Abstract
Diabetes mellitus (DM) serves as an important prognostic indicator in patients with cardiac-related illness. Our objective is to compare survival and neurological outcomes among diabetic and non-diabetic patients who were admitted to the hospital after an out-of-hospital cardiac arrest (OHCA). We searched MEDLINE and EMBASE for relevant articles from database inception to July 2018 without any language restriction. Studies were included if they evaluated patients who presented with OHCA, included mortality and neurological outcome data separately for DM patients and Non-DM patients and reported crude data, odds ratio (OR), relative risk (RR) or hazard ratio (HR). Two investigators independently reviewed the retrieved citations and assessed eligibility. The quality of included studies was evaluated using Newcastle-Ottawa quality assessment scale for cohort studies. Random-effect models using the generic variance method were used to create pooled odds ratios (OR) and 95% confidence intervals (CI). Heterogeneity was assessed using the I2 value. Survival and neurological outcomes (using modified rankin scale and cerebral performance category scale) after OHCA in hospitalized patients with DM compared with patients without DM. Out of 57 studies identified, six cohort studies met the inclusion criteria. In an analysis of unadjusted data, patients with DM had lower odds of survival, pooled OR 0.64; 95% CI, 0.52–0.78, [I2 = 90%]. When adjusted ORs were pooled, the association between DM and survival after OHCA was still significantly reduced, pooled OR 0.78, 95% CI, 0.68–0.89 [I2 = 55%]. Unadjusted pooled OR revealed poor neurological outcomes in patients with DM, pooled OR 0.55, 95% CI, 0.38–0.80 [I2 = 90%]. The result demonstrates significant poor outcomes of in-hospital survival and neurological outcomes among DM patients after OHCA.
Similar content being viewed by others
Introduction
Sudden cardiac arrest (SCA) is reported to account for approximately 15 percent of the total mortality in the United States and other industrialized countries1. In 1999, the estimated number of sudden cardiac deaths in the United States was approximately 450,0002. Recent studies had demonstrated improved survival and neurological outcomes after cardiac arrest3. However, the opportunity to improve the outcomes after cardiac arrest remains to be explored. Most of the risk factors for coronary heart disease (CHD) are also risk factors for SCA, out of which, diabetes mellitus (DM) is considered one of the most important risk factors. Interestingly, type 2 DM patients have been reported to have a 2 to a 4-fold increased risk of out-of-hospital cardiac arrest (OHCA) compared with nondiabetic patients4. Moreover, in an observational study on OHCA, there was a statistically significant reduction in the probability of survival to hospital discharge among patients with chronic conditions, such as congestive heart failure, prior myocardial infarction, hypertension, and diabetes (odds ratio (OR) 0.84 for each additional chronic condition)5. Multiple observational studies have demonstrated an association between DM and decreased survival after OHCA. However, the studies have had varying results. Therefore, to further investigate this relationship, we conducted a systematic literature review and meta-analysis with an intention to summarize all published clinical evidence.
Methods
This study was conducted per PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) statement (Supplementary Table). A systematic literature search of MEDLINE and EMBASE was carried out from inception to July 2018 to identify original studies that investigated the association between DM and survival after OHCA. The systematic literature review was independently conducted by two investigators (DV, AC) using a search strategy that included terms for “diabetes mellitus” and “out-of-hospital cardiac arrest” in human subjects as described in the supplementary table. No language limitation was applied. The last search was performed on July 4, 2018. We contacted the study authors for additional information. Literature search details are explained in the supplementary table. A manual search for further potentially relevant studies using references of the included articles was also performed.
Inclusion criteria also included the following:
-
1.
Observational studies (cross-sectional, case-control or cohort studies) and randomized controlled trials that involved diabetic patients who presented to the hospital after surviving an OHCA.
-
2.
