Abstract
Adult onset Pompe disease is a genetic disorder characterized by slowly progressive skeletal and respiratory muscle weakness. Symptomatic patients are treated with enzymatic replacement therapy with human recombinant alfa glucosidase. Motor functional tests and spirometry are commonly used to follow patients up. However, a serological biomarker that correlates with the progression of the disease could improve follow-up. We studied serum concentrations of TGFβ, PDGF-BB, PDGF-AA and CTGF growth factors in 37 adult onset Pompe patients and 45 controls. Moreover, all patients performed several muscle function tests, conventional spirometry, and quantitative muscle MRI using 3-point Dixon. We observed a statistically significant change in the serum concentration of each growth factor in patients compared to controls. However, only PDGF-BB levels were able to differentiate between asymptomatic and symptomatic patients, suggesting its potential role in the follow-up of asymptomatic patients. Moreover, our results point to a dysregulation of muscle regeneration as an additional pathomechanism of Pompe disease.
Similar content being viewed by others
Introduction
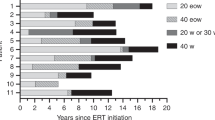
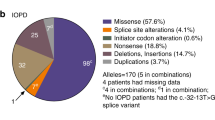
Pompe disease is an autosomal recessive disorder produced by mutations in the GAA gene, which codifies the enzyme acid alpha-glucosidase1. This enzyme metabolizes glycogen to glucose inside the lysosomes of the cells. A lack of it leads to an accumulation of glycogen in body tissues such as liver, neurons, smooth, skeletal or cardiac muscle2. Pompe disease has a wide clinical spectrum ranging from the classical infantile disease (IOPD) to late onset phenotype. IOPD patients develop a quickly progressive disease characterized by generalized muscle weakness and hypertrophic cardiomyopathy, leading to death in the first year of life if left untreated3. Enzymatic replacement therapy with alfa-glucosidase (ERT) is started as early as possible, because IOPD is life-threatening disorder and ERT clearly change patients’ clinical condition4,5.
In contrast, adult onset Pompe patients (AOPD) can have heterogeneous clinical presentations, ranging from isolated hyperckemia to weakness involving the respiratory, axial, pelvic and scapular girdle muscles6,7. Natural history studies suggest that muscle weakness in AOPD progresses very slowly. In some cases, patients develop subtle muscle symptoms, such as postural abnormalities or a change in their walking pattern, that do not influence general motor function and can therefore delay medical consultation8,9. Unlike the procedure for IOPD, guidelines recommend starting ERT in AOPD only if muscle or respiratory weakness is detected in clinical examination10. In fact, asymptomatic AOPD patients are currently followed up using different muscle function tests to try to identify changes in motor performance that could lead to the initiation of treatment11. However, it is possible that the process of muscle degeneration and fibro-fatty substitution, which is irreversible, could have started without yet producing significant changes in motor functional tests12. Moreover, it is not certain that common muscle function tests, such as the 6 minute walking test (6MWT), are precise enough to detect slight changes in motor performance13. For these reasons, having a serum growth factor able to identify patients in which fibro-fatty substitution has begun, would be of great utility14,15.
The main aim of our research was to study the serum concentration of a group of growth factors related to muscle fibrosis, degeneration and inflammation, in a cohort of 37 symptomatic and asymptomatic AOPD patients. We compared the serum concentration of Pompe patients with a control group. We also studied whether there were differences in the serum concentration of these growth factors between symptomatic and asymptomatic patients. In parallel, we evaluated the patients using several motor function tests, spirometry, quantitative muscle MRI (qMRI), and patient-reported outcome measures (PROMs), in order to establish whether or not a correlation between serum concentration and the clinical situation of the patients exists.
Results
Description of the cohort
37 AOPD patients were included in the study. Twenty-nine patients were symptomatic (18 women, 62.1%) and 8 were asymptomatic. Twenty-three of the 29 symptomatic patients were already receiving ERT when first sample was obtained. In the remaining 6 symptomatic patients, blood samples were obtained before ERT was started. Asymptomatic patients were studied in neuromuscular disorder units because high levels of hepatic enzymes or CKs were found in random checkup blood analyses (5 cases) or because they had relatives already diagnosed with Pompe disease (3 cases). The demographic and clinical data of these two groups are described in Table 1. Results of the motor function tests and muscle MRI of the Pompe cohort has been already reported15,16. We compared the ELISA results with serums obtained from age- and sex-matched controls (n = 45).
