Abstract
The multidrug resistant (MDR) opportunistic pathogen Klebsiella pneumoniae has previously been shown to adapt to chlorhexidine by increasing expression of the MFS efflux pump smvA. Here we show that loss of the regulator SmvR, through adaptation to chlorhexidine, results in increased resistance to a number of cationic biocides in K. pneumoniae and other members of the Enterobacteriaceae. Clinical Enterobacteriaceae isolates which lack smvA and smvR also have an increased susceptibility to chlorhexidine. When smvA from Salmonella and K. pneumoniae are expressed in Escherichia coli, which lacks a homologue to SmvAR, resistance to chlorhexidine increased (4-fold) but plasmid carriage of smvA alone was detrimental to the cell. Challenge of K. pneumoniae with chlorhexidine and another cationic biocide, octenidine, resulted in increased expression of smvA (approx. 70 fold). Adaptation to octenidine was achieved through mutating key residues in SmvA (A363V; Y391N) rather than abolishing the function of SmvR, as with chlorhexidine adaptation. Molecular modelling was able to predict that octenidine interacted more strongly with these mutated SmvA forms. These results show that SmvA is a major efflux pump for cationic biocides in several bacterial species and that increased efflux through SmvA can lead to increased chlorhexidine and octenidine tolerance.
Similar content being viewed by others
Introduction
With the rise in the number of infections caused by multi-drug resistant (MDR) pathogens, the pressure on antibiotic usage and infection prevention by other means has increased. This includes the use of biocides for disinfection of surfaces, medical devices and skin prior to operations. There is concern that the indiscriminate use of biocides is able to select for increased tolerance to particular biocides and also cross-resistance to antibiotics1,2,3,4. Indeed, overexpression of MDR efflux pumps such as acrAB-tolC in Escherichia coli5, mexCD-oprJ in Pseudomonas aeruginosa6 and smeDEF in Stenotrophomonas maltophilia7,8 has been linked to increased biocide tolerance.
The bisbiguanide chlorhexidine is widely used in clinical environments for many applications such as in mouth washes and wound dressings. Increased chlorhexidine susceptibility has been linked to deletion of a number of efflux pumps including aceI in Acinetobacter baumannii9 and cepA in Klebsiella pneumoniae10. Previously, we have shown that increased tolerance of chlorhexidine in K. pneumoniae is associated with increased expression of the efflux pump smvA through deletions in the adjacent divergently-transcribed gene termed smvR11.
SmvA was originally described as a chromosomally encoded major facilitator superfamily (MFS) efflux pump implicated in methyl-viologen efflux in Salmonella12,13. SmvR, like other TetR-like repressors is characterised by a HTH DNA binding domain14. The TetR family of regulators include AcrR, BetI and EnvR15,16, as well as those which have been implicated in biocide resistance, such as QacR from Staphylococcus aureus and AdeN from A. baumannii, which regulate the efflux pumps QacA and AdeIJK, respectively17,18. QacR has been shown to interact with cationic compounds such as dequalinium, chlorhexidine and ethidium19,20 by utilising four glutamate residues lining the drug-binding interface to bind to the cationic compounds21. QacR regulates the expression of qacA and also its own expression by binding to specific palindromic repeats in the promoter region15,16.
The aim of this study was to investigate the importance of SmvAR in tolerance to cationic biocides including chlorhexidine. To show this, we have examined whether K. pneumoniae strains, which have mutations in smvR, have decreased susceptibility to a range of cationic biocides, not just chlorhexidine. We also explored the importance of SmvAR in other Enterobacteriaceae (namely Citrobacter sp., Enterobacter sp. and Salmonella enterica serovar Typhimurium) in providing increased tolerance to chlorhexidine. We show that expression of smvAR in E. coli (an organism which appears to lack these genes) leads to decreased chlorhexidine susceptibility and that expression of smvA in K. pneumoniae is upregulated following chlorhexidine challenge. Computer modelling was employed to predict that chlorhexidine is able to bind to SmvA and identified specific residues that are theorised to be involved in the interaction of SmvA with chlorhexidine. Overall this demonstrated a clear role of SmvAR in mediating increased resistance to a range of cationic antiseptics.
