Abstract
To explore the influence of dermatomyositis (DM)-specific cutaneous manifestations (scm) on systemic coagulation and fibrinolysis, we retrospectively studied plasma D-dimer levels with/without venous thromboembolism (VTE), malignancy, infection or other connective tissue diseases (CTDs) and scm. One hundred fifty patients with DM were retrospectively investigated using medical records regarding scm, VTE, malignancy, infection, other CTDs, laboratory data and systemic corticosteroid therapy. All DM patients were categorized as follows: group 1, without scm, VTE, infection, malignancy or other accompanying CTDs; group 2, with scm only; and group 3, with VTE, infection, malignancy and other accompanying CTDs but without scm. The D-dimer plasma levels were significantly increased in group 3 compared with healthy subjects and those in groups 1 and 2 (p < 0.001). The D-dimer plasma level in group 2 was significantly increased compared with healthy subjects and those in group 1 (p < 0.001). Increased D-dimer plasma levels were detected in DM patients with scm without detectable VTE, malignancy, infection or accompanying CTDs. In addition to the known risk factors for increased plasma D-dimer levels in DM patients, including VTE, malignancy, infection and other accompanying autoimmune diseases, the presence of cutaneous manifestations should be considered as a new clinical risk factor.
Similar content being viewed by others
Introduction
Venous thromboembolism (VTE) includes deep venous thrombosis (DVT) and pulmonary embolism (PE) and indicates the presence of a risk for emergency and potentially fatal disease1. Patients with dermatomyositis (DM) have an increased risk of VTE2,3,4,5,6, and the corresponding multivariable hazard ratio for VTE was 8.39 (95% confidence interval [CI]: 3.04–23.14) compared with subjects without DM7. DVT is occasionally asymptomatic8, and most cases with symptomatic PE have additional asymptomatic DVTs9. Therefore, the proper evaluation of accompanying VTE in DM is important.
A close relationship between inflammation and coagulation is well recognized10,11. On the other hand, some severe skin inflammatory diseases cause systemic diseases, including cardiovascular disease12.
DM is an autoimmune inflammatory disease, with characteristic cutaneous manifestations and inflammatory myopathy. Little is known about the influence of these cutaneous manifestations on systemic coagulation and fibrinolysis systems in DM.
Methods
Patients
A retrospective cohort study was performed for all DM patients with data on D-dimer plasma levels who visited the clinic of Dermatology and/or Hematology at Mie University Hospital in Japan from January 1, 2010 to April 30, 2017. DM was diagnosed based on the Classification by Bohan and Peter13,14. Clinically amyopathic DM in this study included patients with amyopathic DM or hypomyopathic DM15,16. The medical records of 150 DM patients were reviewed, and the records were followed-up from the first diagnosis or first appointment until the end of the study or death. The following patients were excluded: (i) patients receiving preceding anticoagulation therapy or chemotherapy; (ii) patients with other known blood coagulation disorders; and (iii) patients within three months of major surgical therapies, cancer chemotherapy or trauma.
Methods
VTE was diagnosed based on clinical manifestations and was confirmed by appropriate physical and radiological examinations, including a whole-leg compression ultrasound examination, ventilation-perfusion scan and/or contrast computed tomography (CT).
The malignancy workup included a complete physical examination, chest radiography, whole-body CT, oesophagogastroduodenoscopy, colonoscopy, mammogram, Papnicolaou smear, trans-vaginal ultrasound examination, cystoscopy, bone marrow aspirate and organ biopsy.
Infection was diagnosed based on physical examinations, radiological examinations (chest radiography, head/neck/chest/abdomen/pelvic CT) and clinical laboratory examinations, including a complete blood cell count; plasma levels of C-reactive protein, lactate dehydrogenase, glutamic oxaloacetic transaminase and glutamic pyruvate transaminase; cytomegalovirus antigenaemia assay; serum beta-D-glucan; procalcitonin; urine qualitative measurement and urine sediment examination.
DM patients without VTE, infection or malignancy for three months before and after D-dimer testing were included in the study.