Growth factor serum levels in Pompe patients compared to controls
Our first aim was to study whether there were differences in growth factor serum levels between Pompe patients and controls. We observed significant differences in PDGF-BB, TGF-β, PDGF-AA and CTGF levels as is shown in Fig. 1. Serum PDGF-BB and TGF-β1 levels were significantly lower in Pompe patients compared to the control group. In the case of PDGF-BB, the median and interquartile range (IQR) value of Pompe serum levels were of 1.739 ng/ml (IQR: 1.467–2.186) compared to 2.360 ng/ml (IQR: 1.494–3.23) in controls (Mann-Whitney U test, p = 0.047). In the case of TGF-β1, Pompe median serum levels were of 46.17 ng/ml (IQR: 36.34–55.48) compared to 55.05 ng/ml (IQR: 46.79–64.8) in controls (Mann-Whitney U test, p = 0.007). However, serum PDGF-AA and CTGF levels were significantly higher compared to control samples. In the case of PDGF-AA, the median Pompe serum levels were 2630 ng/ml (IQR: 2161–3399) compared to 2242 ng/ml (IQR: 1642–3051) in controls (Mann-Whitney U test, p = 0.01). And in the case of CTGF, median Pompe serum levels were of 3.831 ng/ml (2.917–4.999) compared to 2.589 ng/ml (1.503–4.013) in controls (Mann-Whitney U test, p = 0.023).
Serum levels of different cytokines in control group and pompe group. (A) PDGF-BB levels, (B) TGF-β1, (C) PDGF-AA and (D) CTGF levels were measured. Variables are represented as median and interquartile range (IQR). Statistical significance of the results by Mann-Whitney test: *p ≤ 0.05 and **p ≤ 0.01.
PDGF-BB levels differentiate between symptomatic and asymptomatic Pompe patients
Our second aim was to assess whether any of the growth factors studied was able to differentiate between asymptomatic and symptomatic Pompe patients (Fig. 2). We observed that PDGF-BB levels were significantly lower in symptomatic patients (Median: 1.565 ng/ml (IQR: 1.405–2.096) compared to asymptomatic Pompe patients (Median: 2.038 ng/ml (IQR: 1.907–3.803) (Mann-Whitney U test, p = 0.044) (Fig. 2A). In contrast, we did not identify differences in TGF-β1, CTGF and PDGF-AA serum concentration between symptomatic and asymptomatic patients.
Serological levels of four growth factors in three different groups: control, symptomatic Pompe patients and asymptomatic Pompe patients. (A) PDGF-BB levels, (B) TGF-β1, (C) PDGF-AA and (D) CTGF levels were measured. Variables are represented as median and interquartile range (IQR). Comparisons were made using Mann-Whitney test. Statistical significance of the results; *p ≤ 0.05 and **p ≤ 0.01.
As there were significant differences in age between symptomatic and asymptomatic Pompe patients (Table 1), we decided to add a new group of young controls with a mean age of 23 years. We observed significant differences in PDGF-BB serum levels between symptomatic Pompe patients and all other groups, including young controls (mean age = 23 years old) (Mann-Whitney U test, p = 0.0012), all controls and asymptomatic Pompe patients. We did not observe significant differences between controls of different ages and between asymptomatic Pompe patients and young controls (Mann-Whitney U test, p > 0.05) (Fig. 3).
Serological levels of PDGF-BB in different groups: control, young controls, asymptomatic and symptomatic Pompe patients. Variables are represented as median and interquartile range (IQR). Comparisons were made using Mann-Whitney test. Statistical significance of the results; *p ≤ 0.05 and **p ≤ 0.01.