Results
SmvA acts as a more general cationic biocide efflux pump in K. pneumoniae
We utilised transposon mutants in smvA and smvR derived from the K. pneumoniae strain MKP10322 to understand more about the function of SmvAR and its relationship with biocide resistance. These transposon mutants had a T30 transposon (a derivative of Tn5 carrying a chloramphenicol resistance gene) inserted into either smvR or smvA. There were three transposon mutants in smvR (clones KP05926 (∆smvR1), KP05927 (∆smvR2), KP05928 (∆smvR3)) and a single transposon mutant in smvA (KP05925 (∆smvA)). All transposon mutants were whole genome sequenced and details of the position of transposon insertion are provided (Supplementary Table 1). MIC/MBCs were determined against a range of biocides (Table 1). For several cationic biocides, including chlorhexidine, CPC, CTAB, and cetrimide, the absence of SmvR led to a decrease in susceptibility (≥2-fold) relative to MKP103. For ∆smvA there was a 2-fold increase in susceptibility for chlorhexidine, cetrimide, CTAB and HDPCM. Transposon disruption of either smvR or smvA appeared to have no impact on antibiotic resistance for all antibiotics tested (Supplementary Table 2). However, MKP103 contains several antibiotic resistance markers including aminoglycoside resistance genes (aadA2, aph(3′)-Ia, aac(6′)-Ib), fluoroquinolone resistance caused by mutations in GyrA (S83I) and ParC (S80I) as well as colistin resistance, which we hypothesise is caused by a previously undescribed mutation in PhoQ (Y265C). Therefore, it is plausible that any effects caused by loss of SmvA or SmvR function are masked by high level resistance mediated by pre-existing antibiotic resistance mechanisms.
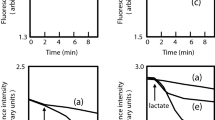
Due to there being a modest difference (2–4 fold) in the MIC values for chlorhexidine of the transposon mutants relative to MKP103, MIC experiments were repeated but the OD600 was recorded every hour to generate a growth profile. For chlorhexidine, as the concentration of biocide increased the differences in growth rate between the mutants and the wild-type (MKP103) became more significant. The smvR transposon mutants reached maximal OD600 values more rapidly in the presence of increased concentrations of chlorhexidine, whilst ∆smvA growth rate was retarded compared to MKP103 at the concentrations shown (Fig. 1).
Growth analysis of MKP103 ∆smvA and ∆smvR clones in the presence of chlorhexidine (CHD). Strains of K. pneumoniae were grown for 20 hrs (up to MIC measurement time) in different concentrations of chlorhexidine. The data presented are the means of four biological independent replicates. Significant differences in growth of MKP103 ∆smvA and MKP103 ∆smvR(1–3) relative to MKP103 are shown in the individual graph legends.
SmvA is upregulated in response to chlorhexidine
Although we have recently shown that smvA is upregulated in mutants which have a non-functional SmvR11, we wanted to ascertain whether smvA transcript levels are altered in direct response to chlorhexidine. Therefore, K. pneumoniae strain MGH 78578, which contains full length smvA and smvR genes, was challenged with sub-MIC (8 mg/L) and lethal (128 mg/L) concentrations of chlorhexidine. The same strain was also challenged with sub-MIC (1 mg/L) and lethal (16 mg/L) concentrations of another cationic biocide, octenidine. This was because octenidine is increasingly used as a substitute for chlorhexidine and, unlike chlorhexidine, MIC/MBC values for octenidine for the smvA/smvR transposon mutants showed no change relative to MKP103. At the sub-MIC level for chlorhexidine, there was a significant upregulation of smvA (70-fold) and smvR (14-fold). At the lethal level there was upregulation of smvA (15-fold) and smvR (3.5 fold). Perhaps surprisingly, given the lack of change in MICs following disruption to either smvR or smvA, after exposure to octenidine, there were similar levels of upregulation for both smvA and smvR as seen after challenge with chlorhexidine at both the sub-MIC and lethal concentrations (Supplementary Fig. S1).
Expression of smvA in E. coli increases tolerance to chlorhexidine
Blast searches revealed that E. coli contained no homologue for SmvAR and the majority of E. coli isolates tested had an MIC value of 0.5–1 mg/L to chlorhexidine (Supplementary Table 3), which is lower than Klebsiella (typically 16–32 mg/L) or other SmvAR containing members of the Enterobacteriaceae family tested. To test whether expression of smvAR from other Enterobacteriaceae would increase the resistance to chlorhexidine in E. coli, smvA and the smvAR region from K. pneumoniae MGH 78578 and Salmonella enterica serovar Typhimurium SL1344 were cloned into TOPO Vector pCR 2.1 and transformed into E. coli TOP10 (K-12) cells. Sequence analysis of several clones indicated that there were often mutations in the smvA sequence despite the original PCR product not showing any such mutations. Two clones, each containing either Salmonella smvA or smvAR or Klebsiella smvA or smvAR, were selected for further MIC testing, including, where possible, clones with no SNPs in smvA or smvR. All clones tested showed increased (4–8 fold) MIC values (2–4 mg/L) for chlorhexidine relative to plasmid only control (0.5 mg/L), but not for other cationic disinfectants tested (Fig. 2A). E. coli expressing Salmonella smvAR consistently gave 2-fold higher MIC values for chlorhexidine relative to clones expressing smvA alone. The growth of strains expressing K. pneumoniae, but especially for S. enterica smvA only, was also significantly reduced relative to SmvAR containing strains (Fig. 2B), potentially indicating that the expression of smvA without its regulator was more toxic to E. coli.
