Abstract
This study investigates the relationship between objective cognitive impairment (OCI), subjective cognitive complaints and depressive symptoms in men and women with classical and non-classical Fabry disease (FD). Cognitive functioning was assessed using a neuropsychological test battery, subjective cognitive complaints using a structured interview and depressive symptoms using a depression scale (CESD). Eighty-one patients were included (mean age 44.5 ± 14.3, 35% men, 74% classical). Subjective cognitive complaints were reported by 64% of all patients. OCI was present in thirteen patients (16%), predominantly in men with classical FD. Thirty-one patients (38%) had a high score (≥16) on the CESD scale. Male sex (OR, 6.8; 95%CI, 1.6–39.8; p = 1.6 * 10−2) and stroke (OR, 6.4; 95% CI, 1.1–41.0; p = 3.7 * 10−2) were independently positively associated with OCI, and premorbid IQ (one IQ point increase: OR, 0.91; 95%CI, 0.82–0.98; p = 3.8 * 10−2) was independently negatively associated with OCI. The CESD-score (one point increase: OR, 1.07; 95% CI, 1.02–1.13; p = 3.3 * 10−3) and a history of depression (OR, 2.7; 95% CI, 1.1–7.3; p = 3.9 * 10−2) were independently positively associated with subjective cognitive complaints. OCI is present in 16% of FD patients, warranting referral for neuropsychological assessment. Nevertheless, subjective cognitive complaints are related to depressive symptoms, emphasizing the importance of recognition and treatment of the latter.
Similar content being viewed by others
Introduction
Fabry disease (FD; OMIM 301500) is a rare, X-linked, lysosomal storage disorder. A mutation in the GLA-gene causes a lack or absence of enzymatic activity of α-galactosidase A resulting in the accumulation of glycosphingolipids, mainly affecting the cardiovascular and nervous system. Sex and phenotype have been determined as important predictors of the disease course in FD1. Women generally have a more attenuated disease course compared to men1. Phenotypically, FD can be split in a milder, non-classical and a classical, more severe phenotype, with multi-organ involvement2.
Frequent cerebral manifestations of FD are the occurrence of white matter lesions (WMLs), TIA and stroke. Furthermore, depressive symptoms are highly prevalent3. WMLs, stroke and depression in itself are known to result in objective cognitive impairment (OCI) in the general population4. Previous studies on OCI in FD were limited by small sample size, often did not incorporate neuroimaging, combined WMLs and stroke as a single entity and did not differentiate between patient groups with different FD phenotypes and sex3,5,6,7. Small study populations also restricted the identification of variables related to OCI in FD.
Subjective cognitive complaints are frequently mentioned by FD patients during their routine clinic visits and were related to depressive symptoms but not to OCI in a recent study in a FD population7. Extending knowledge on the relationship between subjective cognitive complaints and depressive symptoms and/or OCI can have significant implications for the therapeutic measures indicated to address these complaints. The objective of this study was to investigate the prevalence of OCI, subjective cognitive complaints, depressive symptoms and to explore their risk factors and interrelation in patients with FD in general as well as in subgroups defined by sex and FD phenotype.
Results
Baseline characteristics
Of the 154 known FD patients in the AMC, ten patients were not considered eligible because of comorbidity known to influence the neuropsychological test results (autism (n = 2), blindness (n = 1), intellectual and developmental disabilities (n = 3), severe aphasia (n = 1)) or because of insufficient knowledge of the Dutch language (n = 3).
Of the 144 contacted patients, 63 patients were not willing to participate (not interested (n = 29), time constraints (n = 8) and participation being too strenuous (n = 26)). There were no significant differences between participants and non-participants in sex, phenotype, age, TIA, stroke or median Fazekas score (see Supplemental Table E-4 for data on non-participants). A total of 81 patients were included with a mean age of 44.5 ± 14.3 years (range: 19–76 years) (Table 1). Fifty-three patients were women (65%) and 60 patients had classical FD phenotype (74%). Twenty-two patients (27%) reported a history of or a current depression, as diagnosed by their general practitioner, psychologist or psychiatrist, without statistically significant differences between subgroups split by sex and phenotype (p = 6.6 * 10−1).
Subjective cognitive complaints
Fifty-two patients (64%) experienced subjective cognitive complaints in at least one domain, without statistically significant differences between subgroups split by sex and phenotype (p = 3.0 * 10−1) (Table 2).
Objective cognitive impairment
There were no signs of underachievement or lack of motivation in any of the patients based on the TOMM score.
A total of 13 (16%) patients had any OCI, of which four (5%) had severe OCI (Table 2). Seven men with classical FD (41%) had any OCI of which two (12%) had severe OCI. For men with non-classical FD this was three (27%) and one (9%), respectively, and in women with classical FD this was three (7%) and one (2%), respectively. OCI did not occur in women with non-classical FD.
Most abnormal T-scores (T-scores ≤33) were found in the attention and executive functioning domain (Table 2). Decreased T-scores were found in the attention and executive functioning domain in men with classical FD (T-score, 45.6; p = 1.4 * 10−2) and men with non-classical FD (T-score, 46.6; p = 1.2 * 10−2) (Table 3). None of the patients scored <24 on the MMSE, suggesting lack of sensitivity for the detection of OCI in FD using this cut-off. After post-hoc correction there were no differences in premorbid IQ between the subgroups divided by sex and phenotype (Table 3). However, there was a difference looking at sex only: men had a lower premorbid IQ compared to women (W = 468.5, p = 6.6 * 10−3).