To further analyze whether PDGF-BB serum levels were useful for differentiating between symptomatic or asymptomatic patients, we used a receiver operating characteristics curve, or ROC curve, and analyzed area under the curve (AUC). The ROC curve (AUC: 0.737, p = 0.042, 95%CI: 0.539–0.935) (Fig. 4) confirmed that PDGF-BB levels were able to predict which patients were symptomatic and which were asymptomatic. Therefore, patients with lower values than the cut-off level (1.97 ng/ml) had a higher probability of being asymptomatic. Sensitivity and specificity were 75% and 76% respectively.
PDGF-BB levels decrease in Pompe patients but not in other muscle dystrophies
Since the function of PDGF-BB seems to be related with muscle regeneration, we analyzed serum levels of this growth factor in other muscle dystrophies in which regeneration increases, such as Duchenne muscle dystrophy (DMD), Becker muscle dystrophy (BMD) dysferlinopathy (DYSF) and facioscapulohumeral muscular dystrophy (FSH). Clinical and demographic features of these groups are described in Table 2.
We observed that PDGF-BB levels were significantly higher in DMD (Median: 3.14 ng/ml (IQR: 1.6–6.76) (Mann-Whitney U test, p = 0.0469) and BMD (Median: 3.681 ng/ml (IQR: 2.945–4.398) (Mann-Whitney U test, p = 0.0077) compared to controls. We also obtained significant differences in DMD, BMD and FSH (Median: 3.656 ng/ml (IQR: 1.944–5.443) (Mann-Whitney U test, p = 0.0052) compared to Pompe disease (DMD: Mann-Whitney U test, p = 0.0065; DMB: Mann-Whitney U test, p = 0.0001) (Fig. 5).
Serum levels PDGF-BB in muscle dystrophies: Pompe, Duchenne muscle dystrophy (DMD), Becker muscle dystrophy (BMD), dysferlinopathy (DYSF) and facioscapulohumeral muscular dystrophy (FSH). Variables are represented as median and interquartile range (IQR). Statistical significance of the results by Mann-Whitney test: *p ≤ 0.05, **p ≤ 0.01and ***p ≤ 0.001.
Correlation between PDGF-BB serum levels and results of muscle function tests and quantitative muscle MRI
We used the Spearman test to identify if there were any correlations between PDGF-BB serum concentration and the results of the muscle function tests, spirometry, patient-reported outcomes and qMRI. As it is shown in Table 3, we did not find any significant correlation. However, we found a non-significant tendency between PDGF-BB levels and 6MWT, the MRC score, the Myometry score, MIP, and thigh fat fraction measured using 3 point Dixon MRI.
Discussion
In the present study, we found significant differences in the serum concentration of four growth factors related to the process of skeletal muscle degeneration and regeneration in AOPD patients compared to controls. However, only serum levels of PDGF-BB were significantly different when symptomatic patients were compared with asymptomatic patients. In fact, the diagnostic accuracy of the PDGF-BB concentration to distinguish between symptomatic and asymptomatic patients was assessed by ROC curves, determining an optimal cut-off value of 1.97 ng/ml.
It is well known that chronic muscle damage leads to persistent inflammatory infiltration, muscle necrosis and activation of fibro/adipogenic progenitor (FAP) cells17, something that has been studied in dystrophic muscles. Eventually, muscle fibers are lost and substituted by fibro-adipose tissue18. Several growth factors have been related with this process, including those in the present study. TGF-β1 and PDGF-BB play an important role in satellite cell proliferation and fibrotic remodeling19,20,21. TGF-β1 is crucial in the initiation of fibrosis in skeletal muscle20,21,22, and PDGF-AA enhances the process of fibro-adipogenic expansion regulated by FAP cells23,24,25,26. CTGF influences the fibrotic process by inducing the expression and release of collagen type 1 by activated fibroblasts26,27,28. Although the process of muscle degeneration has been well established in animal models of muscular dystrophies such as Duchenne muscle disease, it is not yet completely known whether it happens in the same way as in Pompe disease. However, radiological studies show that skeletal muscle is gradually lost and substituted by fat tissue in patients with adult onset Pompe, mimicking what happens in patients with muscular dystrophies and suggesting a similar skeletal muscle degenerative process29,30,31. Based on this hypothesis, we decided to study the serum concentration of growth factors related with the process of muscle regeneration, degeneration and fibrosis.
