Abstract
There are no clinical guidelines for the timing of cholecystectomy (CCY) after performing therapeutic endoscopic retrograde cholangiopancreatography (ERCP) for choledocholithiasis. We tried to analyze the clinical practice patterns, medical expenses, and subsequent outcomes between the early CCY, delayed CCY, and no CCY groups of patients. 1827 choledocholithiasis patients who underwent therapeutic ERCP were selected from the nationwide population databases of two million random samples. These patients were further divided into early CCY, delayed CCY, and no CCY performed. In our analysis, 1440 (78.8%) of the 1827 patients did not undergo CCY within 60 days of therapeutic ERCP, and only 239 (13.1%) patients underwent CCY during their index admission. The proportion of laparoscopic CCY increased from 37.2% to 73.6% in the delayed CCY group. There were no significant differences (p = 0.934) between recurrent biliary event (RBE) rates with or without early CCY within 60 days of ERCP. RBE event-free survival rates were significantly different in the early CCY (85.04%), delayed CCY (89.54%), and no CCY (64.45%) groups within 360 days of ERCP. The method of delayed CCY can reduce subsequent RBEs and increase the proportion of laparoscopic CCY with similar medical expenses to early CCY in Taiwan’s general practice environment.
Similar content being viewed by others
Introduction
Cholelithiasis is one of the most troublesome diseases and constitutes a substantial burden on healthcare resources worldwide1,2,3. It requires surgical intervention4 and has been seen at an alarming rate over the past two decades in many places, including Taiwan5. The abundant access to food in developing and developed countries places the population at increased risk of obesity, and the incidence rates of cholelithiasis grow accordingly6,7. Choledocholithiasis results mostly from gallstones passing through the cystic duct into the common bile duct (CBD). Therefore, cholecystectomy (CCY) seems a reasonable method for reducing recurrent biliary events (RBEs) after therapeutic endoscopic retrograde cholangiopancreatography (ERCP) stone removal is performed.
Previous retrospective studies have shown that CCY can reduce RBEs8,9 compared with leaving the gallbladder in situ after therapeutic ERCP for choledocholithiasis patients. Two prospective small studies demonstrated that CCY has a protective effect for subsequent RBEs for cholelithiasis patients undergoing ERCP10,11. Although remnant CBD stones sometimes occurred after CCY12, CCY does have the benefit of reducing RBEs. There is no consensus regarding the timing for elective CCY after therapeutic ERCP for choledocholithiasis, despite well-designed retrospective or prospective studies showing 15–20% decrease in RBE rates8,9,13 when performing CCY right after ERCP rather than 7–8 weeks later, since some RBEs happened while awaiting delayed CCY. Financial analysis revealed different results for medical expenses for elective CCY after therapeutic ERCP for choledocholithiasis in Western and Eastern countries9,14.
There are no current guidelines for the optimal timing for performing CCY after therapeutic ERCP. Few or no real-world studies had proven these theories until a large-scale retrospective database study was performed using an American commercial database9. Although this study showed that early CCY can reduce RBEs, and CCY itself can reduce further RBEs in the following year compared with no CCY, the clinical practices in Taiwan are very different due to the different cultural and economic conditions and public health care policies. Therefore, we conducted this current study based on the Taiwan National Health Insurance Research Database (NHIRD).
Methods
This study was approved by the Institutional Review Board (IRB) of Chung Shan Medical University Hospital, Taiwan. The IRB waived the need for informed consent for this retrospective study based on NHIRD. All methods were performed in accordance with the relevant guidelines and regulations and under surveillance by then IRB of Chung Shan Medical University Hospital.
Study design
This study is a population-based retrospective cohort study based on Taiwan’s NHIRD, which covered more than 99% of the entire population15. The NHIRD has been described in detail in previous studies16,17.