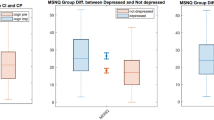
Questionnaires
Thirty-one patients (38.3%) scored ≥16 on the CESD, indicating the presence of depressive symptoms (Table 4), with comparable scores in all subgroups. MSSI scores were higher in men and women with classical FD and men with non-classical disease compared to women with non-classical disease, indicating less severe disease in women with non-classical disease. BPI, MCS and PCS scores were comparable in all subgroups, indicating no differences in pain, mental QoL and physical QoL in all subgroups, respectively. Almost half of all patients (n = 39) experienced poor sleep quality.
Cerebral involvement
Ten patients had a history of stroke as diagnosed by a neurologist, none of them were women with non-classical FD (Table 5). Seventy-three patients (90%) had an MRI brain before the neuropsychological assessment. WMLs were present in 43 patients (58.9%) and were most often mild (total Fazekas score of 1 or 2) (n = 27) (median time between MRI and assessment: 0.7 years).
Variables affecting cognitive domains
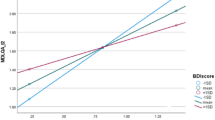
Higher premorbid IQ was related to increased T-scores in all five domains (Table 6). Men generally scored lower on processing speed (β = −5.37; 95%CI −8.92 to −1.81; p = 3.6 * 10−3) compared to women. Other factors related to a lower T-score on processing speed were the pain score (one point increase BPI interference: β = −1.31; 95%CI −2.12 to −0.51; p = 1.8 * 10−3), being single (β = −5.19; 95%CI −8.69 to −1.68; p = 4.3 * 10−3), the MSSI score (one point increase: β = −0.20; 95%CI −0.33 to −0.06; p = 4.9 * 10−3) and BAD (one mm increase: β = −3.68; 95%CI −5.92 to −1.17; p = 4.1 * 10−3). Being employed was positively related to processing speed (β = 4.94; 95%CI 1.46 to 8.42; p = 5.9 * 10−3).
Being single was also negatively related to executive functioning (β = −5.15; 95%CI −8.33 to −1.97; p = 1.8 * 10−3).
BAD and Fazekas score were related to a lower T-score on the memory domain (BAD: increase one mm β = −4.05; 95%CI −6.64 to −0.85; p = 1.2 * 10−2, Fazekas: one point increase β = −1.80; 95%CI −3.10 to −0.51; p = 7.1 * 10−3) as was being single (β = −5.15; 95%CI −10.32 to −2.12; p = 3.4 * 10−3).
Variables affecting objective cognitive impairment
Male sex was positively related to the presence of OCI (rτ = 0.39; 95%CI, 0.15 to 0.58; p = 5.1 * 10–4) (Table 6). This relation was still present when comparing men with classical FD to all other patients (rτ = 0.35; 95%CI, 0.09 to 0.60; p = 1.7 * 10−3). Higher premorbid IQ was negatively related to the presence of OCI (rτ = −0.29; 95%CI, −0.45 to −0.079; p = 2.2 * 10−3). There was a positive relation between brain parameters and the presence of OCI (Fazekas score, rτ = 0.22; 95%CI, −0.02 to 0.41; p = 4.7 * 10−2, BAD, rτ = 0.22; 95%CI, −0.04 to 0.37; p = 2.1 * 10−2). This relation was more robust when only the relationship of severe OCI to the Fazekas score was considered (rτ = 0.31; 95%CI, 0.18 to 0.41; p = 5.2 * 10−3). There was a positive relation between a history of stroke and the presence of OCI (rτ = 0.25; 95%CI, −0.04 to 0.52; p = 2.9 * 10−2). There was no relation between OCI and the CESD score or between OCI and subjective cognitive complaints.
Two logistic regression models were comparable in AIC and both were in agreement with our theoretical concepts. The first model showed that male sex (OR, 6.8; 95%CI, 1.6 to 39.8; p = 1.6 * 10−2) and a history of stroke (OR, 6.4; 95%CI, 1.1 to 41.0; p = 3.7 * 10−2) were independently positively associated with OCI and that premorbid IQ (one IQ point increase: OR, 0.91; 95%CI, 0.82 to 0.98; p = 3.8 * 10−2) was independently negatively related to OCI. The second model showed that male sex (OR, 5.9; 95%CI, 1.4 to 31.7; p = 2.3 * 10−2) and being single (OR, 4.8; 95%CI, 1.2 to 25.2; p = 3.9 * 10−2) were both independently positively associated with OCI and that premorbid IQ (one IQ point increase: OR, 0.91; 95%CI, 0.81 to 0.99; p = 4.6 * 10−2) was independently negatively associated with OCI. Including male sex, a history of stroke, being single and premorbid IQ in one model did not improve the model.