Studies that reported the survival after hospitalization. Hospital survival outcomes were chosen as study outcomes because, though arbitrary, in-hospital mortality will represent a reliable time point to assess short-term mortality where cardiovascular risk factors will play a predominant role. We excluded case reports and case series.
The same investigators independently reviewed the retrieved articles for their eligibility. The Newcastle-Ottawa quality assessment scale (NOS) was used to appraise the quality of included studies in 3 areas including study selection, study comparison, and determination of the outcome of interest6.
Two co-authors (DV and AC) independently extracted data from the included full-text citations. A structured data collection form was used to extract the following data from each study: title of this study, name of the first author, publication year, study dates, country where this study was conducted, number of subjects, demographic data, definition of DM, methods used to identify and verify DM, OHCA, adjusted effect estimates (odds ratio) with 95% CI and covariates that were adjusted in the multivariable analysis. A third investigator (RG) reviewed this data extraction process to ensure accuracy. All disagreements were resolved with discussion between the two abstractors. Data analysis was performed using the REVIEW MANAGER 5.3 software from the Cochrane Collaboration (London, UK). Unadjusted point estimates from each study were pooled using the inverse-variance method. Adjusted point estimates from each study were pooled using the inverse-variance weighting as described by DerSimonian and Laird, which assigned the weight of each study based on its variance7. In light of the high likelihood of heterogeneity due to different study designs, populations and definition of DM, random-effect models were used. Cochran’s Q test and the I2 statistic were used to determine the between-study heterogeneity. A value of I2 of 0–25% represents insignificant heterogeneity, 26–50% represents low heterogeneity, 51–75% represents moderate heterogeneity, and more than 75% represents high heterogeneity8. For all analyses, a P-value of <0.05 was considered statistically significant. A subgroup analysis was performed to assess the study heterogeneity by including studies which have performed robust adjustment for comorbidities (such as chronic obstructive pulmonary disease (COPD)). Sensitivity analysis was also performed to test the robustness of the output and quantify the model’s uncertainty by excluding each study one at a time. Funnel plot analysis was performed to evaluate for publication bias.
Results
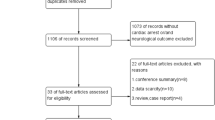
From a total of 4317 citations identified, 57 studies9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68 underwent full-length review. Of these, only 6 cohort studies47,52,57,61,66,68 were included for meta-analysis. Figure 1 delineates the study selection details. All the six included studies were performed in different parts of the world, including 2 Asian studies, 2 European studies, a study from Canada and a study from Australia. All studies are cohort studies (5 retrospective and one prospective cohort study). All the studies included participants based on the utstein guidelines. Most studies adjusted for age and gender. The 6 included studies involved 41,561 patients: 10,871 with DM and 30,690 without DM. Table 1 summarizes the included studies in our analysis.
When we pooled the results of all six studies, we found a statistically significant association between the presence of DM and survival following out-of-hospital cardiac arrests with a pooled adjusted odds ratio of 0.78, 95% confidence interval (CI) 0.68–0.89, demonstrating patients with DM had poor survival following OHCA. There was moderate heterogeneity between studies with an I2 of 55%. Figures 2 and 3 illustrate the unadjusted and adjusted forest plot of this meta-analysis. A subgroup analysis of 3 studies which performed robust adjustment of confounders (ex: COPD) resulted in a reduced heterogeneity of I2 = 0%. Table 2 illustrates the sub-group analysis which demonstrates the reduction in heterogeneity. Sensitivity analysis of included studies revealed similar outcomes with minimal variability in the pooled effect estimate. Table 2 summarizes the results of the sensitivity analysis.
Association of diabetes with survival among patients with OHCA: In this analysis, unadjusted odds ratio that quantify the association between diabetes and survival in OHCA patients was pooled from each study. The pooled odds ratio (black diamond) is 0.64 (95% CI [0.52–0.78]) indicating that diabetes is associated with poor survival.