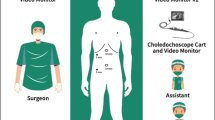
Choledocholithiasis cases were selected from two million random samples from the NHIRD between 2004 and 2011 using the Codes of International Statistical Classification of Diseases and Related Health Problems-9th Edition (ICD-9) recorded during admission. Acute cholangitis or choledocholithiasis patients without concurrent cholecystitis were selected using ICD-9 574.2, 574.5, 574.9, 576.1, 576.2 and therapeutic ERCP defined as endoscopic sphincterotomy (EST; order code 56031B, 56033B), endoscopic papillary balloon dilatation (EPBD; order code 56032B) or endoscopic lithotripsy (order code 28008B, 28035B) during index admission occurring in 2006–2009. Patients who previously underwent therapeutic ERCP for choledocholithiasis or CCY, tracing back from index admission to 2004, were excluded. The observation period selected was from January 2010 to December 2011. A total of 1827 patients with symptomatic choledocholithiasis who underwent therapeutic ERCP for stone removal were selected. We further divided these patients into three categories: (1) CCY done at index admission (early CCY), (2) CCY done within 60 days after index admission (delayed CCY), and (3) no CCY done within 60 days after index admission (no CCY). The details of this study design are shown in Fig. 1. Table 1 shows the age, gender, Charlson Comorbidity Index (CCI) score, hospital classification, economic status and living area condition of the total study population. The proportion of laparoscopic CCY and open CCY, RBEs, CCI scores and economic costs were compared for these three groups. RBEs in our study are defined as admissions or emergency room (ER) visits with a diagnosis of cholelithiasis, choledocholithiasis, cholecystitis, cholangitis and pancreatitis. Selective admissions for delayed CCY within 60 days after index admission were excluded from RBE analysis because they were for selected surgery attempts without symptoms. Since there are no outpatient surgery interventions of the biliary system in Taiwan, the financial analysis of admission and ER visits are complete in our national health insurance system data. Economic analysis of costs of index admission, delayed CCY, RBEs visits and total medical expenses were compared for these three groups under Taiwan’s national health insurance system.
Data processing and statistical analysis
The National Health Insurance Research Database (NHIRD), with two million subjects who are representative of the nationwide population between 2004 and 2011 in Taiwan, was processed using Microsoft SQL Server 2008 R2 (Microsoft Corporation, Redmond, WA, USA) with the SQL programming language. Statistical analysis was done using OpenEpi: open source epidemiologic statistics for public health, version 3.0118. Kaplan-Meier survival analysis was done using R version 3.4.3.
Data obtained from the study were processed using Chi-Square (χ2) tests for categorical variables, one-way ANOVA (Analysis of Variance) for continuous variables, and Log Rank (Mantel-Cox) tests for disease-free survival curves. A two-tailed P-value of 0.05 was considered statistically significant in this study.
Results
The data for 1827 patients who underwent therapeutic ERCP for choledocholithiasis without concurrent cholecystitis were collected. The mean age was 65.5 ± 16.2, and 55.7% were male. In Taiwan, the medical evaluation systems are divided into medical centers, regional hospitals, and local hospitals. Fifty-six percent of these patients received medical treatment at medical centers, with 8.8% receiving endoscopic retrograde biliary drainage stent at index admission; 58.7% of the patients were living in cities. Other detailed information of the study population is shown in Table 1.
Reflecting the culture in Taiwan, surgical intervention was always the last choice for treatment. In our analysis, 1440 (78.8%) of the 1827 patients did not undergo CCY within 60 days after therapeutic ERCP, and only 239 (13.1%) patients underwent CCY during the index admission. Although previous evidence showed early CCY could lead to an increased rate of laparoscopic CCY9, and early laparoscopic CCY could reduce complication rates in acute cholangitis19 and biliary pancreatitis patients20, our study showed a different pattern in Taiwan. Only 89 (37.2%) of the 239 patients underwent laparoscopic CCY in the early CCY group when acute cholangitis was treated at index admission. The proportion of laparoscopic CCY increased to 73.6% (109 of 148) for the delayed CCY group (Table 2).