Variables affecting subjective cognitive complaints
The CESD score was most strongly positively related to subjective cognitive complaints (rτ = 0.36; 95%CI, 0.18 to 0.51; p = 2.7 * 10−5) (Table 6). The PSQI score (rτ = 0.30; 95%CI, 0.13 to 0.45; p = 7.8 * 10−4) and the MSSI score also showed a positive relation to subjective cognitive complaints, the latter relation was mostly driven by the MSSI general and MSSI neurological subscores (MSSI general, rτ = 0.32; 95%CI, 0.15 to 0.48; p = 2.4 * 10−4; MSSI neurological, rτ = 0.32; 95%CI, 0.15 to 0.46; p = 2.7 * 10−4). Being employed was negatively related to subjective cognitive complaints (rτ = −0.29; 95%CI, −0.46 to −0.11; p = 4.6 * 10−3). MCS and PCS scores were also negatively related to subjective cognitive complaints (MCS, rτ = −0.29; 95%CI, −0.45 to −0.10; p = 6.9 * 10−4; PCS, rτ = −0.32; 95%CI, −0.46 to −0.18; p = 1.9 * 10−4).
In a proportional odds model, the CESD score (one point increase: OR, 1.07; 95%CI, 1.02 to 1.13; p = 3.3 * 10−3), a history of depression (OR, 2.7; 95%CI, 1.1 to 7.3; p = 3.9 * 10−2) and the MSSI general score (one point increase: OR, 1.3; 95%CI, 1.1 to 1.5; p = 5.5 * 10−3) were independently positively associated with subjective cognitive complaints.
Discussion
In this large sample of Dutch patients with FD we have, for the first time, shown a relationship between sex, phenotype and risk for OCI. OCI was present in 41% of men with classical disease, affecting mostly the executive functioning domain. In addition, OCI was found in a significant number (27%) of men with non-classical FD. In women with classical FD, however, the prevalence of OCI was markedly lower (7%) and none of the women with non-classical FD had OCI. The risk of OCI in patients with FD was independently related to male sex, a history of stroke and to premorbid IQ.
In a healthy population of male veterans from the United States (n = 4371), slightly younger compared to our cohort (38.4 ± 2.5 years), OCI was found in ~6–7% of this cohort when using similar criteria8. In a second healthy mixed control group (n = 138) of a study on the cognitive effects of type 1 diabetes, with comparable age (49 ± 7 years) to our study population, the prevalence of OCI was 5%9. This indicates that OCI in our population of FD patients is much higher in male patients than would be expected in this age group. In women with FD the prevalence of OCI is comparable to that in the general population. Loeb et al.7 found OCI in 30% of patients with FD, but used different criteria to define OCI and a smaller reference population (n = 80), possibly explaining the differences. The impaired executive domain found in our study is in accordance with previous studies in FD3. Moreover, our study confirms the preliminary finding of a study by Sigmundsdottir et al.5 that men with FD are more likely to get OCI, especially in those with classical disease.
In addition, a relationship between the extent of the WMLs (Fazekas score) and the presence of severe OCI was established. In a previous study a subgroup of patients with markedly increased volumes of white matter lesions showed more cognitive deficits compared to patients with lower lesion volumes6. In the general population, as was found in our study, the positive relationship between WMLs and OCI is not very strong10. It has been postulated that a threshold of WML severity needs to be surpassed before OCI develops10.
The relation between stroke and OCI in the general population has been more firmly established11. Likewise, in our study the relation between a history of stroke and OCI in FD is clearly present. This was also observed in previous studies in FD, albeit using univariate analyses5,7. The positive relationship between (premorbid) IQ and neuropsychological test scores has been firmly established in the general population8,12. It has been theorized that a higher premorbid IQ reflects a greater “cognitive reserve”, thus more decline has to take place before OCI occurs13,14. The observation that higher T-scores in FD patients with higher premorbid IQ lower the chance of OCI fits this hypothesis. We also found a lower median premorbid IQ in men compared to women. Despite this difference, male sex was related to a higher risk of OCI independently of premorbid IQ. Premorbid IQ therefore does not fully explain the differences in prevalence of OCI between men and women with FD.
A new finding is that almost two-thirds of our cohort of FD patients experienced subjective cognitive complaints, without significant differences in prevalence between all subgroups. Interestingly, in our study the subjective cognitive complaints were not related to OCI, but showed a clear relation with both depression in the past and current depressive symptoms. In the general population, the relation between OCI and subjective cognitive complaints is still controversial15. More thoroughly established is that patients with depression have a higher prevalence of subjective cognitive complaints16, as was also previously shown by Loeb et al.7 in a population of FD patients. The relation of depressive symptoms to subjective cognitive complaints further emphasizes the importance of recognizing these symptoms. Conversely, Loeb et al.7 concluded that in patients with FD prevalence of subjective cognitive complaints is not increased. It seems that, in our cohort of FD patients, subjective cognitive complaints were highly prevalent. Of these, subjective memory complaints were present in 46% of our cohort (data not shown), while these are found in 22% of the general population17, indicating that the prevalence in patients with FD could be more than twice as high. The difference to our study might be caused by the difference in assessment (structured interview versus questionnaire) as well as the use of a high cutoff (mean +2 SD compared to a healthy population) for detecting subjective cognitive complaints in the Loeb et al.7 study. The high prevalence (38%) of depressive symptoms in our study is in line with the previously found prevalence of 46% from a mixed cohort of 186 patients with FD18. In populations with chronic diseases or chronic pain various treatments have been shown to improve depressive complaints19,20. Unfortunately, treatment effects and risk factors for depression in FD are largely unknown. Only one small, uncontrolled study (n = 15) looked at the effect of psychological counseling and found all FD patients improving21. Therefore, efficacy of treatment options for depressive symptoms should be topic of further research in FD patients.