We also found a statistically significant association between favorable neurological outcomes in patients with DM after OHCA with a pooled unadjusted odds ratio of 0.55, 95% CI 0.38–0.80. However, there was a considerable study heterogeneity among these studies with a I2 of 90%. Figure 4 illustrates the forest plot of this analysis. Subgroup analysis was not performed for this outcome because the events were crude estimates, and due to a relatively small number of included studies. Sensitivity analysis revealed that there was no statistically significant pooled estimate after excluding the study by Ro YS et al., likely due to the exclusion of a study with a relatively large sample size influencing the outcomes. Table 3 summarizes the results of the sensitivity analysis.
Figure 5 shows the funnel plot for publication bias for survival outcome after OHCA. The plot is mostly symmetric with studies mostly clustering at the apex and middle of the funnel plot. There were no studies at the bottom of the funnel plot, thus, providing a very less likelihood of publication bias.
Funnel plot for adjusted odds ratio on in-hospital survival among DM and non-DM patients after OHCA reveals a low risk for publication bias given a symmetrical distribution of the included studies (black circles) clustering at the apex around the mean effect size (middle dotted line) in the funnel plot.
Discussion
This systematic review and meta-analysis compared the survival and neurological outcomes among DM and non-DM patients who were admitted to the hospital after an out-of-hospital cardiac arrest (OHCA). To our knowledge, this is the first systematic review and meta-analysis comparing outcomes after OHCA, according to diabetes. We identified a reduced survival among patients with DM with pooled adjusted OR 0.78, 95% confidence interval (CI) 0.68–0.89. A potential explanation for lower survival among DM is because patients with DM are associated with larger myocardial infarction (MI) size and reduced reperfusion leading to higher rates of morbidity and mortality. Moreover, metabolic derangements of patients with DM after OHCA (e.g., increased blood glucose variability leading to hyperglycemia or hypoglycemia) may also contribute to lower in-hospital survival rate.
Secondly, we found that patients with DM had poor neurological outcomes (n = 19,832 patients). This is statistically relevant with an unadjusted OR 0.55 (95% CI 0.38–0.80). This is likely due to pre-existing atherosclerotic vascular disease in patients with diabetes who may be at risk for a higher degree of cerebral hypoperfusion during an episode of cardiac arrest.
Although most of the included studies were of high quality as reflected by the high-quality NOS assessment scores, we acknowledge that this meta-analysis has some limitations. Majority of the included studies did not stratify the patients based on the drugs used to treat diabetes, duration of DM and the control of glucose levels by monitoring the HbA1c levels which might have influenced the survival outcomes, and might have explained the heterogeneity among the studies. Misclassification in the diagnosis of DM may have occurred, since some patients with T2DM may be treated only with nonpharmacological therapy such as lifestyle modification. The neurological outcome data in the included studies is limited due to variability of assessment tools used to quantitate neurological outcomes (Cerebral Performance Category scale in studies by Jang et al., Van Hoeijen et al. and Ro YS et al.; and Modified Rankin scale in the study by Parry et al.). Variability in the implementation of post-cardiac arrest hypothermia protocols among the four studies that evaluated neurological outcomes can also explain the heterogeneity of these results.
In summary, this meta-analysis demonstrates significantly lower odds of in-hospital survival after OHCA among DM patients compared with non-DM patients.
Considering the limitations of the data from the included studies, our results should stimulate further research with robust strategies for risk adjustment to elucidate the association between diabetes and poor cardiac outcomes. While DM is a known risk factor for SCA, with these results, future studies are required to determine whether improved blood glucose control reduces the impact of diabetes on the survival outcomes after OHCA. Because risk factors for OHCA, SCA, and CAD are modifiable, appropriate measures to optimize health care utilization in diabetic populations may reduce this gap.
References
Zheng, Z. J., Croft, J. B., Giles, W. H. & Mensah, G. A. Sudden cardiac death in the United States, 1989 to 1998. Circulation. 104(18), 2158–2163 (2001).