PDGF-BB, which is secreted by inflammatory cells and skeletal muscle regenerative fibers, has recently been related with the process of muscle regeneration through the activation of satellite cell proliferation and chemotaxis32. We observed lower levels of serum PDGF-BB in AOPD patients compared to controls. Moreover, PDGF-BB serum concentration was even lower in symptomatic patients, suggesting a correlation with disease progression. As PDGF-BB probably influences muscle regeneration, the lower levels found in AOPD patients might reflect impaired regenerative response in Pompe disease, something that has also been suggested by other authors. Impaired satellite cell activation has been described in muscle samples from Pompe patients33,34,35. Moreover, serum levels of insulin growth-factor-1 and myostatin, two molecules related with the process of satellite cell activation, are lower in serum of Pompe patients compared to controls36.
We did not observe a significant difference in serum levels of TGF-β1, PDGF-AA and CTGF in symptomatic compared to asymptomatic Pompe patients. These three factors have been related with the process of muscles fibrosis, as discussed early. The lower levels of TGF-β1 found in Pompe patients compared to controls, supports the idea that fibrosis is not a major issue in patients with Pompe disease. In fact, Dr. Palermo37 and collaborators did not find an up-regulation of TGFB1 fibrosis-associated genes in skeletal muscle Pompe patients, which supports our findings.
The lower levels of growth factors related to fibrosis and regeneration suggested by the current study could be explained by the lack of sarcolemma damage in Pompe disease. In most muscular dystrophies in which the process of muscle degeneration and regeneration has been studied, muscle damage is produced because of the instability of skeletal muscle membrane. Membrane tears induce a series of responses, such as the release by muscle fibers of cytokines that recruit inflammatory cells and participate in the activation of satellite cells. Persistent inflammatory cells release profibrotic growth factors that lead to the expansion of fibrotic tissue. The process of muscle fiber degeneration in Pompe disease is probably different. There is no evidence of necrosis or inflammatory infiltration38. As opposed to muscle membrane instability, lysosomal rupture has been proposed as the main mechanism leading to muscle fiber necrosis. Glycogen progressively accumulates in lysosomes producing their rupture and the release of lytic enzymes to the sarcoplasm, probably activating the process of autophagy38,39. It is tempting to hypothesize that local cell response is different in Pompe disease, with no recruitment of inflammatory cells, no activation of satellite cells and no release of profibrotic factors. The fact that PDGF-BB levels were higher in serum samples from patients with other muscular dystrophies, and lower in Pompe disease, supports this hypothesis.
The identification of growth factors useful for the follow-up of patients is considered one of the unmet needs in Pompe disease. ERT is being administered to those symptomatic patients, patients with muscle or respiratory muscle weakness. However, patients may develop mild motor disturbances, such as abnormal gait posture, due to the presence of mild axial involvement. Growth factors capable of differentiating between symptomatic and asymptomatic patients could then be a useful tool in follow-up. As we observed significant lower PDGF-BB levels in symptomatic Pompe patients than asymptomatic, we suggest PDGF-BB could be useful to monitorize progression of the disease and help to identify those patients in which the process of muscle degeneration has started without influencing muscle function yet. Other growth factors previously proposed, such as urine glucose tetrasaccharide Glc4 levels40,41, have utility in the diagnosis of Pompe disease, or in monitoring of the treatment but not for differentiating between symptomatic and asymptomatic patients42,43.
To summarize, we have identified a group of four growth factors related to the process of muscle degeneration and regeneration that are differently expressed in Pompe patients compared to controls. Interestingly, PDGF-BB levels were significantly different in symptomatic patients compared to asymptomatic. In our opinion, our results suggest that decreasing levels of PDGF-BB in asymptomatic patients should prompt us to tighten the follow-up of the patient, repeating muscle and respiratory function tests in order to consider starting ERT before muscle degeneration becomes irreversible.
