Abstract
Most research laboratories abide by guidelines and mandates set by their research institution regarding the administration of analgesics to control pain during the postoperative period. Unfortunately, measuring pain originating from the head is difficult, making adequate decisions regarding pain control following stereotaxic surgery problematic. In addition, most postsurgical analgesia protocols require multiple injections over several days, which may cause stress and distress during a critical recovery period. Here we sought to (1) assess the degree of postoperative pain following craniotomy in mice, (2) compare the efficacy of three common rodent analgesics (carprofen, meloxicam and buprenorphine) for reducing this pain and (3) determine whether the route of administration (injected or self-administered through the drinking supply) influenced pain relief post-craniotomy. Using the mouse grimace scale (MGS), we found that injectable analgesics were significantly more effective at relieving post-craniotomy pain, however, both routes of administration decreased pain scores in the first 24 h postsurgery. Specifically, buprenorphine administered independently of administration route was the most effective at reducing MGS scores, however, female mice showed greater sensitivity to carprofen when administered through the water supply. Although it is necessary to provide laboratory animals with analgesics after an invasive procedure, there remains a gap in the literature regarding the degree of craniotomy-related pain in rodents and the efficacy of alternative routes of administration. Our study highlights the limitations of administering drugs through the drinking supply, even at doses that are considered to be higher than those currently recommended by most research institutions for treating pain of mild to moderate severity.
Similar content being viewed by others
Introduction
In neuroscience, there are a variety of approaches and techniques that require direct access to the rodent brain. Consequently, it has become increasingly common for many neuroscience labs to perform craniotomies, an invasive brain surgery in which the brain is accessed via removal of a section of the skull, so that studies involving intracranial injections, cannulations, electrical stimulation, or optical implants can be conducted1,2,3. However, the pharmacological management of post-craniotomy pain has yet to be standardized and there are no current evidence-based recommendations for the alleviation of craniotomy pain in mice. Given that the insufficient management of acute pain following surgery may lead to depression and anxiety4,5 – behaviors directly studied by many neuroscience labs – finely-tuned pain control following craniotomy should be prioritized and properly evaluated.
The establishment of a standardized analgesic regiment for post-craniotomy pain in animals has been hindered by the difficulty in assessing the degree of pain postsurgery and the efficacy of chosen analgesics. Traditional pain measurement in laboratory rodents has heavily relied on evoked pain behaviors. However, these assays are impractical for assessing pain originating from surgical operations involving the head and scalp (see6 for a review). Non-selective proxy measures such as cardiovascular changes, food and water intake, locomotion, and nest construction have been used to measure ‘spontaneous’ pain following injury with varying degrees of success and large inter-subject variability7,8,9. In addition, learning paradigms such as conditioned place preference have also been used to evaluate postoperative pain and pain relief following surgery10, but these studies are often limited by one-trial learning making the assessment of pain over time difficult.
The recent implementation of the grimace scales has expanded our ability to assess pain in rodents11,12 and potentially addresses some of the issues associated with evoked or proxy measures of pain in laboratory animals6. The grimace scale was originally developed for mice based on the facial action coding system for pain in infants and non-verbal humans13. The mouse grimace scale (MGS) measures changes in facial musculature – orbital tightening, nose bulge, cheek bulge, ear change, and whisker change – following injury11. Each feature is given a score of 0 (not present), 1 (moderate) or 2 (severe), which can be scored with remarkably high reliability and accuracy. Although the grimace scale has been readily evaluated in mice11,14,15 and rats12,16, other grimace scales have been developed to capture ‘pain faces’ in horses17, cats18, rabbits19, sheep20 and ferrets21, which have helped to evaluate postoperative pain across species.
The sensitivity of the MGS allows for the detection of postoperative pain upwards of 48 h following surgery14. There is a strong positive correlation between MGS scores and pain-associated behaviors in mice22, suggesting that facial expressions of pain could provide a rapid and reliable clinical pain assessment modality. Because the mouse grimace scale has been shown to be a reliable indicator of pain postsurgery14,15,22, we used it as an assessment tool to characterize the extent and duration of postoperative pain in mice following craniotomy. We evaluated the efficacy of common rodent analgesics: the μ-opioid receptor partial agonist buprenorphine and nonsteroidal anti-inflammatory drugs (NSAID) carprofen and meloxicam. Further, since multiple injections of analgesics are often required for pain management in rodents5, we assessed whether self-administration of these analgesics (i.e. through the drinking supply) offered comparable analgesia to the injectable formulations. We largely find that analgesics administered through an injection route were more effective in reducing MGS scores when compared with free access through the drinking supply. Buprenorphine was the most effective for treating pain in both males and females, although minor sex differences emerged for carprofen.