State-specific mortality from sudden cardiac death–United States, 1999. MMWR Morb Mortal Wkly Rep. 51(6), 123–126 (2002)
Girotra, S. & Chan, P. S. Trends in survival after in-hospital cardiac arrest. The New England journal of medicine. 368(7), 680–681 (2013).
Balkau, B., Jouven, X., Ducimetiere, P. & Eschwege, E. Diabetes as a risk factor for sudden death. Lancet. 354(9194), 1968–1969.
Carew, H. T., Zhang, W. & Rea, T. D. Chronic health conditions and survival after out-of-hospital ventricular fibrillation cardiac arrest. Heart. 93(6), 728–731 (2007).
Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. European Journal of Epidemiology. 25(9), 603–605 (2010).
DerSimonian, R. & Laird, N. Meta-analysis in clinical trials. Controlled clinical trials. 7(3), 177–188 (1986).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. Bmj. 327(7414), 557–560 (2003).
A B, M.T B, J B, H.L T. Influence of diabetes on time of onset of life-threatening cardiac arrhythmias in a population-based study. European Heart Journal. 30, 557–558 (2009)
A H, M.J M, K.J C, A.A.J A, F K. Risk factors in patients with an out-of-hospital cardiac arrest. European Heart Journal. 30, 963–963 (2009).
A P-C, M M-S, A U. et al. Early prognostic predictors after induced hypothermia in patients with out-of-hospital cardiac arrest. European Heart Journal. 37, 973-973 (2016).
A T-K, H B-G, J M, J M, M M, W.J M. Impact of diabetes mellitus on survival in patients with end-stage renal disease: A three-year follow-up. Kidney and Blood Pressure Research. 34(2), 83–86 (2011).
A W, M L, A.L C. et al. Predictors of inhospital mortality following out-ofhospital cardiac arrest: Insights from a single-centre consecutive case series. Postgraduate Medical Journal. 92(1087), 250–254 (2016).
A.K P, R.E C, L.A M, A B, Y.C K. Hypoglycemia requiring ambulance services in patients with type 2 diabetes is associated with increased long-term mortality. Endocrine Practice. 19(1), 29–35 (2013).
A.S F, D L, J.H J, K Z, S S. Risk factors among people surviving out-of-hospital cardiac arrest and their thoughts about lifestyle. European Journal of Cardiovascular Nursing. 12, S13–S14 (2013).
B A, S E, L R, N C-S, A A. Out of hospital cardiac arrest outcomes and resource utilization in the united states: Do females fare worse? Circulation. 134 (2016).
B S, C H, M D, T E. Clinical predictors of neurologic outcome in cardiac arrest patients post induced hypothermia. Chest. 144(4) (2013).
B.C S, V S, C.M N, B R, C.N M. The predictors of outcome of out of hospital cardiac arrest in territory care center. Indian Heart Journal. 65, S18–S18 (2013).
B.D J, S DS, W M, B M. Patients with diabetes have decreased survivability with good neurological outcomes after out-of-hospital cardiac arrest. Circulation. 130 (2014).
B.D S, J.A dFN, L.B M. et al. Diabetes and cardiovascular events in high-risk patients: Insights from a multicenter registry in a middle-income country. Diabetes Research and Clinical Practice. 127, 275–284 (2017).
B.K L, K.W J, H.Y L. Predictors of neurological outcomes in out-of-hospital cardiac arrest survivors treated with therapeutic hypothermia. EMA - Emergency Medicine Australasia. 24, 29–29 (2012).
B.W W, M.D T, B W, M T. Characterization of in-hospital cardiac arrest in adult patients at a tertiary hospital in Kenya. African Journal of Emergency Medicine. 5(2), 70–74 (2015).
Barcan, A. et al. Predictors of Mortality in Patients with ST-Segment Elevation Acute Myocardial Infarction and Resuscitated Out-of-Hospital Cardiac Arrest. Journal of critical care medicine (Universitatea de Medicina si Farmacie din Targu-Mures). 2(1), 22–29 (2016).