This study has some strengths and limitations. Strengths are the precise phenotyping of the studied cohort and the use of a reliable cognitive test battery. Moreover, this study is the first to combine data on subjective cognitive complaints, depressive symptoms, cognitive functioning and MRI brain parameters in subgroups of patients divided by sex and FD phenotype.
We included 81 patients, more than half of the known patients in the Netherlands, a fairly large group for a rare disease like FD. However, we cannot rule out inclusion bias: patients with subjective cognitive complaints might be more interested in participation. Conversely, patients with severe cognitive impairment might not participate due to participation begin to strenuous. Nevertheless, we found no significant differences in patient characteristics, nor in the presence of TIA, stroke or the height of the Fazekas score between participants and non-participants in this study.
MRIs were made using the same standardized protocol, as part of routine follow up. This means that sometimes there was a time gap between the MRI and the neuropsychological assessment, but in most patients this was not more than a year and WMLs are known to increase slowly. Of some patients MRI of the brain was not available, mostly due to the presence of non-MRI compatible ICD/pacemakers. Excluding these patients, however, might also lead to a bias towards less affected patients.
We did not assess a healthy control group ourselves. Instead, we used large normative datasets (median sample size: 471) compiled of healthy control groups from multiple studies. Furthermore, most neuropsychological test results were corrected for age, sex and education level, although not for (premorbid) IQ.
Lastly, we used the Fazekas-scale to assess WMLs in this study. It has been shown that visual rating scales have a lower ceiling compared to volumetric measurements of WMLs22. Perhaps, the use of volumetric measurement of WMLs would have strengthened the relation to OCI.
In conclusion, OCI is present in one-sixth of FD patients, predominantly in men with classical disease. The relation between a history of stroke and OCI in this study re-emphasizes the importance of prevention of stroke in patients with FD. Moreover, the presence of stroke or other clinical indications of OCI warrants referral of FD patients for neuropsychological assessment. The high prevalence of subjective cognitive complaints, equally distributed over the phenotypes and sexes, was not explained by OCI, but showed a clear relation with current or historical depressive complaints. Evaluation of subjective cognitive complaints in patients with FD should therefore include a psychological evaluation and healthcare professionals should focus on recognition and treatment of depressive symptoms.
Methods
Study design and phenotype
The baseline data of an ongoing prospective cohort study on neuropsychological functioning in adult patients (≥18 years) with a definite diagnosis of FD23 are presented. All known adult Fabry patients (n = 154) at the Academic Medical Centre (AMC), the national referral centre for patients with FD in the Netherlands, were screened for eligibility.
All patients were phenotypically characterized as having classical or non-classical FD2, see Supplemental File 1 for criteria. Demographic parameters, clinical and disease characteristics of all patients were gathered from the local Fabry database containing prospectively collected data as well as from medical records.
This study was approved by the Human Research Ethics Committee of the AMC and conducted in accordance with the Declaration of Helsinki in 201324. All participants provided informed consent prior to inclusion and all experiments were performed in accordance with relevant guidelines and regulations. The datasets generated and analyzed during the current study are not publicly available. Because of the rarity of the disease, even anonymized can be linked to a specific individual. In case of a specific scientific question, requests to make part of the dataset available will be reviewed.
Neuropsychological assessment
All included patients completed a neuropsychological test battery assessing language skills, memory, visuospatial perception, processing speed and executive functioning. Language skills were assessed using the Boston Naming Test (BNT)25 and the Wechsler Adult Intelligence Scale IV: Similarities (WAIS-IV: S)26. Memory was assessed using the Dutch version of The Rey Auditory Verbal Learning Test (RAVLT)27 and the Rivermead Behavioural Memory Test (RBMT): Storytelling28, both assessing immediate recall (ir) and delayed recall (dr). Visuospatial perception was assessed using the WAIS IV: Block Design (BD) and the Judgement of Line Orientation (JLO)26,29. Processing speed was assessed using the Trail Making Test part A (TMTA)30, Stroop Word (W) and Stroop Colour (C)31. Executive functioning was assessed using the TMT part B (TMTB)30, Stroop Colour-Word (CW)31, semantic fluencies, referred to as Animal Fluency and Occupational Fluency32 and phonetic fluency, referred to as Letter Fluency33.
T-scores (mean of 50, standard deviation (SD) of 10) were calculated per test using extensive Dutch normative data, except for the JLO, for which we used normative data from the United States. The median normative data sample size was 471 healthy participants (range: 121–1000). All normative data were corrected for age and most subtests also for sex and educational level. See Supplemental Table E-1 for additional information on the neuropsychological test battery.