Introduction of smvA into E. coli leads to increased resistance to chlorhexidine. MIC values to cationic biocides (A) and growth profiles (B) for E. coli expressing plasmids containing smvA or smvAR from S. enterica or K. pneumoniae. For E. coli clones KP indicates the fragment was cloned from K. pneumoniae and ST from S. enterica serovar Typhimurium. smvAR indicates that the fragment contains full length smvA and smvR including their promoters and smvA indicates that the fragment contains a full length smvA including its promoter. C2 indicates clone number 2 etc. Coding mutations found in various fragments are indicated. Control indicates plasmid only. Growth curves are the means of three independent repeats and statistical significance between clones and the control is shown where appropriate. All MIC values are given as mg/L except CET (%). For abbreviations see Table 1.
SmvR mutations are observed in other members of the Enterobacteriaceae upon chlorhexidine exposure and these also impact on cationic biocide resistance
Whilst mutations were observed in K. pneumoniae smvR following adaptation to chlorhexidine, we wanted to understand whether similar mutations were found in other members of the Enterobacteriaceae upon exposure to chlorhexidine. Therefore, strains of Klebsiella oxytoca, Citrobacter freundii, Enterobacter sp. and S. enterica, were exposed to increasing concentrations of chlorhexidine. Several K. pneumoniae strains were also adapted alongside as a control. Results showed that the Klebsiella species were most able to adapt, with 5/7 and 4/7 strains surviving in concentrations of 128 mg/L CHD for K. pneumoniae and K. oxytoca respectively. Mutations observed following chlorhexidine adaptation are described in Table 2. This shows the presence of additional K. pneumoniae mutations in smvR, along with several mutations in the smvAR promoter region, which had not been described in our previous study11. There were no mutations in PhoPQ identified as found previously11 but several strains had deletions in mgrB, the phoP regulator gene. Mutations in mgrB were also found in K. oxytoca but no other strains showed genetic changes in the phoPQ controlled system. SmvR mutations were also found in Salmonella, C. freundii and K. oxytoca strains but not Enterobacter spp. Other mutations of interest include genetic changes in another TetR-family transcriptional regulator ramR, members from the BamABCDE complex involved in OM biogenesis e.g. bamE from Salmonella, and the MltA-interacting protein mipA. Mutations in mipA and bamD have been previously observed in K. pneumoniae11. For mutations in smvR, all mutations in non-Klebsiella species were found in the C-terminal ligand binding region; in Klebsiella mutations were either in the promoter or in the N-terminal DNA binding region. However, we have previously observed mutations throughout the gene (Fig. 3A)11. Therefore, adaptation to chlorhexidine thorough mutations in smvR is not exclusive to K. pneumoniae, but is observed in diverse members of the Enterobacteriaceae. For those adapted strains from the other members of the Enterobacteriaceae with mutations in SmvR, there was an increase in tolerance to chlorhexidine and several other cationic biocides. This suggests that SmvA has a similar role in mediating tolerance to cationic biocides in several members of the Enterobacteriaceae.
Sequence analysis for the smvA and smvR promoter region (A) and protein sequence for SmvR (B) between select members of the Enterobacteriaceae. Consensus sequences from K. pneumoniae (KP), K. oxytoca (KO), C. freundii (CF), E. cloacae complex (EC) and S. Typhimurium (ST) were aligned. Potential DYAD repeats in K. pneumoniae (P1 to P3) are indicated and mutations after CHD adaptation in K. pneumoniae are indicated in the gene and the promoter (bold italic). The −10 and −35 promoter regions are also indicated (underlined). (B) Highly conserved regions in the Enterobacteriaceae in the SmvR protein are indicated in boxes. One of the mutations (H46D) occurs in the N-terminal conserved region within the predicted DNA binding region. *indicates natural sequence variation in K. pneumoniae.
Investigation of Klebsiella, Salmonella, Citrobacter and Enterobacter clinical strains from our collection, which had been whole genome sequenced, showed that a few strains lacked smvAR or had disrupted smvA genes. These strains showed reduced susceptibility to chlorhexidine and other cationic biocides (cetrimide, CPC, CTAB and HDPCM) (Table 3).