The presence of cutaneous manifestations of DM was evaluated clinically by well-trained dermatologists and histologically by pathologists. Cutaneous manifestations included heliotrope rash, Gottron’s papule, Gottron’s sign, facial erythema, periungual changes, inverse Gottron’s papules (Sign), mechanic’s hands, V-neck sign, shawl sign, flagellate erythema, purpura, calcinosis cutis, skin ulcers and erythroderma17.
Measurement of plasma D-dimer
Plasma D-dimer levels were measured via a latex agglutination method using LPIA-ACE D-Dimer II (LSI Medience Corporation, Tokyo, Japan). The normal range of D-dimer levels by the kit used in the present study was less than 1.0 μg/mL, which was established based on the evaluation of 70 healthy subjects.
When the D-dimer levels were measured more than twice in the same patient, we adopted the D-dimer test results that were obtained on the day closest to when the following events were identified: presence/absence of VTE, infection and malignancy. The D-dimer data obtained shortly after major surgery or trauma were omitted.
The Human Ethics Review Committee of Mie University School of Medicine approved this study protocol (approve number: 1728), and informed consent was obtained from all of the patients. This study was performed in accordance with the principles of the Declaration of Helsinki.
Statistical analyses
The results were expressed as the medians (Me) (25th–75th percentiles [IQR]). Differences between the groups were analysed using the Mann-Whitney U test. p-values < 0.05 were considered statistically significant. The significance of frequency was examined using the chi-squared test. All reported p-values are two-sided. All of the statistical analyses were performed using Graphpad Prism software (GraphPad Software, Inc., San Diego, CA, USA).
Results
The DM patients in this study are listed in Table 1. The final samples included 150 DM patients (112 women, 38 men; mean [standard deviation] age, 60.0 [14.2] years). The median follow-up time of this cohort was 10.0 years (range 0.5–25.0 years), with a total follow-up of 1645.5 person-years. In this study, plasma D-dimer levels were measured when cutaneous manifestation disappeared following treatment in 48% (72/150) of DM patients. VTE (n = 11) included deep vein thrombosis (DVT; n = 8), DVT and pulmonary embolism (PE) (n = 2) and PE (n = 1). Patients with VTE taking intravenous immunoglobulin or oral contraceptive pills were excluded. Cases in whom VTE developed after surgery, long-term recumbence, trauma or an airplane flight were excluded. The calculated incidence rate of VTE in DM patients in this study was 6.68 per 1,000 person-years. Malignancy (n = 18) included breast cancer (n = 6), lung cancer (n = 4), colorectal cancer (n = 3), ovarian cancer (n = 2), gastric cancer (n = 1), bladder cancer (n = 1) and gastric cancer and colorectal cancer (n = 1). Patients in whom malignancy had been completely cured were excluded. Infectious diseases (n = 23) included pneumocystis pneumonia (PCP) (n = 3), cytomegalovirus (CMV) infection and PCP (n = 3), bacterial pneumonia (n = 3), CMV infection (n = 2), herpes zoster (n = 2), phlegmone (n = 2), bacteraemia (n = 1), fungaemia (n = 1), viral enteritis (n = 1), cholecystitis and bacteraemia (n = 1), urinary tract infection (n = 1), subcutaneous abscess (n = 1), lung tuberculosis (n = 1) and nontuberculous mycobacterial pulmonary infection (n = 1). Overlapping CTDs (n = 26) included rheumatoid arthritis (RA; n = 11), systemic sclerosis (SSc; n = 8), Sjogren’s syndrome (SS; n = 3), SSc and RA (n = 2) and SSc and SS (n = 2).
Plasma D-dimer and lactate dehydrogenase (LDH) levels were significantly increased in DM patients with VTE compared with those without VTE. The duration of systemic corticosteroid therapy was longer in DM patients without VTE compared with those with VTE (Me 0.71 years [IQR 0.04–8.5] vs. Me 0.28 years [IQR 0.08–5.2]; p = 0.52) (Table 2).