Methods
Patients and study design
This study is part of an ongoing prospective open-label study in which we are following up a group of symptomatic and non-symptomatic AOPD patients annually in our center using muscle function tests, muscle MRI and blood analysis. This study has been registered in Clinicaltrials.gov (identifier NCT01914536). The present research was performed in accordance with Spanish regulation for clinical trials and studies and following the recommendations described in the Declaration of Helsinki. The study was approved by The Ethical Committee of Hospital de la Santa Creu i Sant Pau (HSCSP) in Barcelona. All participants signed an appropriate informed consent form.
The diagnosis of Pompe disease was based on the presence of two mutations in the GAA gene. In cases where a single or no mutation was detected, diagnosis was based on reduced activity in at least two tissues, lymphocytes and skeletal muscle being the most common tissues studied, as has been recently suggested by the European Pompe Consortium10. All patients were considered adult onset since none of them developed symptoms before the age of 18.
We defined a patient as symptomatic when we identified muscle weakness in clinical examination using the Muscle Research Council score (MRC), or when Forced Vital Capacity (FVC), while seated, was lower than 85%. A total of 37 patients were included: 23 symptomatic patients treated with ERT, 6 symptomatic patients untreated with ERT and 8 asymptomatic patients. All treated patients received 20 mg/kg acid alpha-glucosidase intravenously every other week. Untreated symptomatic patients were seen before starting ERT. Clinical and genetic features of this group of patients have been previously published15. In summary, mean age at baseline visit of the 23 symptomatic patients was 49.8 years old. 9 of these patients used sticks or wheelchair for walking, with two of them being fully wheelchair bound. 12 patients used non-invasive ventilation at night. Mean age of the 6 non-treated symptomatic patients was 37.4 years old. Only one patient of this group used the stick for walking and one other patient required noninvasive ventilation at night. 8 presymtomatic AOPD patients were also included (mean age 21 years, 4 women). These patients were diagnosed of Pompe disease because they were relatives of patients with Pompe or because the presence of high CK levels in blood samples. As controls we included 45 patients whose age and sex matched our Pompe cohort (mean age 48 years, 29 women), and 10 more controls whose age and sex matched with asymptomatic Pompe patients (mean age 23 years, 6 women). The controls were volunteers, most of them relatives or caregivers of our Pompe patients that kindly agreed to participate in the study. CKs levels were normal in all control patients (Reference value for our laboratory is <174 U/L).
Growth factors identification
Blood samples were collected at baseline visit before motor function tests were performed. Blood was centrifuged for 1600 g for 9 minutes at 4 °C in order to separate the serum. The serum was aliquoted and stored at −80 °C until analysis.
Serum platelet-derived growth factor BB (PDGF-BB) and transforming growth factor β1 (TGF-β1) levels were measured using commercial enzyme-linked immunosorbent assay (ELISA) kits (R&D, Minneapolis, MN, USA), according to the manufacturer’s instructions. A platelet-derived growth factor AA (PDGF-AA) human ELISA kit was provided by ThermoFisher (Thermo Fisher Scientific, Nepean, Canada) and connective tissue growth factor (CTGF) by EIAAB Science Co (Wuhan, China). Minimum detectable cytokine concentrations for these assays were measured to be 1.7 pg/ml for TGF-β1, 15 pg/ml for PDGF-BB, 40 pg/ml for PDGF-AA and 0.18 ng/ml for CTGF. Samples were measured in duplicate and read on a microplate reader Beckman Coulter AD 340 (Beckam-Coulter, Brea, CA, USA) with AD-LD software.
Muscle function tests
All patients were evaluated by three physiotherapists (I.B., I.P. and E.M.), with experience in neuromuscular disorders, at HSCSP in Barcelona. Physiotherapists evaluated muscle function using the following tests: the 6MWT, time to walk 10 meters, timed up-and-go test, time to climb up and down 4 steps, and the 20 item motor function measure tool (MFM-20). Muscle strength was studied using both MRC and hand-held myometry. The MRC score was the sum of all individual MRC values, while the myometry score was the sum of all individual muscle values. ACTIVLIM, INQoL and SF-36 were used as patient-reported outcome measures. Forced vital capacity while seated and in a lying position, maximum inspiratory pressure (MIP) and maximum expiratory pressure (MEP) values were obtained with a Carefusion Microlab ML 3500 MK8 spirometer (Carefusion, Yorba Linda, CA, USA).