Results
The experimental timeline is shown in Fig. 1. A five-way ANOVA of all data (site × sex × administration route × drug × repeated measure) revealed a main effect for time course (F5,142 = 143.4, p < 0.001), a main effect for administration route (F1,142 = 4.77, p = 0.03) and a three-way interaction between sex, administration route and drug (F5,142 = 2.56, p = 0.03). There was also a three-way interaction between administration route, drug and time course (F25,142 = 2.51, p < 0.001). No other meaningful interactions reached significance (All F’s < 2.2, p > 0.05). Because there was no main effect for site (F1,142 = 2.0, p = 0.16) and analysis of baseline MGS scores showed no difference with respect to the source of the mice (mice bred in-house, 0.07 ± 0.01 vs. mice purchased from CRL, 0.07 ± 0.01; mean ± SEM, two-tailed t-test, t188 = 0.595, p = 0.55), data were combined between and within sites. However, data were separated according to route of administration (injected vs drinking supply) and sex for analysis of the entire postoperative pain period (i.e. 72 h) based on the three-way interactions.
Experimental timeline outlining the pre- and postsurgical periods. For all mice, tap water was replaced with the MediDrop solution 48 hrs prior to surgery. Analgesic drugs were then added to drinking water, as appropriate, beginning 48 hrs prior to surgery. MGS baseline scores were recorded 24 h before craniotomy and at the indicated time points following surgery.
Analysis of injected analgesics
Mean difference scores for each time point (MGS postoperative time point score – MGS baseline score) were calculated as previously done14. The interaction between drug and time point was significant (two-way ANOVA, drug × repeated measures: F25,88 = 4.75, p < 0.001) and posthoc testing (one-way ANOVA at each time point) showed that buprenorphine, carprofen (25 mg/kg) and meloxicam (5 mg/kg) reduced MGS scores compared with saline control across time points within the first 24 hrs following craniotomy (4 h, F5,88 = 7.517, p < 0.001; 6 h, F5,88 = 10.63, p < 0.001; 8 h, F5,88 = 4.27, p = 0.002; 24 h, F5,88 = 5.259, p < 0.001). Carprofen (10 mg/kg; p = 0.002) and meloxicam (2 mg/kg; p < 0.001) had a slower onset, but by 6 h following craniotomy MGS scores were significantly reduced compared with control mice (Fig. 2A). No drugs reduced MGS scores at 48 h (F5,88 = 0.93, p > 0.05) or 72 h (F5,88 = 1.03, p > 0.05) postsurgery even though scores in the saline group were significantly higher than 0 at 48 h postsurgery (t15 = 2.12, p = 0.048). There were no overall sex differences for the injected analgesics (F1,82 = 0.072, p = 0.789), however, data were separated and plotted for male (Fig. 2B) and female (Fig. 2C) mice over the entire postoperative observation period.
Time course postsurgery for injected drugs. Mean difference scores are shown for carprofen (10 and 25 mg/kg), meloxicam (2 and 5 mg/kg) and buprenorphine (0.1 mg/kg) compared with saline (control) for pooled sexes (A), male mice (B), and female mice (C). Each drug has been color-coded as indicated by the legend and significance at each time point was determined by comparing with saline control. The color of the asterisks corresponds to the appropriate drug. *p < 0.05; **p < 0.01, ***p < 0.001.
Analysis of drinking supply analgesics
Mean difference MGS scores for all mice in the drinking supply groups were calculated and plotted as shown in Fig. 3A. A three-way ANOVA (sex × drug × repeated measures) revealed a main effect for drug (F5,84 = 2.82, p = 0.02), while a main effect for sex (F1,84 = 3.55, p = 0.06) and three-way interaction (F25,84 = 1.41, p = 0.087) was approaching significance. To further examine the analgesic efficacy following craniotomy, separate one-way ANOVAs were performed at each time point. None of the drugs significantly reduced MGS scores at the 4 h (F5,89 = 1.32, p = 0.26) and 6 h (F5,89 = 0.71, p = 0.62) time points. However, buprenorphine reduced MGS scores at the 8 h time point (F5,90 = 2.36, p = 0.046) and all drugs reduced MGS scores at the 24 h time point (F5,90 = 7.19, p < 0.001) compared with control mice. No further differences were detected at 48 h (F5,90 = 1.18, p > 0.05) or 72 h (F5,90 = 0.842, p > 0.05). Overall fluid consumption was not significant between drug conditions and likely not a contributing factor for differences in drug effects or lack thereof (drug × time interaction, F15,168 = 0.95, p > 0.05, Fig. 3A inset). In addition, we estimated the average drug dose (in mg/kg) ingested by each mouse and these values were not significantly different from the injected doses when compared using multiple one-sample t-tests (Table 1). As was done for the injected analgesics, data were divided and plotted according to sex (Fig. 3B,C).