When all DM patients were divided into two groups according to the normal range of D-dimer levels (<1.0 μg/mL), the incidence of VTE, malignancy, infection and cutaneous manifestations were significantly increased in DM patients with high D-dimer levels (≥1 μg/mL; HDM) compared with those with normal D-dimer levels (<1 μg/mL; LDM) (p = 0.016, 0.007, 0.029 and <0.001, respectively). Age, C-reactive protein and LDH levels were significantly increased in the HDM group compared with the LDM group (p < 0.001). The platelet (PLT) count was significantly reduced in the HDM group compared with the LDM group (p = 0.034), and activated partial thromboplastin time (APTT) was significantly reduced in the HDM group compared with the LDM group (p = 0.021). The dose of systemic corticosteroid therapy in the HDM group was increased compared with that in the LDM group, but the duration of corticosteroid therapy in the HDM group was reduced compared with the LDM group (p = 0.002 and 0.014, respectively) (Table 3).
In DM patients without VTE, malignancy, infection or other CTD, the plasma levels of D-dimer and LDH were significantly increased in patients with cutaneous manifestations compared with those without cutaneous manifestations (p < 0.001 and 0.004, respectively). The duration and total dose of corticosteroid therapy were significantly reduced in patients with cutaneous manifestations compared with those without cutaneous manifestations (p < 0.001) (Table 4). Interestingly, 83% (34/41) of DM patients with cutaneous manifestations exhibited increased plasma D-dimer levels (Me [IQR]: 1.56 [0.93–3.48] μg/mL; normal <1 μg/mL); however, this proportion was only 31% (14/45) in patients without cutaneous manifestations (Table 4).
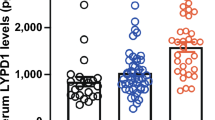
To further analyse the effects of various clinical manifestations on plasma D-dimer levels, patients were categorized into the following three groups: group 1, without cutaneous manifestations, VTE, infection, malignancy or other accompanying CTDs; group 2, with cutaneous manifestations only; and group 3, with VTE, infection, malignancy and other accompanying CTDs but without cutaneous manifestations. D-dimer plasma levels in the three groups were significantly increased compared with healthy subjects (Me [IQR]; 0.28 [0.10–0.40] μg/mL) (p < 0.001). D-dimer plasma levels were significantly increased in group 2 (Me [IQR]; 1.56 [0.93–3.48] μg/mL) compared with group 1 (Me [IQR]; 0.50 [0.26–1.07] μg/mL) (p < 0.001). D-dimer plasma levels were also significantly increased in group 3 (Me [IQR]; 4.41 [1.54–9.00] μg/mL) compared with groups 1 and 2 (p < 0.001). No significant differences in age or sex were noted between groups (Fig. 1).
No specific skin manifestations were related to increased plasma D-dimer levels (Table 5).
Discussion
VTE occasionally requires emergency care and is a potentially fatal disease. Fortunately, the incidence of VTE in the general population is relatively low at approximately 1.17 per 1,000 person-years in a cohort of Olmsted County18. An increased risk for VTE has been reported in patients with DM3,4,5,6,7. Surprisingly, the incidence rate of VTE in DM patients in this study was relatively high at 6.68 per 1,000 person-years. However, the causative factors for VTE in DM remain unclear. Immobility increases the risk of VTE, but the serum CPK levels of the patients with VTE in this study were not increased. Thus, immobility due to severe myositis is not suspected for VTE in DM. Serum LDH levels were increased in DM patients with VTE compared with those without VTE. LDH isozyme in the lung is a component of LDH, and LDH serum levels are increased in PE19,20. In this study, VTE (n = 11) was noted in 3 PE patients, thus influencing this result. Systemic corticosteroid therapy activates coagulation cascades21 and increases the risk of VTE22. Indeed, in this study, APTT was significantly reduced in the HDM group, which was prescribed greater doses of steroids, compared with the LDM group. The difference seemed minimal, but the steroid dose potentially influenced this difference. However, no marked differences in the dose, duration or total dose of systemic corticosteroids were noted between patients with and without VTE in the present study. Thus, neither the severity of myositis nor the therapeutic use of corticosteroids increased the risk of VTE in DM patients in this study. The PLT count was significantly reduced in the HDM group compared with the LDM group. This difference was minimal and might have been affected by the number of infection and malignancy patients in the HDM group.
