyslipidemia awareness, treatment, control and influence factors among adults in the Jilin province in China: a cross-sectional study. Lipids in health and disease 13, 122, https://doi.org/10.1186/1476-511x-13-122 (2014).
Wang, R. et al. Situation of Diabetes and Related Disease Surveillance in Rural Areas of Jilin Province, Northeast China. International journal of environmental research and public health 13, https://doi.org/10.3390/ijerph13060538 (2016).
Tabak, A. G., Herder, C., Rathmann, W., Brunner, E. J. & Kivimaki, M. Prediabetes: a high-risk state for diabetes development. Lancet (London, England) 379, 2279–2290, https://doi.org/10.1016/s0140-6736(12)60283-9 (2012).
Yang, G. et al. Prevalence and Correlates of Prehypertension and Hypertension among Adults in Northeastern China: A Cross-Sectional Study. International journal of environmental research and public health 13, 82, https://doi.org/10.3390/ijerph13010082 (2015).
Wang, R. et al. Prevalence of overweight and obesity and some associated factors among adult residents of Northeast China: a cross-sectional study. BMJ open 6, e010828, https://doi.org/10.1136/bmjopen-2015-010828 (2016).
Zhang, P. et al. Prevalence of Central Obesity among Adults with Normal BMI and Its Association with Metabolic Diseases in Northeast China. PloSone 11, e0160402, https://doi.org/10.1371/journal.pone.0160402 (2016).
Wang, R. et al. Association between passive smoking and mental distress in adult never-smokers: a cross-sectional study. BMJ open 6, e011671, https://doi.org/10.1136/bmjopen-2016-011671 (2016).
Roberts, E. et al. The prevalence of diabetes mellitus and abnormal glucose metabolism in the inpatient psychiatric setting: A systematic review and meta-analysis. General hospital psychiatry 45, 76–84, https://doi.org/10.1016/j.genhosppsych.2017.01.003 (2017).
Chiwanga, F. S. et al. Urban and rural prevalence of diabetes and pre-diabetes and risk factors associated with diabetes in Tanzania and Uganda. Global health action 9, 31440, https://doi.org/10.3402/gha.v9.31440 (2016).
Naseribafrouei, A., Eliassen, B. M., Melhus, M. & Broderstad, A. R. Ethnic difference in the prevalence of pre-diabetes and diabetes mellitus in regions with Sami and non-Sami populations in Norway - the SAMINOR1 study. International journal of circumpolar health 75, 31697, https://doi.org/10.3402/ijch.v75.31697 (2016).
Yang, W. et al. Prevalence of diabetes among men and women in China. The New England journal of medicine 362, 1090–1101, https://doi.org/10.1056/NEJMoa0908292 (2010).
Wang, C. et al. Awareness, treatment, control of diabetes mellitus and the risk factors: survey results from Northeast China. PloS one 9, e103594, https://doi.org/10.1371/journal.pone.0103594 (2014).
Wong, C. K., Lo, Y. Y., Wong, W. H. & Fung, C. S. The associations of body mass index with physical and mental aspects of health-related quality of life in Chinese patients with type 2 diabetes mellitus: results from a cross-sectional survey. Health and quality of life outcomes 11, 142, https://doi.org/10.1186/1477-7525-11-142 (2013).
Cameron, A. J. & Zimmet, P. Z. Expanding evidence for the multiple dangers of epidemic abdominal obesity. Circulation 117, 1624–1626, https://doi.org/10.1161/circulationaha.108.775080 (2008).
Smith, S. C. Jr. & Haslam, D. Abdominal obesity, waist circumference and cardio-metabolic risk: awareness among primary care physicians, the general population and patients at risk–the Shape of the Nations survey. Current medical research and opinion 23, 29–47, https://doi.org/10.1185/030079906x159489 (2007).
Gnavi, R., Karaghiosoff, L., Costa, G., Merletti, F. & Bruno, G. Socio-economic differences in the prevalence of diabetes in Italy: the population-based Turin study. Nutrition, metabolism, and cardiovascular diseases: NMCD 18, 678–682, https://doi.org/10.1016/j.numecd.2007.11.004 (2008).
McWilliams, J. M., Meara, E., Zaslavsky, A. M. & Ayanian, J. Z. Differences in control of cardiovascular disease and diabetes by race, ethnicity, and education: U.S. trends from 1999 to 2006 and effects of medicare coverage. Annals of internal medicine 150, 505–515 (2009).
Lago, R. M., Singh, P. P. & Nesto, R. W. Diabetes and hypertension. Nature clinical practice. Endocrinology & metabolism 3, 667, https://doi.org/10.1038/ncpendmet0638 (2007).
Klen, J., Goricar, K., Janez, A. & Dolzan, V. NLRP3 Inflammasome Polymorphism and Macrovascular Complications in Type 2 Diabetes Patients. Journal of diabetes research 2015, 616747, https://doi.org/10.1155/2015/616747 (2015).
Agyemang, C. et al. Prevalence, awareness, treatment, and control of hypertension among Black Surinamese, South Asian Surinamese and White Dutch in Amsterdam, The Netherlands: the SUNSET study. Journal of hypertension 23, 1971–1977 (2005).
Fernald, F. F. et al. Hypertension awareness, treatment, and control among diabetic and nondiabetic individuals in a multiethnic population in the Netherlands: the HELIUS study. Journal of hypertension 34, 539–547; discussion 547, https://doi.org/10.1097/hjh.0000000000000820 (2016).
Zhang, F. L. et al. The prevalence, awareness, treatment, and control of dyslipidemia in Northeast China: a population-based cross-sectional survey. Lipids in health and disease 16, 61, https://doi.org/10.1186/s12944-017-0453-2 (2017).
Beune, E. J., Haafkens, J. A., Agyemang, C., Schuster, J. S. & Willems, D. L. How Ghanaian, African-Surinamese and Dutch patients perceive and manage antihypertensive drug treatment: a qualitative study. Journal of hypertension 26, 648–656, https://doi.org/10.1097/HJH.0b013e3282f4d20b (2008).
Acknowledgements
The authors would like to thank all participants from the Jilin Province of China and the staff from Jilin University. This study was supported by grants from the Center for Disease Prevention and Control in Jilin Province. This study was supported by a competitive grant from the Scientific Research Foundation of the Health Bureau of Jilin Province, China (Grant Number: 2011Z116) and the Program of International Scientific and Technological Cooperation in Jilin Province (20160414056 G H).
Author information
Authors and Affiliations
Contributions
Bo Li, Youbin Cui and Yaqin Yu designed the study; Rui Wang, Peng Zhang performed the study; Rui Wang and Peng Zhang analyzed the data, Rui Wang, Peng Zhang, Zhijun Li, and Hongfei Cai drafted the manuscript; Xin Lv, Chunshi Gao, and Yuanyuan Song participated amending the manuscript together. All authors approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, R., Zhang, P., Li, Z. et al. The prevalence of pre-diabetes and diabetes and their associated factors in Northeast China: a cross-sectional study. Sci Rep 9, 2513 (2019). https://doi.org/10.1038/s41598-019-39221-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-39221-2
This article is cited by
-
Prevalence of prediabetes and risk of CVD mortality in individuals with prediabetes alone or plus hypertension in Northeast China: insight from a population based cohort study
BMC Public Health (2024)
-
Prevalence, treatment, control of type 2 diabetes and the risk factors among elderly people in Shenzhen: results from the urban Chinese population
BMC Public Health (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.