Abstract
Lower cervical dislocation with facet interlocking is one of the most drastic injuries to the cervical spine. The early reduction is thought critical in preventing progressive secondary spinal cord injury. The authors report a new surgical procedure in the management of lower cervical dislocation with facet interlocking. A total of twenty-one cases received immediate single-staged anterior open reduction, realignment and plate fixation under general anesthesia. After the procedures, most cases exhibited improved neurological function. All patients showed stable fusion at 1-year follow-up. Loss of spinal alignment or kyphotic deformity was not found in any case. Hardware failure including screw loosening or penetrating was not observed. In conclusion, the immediate anterior open reduction and plate fixation is a safe and effective procedure in the management of lower cervical dislocation with facet interlocking.
Similar content being viewed by others
Introduction
Cervical dislocation with facet interlocking is one of the most drastic injuries to the cervical spine. The clinical features including dislocation of the facet joints as well as neurological dysfunction are caused by primary and secondary injury1,2. The goals of treatment of any spinal injury include neurological recovery and spinal segment reconstruction. Although a few studies have reported the treatment procedures of this special clinical situation3,4,5, there are still controversies about the methods of reduction, the timing for surgery, and the modes of stabilization6,7. Currently, realignment by closed traction, followed by anterior, posterior or combined fixation/fusion has been the most common choice, and open reduction has been performed only after failed closed reduction4,8,9. While the use of axial traction to reduce dislocated joints and realign the fractured segment remains the mainstay of acute management, early operative treatment has gained increasing acceptance in recent years10,11,12. The current study aims to take the surgical procedure by immediate reduction as well as reconstruction of the cervical sequence and stability through an anterior surgical procedure.
Methods
Study design
This study is a single center case series which was conducted in Luohe Central Hospital, which was specialized in the management of spinal cord diseases. The study is conducted according to the guideline for case series13. Patients were enrolled from January 2006 to July 2016. The inclusion criteria were: (1) age >16; (2) lower cervical dislocation with facet interlocking confirmed by X-ray/MRI/CT. The exclusion criteria were: (1) neurological or cognitive impairment precluding reliable neurological evaluation; (2) penetration injury; (3) with vertebral/vertebral endplate fracture; (4) with serious osteoporosis; (5) presented in a life-threatening situation with an immediate surgical contraindication. During the research period all patients were assessed for suitability according to the inclusion and exclusion criteria. The study protocol was approved by the ethnic board of Luohe Central Hospital. We stated that informed consent was obtained from all participants and/or their legal guardians.
Management procedure
After admission to the hospital, neurological examination was carried out according to the Frankel classification. To illustrate the extent of the fracture and to determine the adequate surgical procedure, all the patients received both anteroposterior and lateral X-rays as well as a computed tomography (CT) and magnetic resonance imaging (MRI) according to standard protocol.
After the evaluation, the qualified patients will be chosen to take the appropriate surgical procedure to reduce the compression of the spinal cord and reconstruct the cervical sequence and stability.
We adopted an anterior surgical procedure. Under the general anesthesia with intubation, patients were placed at a supine position, with the fixation of forehead. A standard right-sided transverse incision was used. Vertebral levels were identified with intraoperative C-arm fluoroscopic visualization. Complete discectomies were accomplished at the involved level, and protruded disc fragments or small bone fragments compressing the medulla were carefully removed. For unilateral facet interlocking, the distractor screw holes were drilled in the locked side of the vertebral body at the medial margin of the musculus longus colli. For bilateral facet interlocking, the holes were drilled at the median line of the vertebral body. After this, the interspace was gradually widened to about 5–7 millimeter by carefully operating the Caspar distractor (Zhangjiakou Sanxing Medical Instruments Co., Ltd, Zhangjiakou). Thereafter, a periosteal elevator (Zhangjiakou Sanxing Medical Instruments Co., Ltd, Zhangjiakou) was inserted at the disc space to resolve facet locking by a slight distracting force. Finally, the articular gap was filled with allograft bone to facilitate fusion, and the stabilization was carried out with the use of zero-profile plate (Xiamen Dabo Medical Instruments Co., Ltd, Xiamen), which ensured the fusion between the adjacent vertebrae above and below the injured vertebral body.