D-dimers are the products of fibrin hydrolysis, and increased D-dimer levels indicate the presence and digestion of stable fibrin and the activation of the coagulation and fibrinolysis cascades23. The evaluation of plasma D-dimer levels is accepted as a clinical diagnostic test for the presence of VTE24. VTE is a potentially fatal disease, and surveillance of VTE using clinical laboratory tests, including the D-dimer test, is useful for the early detection of VTE of DM. D-dimer levels are also increased in various accompanying diseases, and the careful evaluation of plasma D-dimer levels in cases without clinically obvious thromboembolic disease is required (Supplementary Figure). DM patients are commonly complicated by malignancy, infection and/or other CTDs or RA. Previous studies have demonstrated increased plasma D-dimer levels in patients without demonstrable thrombosis but with malignancy25, infection26 and other autoimmune diseases27.
A close relationship between inflammation and coagulation is well recognized10,11. Various inflammatory mediators activate the coagulation systems, thus downregulating natural anticoagulant mechanisms28. Increased plasma D-dimer levels are not limited to thrombotic diseases and have been reported in some skin diseases, including urticaria29,30, angioedema31, bullous pemphigoid32, atopic dermatitis33 and cutaneous drug reactions33. These diseases have different pathogenic mechanisms, and the existence of multiple different mechanisms underlying increased plasma D-dimer is suspected. Therefore, inflammatory reactions of the cutaneous manifestation itself might be involved in the increased plasma D-dimer levels. Microvascular endothelial injury is a characteristic pathogenic mechanism of DM. The vascular endothelium plays important roles in haemostasis and thrombosis, and an inflammatory mediator-stimulated endothelium initiates coagulation system activation. In this study, plasma D-dimer levels were increased in DM patients with skin manifestations, possibly due to endothelial cell injury associated with DM.
DM-specific skin manifestations represent clinically obvious small-vessel vasculitis and capillary thrombosis, including Gottron’s sign and periungual changes (nail fold thrombosis). These lesions also exhibit histopathological changes of cutaneous vasculitis34,35, vascular fibrin deposition36,37 and C5b-9 deposition in cutaneous vessels36 as well as endothelial injury36. Vascular fibrin deposition was demonstrated in 65% of skin biopsies of DM patients, (93% in amyopathic DM), C5b-9 deposition in 100% (100% in amyopathic DM) and endothelial injury in 78% (100% in amyopathic DM)36. Fibrin is hydrolysed to produce D-dimers, and C5b-9 is associated with coagulation38. Increases in plasma D-dimer levels have been reported in various autoimmune vasculitis conditions, including antineutrophil cytoplasmic antibody-associated vasculitis39, cutaneous polyarteritis nodosa29, Takayasu’s arteritis40, eosinophilic granulomatosis with polyangiitis41 and IgA vasculitis42. Thus, vasculitis induced by skin manifestations is suspected to be pathogenic for plasma D-dimer elevation in DM. Regarding the association between inflammatory cytokines and DM, inflammatory cytokine expression (IL-1α, IL-1β and TNF-α) is increased in the muscular lesions of DM43. The involvement of IL-1s in the pathogenesis of skin manifestations in DM was proven based on the clinical effects of IL-1 antagonist when administered for the treatment of DM-associated skin ulcers44. Inflammatory cytokines affect tissue factor by playing a central role in the initiation of inflammation-induced coagulation and the regulation of physiologic anticoagulation11,45 (Fig. 2). In addition, a positive association has been reported between inflammatory mediators and VTE recurrence46.
Within DM-specific skin manifestations, as described earlier, coagulation is thought to be locally activated according to local inflammation associated with the development of DM-specific skin manifestations (Fig. 2). In this study, increased plasma D-dimer levels were associated with DM-specific skin manifestations, even if there was no thrombosis, infection, malignancy or other autoimmune disease (Fig. 1). From this, strong inflammation within DM-specific skin manifestations is thought to first induce local activation of coagulation, which potentially leads to the systemic activation of coagulation. When considering other pathologies of increased D-dimer plasma levels in DM patients with DM-specific cutaneous manifestations, it is also possible that intravascular inflammation influences the systemic activation of coagulation. However, in this study, CRP plasma levels were not significantly increased in DM patients with DM-specific cutaneous manifestations compared with those of DM patients without DM-specific cutaneous manifestations (Table 4). Therefore, inflammation within DM-specific skin manifestations likely influences the systemic activation of coagulation.