General cognitive functioning was screened using the Mini Mental State Exam (MMSE)34. Motivation and underachievement were assessed using the Test of Memory Malingering (TOMM)35. An estimation of intelligence was done using the Dutch Adult Reading Test (DART), the Dutch version of the National Adult Reading which correlates strongly with intellectual ability and is relatively resistant to change by neurological impairment36.
The neuropsychological test battery was preceded by a structured interview assessing subjective cognitive complaints, addressing the following domains: memory, attention and executive complaints. This resulted in a score ranging from 0 to 3: no subjective cognitive complaints (0), subjective cognitive complaints in one domain (1), in two domains (2) or in all three domains (3), see Supplemental File 2.
Objective cognitive impairment
OCI was defined as a T-score ≤33 (<5th percentile, −1.67 SD) on at least two neuropsychological tests, resembling statistical significance of two one-tailed tests with p < 0.05. Severe OCI was defined as a T-score ≤30 (<2.3rd percentile, −2 SD) on at least two neuropsychological tests, resembling statistical significance of two two-tailed tests with p < 0.05. We choose the cutoff of −1.67 SD to prevent high rates of false positives, a strategy which has been recommended for other diseases as well37. To decrease the family-wise error rate, one or more T-scores ≤33 or ≤30 in the following combination of tests assessing a similar cognitive domain, were regarded as a single abnormal T-score: Animal Fluency and/or Occupational Fluency and/or Letter Fluency, RAVLT ir and/or RBMT ir, RAVLT dr and/or RBMT dr, TMTA and/or Stroop W and/or Stroop C, TMTB and/or Stroop CW, WAIS-IV: BD and/or JLO.
Questionnaires
Depressive symptoms were measured using The Centre for Epidemiological Studies – Depression scale (CESD)38. Twenty items on depressive symptoms experienced in the last week are scored on a four point Likert scale (range 0 to 3). Total scores range from 0 to 60 points and patients with scores ≥16 were classified as having depressive symptoms39.
Pain was measured using the Brief Pain Inventory (BPI) which is divided in three separate sub scores: 1) worst pain, 2) average pain and 3) pain interference with life. The latter is an average score of the influence of pain on general activity, mood, walking, work, enjoyment of life, relations and sleep. Pain scores are graded from 0 (absence of pain) to 10 (worst possible pain)40.
Quality of life (QoL) was obtained using the Dutch version of the Short Form-36 Health Survey (SF-36). The SF-36 assesses eight domains of QoL which are calculated using Dutch normative data41. The eight domains can be grouped into two summary scores: the Physical Component Summary (PCS) and the Mental Component Summary (MCS) that are standardized using normative data from the US population and are presented as T-scores42.
Sleep quality was measured using The Pittsburgh Sleep Quality Index (PSQI)43. The PSQI assesses seven domains which are graded from 0 to 3, resulting in a score ranging from 0 to 21. PSQI scores >5 are indicative for poor sleep quality.
Fabry Disease severity was assessed using the Mainz Severity Score index (MSSI, range: 0–76)44. The MSSI is composed of four subscales that cover general (range: 0–18), neurological (range: 0–20), renal (range: 0–18) and cardiac (range: 0–20) signs and symptoms of the disease.
Brain MRI
MRI of the brain was performed yearly or biannually as part of routine follow-up on a 3-T system (Philips Ingenia, Philips Medical Systems, Best, The Netherlands). All MRIs of the brain were made using the same standardized protocol, see Supplemental Table E-2 more information on MRI settings per sequence. Eight patients had no MRI of the brain, six because of the presence of an MRI non-compatible pacemaker or ICD and one because of claustrophobia. In one patient the brain MRI was made in a different hospital. MRIs were re-evaluated by two neuroradiologists, (MRL evaluated basilar artery pathology, MGL evaluated infarctions, WMLs and atrophy), blinded for all patient characteristics. White matter lesions (WMLs) were rated on axial FLAIR using the Fazekas scale, ranging from 0 (no WMLs) to 6 (confluent periventricular and deep WMLs)45. Presence and number of (lacunar) infarctions was rated on DWI, axial T2 and FLAIR images. Basilar artery diameter (BAD) was rated on axial T2 images46. Atrophy of medial and temporal lobe were rated on T1 3D GRE images using the Medial Temporal lobe Atrophy rating scale (MTA)47. See Supplemental Table E-3 for additional information on the scales.
Statistical methods
Data are presented as median and range or mean ± SD where appropriate. R (version 3.3.1) and SPSS version 24.0 (SPSS Inc. Chicago, Illinois, USA) were used for statistical analysis. Between subgroup differences were compared using the Kruskall-Wallis test, one way ANOVA and Fisher’s exact test where appropriate. Post hoc analyses were done with the Dunn test, Tukeys test and 2 × 2 Fisher’s exact tests with Bonferroni-Holm correction for abovementioned tests, respectively. Included and excluded patients were compared as a whole group and per subgroup divided for sex and phenotype. To check if neuropsychological test results differed from the average from the reference cohort, T-scores were compared to a T-score of 50 using a one-sided sign test.