Time course postsurgery for drugs added to the water supply. Mean difference scores are shown for carprofen (10 and 25 mg/kg), meloxicam (2 and 5 mg/kg) and buprenorphine (0.1 mg/kg) compared with saline (control) for pooled sexes (A), male mice (B), and female mice (C). Inset in A shows the time course of fluid consumption for mice over the postoperative monitoring period. Each drug has been color coded as indicated by the legend and significance at each time point was determined by comparing with saline control. The color of the asterisks corresponds to the appropriate drug. *p < 0.05; **p < 0.01, ***p < 0.001.
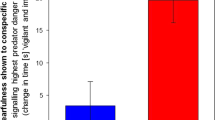
Area Under Curve Analysis
To better compare the effect of drug treatment, sex and route of administration on postcraniotomy pain, we computed a single value (area under the curve; AUC) to represent each drug over the entire postoperative period. There was a main effect for drug (F5,166 = 12.44, p < 0.001) and administration route (F1,166 = 13.88, p < 0.001), but not sex (F1,166 = 0.037, p > 0.05). However, the interaction between drug, administration route and sex was highly significant (F5,166 = 3.54, p < 0.01). As shown in Fig. 4, there were no major differences between drug treatment when administered through an injection or water supply for either sex. Additionally, carprofen had a greater analgesic effect in female mice when given via the water supply compared with the injected route (10 mg/kg, p < 0.001; 25 mg/kg, p = 0.05).
Comparison of AUC scores for control, carprofen (10 and 25 mg/kg), meloxicam (2 and 5 mg/kg) and buprenorphine (0.1 mg/kg) over the entire 72 h postoperative period compared across administration route (injected vs. water supply). Pooled sexes (A), male mice (B) and female mice (C) are shown. Comparisons were conducted between administration routes for each panel, with lower AUC scores for female mice administered carprofen through the water supply. *p < 0.05, **p < 0.01.
In order to determine whether these effects generalized to another mouse strain, we assessed the AUC of MGS scores for C57BL/6 N mice following craniotomy. We first noticed that the facial features of C57BL/6 N were more difficult to distinguish than CD-1 mice (Fig. 5). In C57BL/6 N mice, whiskers were particularly difficult to distinguish against the dark fur and were not scored. As such, orbital tightening, nose bulge, cheek bulge, and ear position were quantified and averaged to calculate the total MGS score for C57BL/6 N mice. AUC was analyzed to remove the influence of time course and directly compare drug effects and administration route. Two-way ANOVA (drug × administration route) revealed a significant main effect for drug (F5,82 = 3.38, p = 0.008), but neither administration route (F1,82 = 2.55, p = 0.11) nor the interaction (F5,82 = 1.26, p = 0.29) reached statistical significance. Carprofen (25 mg/kg) and meloxicam (5 mg/kg) significantly reduced the AUC when compared with control (Fig. 6A; Tukey’s, p < 0.05 and p < 0.01, respectively), indicating an analgesic effect. However, the degree of analgesia by carprofen or meloxicam in C57BL/6 N mice was less than CD-1 mice. This reduced analgesic effect of carprofen and meloxicam paralleled the overall lower MGS scores in the C57BL/6 N control mice compared to CD-1 mice (Fig. 6B, t45 = 5.53, p < 0.001).
Representative images and corresponding scores for CD-1 and C57BL/6 N control mice at baseline, 8 h and 48 h postcraniotomy. CD-1 images were scored using 5 action units, orbital tightening, nose bulge, cheek bulge, ear change and whisker change. All of the action units except for whisker change were scored for C57Bl/6 N due to the poor detection of whiskers in the dark colored mice.
Area under the Curve (AUC) analysis for C57BL/6 N mice. (A) AUC scores for C57BL/6 N mice that were treated with carprofen (10 and 25 mg/kg), meloxicam (2 and 5 mg/kg) and buprenorphine (0.1 mg/kg). For each condition, the scores of individual mice are presented as a dot plot with injectable analgesics indicated by the green circles and analgesics administered through the water supply as orange circles. In contrast with CD-1 mice, MGS scores for the carprofen (25 mg/kg) and meloxicam (5 mg/kg) groups were significantly lower than control mice. (B) Overall higher MGS scores were found in CD-1 control mice when compared with C57BL/6 N mice. *p < 0.05; **p < 0.01, ***p < 0.001.