Further sequence analysis of the shared promoter region for smvAR revealed the presence of three palindromic DYAD motifs which are typical for Tet-repressors and have been described for QacR15. In particular one palindromic motif (P3) was highly conserved between all species analysed (Fig. 3A). Indeed, SNPs in the smvAR promoter region, of Klebsiella strains after adaptation to chlorhexidine, affected the symmetry of palindromic sequence P3, which indicated that this is a likely SmvR binding site. Alignment of the 138 bp intergenic region for smvA and smvR for all K. pneumoniae strains in our database (approx. 90) showed that the sequence is highly conserved with most changes being sequence-type associated, although several strains have an affected palindromic motif (P1) (Supplementary Fig. S2). These strains do not appear to have a noticeable change in chlorhexidine MIC, possibly indicating that P1 is not important for SmvR binding. There are sigma70 −35 and −10 regions predicted for smvR but not for smvA which may indicate that under normal conditions smvA expression may be downregulated. Analysis of the SmvR sequence from several members of the Enterobacteriaceae showed areas of conserved homology, in particular two areas highlighted in Fig. 3B and Supplementary Fig. S3, one in the predicted DNA binding N-terminal domain and one in the C-terminal substrate recognition domain which may indicate that similar substrates are recognised by the SmvR proteins from various different species.
Chlorhexidine is able to bind to SmvA through specific residues
To understand potential interactions between SmvA and chlorhexidine, homology modelling and molecular docking studies were employed. These were able to show that theoretically chlorhexidine is able to interact with the central channel of SmvA (Fig. 4). A 100 ns molecular dynamics (MD) simulation provided information about the interaction of chlorhexidine with the binding pocket in SmvA. The complex remained stable during the course of the simulation largely due to the formation of hydrogen bonds and hydrophobic interactions with different residues. Hydrogen bond analysis showed that there are two permanent hydrogen bonds for SmvA-Chlorhexidine centred at residue Q392.
SmvA mutations occur in response to octenidine adaptation
Given the result that smvA was upregulated following exposure to octenidine, we sought to understand whether SmvA is also involved in the adaptive mechanism(s) associated with increased octenidine resistance. Strains of K. pneumoniae were adapted to octenidine in a similar manner to chlorhexidine. Several strains were able to survive in concentrations of 32–64 mg/L octenidine. When these were tested for increased MIC/MBC to octenidine there was only a two-fold increase for adapted strains compared to the parental strains (Table 4). There was also no noticeable cross-resistance to chlorhexidine or other cationic biocides. However, in general, these mutants again showed a significantly reduced doubling time, compared to their parental strains, in the presence of sub MIC-levels of either octenidine or chlorhexidine (Fig. 5), indicative of greater fitness under these conditions.
Analysis of the whole genome sequences for these adapted strains showed that they all contained a SNP in smvA with the majority (4/6 strains) containing a mutation which changed amino acid 363. The other mutations which were found were L364Q and Y391N in one strain each. All these mutations likely affect the binding and positioning of the L364 and E392 residues, which were flagged as important for hydrogen bond formation in chlorhexidine binding (Fig. 4). Molecular docking of octenidine with the wild type SmvA and the A363V and Y319N mutants showed good binding energy −50.62, −49.43 and −47.77 kcal/mol respectively. However, the mutant A363V showed slightly better energy of binding (−49.43 kcal/mol) compared to Y319N mutant (−47.77 kcal/mol), and the A363V mutant complex also displayed better ChemScore value (48) compared to both wild type (45) and Y391N mutant (43). A 100 ns MD simulation was carried out to investigate the molecular level interactions within the dynamic system, and the post-MD simulation analysis showed superior relative binding free energy values for both mutant A363V (−58.65 kcal/mol) and Y319N (−57.84 kcal/mol) complexes compared to the wild type (−45.31 kcal/mol) complex (Table 5). The 2D interaction analysis of the complexes after the MD simulation highlighted notably stronger interactions, both electrostatic and hydrophobic, with the mutant A363V structure compared to the wild type structure (Fig. 6) and Y319N mutant (Supplementary Fig. S4), which supports the energy values obtained for the complexes. The energy values and interaction analysis suggest both wild type and mutant SmvA have a sufficient specificity and selectivity to octenidine that can form stable complexes with good energy of binding, which consequently could lead to transport of octenidine across the channel.
Discussion
This study has shown that SmvA is an important efflux pump for chlorhexidine and other cationic biocides in K. pneumoniae and other members of the Enterobacteriaceae tested. This is also the first study to describe a potential resistance mechanism for K. pneumoniae to octenidine and suggests that adaptation to chlorhexidine and octenidine occurs through a common mechanism (SmvAR). With increasing use of antiseptics, particularly to help combat the spread of MDR infections, there has been a lack of surveillance to look for the prevalence of potential antiseptic resistance mechanisms23. We and others have shown that bacterial strains of K. pneumoniae and S. aureus isolated in the last few years have higher MIC values to chlorhexidine and octenidine than strains isolated before the widespread use of these antiseptics24,25. Therefore, it is possible that bacteria are becoming more tolerant to these antiseptics by mechanisms highlighted in this study.