Comorbidity profile
The early CCY, delayed CCY, and no CCY cohorts were compared using age, gender and parameters of CCI scores. The results showed significant differences in patient age, CCI scores, underlying congestive heart failure, chronic pulmonary disease, peptic ulcer disease, mild and moderate to severe liver disease, and malignant disease between these three groups of patients. The oldest patients were found in the no CCY group followed by the early CCY group. The proportions of congestive heart failure, chronic pulmonary diseases, and CCI scores were highest in the no CCY group followed by the early CCY group. The proportion of peptic ulcer disease, liver disease, and malignant diseases were highest in the no CCY group followed by the delayed CCY group. The general conditions were the worst in the no CCY patients in our real-world study. All of the CCI score comparison results are shown in Table 3.
Recurrent biliary events
The analysis of RBEs was divided into two time periods after index admission: from day 1 to day 60, and day 61 to day 360. There were 239 patients who underwent early CCY and another 1588 patients who did not undergo CCY initially at index admission. Within the first 60 days, there were 44 RBEs that occurred in 39 early CCY patients and 292 RBEs that occurred in 238 non-early-CCY patients. The RBE rate was 18.03% in the early CCY group and 17.78% in the non-early-CCY group. There were no significant differences (p = 0.934) between these two RBE rates. RBE event-free survival was analyzed with Kaplan-Meier statistics as shown in Fig. 2A.
During the second time period, from day 61 to day 360, 38 RBEs occurred in 23 (of 239) patients in the early CCY group, 16 RBEs occurred in 11 (of 148) patients in the delayed CCY group, and 620 RBEs occurred in 316 (of 1440) patients in the no CCY group. The RBE event-free survival rates were 85.04%, 89.54%, 64.45%, respectively, and there were significant differences between early and delayed CCY compared to no CCY (p < 0.0001), as shown in Fig. 2B.
Medical expenses
Medical expenses for index admission, delayed CCY, subsequent admissions and ER visits due to subsequent RBEs, together with total medical charges, were calculated for the three groups. The average medical expense for the early CCY patients at index admission was 146,717 NT dollars, which was significantly higher than that for the delayed CCY and no CCY patients (p < 0.001). The average financial cost for the delayed CCY patients was 81,759 NT dollars. The average cost for RBEs was 11,026 NT dollars for the early CCY group, 8,960 NT dollars for the delayed CCY group, and 28,378 NT dollars for the no CCY group. The average medical expenses for RBEs was the lowest in the delayed CCY group (p = 0.004) and was statistically different from the early and no CCY groups. The average amounts of total medical expenses were the lowest for the no CCY group (p < 0.001) and were similar for the early and delayed CCY groups (p = 0.294). The medical cost comparisons are shown in Table 4.
Discussion
In our study, the data were collected for patients who underwent therapeutic ERCP for choledocholithiasis without cholecystitis (from a retrospective database that included a random selection of approximately 10% of the Taiwan population), and we noticed that only 21.2% underwent CCY within 60 days of the index admission. This phenomenon can be attributed to cultural factors and the different types of CBD stones (the brownish stones resulting from chronic infection, without gallbladder stones) that play an important role in the Asian population21. Forty-four percent of the patients completed treatment at local and regional hospitals (as opposed to medical centers). Compared with current data from Western countries – where the rate of laparoscopic CCY in Australia is well over 95%, the rate of conversion to open CCY is only approximately 2.5%, and the rate of laparoscopic CCY in the United States of America is above 90%9 – the proportion of laparoscopic CCY in our results is only 51.16%. The average hospital stay was prolonged in open CCY patients, regardless of whether early or late CCY was performed. This outcome may be another reason that the proportion of patients willing to undergo prophylactic CCY treatment in Taiwan is relatively low.