Discussion
Unless postoperative pain is specifically being studied, pain control following surgery is an absolute requirement. The severity of pain following craniotomy has historically been viewed as minimal, but recent data suggests otherwise23. This makes the detection of craniotomy-related pain in animals critically important for refinement, but since species and individual responses to pain are variable, evaluation and treatment of this pain are difficult. In the present study, we used the MGS to provide evidence that spontaneous pain following craniotomy lasted upwards of 48 h and commonly used analgesics reduced this pain when administered as an injected substance or through the drinking supply. We observed statistically significant reductions in MGS scores for all drugs given through both routes of administration, however, injected analgesics were more effective in the immediate hours (4 to 8 h) after surgery. Overall no sex differences were evident between drugs, but the NSAID carprofen was more efficacious for female mice when self-administered through the drinking supply (Fig. 4). In addition, we find that MGS scores were significantly lower for C57BL/6 N mice following craniotomy, when compared with CD-1 mice and much higher doses of NSAIDS (carprofen or meloxicam) than currently recommended (Table 2) were required to reduce these scores.
In lab animals, the majority of analgesics are administered through an injectable formulation following surgery. However, recent trends and innovations have led to the development of alternative vehicles for the administration of drugs to reduce handling-related stress, such as gel formulations24, sucralose in the water supply25 or medicated pellets26. We tested MediDrop sucralose, a sweetened water gel for medication delivery (antibiotics, analgesics or experimental compounds), but did not find a clear advantage for analgesic administration following craniotomy when compared with equivalent injectable formulations – except when the NSAID carprofen was administered to female mice. Although, we did not measure serum concentration of drugs, we estimate from the consumption of water throughout the postoperative period that comparable levels of drug dosing were achieved for all mice, independent of administration route (Table 1).
Oral administration of analgesic drugs is intended to reduce the negative impact that restraint stress has on laboratory animals. Inherently, this is progressive because the stress associated with repeated physical restraint has been shown to negatively impact heart rate, body temperature, blood glucose and hormonal levels in mice (see27 for a review). In addition, restraint stress has been shown to delay cutaneous wound healing in mice28, which may increase the risk of postsurgical infection and hemorrhage. Further, there are indications that routine laboratory manipulations, including picking mice up by the tail increases their anxiety and stress responses29, while the simple presence of a male-experimenter increases corticosterone30. Thus, an effective self-administration system for analgesics would offer tremendous benefits for reducing the negative impacts associated with experimenter-mouse interactions. The MediDrop system as used here may offer advantages in drug administration, but this benefit may be small and details such as dose-response and consumption period prior to surgery need to be refined. Because rodents have a natural aversion to new foods, sucralose was added to the water two days prior to surgery, which allowed mice to habituate to the novel taste and ensured that consumption remained constant throughout the postoperative testing period. We do not believe that prolonging the presurgical sucralose consumption period would have increased analgesic efficacy because previous studies have shown that only 15 h of voluntary buprenorphine ingestion was required to reach similar or higher blood concentrations than subcutaneous administration24. Previous studies have suggested that the willingness of the animal to ingest water may enhance inter-subject variation31, but that does not apply here as there was comparable water consumption between all of our water supply groups (Fig. 3A inset). Alternative approaches have been adopted to allow mice to voluntarily ingest analgesics, such as dissolving drugs in a sticky nut and chocolate paste (i.e. Nutella®), which mice readily consume, but this is not a sustainable solution as Nutella® has a high content of fat and sugar making it undesirable as a delivery vehicle for pain studies given the impact of diet and inflammation on pain32.
We believe that the current findings represent the most thorough assessment of postoperative craniotomy pain in mice. The evaluation of different drugs, routes of administration, surgery and testing sites, mouse sex and mouse strain using the MGS as a primary output demonstrate the reliability of the MGS, but also point toward the CD-1 mouse strain as an optimal choice for analgesic drug screening using this assay. Since, we were not investigating whether MGS was able to ‘detect’ pain following surgery and all mice received the same surgical manipulation (i.e. sham craniotomy), we did not attempt to blind the coder to baseline or surgical condition. Previous studies have blinded across surgical condition, but these studies typically compared a sham vs. surgical manipulation (i.e. cervical radiculopathy), where surgical status would almost certainly impact grimace scores33. Grimace scales have shown excellent consistency in pain detection among rodents and other species11,12,14,17,21, however no single study has ever compared generalizability among experimenters, testing sites or pharmacological effects. Both the MGS and RGS (rat grimace scale) show robust inter-rater reliability, but these analyses have largely been conducted among individuals within the same test site and coding the same set of images. Given that husbandry practices may significantly alter mouse physiology and behavior, which may contribute to the lack of reproducibility in the literature, we did not make a deliberate effort to standardize practices between centers. Instead, we assessed the reliability and robustness of the MGS for craniotomy detection between centers and found no site-specific differences. This gives confidence in our results and supports the consistency of the MGS for detecting spontaneous pain following craniotomy despite differences in environmental conditions and experimental personnel. Our results were less robust for craniotomy detection when the C57BL/6 N mouse stain was used, but these mice had overall lower MGS scores than CD-1 mice.