LDH is present in various organs, including the skin, lung and others. We thus considered the effect of LDH on pulmonary infarction (Table 2) and skin (Table 4). In Table 3, we also considered the effect from various organs affected by malignancy or infection as well as pulmonary infarction and skin. Clinically, LDH is not a specific test for the assessment of suspected DVT or the examination of coagulation compared with D-dimer levels. In DM, a clinically important association is noted between increased plasma D-dimer levels and DM-specific skin manifestations, as our current evidence suggests. This finding suggests that the plasma D-dimer levels in DM patients exhibit clinical importance similar to that noted in SLE47.
The limitations associated with our study are its retrospective nature and the limited number of patients involved. In addition, we cannot completely exclude the possible presence of micro VTE in patients with increased plasma D-dimer levels, which is undetectable, even when using various imaging examinations.
However, the D-dimer levels in 7 (17%) of 41 DM patients with skin manifestations were within the normal range in this study (Table 4). Therefore, the presence of cutaneous manifestations in DM patients does not necessarily indicate increased plasma D-dimer levels. This finding might be due to the time of D-dimer sampling during the clinical course of DM and the heterogeneity of skin manifestations in DM. Unfortunately, we were unable to detect a specific DM skin lesion relevant to D-dimer elevation in this study due to the relatively small sample size (Table 5). A long lag time is occasionally present between D-dimer elevation and PE and DVT development48. Further studies are required to determine specific skin manifestations and the ideal sampling time for the evaluation of D-dimer levels for the risk of VTE management.
Conclusions
In the present study, we identified DM-specific cutaneous manifestations as a new marker for activated coagulation cascade and increased plasma D-dimer levels. The risk of VTE is increased in DM and SLE patients, and we should carefully monitor plasma D-dimer levels, skin manifestations and clinical manifestations of thrombotic events in DM patients.
References
Goldhaber, S. Z., Visani, L. & De Rosa, M. Acute pulmonary embolism: clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER). Lancet. 353(9162), 1386–9 (1999).
Gaitonde, S. D. & Ballou, S. P. Deep venous thrombosis in dermatomyositis. J Rheumatol. 35(11), 2288 (2008).
Zöller, B., Li, X., Sundquist, J. & Sundquist, K. Risk of pulmonary embolism in patients with autoimmune disorders: a nationwide follow-up study from Sweden. Lancet. 379(9812), 244–249 (2012).
Chung, W. S., Lin, C. L., Sung, F. C., Lu, C. C. & Kao, C. H. Increased risk of venous thromboembolism in patients with dermatomyositis/polymyositis: a nationwide cohort study. Thromb Res. 134(3), 622–626 (2014).
Ramagopalan, S. V., Wotton, C. J., Handel, A. E., Yeates, D. & Goldacre, M. J. Risk of venous thromboembolism in people admitted to hospital with selected immune-mediated diseases: record-linkage study. BMC Med. 10, 9:1 (2011).
Selva-O’Callaghan, A., Fernández-Luque, A., Martínez-Gómez, X., Labirua-Iturburu, A. & Vilardell-Tarrés, M. Venous thromboembolism in patients with dermatomyositis and polymyositis. Clin Exp Rheumatol. 29(5), 846–9 (2011).
Carruthers, E. C., Choi, H. K., Sayre, E. C. & Aviña-Zubieta, J. A. Risk of deep venous thrombosis and pulmonary embolism in individuals with polymyositis and dermatomyositis: a general population-based study. Ann Rheum Dis. 75, 110–116 (2016).
Satoh, T. et al. High incidence of silent venous thromboembolism before treatment in ovarian cancer. Br J Cancer. 97, 1053–1057 (2007).
Kearon, C. Natural history of venous thromboembolism. Circulation. 107, I22–30 (2003).
Cermak, J. et al. Vercellotti. C-Reactive Protein Induces Human Peripheral Blood Monocytes to Synthesize Tissue Factor. Blood. 82(2), 513–520 (1993).
Levi, M. & van der Poll, T. Inflammation and coagulation. Crit Care Med. 38(2 Suppl), S26–34 (2010).