T-scores per cognitive domain were obtained calculating mean T-scores of all tests addressing this domain. Variables were included in the univariate analyses if they were deemed as potentially related to OCI trough literature search in the general population or previous studies on OCI and FD. Next, the univariate models were used to identify variables for multivariate models. Linear regression was used to analyze the univariate relation between variables and T-scores per cognitive domain. Kendall’s tau-b (rτ) was used to analyze the univariate relation between variables and subjective cognitive complaints (range 0–3) and between variables and OCI (binary, yes/no) (Table 6). Bootstrapping was used to calculate bias corrected accelerated 95% confidence intervals (CI) of Kendall’s tau-b, stratified for sex. To minimize the effect of multiple testing, the relation between a variable and OCI was first tested. If the relation between a variable and OCI was (very) weak (≈rτ < 0.1, ≈p > 0.25) a relation between the variable and T-scores per cognitive domain was not tested. To correct for false discovery rate we used the Benjamini-Hochberg procedure in Table 648.
A multiple logistic regression model was used to check which variables are independent risk factors of OCI and a proportional odds model was used to check which variables are independent risk factors of subjective cognitive complaints. Both models were iteratively built selecting variables from univariate models (inclusion if p < 0.10). The Akaike Information Criterion (AIC) was used to optimize the models. We chose the simplest models and compared them to our theoretical concepts. Variance inflation factor was used to explore potential multicollinearity in the logistic regression model. A likelihood ratio test was used to test proportionality of odds, comparing the goodness of fit of the proportional odds model to its multinomial counterpart.
P-values < 0.05 were considered statistically significant. If multiple tests were carried out regarding a single hypothesis, the results were corrected using the Bonferroni-Holm correction, to control for the family wiser error rate49.
Results were reported in accordance with the STROBE guidelines50.
References
Arends, M. et al. Characterization of Classical and Nonclassical Fabry Disease: A Multicenter Study. J Am Soc Nephrol 28, 1631–1641, https://doi.org/10.1681/ASN.2016090964 (2017).
van der Tol, L. et al. Uncertain diagnosis of fabry disease in patients with neuropathic pain, angiokeratoma or cornea verticillata: consensus on the approach to diagnosis and follow-up. JIMD Rep 17, 83–90, https://doi.org/10.1007/8904_2014_342 (2014).
Bolsover, F. E., Murphy, E., Cipolotti, L., Werring, D. J. & Lachmann, R. H. Cognitive dysfunction and depression in Fabry disease: a systematic review. Journal of inherited metabolic disease 37, 177–187, https://doi.org/10.1007/s10545-013-9643-x (2014).
Wardlaw, J. M., Valdés Hernández, M. C. & Muñoz-Maniega, S. What are White Matter Hyperintensities Made of?: Relevance to Vascular Cognitive Impairment. Journal of the American Heart Association: Cardiovascular and Cerebrovascular Disease 4, e001140, https://doi.org/10.1161/JAHA.114.001140 (2015).
Sigmundsdottir, L. et al. Cognitive and psychological functioning in Fabry disease. Arch Clin Neuropsychol 29, 642–650, https://doi.org/10.1093/arclin/acu047 (2014).
Schermuly, I. et al. Neuropsychiatric symptoms and brain structural alterations in Fabry disease. Eur J Neurol 18, 347–353, https://doi.org/10.1111/j.1468-1331.2010.03155.x (2011).
Loeb, J., Feldt-Rasmussen, U., Madsen, C. V. & Vogel, A. Cognitive Impairments and Subjective Cognitive Complaints in Fabry Disease: A Nationwide Study and Review of the Literature. JIMD Rep. https://doi.org/10.1007/8904_2018_103 (2018).
Donnell, A. J., Belanger, H. G. & Vanderploeg, R. D. Implications of psychometric measurement for neuropsychological interpretation. The Clinical neuropsychologist 25, 1097–1118, https://doi.org/10.1080/13854046.2011.599819 (2011).
Nunley, K. A. et al. Clinically Relevant Cognitive Impairment in Middle-Aged Adults With Childhood-Onset Type 1 Diabetes. Diabetes Care 38, 1768–1776, https://doi.org/10.2337/dc15-0041 (2015).
Desmond, D. W. Cognition and White Matter Lesions. Cerebrovascular Diseases 13(suppl 2), 53–57, https://doi.org/10.1159/000049151 (2002).
Makin, S. D., Turpin, S., Dennis, M. S. & Wardlaw, J. M. Cognitive impairment after lacunar stroke: systematic review and meta-analysis of incidence, prevalence and comparison with other stroke subtypes. J Neurol Neurosurg Psychiatry 84, 893–900, https://doi.org/10.1136/jnnp-2012-303645 (2013).
Binder, L. M., Iverson, G. L. & Brooks, B. L. To Err is Human: “Abnormal” Neuropsychological Scores and Variability are Common in Healthy Adults. Archives of Clinical Neuropsychology 24, 31–46, https://doi.org/10.1093/arclin/acn001 (2009).
Tucker-Drob, E. M., Johnson, K. E. & Jones, R. N. The cognitive reserve hypothesis: a longitudinal examination of age-associated declines in reasoning and processing speed. Developmental psychology 45, 431–446, https://doi.org/10.1037/a0014012 (2009).