It’s been previously reported that MGS scores – both baseline and in response to injury – differ between mouse strains. Using cage-side, clinical assessment, C57BL/6 mice were observed to have lower baseline MGS scores than CD-1 mice, which have lower MGS scores than C3H/He mice15. Further, DBA/2, but not CBA mice show an increase in MGS scores following exposure to isoflurane anesthesia, which should be considered when using the MGS to assess changes in postsurgical pain34. CD-1 mice also show a slight increase in MGS scores following isoflurane exposure, but these increases are only observed 1-hr post-anesthesia and were very modest in comparison to the changes in MGS that were associated with craniotomy observed here14. In addition, administration of common analgesics had no effect on MGS scores in the absence of postsurgical pain14,34. Moreover, as we were investigating optimal analgesic strategies for treatment of postoperative pain, we necessarily performed craniotomy surgery under isoflurane anesthesia in all groups and incorporated several test time points, from hours to days postsurgery, to evaluate analgesic efficacy. Finally, anesthetic-analgesic administration influenced measures of spontaneous postoperative pain, but only when movement was required (i.e. nest consolidation, locomotion, and grooming)35. Because MGS scores are not influenced by decreased locomotion, we believe that our current findings reflect best practices to address spontaneous pain following surgery.
Overall, our results highlight the need for postoperative analgesia following craniotomy, preferably in the form of an injected over self-administered analgesic. Further, buprenorphine provides more effective analgesia compared to commonly used NSAIDs following craniotomy.
Methods and Materials
Mice and test facilities
All experiments were approved by the appropriate animal care committees at the University of Toronto and conducted in accordance with the Canadian Council on Animal Care (CCAC) guidelines and the Ontario Animals for Research Act. Male and female CD-1 [Crl:CD1(ICR)] outbred mice (6–8 weeks of age) were tested in two different facilities. Mice tested at the University of Toronto Mississauga (Martin lab, n = 96 total) were bred in-house (n = 76) or purchased from Charles River Laboratories (n = 20). Mice tested at the University of Toronto St. George campus (Bonin Lab) were all purchased from Charles River (CD-1, n = 94; C57BL/6 N, n = 94). C57BL/6 N mice (of both sexes) were assessed by the Bonin Lab to determine whether findings in CD-1 mice were generalizable to another commonly used mouse strain. Mice bred at the University of Toronto Mississauga vivarium were housed with same-sex littermates in groups of 4–5 per cage at weaning. Prior to the start of the experiments, these mice were separated and individually housed for one-week. All mice purchased from Charles River (in both labs) were housed individually upon arrival and allowed a one-week habituation period. Both facilities were temperature controlled (20 ± 1 °C) with 12:12 h light:dark cycle and experiments were only conducted during the light period. A compressed cotton nesting square and crinkled paper bedding were provided in each cage as a source of environmental enrichment. All mice had access to food (Harlan Teklad 8604) and water ad libitum, however, water was switched to sucralose (MediDrop, Westbrook, ME) two days prior to surgery. Mice only underwent one surgery, and equal numbers of male and female mice were tested in each cohort. For the C57BL/6 N experiments, n = 4 mice per sex per group were used because no major sex differences emerged, and accurate detection of facial features was difficult in dark-colored mice, making any precise comparison between the two strains problematic.