Yamanaka, K. et al. Persistent release of IL-1s from skin is associated with systemic cardio-vascular disease, emaciation and systemic amyloidosis: the potential of anti-IL-1 therapy for systemic inflammatory diseases. PLoS One Aug 13; 9(8) (2014).
Bohan, A. & Peter, J. B. Polymyositis and dermatomyositis (first of two parts). N Engl J Med. 292, 403–7 (1975).
Bohan, A. & Peter, J. B. Polymyositis and dermatomyositis (second of two parts). N Engle J Med. 292, 344–7 (1975).
Sontheimer, R. D. Cutaneous features of classic dermatomyositis and amyopathic dermatomyositis. Curr Opin Rheumatol. 11(6), 475–482 (1999).
Sontheimer, R. D. Would a new name hasten the acceptance of amyopathic dermatomyositis (dermatomyositis siné myositis) as a distinctive subset within the idiopathic inflammatory dermatomyopathies spectrum of clinical illness? J Am Acad Dermatol. 46(4), 626–636 (2002).
Muro, Y., Sugiura, K. & Akiyama, M. Cutaneous Manifestations in Dermatomyositis: Key Clinical and Serological Features-a Comprehensive Review. Clinic Rev Allerg Immunol. 51, 293–302 (2016).
Silverstein, M. D. et al. Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study. Arch Intern Med. 158(6), 585–93 (1998).
Ben, S. Q. et al. The dynamic changes of LDH isoenzyme 3 and D-dimer following pulmonary thromboembolism in canine. Thromb Res. 120(4), 575–83 (2007).
Babaoglu, E. et al. Importance of biomarkers in risk stratification of pulmonary thromboembolism patients. J Investig Med. 62(2), 328–31 (2014).
Brotman, D. J. et al. Effects of short-term glucocorticoids on hemostatic factors in healthy volunteers. Thromb Res. 118, 247–52 (2006).
Stuijver, D. J. et al. Use of oral glucocorticoids and the risk of pulmonary embolism: a population-based case–control study. Chest. 143, 1337–42 (2013).
Fareed, J. et al. Useful laboratory tests for studying thrombogenesis in acute cardiac syndromes. Clin Chem. 44(8 Pt 2), 1845–1853 (1998).
Wada, H. et al. Elevated levels of soluble fibrin or D-dimer indicate high risk of thrombosis. J Thromb Haemost. 4(6), 1253–8 (2006).
Mego, M. et al. Circulating tumour cells are linked to plasma D-dimer levels in patients with metastatic breast cancer. Thromb Haemost. 113(3), 593–8 (2015).
Kinasewitz, G. T. et al. Universal changes in biomarkers of coagulation and inflammation occur in patients with severe sepsis, regardless of causative micro-organism [ISRCTN74215569]. Crit Care. 8(2), R82–90 (2004).
Inoh, M., Tokuda, M., Kiuchi, H., Kurata, N. & Takahara, J. Evaluating systemic lupus erythematosus disease activity using molecular markers of hemostasis. Arthritis Rheum. 39(2), 287–91 (1996).
Esmon, C. T. The interactions between inflammation and coagulation. Br J Haematol. 131(4), 417–30 (2005).
Kirchhof, M. G., Lee, A. Y. & Dutz, J. P. D-dimer levels as a marker of cutaneous disease activity: case reports of cutaneous polyarteritis nodosa and atypical recurrent urticaria. JAMA Dermatol. 150(8), 880–884 (2014).
Takahagi, S. et al. Coagulation/fibrinolysis and inflammation markers are associated with disease activity in patients with chronic urticaria. Allergy. 65(5), 649–656 (2010).
Reshef, A., Zanichelli, A., Longhurst, H., Relan, A. & Hack, C. E. Elevated D-dimers in attacks of hereditary angioedema are not associated with increased thrombotic risk. Allergy. 70(5), 506–13 (2015).
Marzano, A. V., Tedeschi, A., Polloni, I., Crosti, C. & Cugno, M. Prothrombotic state and impaired fibrinolysis in bullous pemphigoid, the most frequent autoimmune blistering disease. Clin Exp Immunol. 171(1), 76–81 (2013).