Regarding the proportion of laparoscopic CCY, we saw a higher laparoscopic CCY rate in the delayed CCY group compared with that of the early CCY group; this outcome was different from the main worldwide study results. This outcome can be explained by noting that (1) we saw more chronic pulmonary disease patients (31.8% vs 21.6%) who were possibly less tolerant of the air effects of the laparoscopic surgery, in our early CCY group; (2) there was a relative low confidence level among surgeons and popularity of laparoscopic surgical equipment in local and regional hospitals in Taiwan between 2004–2011.
Timing of prophylactic cholecystectomy
Early CCY, rather than delayed CCY (>7 days after admission), is preferable for patients who require hospitalization for acute cholecystitis22,23 and selected gallstone pancreatitis patients24,25. In the Western world (with better medical standards), the same finding was reproduced for prophylactic CCY for symptomatic choledocholithiasis patients who underwent ERCP. Previous studies showed that early CCY could prevent the RBEs that occurred while waiting for the procedure and reduce the rate of subsequent events. As we know, repeated endoscopic biliary intervention could be used as rescue therapy26,27,28 for dealing with laparoscopic CCY complications. In our study, early CCY did not reduce the interval RBEs compared with delayed CCY for patients of older age and poor cardiopulmonary function. This outcome may have occurred because most clinical studies were done with experienced doctors in well-equipped hospitals. Our results show that early CCY does not guarantee reduction of interval RBEs in a less experienced and less well equipped general practice environment.
We found that CCY, either early or delayed, reduced the subsequent RBEs in the following year; this finding is consistent with the results of many small prospective studies.
Medical expenses
With financial impact taken into consideration, the method of delayed CCY leads to a smaller medical expense under the clinical practice pattern in Taiwan. The early CCY method leads to an even larger average total medical expense in the following year compared with the no CCY group. After we evaluated the costs of laparoscopic CCY and open CCY, early open CCY patients spent 167115 NT dollars and 19 admission days on average, while late open CCY patients spent 124069 NT dollars and 14 admission days on average. The costs and hospital stays for laparoscopic CCY, 94339 NT dollars in 10 days and 54055 NT dollars in 5 days in early and late laparoscopic CCY patients, respectively, were much lower than that for open CCY patients. The detailed comparisons of laparoscopic CCY and open CCY are listed in the supplementary table. The proportion of open CCY in the early CCY group is high, and this proportion helps to explain why the medical expenses are much higher in the early CCY group compared to the delayed CCY or no CCY groups. Our results support the two-stage treatment clinical pattern29 under the current diagnosis-related group (DRG) charges (National Health Insurance) for cholelithiasis used in Taiwan.
There are limitations to our study. For example, medical comorbidity associated with retrospective database analysis-related selection bias may confound the association between the timing of surgeries and the risks of subsequent RBEs. This analysis was conducted using a randomly selected population-based database, reflecting the current medical practice pattern in Taiwan, and we acknowledge the results could be different for highly skilled surgical hospitals. Additionally, the study groups were heterogeneous in age and some parameters of CCI scores. Further prospective randomized studies involving different levels of hospitals may be needed to clarify these issues.
In conclusion, we find that CCY does protect patients from subsequent RBEs in the following year, but early CCY at index admission does not provide protection for choledocholithiasis patients who underwent therapeutic ERCP in general practice in Taiwan. The method of delayed CCY can reduce medical expenses and the risks of subsequent RBEs and increase the proportion of laparoscopic CCY in Taiwan’s general practice environment.
References
Nealon, W. H., Urrutia, F., Fleming, D. & Thompson, J. C. The economic burden of gallstone lithotripsy. Will cost determine its fate? Ann Surg 213, 645–649, discussion 649–650 (1991).
Bodmer, M., Brauchli, Y. B., Krahenbuhl, S., Jick, S. S. & Meier, C. R. Statin use and risk of gallstone disease followed by cholecystectomy. JAMA 302, 2001–2007, https://doi.org/10.1001/jama.2009.1601 (2009).
Everhart, J. E. & Ruhl, C. E. Burden of digestive diseases in the United States part I: overall and upper gastrointestinal diseases. Gastroenterology 136, 376–386, https://doi.org/10.1053/j.gastro.2008.12.015 (2009).