Digital video
Mice were placed individually on a tabletop in cubicles (9 × 5 × 5 cm high) with 2 walls of transparent acrylic glass and 2 side walls of removable stainless steel. Two high-resolution (1920 × 1080) digital video cameras (High-Definition Handycam Camcorder, model HDR-CX405, Sony, San Jose, CA) were placed immediately outside both acrylic glass walls to maximize the opportunity for clear facial shots. Video was taken for 30-min before surgery (−1 day) and for 30-min periods centered around the postsurgical time points considered (4, 6, 8, 24, 48, and 72 h). For baseline videos, mice were acclimated to the cubicle for 15 min prior to recording. The videos were subsequently analyzed, and one clear facial image per mouse was taken for every three minutes of video. Image files were cropped and then copied into PowerPoint (Microsoft, Redmond, WA) with one image per slide. A PowerPoint macro (http://www.tushar-mehta.com/power-point/randomslideshow/index.htm) was used to randomize the slide order. Identifications were removed to ensure that a single, experienced experimenter (C. Cho) was blind to drug treatment, route of administration, sex and site. Average MGS scores for each mouse were then calculated by averaging individual action unit scores across the entire duration of recording for each time point and mean difference scores were obtained by subtracting baseline MGS scores from the time point following surgery. In CD-1 mice, all action units (orbital tightening, nose bulge, cheek bulge, ear position and whiskers) were scored. In C57BL/6 N mice, we did not score whiskers because they were difficult to distinguish against the dark fur of the mice, so MGS scores for these mice were the average of the other 4 action units. The brightness and contrast of all images was equally adjusted using Microsoft PowerPoint to better distinguish facial features.
Surgery
A craniotomy, designed to mimic a neurosurgical procedure, was performed under isoflurane–oxygen-anesthesia (isoflurane: induction 4%, maintenance, 1.5–2%; oxygen: maintained at 1%) Surgeons had varied degrees of surgical experience (Martin lab: C.Cho, 5+ years surgical experience, n = 16 mice; M.L., 1+ year surgical experience, n = 80 mice; Bonin lab: C.C., lab animal veterinarian, 7+ years surgical experience, n = 188) and the time of an average surgery was approximately 20 min/mouse. Following anesthesia, mice were placed in a stereotaxic frame (BenchmarkTM, myNeuroLab) and administered a bolus of saline (0.1 ml/g of bodyweight, s.c.) to prevent dehydration; mice in the injectable analgesic groups were also given their first treatment at this time. After shaving and disinfection of the surgical site, the skull was exposed following a 1.3-cm midline incision, and a 0.6 mm diameter circular craniotomy was performed over the skull region at coordinates AP = −2.46, ML = 0.55 from bregma. A needle (30 G) was then used to remove the dura from the surface of the brain taking care to avoid puncturing the brain. The scalp was then sutured (6–0 vicryl, Ethicon) and mice were allowed to recover on a 37 °C heat pad with access to water and one pellet of food. Mice were monitored until ambulatory and then transferred to the experimental behavioral room for MGS assessment. All surgeries were performed at 900 h ± 1 h with MGS images consistently captured at 4, 6, 8, 24, 48, and 72 h following surgery. All surgeons were blind to drug treatment.
Injectable Administration of Drugs
Carprofen (10 and 25 mg/kg), meloxicam (2 and 5 mg/kg), and buprenorphine (0.1 mg/kg) were obtained from CDMV (St Hyacinthe, Quebec, Canada) and dissolved in physiologic saline. Injections were given subcutaneously immediately before surgery and at 12 h time intervals following surgery. For the control group, saline injections were given at the same frequency as the drug groups and all injections were administered in a volume of 0.1 ml/g body weight. Doses were selected based on standard operating procedure and guidelines outlined by the University of Toronto, which considers craniotomy-related pain to be of mild-moderate severity. Table 2. outlines the University of Toronto dose recommendations for mouse analgesics following surgery, the preferred route of administration and frequency at which the analgesic should be administered. In most cases we selected doses at or above the upper range of these recommendations because previous studies have highlighted the inadequacy of recommended analgesic doses for treating postoperative pain in rodents14,16.
Oral Administration of Drugs
Carprofen (10 and 25 mg/kg), meloxicam (2 and 5 mg/kg), and buprenorphine (0.1 mg/kg) were dissolved in MediDrop Sucralose (https://www.clearh2o.com/research-products/medidrop/medidrop-sucralose.html) and made accessible to mice from 48 h prior to surgery. At the start of the experiment, a fixed amount of water/sucralose was given (192 ml) in a water bottle. On each day – before the start of the surgery or behavioural experiments – the remaining volume of water/sucralose was measured using a graduated cylinder. The amount of analgesic added to sucralose was calculated based on the average sucralose consumptions of naïve CD-1 males (0.38 ml/g body weight/day; n = 8) and females (0.48 ml/g body weight/day; n = 8).