The addition of smvAR from Salmonella and Klebsiella into E. coli increased tolerance to chlorhexidine; but when the regulator was not present, smvA was likely to be highly expressed and caused a growth defect in the cell. Mutations were often observed in smvA or its promoter, which are likely minimising the damaging effect of overexpressed smvA on cell growth. Overexpression of another native MFS pump in E. coli (mdtM) has also been shown to be energetically costly26. Klebsiella strains were able to tolerate high levels of smvA expression (above 50-fold) in sub-MIC levels of chlorhexidine and those strains which had mutations in SmvR following chlorhexidine adaptation, generally had a constitutive 10–25 fold increase in smvA expression11. However, qPCR analysis in this study was performed after exposure to chlorhexidine for 20 mins and therefore the long-term effect of highly increased expression of smvA is unknown. Several adapted strains from a previous study were found to have additional mutations, such as those observed in PhoPQ, which may help to stabilise the membrane and compensate for the increased levels of SmvA11. PhoPQ mutations were found to contribute towards colistin resistance, but on their own did not increase resistance to chlorhexidine11,27.
Mutations in palindromic repeats present in the promoter of smvA identified after chlorhexidine adaptation presumably affect the binding of SmvR to the smvA promoter, leading to overexpression of smvA. The E. coli efflux pump, MdfA, which is thought to efflux specific divalent cationic compounds like chlorhexidine, is naturally present in a closed state and undergoes a conformation change upon binding of specific compounds28,29. Therefore, SmvA could also exist in two states, which depend on the presence of cationic compounds. Efflux systems may be recruited in response to environmental and external stress30 and the inactivation of the “stress response” in P. aeruginosa led to increased susceptibility to several antimicrobials31, highlighting its importance in antimicrobial resistance. We have yet to understand the main function of SmvA in K. pneumoniae and whether it is specific for cationic compounds or part of a less-specific stress response. We also do not understand whether SmvR is able to respond to a variety of external stimuli and regulate multiple genes rather than just smvA. Several K. pneumoniae strains from the Murray collection, which were isolated before the widespread use of many cationic biocides, contain smvA genes with no sequence deviation from modern day clinical isolates24, suggesting that this MFS pump has other naturally-occurring substrates. In Klebsiella, it is possible that multiple pumps are involved in the efflux of chlorhexidine. The finding of mutations in ramR, the indirect regulator of acrAB, in multiple strains after adaptation to chlorhexidine suggests a role for acrAB in chlorhexidine efflux. Other studies have indicated that specific pumps cepA and kpnGH are important in chlorhexidine efflux10,32. However, we have never observed mutations in either of these pumps following chlorhexidine adaptation and all strains of Enterobacteriaceae which lacked smvAR and were highly susceptible to chlorhexidine appeared to contain full length cepA and kpnGH equivalent genes.
Although we have yet to find clinical isolates of Klebsiella sp. with mutations in SmvR, we have recently identified a naturally occurring smvR deletion in Proteus mirabilis with elevated MICs for chlorhexidine (Pelling et al., manuscript in preparation). It is, however, clear that clinical isolates lacking smvAR are more susceptible to the action of cationic biocides. A homologue of smvA and its regulator has been found on a genomic island SmarGI1-1, containing the carbapenemase sme-2 in Serratia marcescens33, which can be transferred between Serratia strains34. This raises the possibility of transfer of SmvAR to other species, which may contribute to more widespread and increased chlorhexidine tolerance in clinical pathogens. Transfer of smvAR to different species and/or smvR deletion in clinical strains is therefore, likely to have a significant impact on bacterial resistance to multiple cationic biocides.
This study has highlighted the importance of the efflux pump SmvA in generating increased resistance to chlorhexidine, octenidine and other cationic biocides in Klebsiella and other Enterobacteriaceae. Increased smvA expression, whether as a response to chlorhexidine or octenidine exposure, or due to possible plasmid transfer, may cause a concern for the effectiveness of infection prevention procedures in the clinic. Monitoring smvAR mutations in clinical strains would provide an early warning of potential reductions in susceptibility to critical antiseptics, either directly by SmvA overproduction or in association with other resistance mechanisms.