Muscle imaging
All patients were examined in a Philips Achieva XR 1.5 Teslas located at HSCSP. We used the same positioning protocol for all patients: supine position with legs stretched, the patella facing upward and the ankles in a neutral position.
3D 3-point Dixon images were acquired with the following acquisition parameters: TR/TE = 5.78/1.8, 4 ms, flip angle = 15°, FOV = 520 × 340 × 300 mm, voxel size = 1 × 1 × 3 mm.
Analysis of the 3-point Dixon MR images was performed using the PRIDE (Philips Research Image Development Environment) tool, as has been reported previously15,42. ROIs were manually drawn on five slices of the following muscles: rectus femoris, vastus intermedius, vastus lateralis, vastus medialis, adductor magnus, sartorius, gracilis, semitendinosus and semimembranosus, and on three slices of biceps femoris long head, biceps femoris short head and adductor longus
Data analysis
Non-parametric tests were used for the statistical analysis of the variables. The Mann-Whitney U test investigated whether there were significant differences in variables between groups (symptomatic vs asymptomatic and control vs Pompe). We used Spearman’s rank correlation (coefficient reported as ρ) to investigate any correlation between the serum concentration of growth factors and the results of the muscle function tests, spirometry, quality of life scales and the thigh fat fraction obtained using qMRI. As we ran multiple correlations, a Bonferroni test was performed to avoid type 1 errors. Finally, a ROC curve was performed to study whether PDGF-BB levels were able to differentiate between symptomatic and asymptomatic Pompe patients with high sensitivity and specificity. The results of all statistical studies were considered significant if P was lower than 0.05. Statistical studies were performed using IBM SPSS® Statistics software version 21. The datasets generated during the current study are available from the corresponding author on reasonable request.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
van der Ploeg, A. T. & Reuser, A. J. J. Pompe’s disease. Lancet (London, England) 372, 1342–53 (2008).
Fukuda, T., Roberts, A., Plotz, P. H. & Raben, N. Acid alpha-glucosidase deficiency (Pompe disease). Curr. Neurol. Neurosci. Rep. 7, 71–7 (2007).
Bembi, B. et al. Diagnosis of glycogenosis type II. Neurology 71, S4–11 (2008).
Yang, C.-F. et al. Very Early Treatment for Infantile-Onset Pompe Disease Contributes to Better Outcomes. J. Pediatr. 169, 174–180.e1 (2016).
Parini, R. et al. Long term clinical history of an Italian cohort of infantile onset Pompe disease treated with enzyme replacement therapy. Orphanet J. Rare Dis. 13, 32 (2018).
Hagemans, M. L. C. et al. Disease severity in children and adults with Pompe disease related to age and disease duration. Neurology 64, 2139–2141 (2005).
Schüller, A., Wenninger, S., Strigl-Pill, N. & Schoser, B. Toward deconstructing the phenotype of late-onset Pompe disease. Am. J. Med. Genet. Part C Semin. Med. Genet. 160C, 80–88 (2012).
McIntosh, P. T., Case, L. E., Chan, J. M., Austin, S. L. & Kishnani, P. Characterization of gait in late onset Pompe disease. Mol. Genet. Metab. 116, 152–6 (2015).
Valle, M. S. et al. Quantitative analysis of upright standing in adults with late-onset Pompe disease. Sci. Rep. 6, 37040 (2016).
van der Ploeg, A. T. et al. European consensus for starting and stopping enzyme replacement therapy in adult patients with Pompe disease: a 10-year experience. Eur. J. Neurol. 24, 768–e31 (2017).
Working Group, M. E. N. A. P. F. et al. Diagnosis and treatment of late-onset Pompe disease in the Middle East and North Africa region: consensus recommendations from an expert group. BMC Neurol. 15, 205 (2015).