Statistical analyses
All statistical analyses were performed using SPSS version 20 (SPSS, Chicago, IL), with a criterion of α = 0.05. Normality and homoscedasticity of all data sets were confirmed by using the Shapiro–Wilk and Levene tests, respectively, and thus parametric statistics were used in all cases. Time-course data were analyzed using repeated-measures ANOVA, followed where appropriate by posthoc testing for repeated measures with Sidak correction for multiple comparisons. For initial analysis, time course data were separated according to the route of administration—that is, all drugs were first compared based on administration route (i.e. injectable or water supply). In addition, data were further quantified with respect to the area under the time course curve (using the trapezoidal method) over the postoperative testing period (72 h in all cases). The area under the curve data were analyzed using either a one-, two-, or three-way ANOVA followed by Dunnett’s case-comparison posthoc test. Calculated drug doses for the oral administration groups were analyzed by one-sample Student t test, comparing the calculated with the actual injected dose of each drug. The routes of administration were directly compared for all drugs through area under the curve analysis.
Change history
25 October 2019
An amendment to this paper has been published and can be accessed via a link at the top of the paper.
References
Liu, J. et al. Syringe-injectable electronics. Nat Nanotechnol 10, 629–636 (2015).
Herman, A. M., Huang, L., Murphey, D. K., Garcia, I. & Arenkiel, B. R. Cell type-specific and time-dependent light exposure contribute to silencing in neurons expressing Channelrhodopsin-2. Elife 3, e01481 (2014).
Isosaka, T. et al. Htr2a-Expressing Cells in the Central Amygdala Control the Hierarchy between Innate and Learned Fear. Cell 163, 1153–1164 (2015).
Carr, E. C. J., Thomas, V. N. & Wilson-Barnet, J. Patient experiences of anxiety, depression and acute pain after surgery: a longitudinal perspective. Int J Nurs Stud 42, 521–530 (2005).
Pogatzki-Zahn, E. M., Segelcke, D. & Schug, S. A. Postoperative pain-from mechanisms to treatment. Pain Rep 2, e588 (2017).
Mogil, J. S. Animal models of pain: progress and challenges. Nature Reviews Neuroscience 10, 283–294 (2009).
Deuis, J. R., Dvorakova, L. S. & Vetter, I. Methods Used to Evaluate Pain Behaviors in Rodents. Frontiers in Molecular Neuroscience 10 (2017).
Rock, M. L. et al. The Time-to-Integrate-to-Nest Test as an Indicator of Wellbeing in Laboratory Mice. J Am Assoc Lab Anim 53, 24–28 (2014).
Jacobsen, K. R., Kalliokoski, O., Teilmann, A. C., Hau, J. & Abelson, K. S. P. Postsurgical Food and Water Consumption, Fecal Corticosterone Metabolites, and Behavior Assessment as Noninvasive Measures of Pain in Vasectomized BALB/c Mice. J Am Assoc Lab Anim 51, 69–75 (2012).
Navratilova, E. et al. Endogenous Opioid Activity in the Anterior Cingulate Cortex Is Required for Relief of Pain. Journal of Neuroscience 35, 7264–7271 (2015).
Langford, D. J. et al. Coding of facial expressions of pain in the laboratory mouse. Nat Methods 7, 447–449 (2010).
Sotocinal, S. G. et al. The Rat Grimace Scale: a partially automated method for quantifying pain in the laboratory rat via facial expressions. Mol Pain 7, 55 (2011).
Ekman, P., Wallace, F. Facial Action Coding System: A Technique for the Measurement of Facial Movement (1978).
Matsumiya, L. C. et al. Using the Mouse Grimace Scale to reevaluate the efficacy of postoperative analgesics in laboratory mice. J Am Assoc Lab Anim Sci 51, 42–49 (2012).
Miller, A. L. & Leach, M. C. The Mouse Grimace Scale: A Clinically Useful Tool? PLoS One 10, e0136000 (2015).
Waite, M. E. et al. Efficacy of Common Analgesics for Postsurgical Pain in Rats. J Am Assoc Lab Anim Sci 54, 420–425 (2015).
Dalla Costa, E. et al. Using the Horse Grimace Scale (HGS) to Assess Pain Associated with Acute Laminitis in Horses (Equus caballus). Animals (Basel) 6 (2016).
Holden, E. et al. Evaluation of facial expression in acute pain in cats. J Small Anim Pract 55, 615–621 (2014).
Keating, S. C., Thomas, A. A., Flecknell, P. A. & Leach, M. C. Evaluation of EMLA cream for preventing pain during tattooing of rabbits: changes in physiological, behavioural and facial expression responses. Plos One 7, e44437 (2012).
Hageri, C. et al. The Sheep Grimace Scale as an indicator of post-operative distress and pain in laboratory sheep. Plos One 12 (2017).
Reijgwart, M. L. et al. The composition and initial evaluation of a grimace scale in ferrets after surgical implantation of a telemetry probe. PLoS One 12, e0187986 (2017).
Leach, M. C. et al. The Assessment of Post-Vasectomy Pain in Mice Using Behaviour and the Mouse Grimace Scale. Plos One 7 (2012).