After surgery, all the patients were treated and rehabilitated in a timely manner as usual. Neurological status was recorded at initial presentation, preoperatively, and at time of discharge from the hospital or transfer to a rehabilitation unit. Neurological function was recorded as Frankel grade. The Frankel Grade was recorded as Levels 1 to 5, corresponding to Grades A to E, respectively. All the medical treatments are in accordance with the Chinese Expert consensus on Evaluation, Treatment and Rehabilitation of Traumatic Spinal Cord Injury14.
Results
Participants
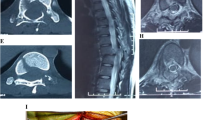
During the study period, 21 patients (14 males) fulfilled the inclusion criteria. Thirteen patients sustained their injuries in traffic accidents, 6 patients were injured in falls, and 2 patients were injured by falling objects. Dislocation occurred at C3/4 in 2 patients, C4/5 in 4 patients, C5/6 in 4 patients and C6/7 in 11 patients. In 7 patients the facet interlocking was unilateral; in 14 patients it was bilateral. Neurological symptoms were presented in all cases, although with different degrees of severity. The detailed characteristics of the included patients are listed in Table 1. Surgery procedure is illustrated in Fig. 1. And the surgery images of a protocol patient are presented in Fig. 2.
Schematic diagrams to illustrate the surgery procedure. (A) For unilateral facet interlocking, the distractor screw holes are drilled in the locked side of the vertebral body at the medial margin of the longus colli; the interspace is gradually widened to about 5–7 millimeter by carefully operating the Caspar distractor mechanism; and a periosteal elevator is inserted at the disc space to resolve facet interlocking by a slight distracting force. (B) For bilateral facet interlocking, the holes are drilled at the median line of the vertebral body; the interspace is gradually widened to about 5–7 millimeter by carefully operating the Caspar distractor mechanism; and a periosteal elevator is inserted at the disc space to resolve facet locking by a slight distracting force.
Protocol patient with C6/7 dislocation and right-side facet interlocking. (A) At presentation, sagittal position CT indicates C6/7 dislocation, and a small bone fragment presents at the posterior margin of the vertebral body of C6. (B) Horizontal position CT reveals a small bone fragment presents at the posterior margin of the vertebral body of C6. (C) Sagittal position MRI reveals C6/7 dislocation, disc herniation and compression of the spinal cord. (D) Stereoscopic reconstructed CT reveals C6/7 dislocation and facet interlocking at the right-side of C6. (E) Intraoperative C-arm fluoroscopic visualization. (F) Operative incision. (G) The anteroposterior and lateral view of cervical spine radiography after surgery. (H) Two weeks after the surgery, the MRI indicates the cervical sequence and stability was reconstructed, and the compression of the spinal cord was released completely. (I) Three months after the surgery, the reconstructed CT reveals complete postoperative realignment and fusion was achieved.
Outcomes and follow-up
Patients were operated on timely after admission to the hospital and no intraoperative complications were observed. Cerebrospinal fluid leakage occurred in 2 cases which subsided with conservative treatment. During the follow-up period, all 21 patients showed stable fusion at a minimum of 1-year follow-up, assessed by lateral radiographs as isodense bone bridging across the endplates. Loss of spinal alignment or kyphotic deformity was not found in any case. Hardware failure including screw loosening or penetrating was not observed. At the 1-year follow-up, none of the patients complained of relevant neck pain.
The neurological status on admission and by the end of follow-up is listed in Fig. 3. During the course of the follow-up, 15 patients (71.4%) exhibited improved neurological function, and deterioration of neurological function was not observed.
Discussion
Main results
The current study reported a new surgical procedure in the management of lower cervical dislocation with facet interlocking, which combined the mostly important two steps: the reliving the spinal compression and the reconstruction of the cervical sequence and stability. The results indicated that the neurological function was greatly improved in the majority patients while no deterioration of neurological function was observed. Besides, complete postoperative realignment and fusion was achieved in all patients and maintained throughout the follow-up period.