Materials and Methods
Growth of bacterial strains and adaptation to biocides
All strains were grown in tryptic soy broth (TSB) with aeration or on tryptic soy agar at 37 °C unless otherwise stated. Transposon mutants from K. pneumoniae MKP103 have been described previously22. All transposon mutants were whole genome sequenced prior to use. Adaptation to biocides was carried out as described previously35 except that the starting concentrations were 4 mg/L chlorhexidine up to a final concentration of 128 mg/L. For octenidine the starting concentration was 1 mg/L up to 64 mg/L.
Determination of MIC/MBC
Broth-Microdilution MIC analysis was performed as described previously36. All MIC’s were performed in TSB media using polystyrene 96 well plates (Corning, Flintshire, UK) except for the polymyxins, where polypropylene plates (Griener Bio-One Ltd, Stonehouse, UK) were utilised. Bacterial growth in the presence of biocides was measured by taking an OD600 reading every hour for 20 hours using a FLUOstar Omega plate reader (BMG Labtech GMBH, Ortenberg, Germany). For MBC testing, 10 µl of suspension was removed from each well of the MIC microtiter plate where no bacterial growth was observed, along with the two wells immediately below the MIC where growth was observed. These were spotted on TSA plates and incubated at 37 °C for 24 h. The MBC was defined as the lowest concentration of antibiotic/disinfectant at which no bacterial growth was observed in three replicate experiments.
Whole genome sequencing and Real Time-PCR
This was carried out as previously described11 and PHE Galaxy was used to analyse genetic changes37. Quantitative Real Time PCR was carried out and analysed as previously described using primers already described11. Exposure to chlorhexidine or octenidine was for 30 mins.
Cloning smvA(R) fragments into E. coli
K. pneumoniae and S. enterica serovar Typhimurium smvA and smvAR fragments were amplified from strains MGH 78578 and SL1344 respectively using primers described in Supplementary Table 4. Fragments were subsequently cloned into pCR 2.1 TOPO vector (Invitrogen) according to manufacturer’s instructions. Plasmids were then transformed into E. coli TOP10 cells and positive colonies selected for on TSA plates containing kanamycin (30 mg/L). Plasmid transformation was confirmed by PCR using standard M13 forward and reverse primers. A selection of plasmids were purified and the smvA(R) fragment sequence confirmed by Sanger sequencing.
Homology modelling and generation of the SmvA Structures
The interaction of the wild-type SmvA efflux pump and its A363V and Y391N mutant forms in complex with different ligands was explored using computational methods including molecular docking, molecular dynamics (MD) simulation, molecular mechanics, Poisson-Boltzmann surface area/molecular mechanics and generalised Born surface area (MM-PBSA/MM-GBSA) calculation. Homology modelling was utilised for the generation of the structural model of the transporter in PDB format. The I-TASSER webserver38,39,40 was used for the homology modelling of SmvA structural model from K. pneumoniae, using the FASTA formatted target sequence with UniProt entry number of A6T9N7. C-score is a confidence score for estimating the quality of predicted models by I-TASSER, and a C-score of −1.08 was obtained for this model which is well within the acceptable range [−5, 2]. The generated model was without any gap, and all the segments were solved. Accelrys Discovery Studio 2017 was used to add probable missing side chains in the generated model. The mutant forms of SmvA were generated as A363V and Y391N individually, by the PyMOL program. The structures were minimised by the AMBER package program41,42 before carrying out the molecular docking and running MD simulations. Additional computational modelling methods are listed in supplementary methods.
Statistical analysis
All bacterial growth curves were analysed by calculating the time taken to reach half the maximal OD and then comparing these values with relevant controls using a Students Unpaired T-test. Real Time PCR data was analysed for significance using the Students Unpaired T-test. For significance P values < 0.0001 ****; 0.001–0.0001 ***; 0.01–0.001 **; 0.05–0.01 *; ≥0.05 non-significant were used.
References
Schwaiger, K. et al. Insusceptibility to disinfectants in bacteria from animals, food and humans—is there a link to antimicrobial resistance? Front Microbiol 5, 88, https://doi.org/10.3389/fmicb.2014.00088. (2014).
Russell, A. D., Tattawasart, U., Maillard, J. Y. & Furr, J. R. Possible link between bacterial resistance and use of antibiotics and biocides. Antimicrob Agents Chemother 4, 2151 (1998).
Walsh, S. E. et al. Development of bacterial resistance to several biocides and effects on antibiotic susceptibility. J Hosp Infect 55, 98–107 (2003).
Randall, L. P. et al. Commonly used farm disinfectants can select for mutant Salmonella enterica serovar Typhimurium with decreased susceptibility to biocides and antibiotics without compromising virulence. J Antimicrob Chemother 60, 1273–1280 (2007).