Chowdhury, T. et al. Perioperative Factors Contributing the Post-Craniotomy Pain: A Synthesis of Concepts. Front Med (Lausanne) 4, 23 (2017).
Hovard, A., Teilmann, A., Hau, J. & Abelson, K. The applicability of a gel delivery system for self-administration of buprenorphine to laboratory mice. Lab Anim 49, 40–45 (2015).
Marx, J. O., Vudathala, D., Murphy, L., Rankin, S. & Hankenson, F. C. Antibiotic administration in the drinking water of mice. J Am Assoc Lab Anim Sci 53, 301–306 (2014).
Molina-Cimadevila, M. J. et al. Oral self-administration of buprenorphine in the diet for analgesia in mice. Lab Anim 48, 216–224 (2014).
Balcombe, J. P., Barnard, N. D. & Sandusky, C. Laboratory routines cause animal stress. Contemp Top Lab Anim Sci 43, 42–51 (2004).
Padgett, D. A., Marucha, P. T. & Sheridan, J. F. Restraint stress slows cutaneous wound healing in mice. Brain Behav Immun 12, 64–73 (1998).
Hurst, J. L. & West, R. S. Taming anxiety in laboratory mice. Nat Methods 7, 825–826 (2010).
Sorge, R. E. et al. Olfactory exposure to males, including men, causes stress and related analgesia in rodents. Nat Methods 11, 629–632 (2014).
Jessen, L., Christensen, S. & Bjerrum, O. J. The antinociceptive efficacy of buprenorphine administered through the drinking water of rats. Lab Anim 41, 185–196 (2007).
Totsch, S. K. et al. Total Western Diet Alters Mechanical and Thermal Sensitivity and Prolongs Hypersensitivity Following Complete Freund’s Adjuvant in Mice. J Pain 17, 119–125 (2016).
Philips, B. H., Weisshaar, C. L. & Winkelstein, B. A. Use of the Rat Grimace Scale to Evaluate Neuropathic Pain in a Model of Cervical Radiculopathy. Comparative Med 67, 34–42 (2017).
Miller, A., Kitson, G., Skalkoyannis, B. & Leach, M. The effect of isoflurane anaesthesia and buprenorphine on the mouse grimace scale and behaviour in CBA and DBA/2 mice. Appl Anim Behav Sci 172, 58–62 (2015).
Oliver, V. L., Thurston, S. E. & Lofgren, J. L. Using Cageside Measures to Evaluate Analgesic Efficacy in Mice (Mus musculus) after Surgery. J Am Assoc Lab Anim 57, 186–201 (2018).
Acknowledgements
We thank Jasmine Hg, Annissa Ho, and Jerry Li for their assistance with the data organization and coding. This research was supported by the Canada Research Chairs Program (L.J.M. and R.P.B.), American College of Laboratory Animal Medicine (R.P.B), the University of Toronto Centre for the Study of Pain (R.P.B), the Research Scholars and Activity Fund, University of Toronto Mississauga (L.J.M.) and the Natural Sciences and Engineering Research Council of Canada (I.L.). Chulmin Cho was partially supported by a trainee fellowship from the University of Toronto Centre for the Study of Pain.
Author information
Authors and Affiliations
Contributions
L.J.M. and R.P.B. conceived of the project. C.Cho., V.M., I.L., C.C., M.L., M.D., C.P. and P.U. collected data. C.Cho., D.H. and L.J.M. analyzed data. L.J.M. wrote the paper with input from C.Cho., V.M. and M.L. All authors edited and commented on the paper.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cho, C., Michailidis, V., Lecker, I. et al. Evaluating analgesic efficacy and administration route following craniotomy in mice using the grimace scale. Sci Rep 9, 359 (2019). https://doi.org/10.1038/s41598-018-36897-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-36897-w
This article is cited by
-
Anesthesia and analgesia for common research models of adult mice
Laboratory Animal Research (2022)
-
Activation of locus coeruleus-spinal cord noradrenergic neurons alleviates neuropathic pain in mice via reducing neuroinflammation from astrocytes and microglia in spinal dorsal horn
Journal of Neuroinflammation (2022)
-
Distinct nociception processing in the dysgranular and barrel regions of the mouse somatosensory cortex
Nature Communications (2022)
-
Administration of meloxicam to improve the welfare of mice in research: a systematic review (2000 – 2020)
Veterinary Research Communications (2022)
-
The Role of the Possible Receptors and Intracellular Pathways in Protective Effect of Exogenous Anandamide in Kindling Model of Epilepsy
Neurochemical Research (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.