In relevance to other studies
Patients suffering cervical dislocation are at high risk of multiple systemic complications including infections of pulmonary or urinary tract, musculoskeletal contractions and deep vein thrombosis. Great efforts have made to improve the prognosis of the disease and to promote the rehabilitation of patients. Despite the great progressions have been made in recent years, the optimal medical and surgical treatment procedure still remains controversial.
One of the controversies centers on how to perform the reduction. It has been well documented that the nerve injury involves both primary and secondary injury mechanisms15. The primary injury, usually caused by rapid spinal cord compression and contusion, initiates a signaling cascade of down-stream events collectively known as secondary injury. Because damage in the primary phase cannot be prevented, all approaches focus on restricting damage in the secondary phase of the injury16, and reduction has been deemed as the most effective measure to prevent progressive secondary injury17. While closed reduction remains the mainstay of acute management18, the drawbacks of this method have been well documented19. Closed reduction was performed through cervical traction under local anesthesia, along with immobilization in a Halo thoracic brace. The force was increased gradually until the spinal canal has been restored to at least two-thirds its normal sagittal diameter, followed by an open surgery to reduce fracture-dislocation or to remove soft-tissue compression8. The closed reduction procedure may cost 1 hour or more, which precludes an immediate reduction. Furthermore, to ensure the safety of the reduction process, surgeons must confirm that there are no occupying lesions such as disc-material and bony fragments which can cause cord damage during the reduction; the reduction process should be monitored intensively; and a closed reduction should not be attempted on an obtunded patient in most circumstances. On the contrary, all the drawbacks mentioned above could be resolved by the immediate open reduction surgery.
Another controversy centers on which approach should be chosen20,21,22. The anterior approach is generally the best choice when reduction of the neural elements is required23,24, it has been reported to result in high fusion rates, good clinical outcomes and low rates of fixation failure22,25,26. The main deficit of the anterior approach is the mechanically instability, which has led to the clinical recommendation for additional posterior fixation or external immobilization27. While combined anterior and posterior fixation results in much better stability, patients may expose to increased risk of iatrogenic injury due to the longer operation time, the need to change the patient’s position, and the complexity of the operation. An anterior approach along with plate stabilization overcomes all the deficits by limiting surgical trauma, reducing operation time and no need to change body position during the procedure. Besides, immediate postoperative stability also allows for earlier mobilization and subsequent rehabilitation.
The safety of the surgical procedure was also documented in the current study. Serious complications including infection, reaction to foreign bodies and loosening screws were not experienced. The most feared complication, penetration of the dura and spinal cord damage by drilling or screw placement, was not encountered. There was no one case of worsening neurological function after the procedure. An ultimately stable fusion position was achieved in every case. Additionally, the Caspar distractor has made the procedure simpler and safer, by providing better visualization of the disc space, superior distraction and alignment. Nevertheless, fixation failure has been reported by previous studies with similar surgical procedure25,26. For example, Johnson et al. reported an overall radiographic failure rate of 13% in 87 patients with unilateral and bilateral facet fracture subluxations who were treated by anterior cervical discectomy, fusion, and plating. The failure is strongly correlated with fractures of the facets and fractures of the superior endplate of the lower vertebra. Anissipour et al. reported a treatment failure rate of 8% in 36 patients. According to their study, endplate fractures of the inferior level in jumped facets appears to be a major risk factor of fixation failure. However, in the series of the current study, according to the exclusion criteria, we had excluded those patients with facet or endplate fracture. This may explain the 100% fusion rate, no incidence of hardware failure or subsidence after surgery. Still, surgeons should be required to be specifically trained to perform this procedure safely.
Limitations
When interpreting the results of the current study, several limitations need to be acknowledged. First, while potential confounding factors was minimized by the small number of patients in a single center, it is difficult to extrapolate our results to other hospitals. Second, the current study is designed as an uncontrolled case series and lacks a contemporaneous internal control group. In the future, researchers should organize prospective multi-center trials to deliver valuable data regarding the optimal management procedure with convincing results.