Schirmer, B. D., Winters, K. L. & Edlich, R. F. Cholelithiasis and cholecystitis. J Long Term Eff Med Implants 15, 329–338 (2005).
Huang, J. et al. Nationwide epidemiological study of severe gallstone disease in Taiwan. BMC Gastroenterol 9, 63, https://doi.org/10.1186/1471-230X-9-63 (2009).
Shaffer, E. A. Epidemiology and risk factors for gallstone disease: has the paradigm changed in the 21st century? Curr Gastroenterol Rep 7, 132–140 (2005).
Shaffer, E. A. Gallstone disease: Epidemiology of gallbladder stone disease. Best Pract Res Clin Gastroenterol 20, 981–996, https://doi.org/10.1016/j.bpg.2006.05.004 (2006).
Schiphorst, A. H. et al. Timing of cholecystectomy after endoscopic sphincterotomy for common bile duct stones. Surg Endosc 22, 2046–2050, https://doi.org/10.1007/s00464-008-9764-8 (2008).
Huang, R. J., Barakat, M. T., Girotra, M. & Banerjee, S. Practice Patterns for Cholecystectomy After Endoscopic Retrograde Cholangiopancreatography for Patients With Choledocholithiasis. Gastroenterology 153, 762–771 e762, https://doi.org/10.1053/j.gastro.2017.05.048 (2017).
Boerma, D. et al. Wait-and-see policy or laparoscopic cholecystectomy after endoscopic sphincterotomy for bile-duct stones: a randomised trial. Lancet 360, 761–765, https://doi.org/10.1016/S0140-6736(02)09896-3 (2002).
Lau, J. Y. et al. Cholecystectomy or gallbladder in situ after endoscopic sphincterotomy and bile duct stone removal in Chinese patients. Gastroenterology 130, 96–103, https://doi.org/10.1053/j.gastro.2005.10.015 (2006).
Phillips, M. R. et al. Surgical and endoscopic management of remnant cystic duct lithiasis after cholecystectomy–a case series. J Gastrointest Surg 18, 1278–1283, https://doi.org/10.1007/s11605-014-2530-4 (2014).
Reinders, J. S. et al. Early laparoscopic cholecystectomy improves outcomes after endoscopic sphincterotomy for choledochocystolithiasis. Gastroenterology 138, 2315–2320, https://doi.org/10.1053/j.gastro.2010.02.052 (2010).
Jones, M., Johnson, M., Samourjian, E., Schlauch, K. & Ozobia, N. ERCP and laparoscopic cholecystectomy in a combined (one-step) procedure: a random comparison to the standard (two-step) procedure. Surg Endosc 27, 1907–1912, https://doi.org/10.1007/s00464-012-2647-z (2013).
Cheng, T. M. Taiwan’s new national health insurance program: genesis and experience so far. Health Aff (Millwood) 22, 61–76 (2003).
Wu, C. Y. et al. Early Helicobacter pylori eradication decreases risk of gastric cancer in patients with peptic ulcer disease. Gastroenterology 137(1641–1648), e1641–1642, https://doi.org/10.1053/j.gastro.2009.07.060 (2009).
Wu, C. Y. et al. Histamine2-receptor antagonists are an alternative to proton pump inhibitor in patients receiving clopidogrel. Gastroenterology 139, 1165–1171, https://doi.org/10.1053/j.gastro.2010.06.067 (2010).
Dean AG, S. K. & Soe, M. M. OpenEpi: Open Source Epidemiologic Statistics for Public Health, Version., www.OpenEpi.com (updated 2013/04/06, accessed 2018/01/06).
Li, V. K., Yum, J. L. & Yeung, Y. P. Optimal timing of elective laparoscopic cholecystectomy after acute cholangitis and subsequent clearance of choledocholithiasis. Am J Surg 200, 483–488, https://doi.org/10.1016/j.amjsurg.2009.11.010 (2010).