Wallace, G. Q. & McNally, E. M. Mechanisms of Muscle Degeneration, Regeneration, and Repair in the Muscular Dystrophies. Annu. Rev. Physiol. 71, 37–57 (2009).
Morrow, J. M. et al. MRI biomarker assessment of neuromuscular disease progression: a prospective observational cohort study. Lancet Neurol. 15, 65–77 (2016).
Straub, V. et al. Stakeholder cooperation to overcome challenges in orphan medicine development: the example of Duchenne muscular dystrophy. Lancet. Neurol. 15, 882–890 (2016).
Figueroa-Bonaparte, S. et al. Muscle MRI Findings in Childhood/Adult Onset Pompe Disease Correlate with Muscle Function. PLoS One 11, e0163493 (2016).
Figueroa-Bonaparte, S. et al. Quantitative muscle MRI to follow up late onset Pompe patients: a prospective study. Sci. reports 8, 10898 (2018).
Smith, L. R. & Barton, E. R. Regulation of fibrosis in muscular dystrophy. Matrix Biol. 68–69, 602–615 (2018).
Joe, A. W. B. et al. Muscle injury activates resident fibro/adipogenic progenitors that facilitate myogenesis. Nat. Cell Biol. 12, 153–163 (2010).
Yablonka-Reuveni, Z., Balestreri, T. M. & Bowen-Pope, D. F. Regulation of proliferation and differentiation of myoblasts derived from adult mouse skeletal muscle by specific isoforms of PDGF. J. Cell Biol. 111, 1623–9 (1990).
Li, Y. et al. Transforming Growth Factor-β1 Induces the Differentiation of Myogenic Cells into Fibrotic Cells in Injured Skeletal Muscle. Am. J. Pathol. 164, 1007–1019 (2004).
Kamila, D., Paulina, K., A, C. M. & Malgorzata, Z. The role of TGF- β1 during skeletal muscle regeneration †. Cell Biol Int 41, 706–715 (2017).
Zanotti, S., Gibertini, S. & Mora, M. Altered production of extra-cellular matrix components by muscle-derived Duchenne muscular dystrophy fibroblasts before and after TGF-β1 treatment. Cell Tissue Res 339, 397–410 (2010).
Ieronimakis, N. et al. PDGFR signalling promotes fibrogenic responses in collagen-producing cells in Duchenne muscular dystrophy. J. Pathol. J Pathol 240, 410–424 (2016).
Burks, T. N. & Cohn, R. D. Role of TGF-β signaling in inherited and acquired myopathies. Skelet. Muscle 1, 19 (2011).
Olson, L. E. & Soriano, P. Increased PDGFRalpha activation disrupts connective tissue development and drives systemic fibrosis. Dev. Cell 16, 303–13 (2009).
Kendall, R. T. & Feghali-Bostwick, C. A. Fibroblasts in fibrosis: Novel roles and mediators. Front. Pharmacol. 27, 1–13 (2014).
Leask, A. CCN2: a novel, specific and valid target for anti-fibrotic drug intervention. Expert Opin. Ther. Targets 17, 1067–1071 (2013).
Morales, M. G. et al. CTGF/CCN-2 over-expression can directly induce features of skeletal muscle dystrophy. J. Pathol. 225, 490–501 (2011).
Carlier, R.-Y. et al. Whole-body muscle MRI in 20 patients suffering from late onset Pompe disease: Involvement patterns. Neuromuscul. Disord. 21, 791–799 (2011).
Carlier, P. G. et al. Skeletal muscle quantitative nuclear magnetic resonance imaging follow-up of adult Pompe patients. J. Inherit. Metab. Dis. 38, 565–572 (2015).
Alejaldre, A. et al. Trunk muscle involvement in late-onset Pompe disease: study of thirty patients. Neuromuscul. Disord. 22(Suppl 2), S148–54 (2012).
Piñol-Jurado, P. et al. Platelet-Derived Growth Factor BB Influences Muscle Regeneration in Duchenne Muscle Dystrophy. Am. J. Pathol. 187, 1814–1827 (2017).