Conclusions
The immediate anterior open reduction and plate fixation is a safe and effective procedure in the management of lower cervical dislocation with facet interlocking. The reduction is done immediately with the Caspar distractor under visual inspection, which allow complete removal of bone fragments and disc material extruded into the spinal canal from the fracture-dislocations. Facet interlocking is resolved by a slight distracting force with the use of a periosteal elevator. Stable fusion with the use of zero-profile plate was observed in all patients of the current study. Therefore, we prefer this technique over others in the management of lower cervical dislocation with facet interlocking. Future studies with a prospective design and larger sample size are needed to further validate the anterior-only surgical approach in the management of lower cervical dislocation and to explore the most appropriate surgical method for those with facet or endplate fracture.
References
Young, W. Secondary CNS injury. Journal of neurotrauma 5, 219–221 (1988).
Young, W. The post-injury responses in trauma and ischemia. Secondary injury or protective mechanisms? Central nervous system trauma: journal of the American Paralysis Association 4, 27–51 (1987).
Key, A. Cervical spine dislocations with unilateral facet interlocking. Paraplegia 13, 208–215 (1975).
Lu, K., Lee, T.-C. & Chen, H.-J. Closed Reduction of Bilateral Locked Facets of the Cervical Spine Under General Anaesthesia. Acta Neurochirurgica 140, 1055–1061 (1998).
Wolf, A. et al. Operative management of bilateral facet dislocation. Journal of neurosurgery 75, 883–890 (1991).
Lee, J. Y., Nassr, A., Eck, J. C. & Vaccaro, A. R. Controversies in the treatment of cervical spine dislocations. The spine journal: official journal of the North American Spine Society 9, 418–423 (2009).
Maiman, D. J., Larson, S. J. & Benzel, E. C. Neurological improvement associated with late decompression of the thoracolumbar spinal cord. Neurosurgery 14, 302–307 (1984).
Cotler, J. M. et al. Closed reduction of traumatic cervical spine dislocation using traction weights up to 140 pounds. Spine 18, 386–390 (1993).
Gelb, D. E. et al. Initial Closed Reduction of Cervical Spinal Fracture-Dislocation Injuries. Neurosurgery 72, 73–83 (2013).
Fehlings, M. G. et al. Early versus delayed decompression for traumatic cervical spinal cord injury. Results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS). PloS one 7, e32037 (2012).
Grassner, L. et al. Early Decompression (<8 h) after Traumatic Cervical Spinal Cord Injury Improves Functional Outcome as Assessed by Spinal Cord Independence Measure after One Year. Journal of neurotrauma 33, 1658–1666 (2016).
Aebi, M., Mohler, J., Zäch, G. A. & Morscher, E. Indication, surgical technique, and results of 100 surgically-treated fractures and fracture-dislocations of the cervical spine. Clinical Orthopaedics and Related Research, 244–257 (1986).
Kempen, J. H. Appropriate use and reporting of uncontrolled case series in the medical literature. American journal of ophthalmology 151, 7–10.e1 (2011).
Jianjun Li et al. Expert consensus on Evaluation, Treatment and Rehabilitation of Traumatic Spinal CordInjury [J]. Zhongguo Kangfu Lilun Yu Shijian 23, 274–287 (2017).
Fehlings, M. G., Sekhon, L. H. & Tator, C. The role and timing of decompression in acute spinal cord injury. What do we know? What should we do? Spine 26, S101–10 (2001).
Tator, C. H., Fehlings, M. G., Thorpe, K. & Taylor, W. Current use and timing of spinal surgery for management of acute spinal surgery for management of acute spinal cord injury in North America. Results of a retrospective multicenter study. Journal of neurosurgery 91, 12–18 (1999).