McMurry, L. M., Oethinger, M. & Levy, S. B. Overexpression of marA, soxS, or acrAB produces resistance to triclosan in laboratory and clinical strains of Escherichia coli. FEMS Microbiol Lett 166, 305–309 (1998).
Chuanchuen, R. et al. Cross-resistance between triclosan and antibiotics in Pseudomonas aeruginosa is mediated by multidrug efflux pumps: Exposure of a susceptible mutant strain to triclosan selects nfxB mutants overexpressing MexCD-OprJ. Antimicrob Agents Chemother 45, 428–432 (2001).
Sanchez, P., Moreno, E. & Martinez, J. L. The biocide triclosan selects Stenotrophomonas maltophilia mutants that overproduce the SmeDEF multidrug efflux pump. Antimicrob Agents Chemother 49, 781–782 (2005).
Hernandez, A., Ruiz, F. M., Romero, A. & Martinez, J. L. The binding of triclosan to SmeT, the repressor of the multidrug efflux pump SmeDEF, induces antibiotic resistance in Stenotrophomonas maltophilia. PLoS Pathog 7 (2011).
Hassan, K. A. et al. Transcriptomic and biochemical analyses identify a family of chlorhexidine efflux proteins. Proc Natl Acad Sci USA 110, 20254–20259 (2013).
Fang, C. T., Chen, H. C., Chuang, Y. P., Chang, S. C. & Wang, J. T. Cloning of a cation efflux pump gene associated with chlorhexidine resistance in Klebsiella pneumoniae. Antimicrob Agents Chemother 46, 2024–2028 (2002).
Wand, M. E., Bock, L. J., Bonney, L. C. & Sutton, J. M. Mechanisms of increased resistance to chlorhexidine and cross-resistance to colistin following exposure of Klebsiella pneumoniae clinical isolates to chlorhexidine. Antimicrob Agents Chemother 61, e01162–16, https://doi.org/10.1128/AAC.01162-16 (2017).
Villagra, N. et al. SmvA, and not AcrB, is the major efflux pump for acriflavine and related compounds in Salmonella enterica serovar Typhimurium. J Antimicrob Chemother 62, 1273–1276 (2008).
Santiviago, C. A. et al. The Salmonella enterica sv. Typhimurium smvA, yddG and ompD (porin) genes are required for the efficient efflux of methyl viologen. Mol Microbiol 46, 687–698 (2002).
Kisker, C., Hinrichs, W., Tovar, K., Hillen, W. & Saenger, W. The complex formed between Tet repressor and tetracycline-Mg2+ reveals mechanism of antibiotic resistance. J Mol Biol 247, 260–280 (1995).
Ramos, J. L. et al. The TetR family of transcriptional repressors. Microbiol Mol Biol Rev 69, 326–356 (2005).
Cuthbertson, L. & Nodwell, J. R. The TetR family of regulators. Microbiol Mol Biol Rev 77, 440–475 (2013).
Grkovic, S., Brown, M. H., Roberts, N. J., Paulsen, I. T. & Skurray, R. A. QacR is a repressor protein that regulates expression of the Staphylococcus aureus multidrug efflux pump QacA. J Biol Chem 273, 18665–18673 (1998).
Fernando, D. M., Xu, W., Loewen, P. C., Zhanel, G. G. & Kumar, A. Triclosan can select for an AdeIJK-overexpressing mutant of Acinetobacter baumannii ATCC 17978 that displays reduced susceptibility to multiple antibiotics. Antimicrob Agents Chemother 58, 6424–6431 (2014).
Mitchell, B. A., Brown, M. H. & Skurray, R. A. QacA, multidrug efflux pump from Staphylococcus aureus: comparative analysis of resistance to diamidines, biguanidines, and guanylhydrazones. Antimicrob Agents Chemother 42, 475–477 (1998).
Schmacher, M. A. et al. Structural mechanisms of QacR induction and multidrug recognition. Science 294, 2158–2163 (2001).
Schmacher, M. A. & Brennan, R. G. Structural mechanisms of multidrug recognition and regulation by bacterial multidrug transcription factors. Mol Micro 45, 885–893 (2002).
Ramage, B. et al. Comprehensive arrayed transposon mutant library of Klebsiella pneumoniae outbreak strain KPNIH1. J Bacteriol, https://doi.org/10.1128/JB.00352-17 (2017).
Harbarth, S., Tuan Soh, S., Horner, C. & Wilcox, M. H. Is reduced susceptibility to disinfectants and antiseptics a risk in healthcare settings? A point/counterpoint review. J Hosp Infect 87, 194–202 (2014).
Wand, M. E. et al. Characterization of pre-antibiotic era Klebsiella pneumoniae isolates with respect to antibiotic/disinfectant susceptibility and virulence in Galleria mellonella. Antimicrob Agents Chemother 59, 3966–72 (2015).