Gurusamy, K. S., Nagendran, M. & Davidson, B. R. Early versus delayed laparoscopic cholecystectomy for acute gallstone pancreatitis. Cochrane Database Syst Rev, CD010326, https://doi.org/10.1002/14651858.CD010326.pub2 (2013).
Tsui, W. M. et al. Hepatolithiasis and the syndrome of recurrent pyogenic cholangitis: clinical, radiologic, and pathologic features. Semin Liver Dis 31, 33–48, https://doi.org/10.1055/s-0031-1272833 (2011).
Riall, T. S., Zhang, D., Townsend, C. M. Jr., Kuo, Y. F. & Goodwin, J. S. Failure to perform cholecystectomy for acute cholecystitis in elderly patients is associated with increased morbidity, mortality, and cost. J Am Coll Surg 210, 668–677, 677–669, doi:10.1016/j.jamcollsurg.2009.12.031 (2010).
Gurusamy, K. S. & Samraj, K. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Cochrane Database Syst Rev, CD005440, https://doi.org/10.1002/14651858.CD005440.pub2 (2006).
Uhl, W. et al. Acute gallstone pancreatitis: timing of laparoscopic cholecystectomy in mild and severe disease. Surg Endosc 13, 1070–1076 (1999).
Aboulian, A. et al. Early cholecystectomy safely decreases hospital stay in patients with mild gallstone pancreatitis: a randomized prospective study. Ann Surg 251, 615–619, https://doi.org/10.1097/SLA.0b013e3181c38f1f (2010).
Kaffes, A. J. et al. Impact of endoscopic intervention in 100 patients with suspected postcholecystectomy bile leak. Gastrointest Endosc 61, 269–275 (2005).
Sandha, G. S., Bourke, M. J., Haber, G. B. & Kortan, P. P. Endoscopic therapy for bile leak based on a new classification: results in 207 patients. Gastrointest Endosc 60, 567–574 (2004).
Chow, S. et al. Successful treatment of post-cholecystectomy bile leaks using nasobiliary tube drainage and sphincterotomy. Am J Gastroenterol 92, 1839–1843 (1997).
Hu, W. Y., Yeh, C. F., Shiao, A. S. & Tu, T. Y. Effects of diagnosis-related group payment on health-care provider behaviors: A consecutive three-period study. J Chin Med Assoc 78, 678–685, https://doi.org/10.1016/j.jcma.2015.06.012 (2015).
Acknowledgements
This work was jointly supported by grants from Chung Shan Medical University Hospital research program, Taichung, Taiwan (CSH- 2013-C-032).
Author information
Authors and Affiliations
Contributions
Conception and design: Chi-Chih Wang, Ming-Hseng Tseng, Chun-Che Lin, Acquisition of data: Ming-Hseng Tseng, Wen-Wei Sung, Analysis and interpretation of data: Chi-Chih Wang, Yao-Tung Wang, Drafting of the manuscript: Chi-Chih Wang, Ming-Chang Tsai, Tzu-Wei Yang, Critical revision of the manuscript: Ming-Hseng Tseng, Shih-Ming, Huang, Hsuan-Yi Chen, Statistical analysis: Ming-Hseng Tseng, Wen-Wei Sung, Supervision: Ming-Hseng Tseng, Chun-Che Lin.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, CC., Tsai, MC., Wang, YT. et al. Role of Cholecystectomy in Choledocholithiasis Patients Underwent Endoscopic Retrograde Cholangiopancreatography. Sci Rep 9, 2168 (2019). https://doi.org/10.1038/s41598-018-38428-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-38428-z
This article is cited by
-
Solve study: a study to capture global variations in practices concerning laparoscopic cholecystectomy
Surgical Endoscopy (2022)
-
Destiny for Rendezvous: Is Cholecysto/Choledocholithiasis Better Treated with Dual- or Single-Step Procedures?
Digestive Diseases and Sciences (2022)
-
Outcomes following early versus delayed cholecystectomy performed for acute cholangitis
Surgical Endoscopy (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.