C D, J B, K S, S B, P C. Out-of-hospital cardiac arrests in young adults in Melbourne, Australia - Adding coronial data to a cardiac arrest registry. Australasian Journal of Paramedicine. 10(2), 4–4 (2013).
C G, A M, F C, C D. In-hospital cardiac arrest: Factors in the decision not to resuscitate. the impact of an organized in-hospital emergency system. Revista Portuguesa de Cardiologia. 28(2), 131–141 (2009).
C.-H W, C.-H H, W.-T C. et al. Associations between blood glucose level and outcomes of adult in-hospital cardiac arrest: A retrospective cohort study. Cardiovascular Diabetology. 15(1) (2016).
D A, C H, A F, A C, D.S J, F H. Outcomes and predictors of in-hospital mortality in cardiac arrest patients undergoing therapeutic hypothermia without cardiac catheterization: Return of spontaneous circulation, cooling and catheterization registry (rosccc registry). Canadian Journal of Cardiology. 29(10), S274–S274 (2013).
D A, S S, T N, E R. Diabetes mellitus and the risk of sudden cardiac death: A systematic review and meta-analysis of prospective studies. Nutrition, Metabolism and Cardiovascular Diseases. 28(6), 543–556 (2018).
D Z, I A, G N, L S, G B, A P. In-Hospital outcome of patients resuscitated from out-ofhospital cardiac arrest. Giornale Italiano di Cardiologia. 13(5), 159S–159S (2012).
D.A VH, M.T B, A B, P.C S, A DB, H.L T. Reduced prehospital survival rate after out-of-hospital cardiac arrest in patients with diabetes mellitus type 2: A prospective community-based study. Circulation. 130 (2014).
D.A VH, M.T B, A B. et al. Reduced pre-hospital and in-hospital survival rates after out-of-hospital cardiac arrest of patients with type-2 diabetes mellitus: An observational prospective community-based study. Europace. 17(5), 753–760 (2015).
D.S S, N S, T.D R. et al. Type 2 diabetes mellitus and the risk of sudden cardiac arrest in the community. Reviews in Endocrine and Metabolic Disorders. 11(1), 53–59 (2010).
E A, L S, A M, F G, N N, S M. Characteristics, management and acute outcome of patients admitted following out-of-hospital cardiac arrest. Canadian Journal of Cardiology. 30(10), S86–S87 (2014).
E K, A B, S B. et al. Trends in the management and outcomes of patients admitted with acute coronary syndrome complicated by cardiogenic shock over the past decade: Real world data from the acute coronary syndrome Israeli survey (ACSIS). Oncotarget. 8(26), 42876–42886 (2017).
Eranti, A. et al. Diabetes, glucose tolerance, and the risk of sudden cardiac death. BMC Cardiovascular Disorders. 16(1) (2016).
F.A M, V.N F, B.S.B.S T. et al. Glycosylated hemoglobin is associated with decreased endothelial function, high inflammatory response, and adverse clinical outcome in non-diabetic STEMI patients. Atherosclerosis. 243(1), 124–130 (2015).
Forslund, A. S., Lundblad, D., Jansson, J. H., Zingmark, K. & Söderberg, S. Risk factors among people surviving out-of-hospital cardiac arrest and their thoughts about what lifestyle means to them: A mixed methods study. BMC Cardiovascular Disorders. 13 (2013).
Forslund, A. S. et al. Risk factors among people surviving out-of-hospital cardiac arrest and their thoughts about what lifestyle means to them: A mixed methods study. BMC Cardiovascular Disorders. 13 (2013).
G P, M C, M S. Outcomes of out of hospital cardiac arrest in patients undergoing therapeutic hypothermia. Journal of the American College of Cardiology. 63(12), A344–A344 (2014).