Rentz, D. M. et al. Use of IQ-adjusted norms to predict progressive cognitive decline in highly intelligent older individuals. Neuropsychology 18, 38–49, https://doi.org/10.1037/0894-4105.18.1.38 (2004).
Burmester, B., Leathem, J. & Merrick, P. Subjective Cognitive Complaints and Objective Cognitive Function in Aging: A Systematic Review and Meta-Analysis of Recent Cross-Sectional Findings. Neuropsychology Review 26, 376–393, https://doi.org/10.1007/s11065-016-9332-2 (2016).
Reid, L. M. & MacLullich, A. M. J. Subjective Memory Complaints and Cognitive Impairment in Older People. Dementia and Geriatric Cognitive Disorders 22, 471–485, https://doi.org/10.1159/000096295 (2006).
Bassett, S. S. & Folstein, M. F. Memory complaint, memory performance, and psychiatric diagnosis: a community study. Journal of geriatric psychiatry and neurology 6, 105–111, https://doi.org/10.1177/089198879300600207 (1993).
Cole, A. L. et al. Depression in adults with Fabry disease: a common and under-diagnosed problem. J Inherit Metab Dis 30, 943–951, https://doi.org/10.1007/s10545-007-0708-6 (2007).
Williams, A. C., Eccleston, C. & Morley, S. Psychological therapies for the management of chronic pain (excluding headache) in adults. The Cochrane database of systematic reviews 11, Cd007407, https://doi.org/10.1002/14651858.CD007407.pub3 (2012).
Clarke, D. M. & Currie, K. C. Depression, anxiety and their relationship with chronic diseases: a review of the epidemiology, risk and treatment evidence. The Medical journal of Australia 190, S54–60 (2009).
Ali, N., Gillespie, S. & Laney, D. Treatment of Depression in Adults with Fabry Disease. JIMD Rep 38, 13–21, https://doi.org/10.1007/8904_2017_21 (2018).
Kapeller, P. et al. Visual rating of age-related white matter changes on magnetic resonance imaging: scale comparison, interrater agreement, and correlations with quantitative measurements. Stroke 34, 441–445 (2003).
Smid, B. E. et al. Uncertain diagnosis of Fabry disease: consensus recommendation on diagnosis in adults with left ventricular hypertrophy and genetic variants of unknown significance. Int J Cardiol 177, 400–408, https://doi.org/10.1016/j.ijcard.2014.09.001 (2014).
World Medical Association Declaration of Helsinki. ethical principles for medical research involving human subjects. Jama 310, 2191–2194, https://doi.org/10.1001/jama.2013.281053 (2013).
Kaplan, E., Goodglass, H. & Weintraub, S. (Lee & Febiger, Philadelphia, 1983).
WAIS-IV-NL: Afname- en scoringshandleiding. (NCS Pearson, Inc, 2012).
Van der Elst, W., van Boxtel, M. P., van Breukelen, G. J. & Jolles, J. Rey’s verbal learning test: normative data for 1855 healthy participants aged 24–81 years and the influence of age, sex, education, and mode of presentation. J Int Neuropsychol Soc 11, 290–302, https://doi.org/10.1017/s1355617705050344 (2005).
Van Balen, H. G. G. & Groot Zwaaftink, A. J. M. (Pearson Information and Assessment BV, Amsterdam, 1993).
Benton, A. L., Sivan, A. B., Hamsher, K. S., Varney, N. R. & Spreen, O. Contributions to Neuropsychological Assessment—A Clinical Manual. 2 edn, (Oxford University Press, 1994).
Partington, J. E. & Leiter, R. G. (Psychological Services Center, Washington, DC, 1949).
Stroop, J. R. Studies of interference in serial verbal reactions. Journal of Experimental Psychology 18, 643–662 (1935).
Mulder, J. L., Dekker, P. H. & Dekker, R. (PITS Uitgeverij BV, Leiden, 2006).
Schmand, B., Groenink, S. C. & van den Dungen, M. [Letter fluency: psychometric properties and Dutch normative data]. Tijdschrift voor gerontologie en geriatrie 39, 64–76 (2008).
Folstein, M. F., Robins, L. N. & Helzer, J. E. The Mini-Mental State Examination. Archives of general psychiatry 40, 812, https://doi.org/10.1001/archpsyc.1983.01790060110016 (1983).
Rees, L. M., Tombaugh, T. N., Gansler, D. A. & Moczynski, N. P. Five validation experiments of the Test of Memory Malingering (TOMM). Psychological Assessment 10, 10–20, https://doi.org/10.1037/1040-3590.10.1.10 (1998).
Schmand, B., Bakker, D., Saan, R. & Louman, J. The Dutch Reading Test for Adults: a measure of premorbid intelligence level. Tijdschrift voor gerontologie en geriatrie 22, 15–19 (1991).
Gisslen, M., Price, R. W. & Nilsson, S. The definition of HIV-associated neurocognitive disorders: are we overestimating the real prevalence? BMC infectious diseases 11, 356, https://doi.org/10.1186/1471-2334-11-356 (2011).
Radloff, L. S. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement 1, 385–401, https://doi.org/10.1177/014662167700100306 (1977).