Hardy, K. et al. Increased Usage of antiseptics is associated with reduced susceptibility in clinical isolates of Staphylococcus aureus. MBio 9, pii: e00894–18, https://doi.org/10.1128/mBio.00894-18 (2018).
Holdsworth, S. R. & Law, C. J. Multidrug resistance protein MdtM adds to the repertoire of antiporters involved in alkaline pH homeostasis in Escherichia coli. BMC Microbiol 13, 113, https://doi.org/10.1186/1471-2180-13-113 (2013).
Wand, M. E., Bock, L. J. & Sutton, J. M. Retention of virulence following colistin adaptation in Klebsiella pneumoniae is strain-dependent rather than associated with specific mutations. J Med Microbiol 66, 959–964 (2017).
Zomot, E. et al. A new critical conformational determinant of multidrug efflux by an MFS transporter. J Mol Biol 430, 1368–1385 (2018).
Fluman, N., Adler, J., Rotenberg, S. A., Brown, M. H. & Bibi, E. Export of a single drug molecule in two transport cycles by a multidrug efflux pump. Nat Commun 5, 4615, https://doi.org/10.1038/ncomms5615 (2014).
Poole, K. Stress responses as determinants of antimicrobial resistance in Pseudomonas aeruginosa: multidrug efflux and more. Can J Microbiol 60, 783–91 (2014).
Nguyen, D. et al. Active starvation responses mediate antibiotic tolerance in biofilms and nutrient-limited bacteria. Science 334, 982–986 (2011).
Srinivasan, V. B., Singh, B. B., Privadarshi, N., Chauhan, N. K. & Rajamohan, G. Role of novel multidrug efflux pump involved in drug resistance in Klebsiella pneumoniae. PLoS One 13, e96288 (2014).
Mataseje, L. F. et al. Serratia marcescens harbouring SME-type class A carbapenemases in Canada and the presence of bla SME on a novel genomic island SmarGI1-1. J Antimicrob Chemother 69, 1825–1829 (2014).
Hopkins, K. L. et al. Serratia marcescens producing SME carbapenemases: an emerging resistance problem in the UK? J Antimicrob Chemother 72, 1535–1537 (2017).
Bock, L. J., Wand, M. E. & Sutton, J. M. Varying activity of chlorhexidine-based disinfectants against Klebsiella pneumoniae clinical isolates and adapted strains. J Hosp Infect 93, 42–48, https://doi.org/10.1016/j.jhin.2015.12.019 (2016).
Bock, L. J., Hind, C. K., Sutton, J. M. & Wand, M. E. Growth media and assay plate material can impact on the effectiveness of cationic biocides and antibiotics against different bacterial species. Lett Appl Microbiol 66, 368–377 (2018).
Batut, B. et al. The Galaxy platform for accessible, reproducible and collaborative biomedical analyses: 2018 update. Nucleic Acids Res 46(W1), W537–W544, https://doi.org/10.1093/nar/gky379 (2018).
Zhang, Y. I-TASSER server for protein 3D structure prediction. BMC Bioinformatics 9, 40 (2008).
Roy, A., Kucukural, A. & Zhang, Y. I-TASSER: a unified platform for automated protein structure and function prediction. Nat Protoc 5, 725–738 (2010).
Yang, J. et al. The I-TASSER Suite: protein structure and function prediction. Nat Methods 12, 7–8 (2015).
Case, D. A. et al. The Amber biomolecular simulation programs. J Comput Chem 26, 1668–1688 (2005).
Case, D. A. et al. AMBER 12. University of California, San Francisco (2012).
Acknowledgements
This project was funded by Public Health England GIA grant project 109506. The views expressed are those of the authors and not necessarily those of the funding body.
Author information
Authors and Affiliations
Contributions
M.W. wrote the main manuscript text. M.W., S.J. and K.M.R. prepared the figures. M.W., S.J., L.B. and K.M.R. performed all experiments. M.W., K.M.R. and J.M.S. designed and evaluated results from all experiments. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wand, M.E., Jamshidi, S., Bock, L.J. et al. SmvA is an important efflux pump for cationic biocides in Klebsiella pneumoniae and other Enterobacteriaceae. Sci Rep 9, 1344 (2019). https://doi.org/10.1038/s41598-018-37730-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-37730-0
This article is cited by
-
Pseudomonas aeruginosa adapts to octenidine via a combination of efflux and membrane remodelling
Communications Biology (2021)
-
The Acinetobacter baumannii disinfectant resistance protein, AmvA, is a spermidine and spermine efflux pump
Communications Biology (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.