La Rosa, G., Conti, A., Cardali, S., Cacciola, F. & Tomasello, F. 10.1038@sj.sc.3101627 // Does early decompression improve neurological outcome of spinal cord injured patients? Appraisal of the literature using a meta-analytical approach. Spinal Cord 42, 503–512 (2004).
Papadopoulos, S. M. et al. Immediate spinal cord decompression for cervical spinal cord injury. Feasibility and outcome. The Journal of trauma 52, 323–332 (2002).
Fehlings, M. G. & Tator, C. H. An evidence-based review of decompressive surgery in acute spinal cord injury. Rationale, indications, and timing based on experimental and clinical studies. Journal of neurosurgery 91, 1–11 (1999).
Southwick, W. O. & Robinson, R. A. Surgical approaches to the vertebral bodies in the cervical and lumbar regions. The Journal of bone and joint surgery. American volume 39-A, 631–644 (1957).
Brodke, D. S., Anderson, P. A., Newell, D. W., Grady, M. S. & Chapman, J. R. Comparison of Anterior and Posterior Approaches in Cervical Spinal Cord Injuries. Journal of Spinal Disorders & Techniques 16, 229–235 (2003).
Song, K.-J. & Lee, K.-B. Anterior versus combined anterior and posterior fixation/fusion in the treatment of distraction-flexion injury in the lower cervical spine. Journal of clinical neuroscience: official journal of the Neurosurgical Society of Australasia 15, 36–42 (2008).
Aebi, M. Surgical treatment of upper, middle and lower cervical injuries and non-unions by anterior procedures 19, S33–9 (2010).
Caspar, W., Barbier, D. D. & Klara, P. M. Anterior cervical fusion and Caspar plate stabilization for cervical trauma. Neurosurgery 25, 491–502 (1989).
Anissipour, A. K. et al. Traumatic Cervical Unilateral and Bilateral Facet Dislocations Treated With Anterior Cervical Discectomy and Fusion Has a Low Failure Rate. Global spine journal 7, 110–115 (2017).
Johnson, M. G. et al. The radiographic failure of single segment anterior cervical plate fixation in traumatic cervical flexion distraction injuries. Spine 29, 2815–2820 (2004).
Kim, S.-M., Lim, T. J., Paterno, J., Park, J. & Kim, D. H. A biomechanical comparison of three surgical approaches in bilateral subaxial cervical facet dislocation. Journal of neurosurgery. Spine 1, 108–115 (2004).
Acknowledgements
This work was financed by grants from National Health and Family Planning Commission of the People’s Republic of China (W2014ZT096) and Henan Provincial Health and Family Planning Commission (201504092).
Author information
Authors and Affiliations
Contributions
All authors contributed to data collection and wrote the manuscript. Yuwei Li and Haijiao Wang drafted the study protocol. Peng Zhou and Cheng Li performed literature review. Wei Cui, Wei Xiao and Yan Wen collected data. Peng Zhou and Haoran Wang performed the analyses. Yuwei Li, Haoran Wang and Haijiao Wang drafted the paper. All authors critically reviewed the paper. Haoran Wang and Haijiao Wang had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Haoran Wang and Haijiao Wang are the guarantors of the paper. All authors approved the current manuscript to be published, attested that they contributed substantially to the current work, and disclosed that there was no writing assistance.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that the work described is original research that has not been published previously, and not under consideration for publication elsewhere, in whole or in part. The authors have no personal or institutional financial interest in drugs, materials, or devices described in the current work. The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper. The current study was approved by the ethnic board of Luohe Central Hospital. All research was performed in accordance with the Chinese Expert consensus on Evaluation, Treatment and Rehabilitation of Traumatic Spinal Cord Injury. We confirmed that informed consent was obtained from all participants and/or their legal guardians. We clarified that the drawings in Figures 1 and 2 were drawn by the authors Yuwei Li and Wei Cui.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, Y., Zhou, P., Cui, W. et al. Immediate anterior open reduction and plate fixation in the management of lower cervical dislocation with facet interlocking. Sci Rep 9, 1286 (2019). https://doi.org/10.1038/s41598-018-37742-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-37742-w
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.