Marzano, A. V. et al. Activation of coagulation in bullous pemphigoid and other eosinophil-related inflammatory skin diseases. Clin Exp Immunol. 165(1), 44–50 (2011).
Feldman, D., Hochberg, M. C., Zizic, T. M. & Stevens, M. B. Cutaneous vasculitis in adult polymyositis/dermatomyositis. J Rheumatol. 10(1), 85–9 (1983).
Kawakami, T., Mizoguchi, M., Saito, R. & Soma, Y. Histopathological evidence of small-vessel vasculitis within the skin and lungs associated with interstitial pneumonia in an adult patient with dermatomyositis. Clin Exp Dermatol. 33(4), 415–7 (2008).
Crowson, A. N. & Magro, C. M. The role of microvascular injury in the pathogenesis of cutaneous lesions of dermatomyositis. Hum Pathol. 27(1), 15–9 (1996).
Fiorentino, D., Chung, L., Zwerner, J., Rosen, A. & Casciola-Rosen, L. The mucocutaneous and systemic phenotype of dermatomyositis patients with antibodies to MDA5 (CADM-140): a retrospective study. J Am Acad Dermatol. 65(1), 25–34 (2011).
Wiedmer, T., Esmon, C. T. & Sims, P. J. Complement proteins C5b-9 stimulate procoagulant activity through platelet prothrombinase. Blood 68, 875–880 (1986).
Ma, T. T., Huang, Y. M., Wang, C., Zhao, M. H. & Chen, M. Coagulation and fibrinolysis index profile in patients with ANCA-associated vasculitis. PLoS One 19(9(5)), e97843 (2014).
Akazawa, H., Ikeda, U., Yamamoto, K., Kuroda, T. & Shimada, K. Hypercoagulable state in patients with Takayasu’s arteritis. Thromb Haemost. 75(5), 712–6 (1996).
Marzano, A. V., Tedeschi, A., Rossio, R., Fanoni, D. & Cugno, M. Prothrombotic state in Churg-Strauss syndrome: a case report. J Investig Allergol Clin Immunol. 20(7), 616–9 (2010).
Brendel-Müller, K., Hahn, A., Schneppenheim, R. & Santer, R. Laboratory signs of activated coagulation are common in Henoch-Schönlein purpura. Pediatr Nephrol. 16(12), 1084–8 (2001).
Lundberg, I., Ulfgren, A. K., Nyberg, P., Andersson, U. & Klareskog, L. Cytokine production n muscle tissue of patients with idiopathic inflammatory myopathies. Arthritis Rheum. 40(5), 865–74 (1997).
Groh, M. et al. Interleukin-1 receptor antagonist for refractory anti-MDA5 clinically amyopathic dermatomyopathy. Clinical Experimental Rheumatology. 33, 904–905 (2015).
Levi, M. & van der Poll, T. Two-way interactions between inflammation and coagulation. Trends Cardiovasc Med. 15(7), 254–9 (2005).
van Aken, B. E., den Heijer, M., Bos, G. M., van Deventer, S. J. & Reitsma, P. H. Recurrent venous thrombosis and markers of inflammation. Thromb Haemost. 83(4), 536–9 (2000).
Anders, H. J. Predicting thrombosis in systemic lupus erythmatosus. Nat Clin Pract Nephrol. 5(2), 68–69 (2009).
Kirchhof, M. G. & Dutz, J. P. Amyopathic dermatomyositis-related thrombophilia. JAMA Dermatol. 151(5), 559–61 (2015).
Author information
Authors and Affiliations
Contributions
K.H. designed the study and wrote the initial draft of the manuscript. H.W., K.Y. and H.M. contributed to the analysis and interpretation of data and assisted in the preparation of the manuscript. K.H., H.W., A.H., T.A., K.T., R.M., M.K. and K.Y. contributed to data collection and interpretation and critically reviewed the manuscript. All of the authors approved the final version of the manuscript and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Habe, K., Wada, H., Higashiyama, A. et al. Elevated plasma D-dimer levels in dermatomyositis patients with cutaneous manifestations. Sci Rep 9, 1410 (2019). https://doi.org/10.1038/s41598-018-38108-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-38108-y
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.