G S, M S, T R, R.H S. Predictors of neurologic outcome in patients treated with systemic hypothermia after successful cardiopulmonary resuscitation. European Heart Journal. 31, 645–645 (2010).
G.H M, K.B S, J.L P. et al. Temporal trends in survival of patients with and without diabetes following out-ofhospital cardiac arrest: A nationwide danish study. BMJ Open. 8, A8–A8 (2018).
H.D AM, G PB, S L-B. et al. Neurological assessment in survivors of out-of-hopital cardiac arrest who underwent therapeutic hypothermia. European Heart Journal: Acute Cardiovascular Care. 5, 163–164 (2016).
Hallstrom, A. P., Cobb, L. A. & Yu, B. H. Influence of comorbidity on the outcome of patients treated for out-of-hospital ventricular fibrillation. Circulation. 93(11), 2019–2022.
I U, W B, J S, J R. Factors affecting the occurrence of out-of-hospital cardiac arrest. European Journal of Cardiovascular Nursing. 14, 94–94 (2015).
J C, N C, N S. Determinants of death associated with out-of-hospital cardiac arrest presenting to a single tertiary referral hospital. Heart Lung and Circulation. 24, S145–S145 (2015).
J H, L E, B W. et al. Hospital mortality after out-of-hospital cardiac arrest among patients found in ventricular fibrillation. Resuscitation. 29(1), 11–21 (1995).
Jang, D. B. et al. Interaction of the diabetes mellitus and cardiac diseases on survival outcomes in out-of-hospital cardiac arrest. American Journal of Emergency Medicine. 34(4), 702–707 (2016).
K D, S B, I.R D, L.J M, M P. The association between diabetes status and survival following an out-of-hospital cardiac arrest: A retrospective cohort study. Circulation. 134 (2016).
K.G B, M.M B, F Ş. et al. Predictors of neurologically favorable survival among patients with out-of-hospital cardiac arrest: A tertiary referral hospital experience. Turk Kardiyoloji Dernegi Arsivi. 2017, 45(3), 254–260 (2017).
Kucharska-Newton, A. M. et al. Diabetes and the risk of sudden cardiac death, the Atherosclerosis Risk in Communities study. Acta Diabetologica. 47(SUPPL. 1), S161–S168 (2010).
L.L.A B, N vA, S B, J.G vdH, C.W.E H. Predictors of poor neurologic outcome in patients after cardiac arrest treated with hypothermia: A retrospective study. Resuscitation. 82(6), 696–701 (2011).
M L, A.-B T, J H, Larsson M, Thorén AB, Herlitz J. A history of diabetes is associated with an adverse outcome among patients admitted to hospital alive after an out-of-hospital cardiac arrest. Resuscitation. 66(3), 303–307 (2005).
M P, K D, S B. et al. The association between diabetes status and survival following an out-of-hospital cardiac arrest: A retrospective cohort study. Resuscitation. 113, 21–26 (2017).
M S, L.J M, D S. et al. Predictors of long-term mortality for survivors of out-of-hospital cardiac arrest. Circulation. 132 (2015).
P P, S G, S A. et al. Patients with a history of diabetes have a lower survival rate after in-hospital cardiac arrest. Resuscitation. 76(1), 37–42 (2008).
P T, M J, L F, J.D K. Diabetes Mellitus type 2 is an important risk factor for sudden cardiac arrest in patients with STEMI. European Heart Journal. 2015;36, 423–423. (2015)
Parry, M., Danielson, K., Brennenstuhl, S., Drennan, I. R. & Morrison, L. J. The association between diabetes status and survival following an out-of-hospital cardiac arrest: A retrospective cohort study. Resuscitation. 113, 21–26 (2017).
R.B D, E.D A, L.V C. et al. Diabetes mellitus and glucose as predictors of mortality in primary coronary percutaneous intervention. Arquivos Brasileiros de Cardiologia. 03(4), 323–329 (2014).