Thurberg, B. L. et al. Characterization of pre- and post-treatment pathology after enzyme replacement therapy for Pompe disease. Lab. Investig. 86, 1208–1220 (2006).
Schaaf, G. J. et al. Lack of robust satellite cell activation and muscle regeneration during the progression of Pompe disease, https://doi.org/10.1186/s40478-015-0243-x.
Lagalice, L. et al. Satellite cells fail to contribute to muscle repair but are functional in Pompe disease (glycogenosis type II). Acta Neuropathol Commun. 6, 116 (2018).
Chien, Y.-H., Han, D.-S., Hwu, W.-L., Thurberg, B. L. & Yang, W.-S. Myostatin and Insulin-Like Growth Factor I: Potential Therapeutic Biomarkers for Pompe Disease. PLoS One 8, e71900 (2013).
Palermo, A. T. et al. Transcriptional response to GAA deficiency (Pompe disease) in infantile-onset patients. Mol. Genet. Metab. 106, 287–300 (2012).
Pascarella, A. et al. Vacuolated PAS-positive lymphocytes as an hallmark of Pompe disease and other myopathies related to impaired autophagy. J. Cell. Physiol. https://doi.org/10.1002/jcp.26365, (2017).
Raben, N. & Plotz, P. Role of autophagy in the pathogenesis of Pompe disease. Acta Myol. 26, 45–48 (2007).
Young, S. P. et al. Assessing disease severity in Pompe disease: The roles of a urinary glucose tetrasaccharide biomarker and imaging techniques. Am. J. Med. Genet. Part C Semin. Med. Genet. 160C, 50–58 (2012).
Manwaring, V. et al. Urine analysis of glucose tetrasaccharide by HPLC; a useful marker for the investigation of patients with Pompe and other glycogen storage diseases. J. Inherit. Metab. Dis. 35, 311–316 (2012).
An, Y. et al. Glucose tetrasaccharide as a biomarker for monitoring the therapeutic response to enzyme replacement therapy for Pompe disease. Mol. Genet. Metab. 85, 247–254 (2005).
Young, S. P. et al. Long-term monitoring of patients with infantile-onset Pompe disease on enzyme replacement therapy using a urinary glucose tetrasaccharide biomarker. Genet. Med. 11, 536–541 (2009).
Acknowledgements
We would like to thank the Spanish Association of Patients with Glycogenosis (www.glucogenosis.org) for their support to our investigation. We thank Neil McMillan for editorial support and Ignasi Gich for support with statistics. We thank the MRI whole technician team Esther Alemany, Nieves Campillos, Elisenda Mestres, Eugenia Torres, Ricard Cullell, Ingrid Rubio, Alberto Fernández and Mario González for their patience and support to the study. We also thank Mrs. Concepción Escolá for her assistance during the visits of the study. This investigation was sponsored by a grant from the Spanish Ministry of Health, Fondos FEDER-ISCIII PI15/01822 to Dr. Jordi Díaz-Manera and funds from Fundacion Isabel Gemio.
Author information
Authors and Affiliations
Author notes
A comprehensive list of consortium members appears at the end of the paper
Consortia
Contributions
E.F.S. performed the experimental part, analyzed the results, did the statistical analysis and prepared the figures and wrote the paper. A.C.R. and X.S.C. designed the protocol, analyzed the results and reviewed the paper. S.F.B. designed the protocol, visited the patients and analyzed muscle MRIs. S.S. coordinated the study, visited the patients and reviewed the paper. I.B., I.P. and E.M. designed the protocol, visited the patients and acquired motor function data. M.M. and J.L. designed the protocol and wrote the paper. C.N.P. and J.A.P. visited the patients and reviewed the paper. I.I. and E.G. designed and discussed the protocol. J.D.M. designed the protocol, visited the patients, analyzed the images, analyzed the results, did the statistical analysis, wrote the paper and obtained funding for the study.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fernández-Simón, E., Carrasco-Rozas, A., Gallardo, E. et al. PDGF-BB serum levels are decreased in adult onset Pompe patients. Sci Rep 9, 2139 (2019). https://doi.org/10.1038/s41598-018-38025-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-38025-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.