Bouma, J., Ranchor, A. V., Sanderman, R. & Van Sonderen, E. (ed. NCG) (UMCG, 2012).
Cleeland, C. S. & Ryan, K. M. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore 23, 129–138 (1994).
Aaronson, N. K. et al. Translation, validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. Journal of clinical epidemiology 51, 1055–1068 (1998).
Ware, J. E. et al. Comparison of Methods for the Scoring and Statistical Analysis of SF-36 Health Profile and Summary Measures: Summary of Results from the Medical Outcomes Study. Medical care 33, AS264–AS279 (1995).
Buysse, D. J., Reynolds, C. F. 3rd, Monk, T. H., Berman, S. R. & Kupfer, D. J. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry research 28, 193–213, https://doi.org/10.1016/0165-1781(89)90047-4 (1989).
Whybra, C. et al. The Mainz Severity Score Index: a new instrument for quantifying the Anderson-Fabry disease phenotype, and the response of patients to enzyme replacement therapy. Clinical genetics 65, 299–307, https://doi.org/10.1111/j.1399-0004.2004.00219.x (2004).
Fazekas, F., Chawluk, J. B., Alavi, A., Hurtig, H. I. & Zimmerman, R. A. MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR. American journal of roentgenology 149, 351–356, https://doi.org/10.2214/ajr.149.2.351 (1987).
Fellgiebel, A. et al. Diagnostic utility of different MRI and MR angiography measures in Fabry disease. Neurology 72, 63–68, https://doi.org/10.1212/01.wnl.0000338566.54190.8a (2009).
Scheltens, P. et al. Atrophy of medial temporal lobes on MRI in “probable” Alzheimer’s disease and normal ageing: diagnostic value and neuropsychological correlates. J Neurol Neurosurg Psychiatry 55, 967–972, https://doi.org/10.1136/jnnp.55.10.967 (1992).
Benjamini, Y. & Hochberg, Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. Journal of the Royal Statistical Society. Series B (Methodological) 57, 289–300, https://doi.org/10.2307/2346101 (1995).
Holm, S. A Simple Sequentially Rejective Multiple Test Procedure. Scandinavian Journal of Statistics 6, 65–70, https://doi.org/10.2307/4615733 (1979).
von Elm, E. et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Bmj 335, 806–808, https://doi.org/10.1136/bmj.39335.541782.AD (2007).
Acknowledgements
We would like to thank Shirley Klein–van Loon and Frederique Bos for help with the data acquisition and Paul Groot for the acquisition of the MRIs. The abstract of this article was presented as a poster at the 14th annual WORLD symposium San Diego (2018). Study funded by the Academic Medical Center (innovation grant 2014).
Author information
Authors and Affiliations
Contributions
S. Körver: study design, acquisition, analysis and interpretation of data, first draft of manuscript. Gert J. Geurtsen: study design, interpretation of data, study supervision, critical revision of manuscript. Carla E.M. Hollak: study concept, study design, interpretation of data, study supervision, critical revision of manuscript. Ivo N. van Schaik: interpretation of data, study supervision, critical revision of manuscript. Maria G.F. Longo: acquisition and interpretation of data, critical revision of manuscript. Marjana R. Lima: acquisition and interpretation of data, critical revision of manuscript. Leonardo Vedolin: critical revision of manuscript. Marcel G.W. Dijkgraaf: statistical support, critical revision of manuscript. Mirjam Langeveld: interpretation of data, study supervision, critical revision of manuscript.
Corresponding author
Ethics declarations
Competing Interests
Simon Körver, Gert J. Geurtsen, Maria G.F. Longo, Marjana R. Lima, Leonardo Vedolin and Marcel G.W. Dijkgraaf declare no competing interests. Carla E.M. Hollak declares that Sphinx (through AMC-research BV) is involved in pre-marketing studies with Sanofi-Genzyme, Protalix and Idorsia; she does not have any other financial relationship with pharmaceutical companies and reports no nonfinancial competing interests. Ivo N. van Schaik chairs a steering committee for CSL Behring and received departmental honoraria for serving on scientific advisory boards for CSL Behring and Baxter. All lecturing and consulting fees for INS were donated to the Stichting Klinische Neurologie, a local foundation that supports research in the field of neurological disorders. He reports no non-financial competing interests. Mirjam Langeveld declares that Sphinx (through AMC-research BV) is involved in pre-marketing studies with Sanofi- Genzyme, Protalix and Idorsia; she does not have any other financial relationship with pharmaceutical companies and reports no nonfinancial competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Körver, S., Geurtsen, G.J., Hollak, C.E.M. et al. Predictors of objective cognitive impairment and subjective cognitive complaints in patients with Fabry disease. Sci Rep 9, 188 (2019). https://doi.org/10.1038/s41598-018-37320-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-37320-0
This article is cited by
-
The impact of demographic and clinical characteristics on the trajectories of health-related quality of life among patients with Fabry disease
Orphanet Journal of Rare Diseases (2021)
-
Depressive symptoms in Fabry disease: the importance of coping, subjective health perception and pain
Orphanet Journal of Rare Diseases (2020)
-
Mechanisms of cognitive dysfunction in CKD
Nature Reviews Nephrology (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.