S.D S, Y.S R, Y.H K, K.J S. Association between prevalence of diabetes and incidence of out-of-hospital cardiac arrest according to age group: A nationwide case-control study. Academic Emergency Medicine. 20(5), S265–S265 (2013).
V.N F, F.C.D.S G, N.S M. et al. Diabetes mellitus unawareness is a strong determinant of mortality in patients manifesting myocardial infarction. Current Medical Research and Opinion. 29(11), 1423–1427 (2013).
Van Hoeijen, D. A. et al. Reduced pre-hospital and in-hospital survival rates after out-of-hospital cardiac arrest of patients with type-2 diabetes mellitus: An observational prospective community-based study. Europace. 17(5), 753–760 (2015).
Vyas, A. et al. Early Coronary Angiography and Survival after Out-of-Hospital Cardiac Arrest. Circulation: Cardiovascular Interventions. 8, 10 (2015).
Y.S R, S.D S, K.J S, E.J L. Interaction between diabetes and hypothermia on outcomes after out-of-hospital cardiac arrest: A nationwide observational study. Circulation. 130 (2014).
Y.S R, S.D S, K.J S. et al. Interaction effects between hypothermia and diabetes mellitus on survival outcomes after out-of-hospital cardiac arrest. Resuscitation. 90, 35–41 (2015).
Y.S R, S.D S, K.J S. et al. Risk of diabetes mellitus on incidence of outof-hospital cardiac arrests: A case-control study. PLoS ONE. 11(4) (2016).
Z N, R N, E A. et al. Effect of diabetes and pre-hospital blood glucose level on survival and recovery after out-of-hospital cardiac arrest. Critical care and resuscitation: journal of the Australasian Academy of Critical Care Medicine. 18(2), 69–77 (2016).
Zaccardi, F., Khan, H., Laukkanen, JA, F Z, H K, J.A L. Diabetes mellitus and risk of sudden cardiac death: A systematic review and meta-analysis. International Journal of Cardiology. 177(2), 535–537 (2014).
Ro, Y. S. et al. Risk of Diabetes Mellitus on Incidence of Out-of-Hospital Cardiac Arrests: A Case-Control Study. PLoS One. 11(4) (2016).
Author information
Authors and Affiliations
Contributions
Dinesh Voruganti MBBS- Conceived and designed the analysis, collected the data, contributed data or analysis tools, performed the analysis, wrote the paper; Adithya Chennamadhavuni MBBS- Conceived and designed the analysis, contributed data or analysis tools, performed the analysis, wrote the paper; Rohan Garje MBBS collected the data, contributed data or analysis tools, performed the analysis; Ghanshyam Palamaner Subash Shantha MBBS contributed data or analysis tools, wrote the paper; Marin L Schweizer Ph.D. contributed data or analysis tools, wrote the paper; Saket Girotra MD contributed data or analysis tools, wrote the paper; Michael Giudici MD Conceived and designed the analysis, contributed data or analysis tools, wrote the paper.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Voruganti, D.C., Chennamadhavuni, A., Garje, R. et al. Association between diabetes mellitus and poor patient outcomes after out-of-hospital cardiac arrest: A systematic review and meta-analysis. Sci Rep 8, 17921 (2018). https://doi.org/10.1038/s41598-018-36288-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-36288-1
This article is cited by
-
Implantable cardioverter defibrillator and cardiac resynchronization treatment in people with type 2 diabetes: a comparison with age- and sex matched controls from the general population
Cardiovascular Diabetology (2024)
-
High HbA1c is associated with decreased 6-month survival and poor outcomes after out-of-hospital cardiac arrest: a retrospective cohort study
Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine (2020)
-
Glycated Hemoglobin is Associated with Glycemic Control and 6-Month Neurologic Outcome in Cardiac Arrest Survivors Undergoing Therapeutic Hypothermia
Neurocritical Care (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.