Abstract
There is no consensus among the existing literature on the relationship between ABO blood groups and risk of Helicobacter pylori infection. However, histo-blood group carbohydrates are proposed to influence the risk of acquiring this pathogen via effects on adhesion to the gastric mucosa. The objective of this meta-analysis was to evaluate the association between ABO blood groups and H. pylori infection. All relevant epidemiological studies published in English (up to October 2017) was retrieved through an extensive systematic literature search of MEDLINE/PubMed databases. Pooled estimates of effects were obtained through the use of fixed and random effects meta-analyses. Individuals with O blood group were more likely to be infected with H. pylori (pooled odds ratio (OR) 1.163; 95% confidence interval (CI) 1.074–1.259; P < 0.001). While individuals with B and AB blood group were less likely to be infected with H. pylori (OR 0.831; 95% CI 0.738–0.935; P = 0.002 and OR 0.709; 95% CI 0.605–0.832; P < 0.001, respectively). The results from this meta-analysis of observational studies suggest an estimated 16.3% increased odds of H. pylori infection amongst individuals with the O blood group. If this observed association is causal, a better understanding of the underlying mechanisms could provide indications to potential prevention strategies for H. pylori infection.
Similar content being viewed by others
Introduction
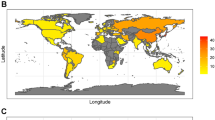
Helicobacter pylori is a Gram-negative spiral-shaped pathogenic bacterium which inhabits the human gastric mucosa. The bacterium is present in approximately half of the world’s population1,2, but it causes symptomatic disease (peptic ulcer disease and gastric malignancy) in only 10–15% of those infected3,4. In 1994, H. pylori was categorized as a class I carcinogen by the International Agency for Research on Cancer (IARC), a division of the World Health Organization (WHO) and considered to be the major risk factor of gastric cancer5. Understanding who is likely to become infected and develop disease is extremely important, especially with increasingly common antibiotic resistant strains and the lack of an effective vaccine6.
The mechanisms by which H. pylori is usually acquired and its route of transmission remain unclear, however close human contact is required. Previous epidemiological studies showed that household hygiene practices and socioeconomic status (as defined by occupation, family income level, and living conditions) are important risk factors for H. pylori infection7,8. These factors are thought to partially explain why rates of H. pylori infection vary between populations. Furthermore, a recent study showed a significant higher prevalence of H. pylori infection in sexual partners of H. pylori-infected subjects than in controls9.
Whilst most of the available literature on risk factors for H. pylori infection have focused on environmental and lifestyle factors (e.g. smoking and diet), an increasing body of evidence for the role of genetic factors in susceptibility to H. pylori infection has recently emerged10,11. One genetically determined trait with known polymorphic expression between individuals and populations that has attracted interest as potential risk factors for H. pylori infection is ABO blood group12. This premise was developed from previous studies showing a higher frequency of blood group O amongst patients with duodenal ulcer13. Since duodenal ulcer disease is associated with antral H. pylori infection in 90–100% of cases, blood group O might also be a risk factor for acquiring H. pylori infection. ABO blood groups have also been investigated as risk factors for H. pylori associated gastric cancer, however there are conflicting studies due to multiple confounding effects14. Since the discovery of the ABO blood group, there has been an ongoing interest in the potential role of blood groups in infectious disease. Blood group antigens are receptors for toxins, parasites, and bacteria, where they can facilitate colonization or invasion or evade host clearance mechanisms15. Previous studies demonstrated that blood-group antigen-binding adhesion (BabA) mediate adherence of H. pylori to human Lewisb (α-1,3/4-difucosylated) blood-group antigens on gastric epithelial cells16,17.
During the last few decades, evidence for the role of ABO groups as potential risk factors for H. pylori infection has emerged from animal model studies and epidemiological data18,19,20. H. pylori infection was found in some studies to be positively associated with O blood group18,21, whilst others found no correlations19,20,22,23.
Meta-analysis is a well-established method that pools data from smaller inconclusive studies to provide greater statistical power24. Therefore, the current systematic review and meta-analysis of the relevant epidemiologic literature aims to quantify the association between ABO blood group and H. pylori infection status.
Methods
Literature search and study selection
Comprehensive inclusion and exclusion criteria were pre-defined and then used to objectively identify relevant epidemiological studies in MEDLINE/PubMed databases (up to October 2017). The studies had to satisfy the following requirements: (i) published in English; (ii) cross-sectional, cohort, case–control study, or randomized controlled trial; (iii) ABO blood groups were defined using the slide method, tube test, microplate technology, column/gel centrifugation, surface imprinting of erythrocytes, use of synthetic and natural receptors for ABO blood group sensors, chromatography and filtration paper based diagnostics, and any other molecular blood typing methods, (iv) H. pylori infection was determined using a stool antigen test, serum H. pylori-specific IgG using ELISA, 13C- or 14C-labelled urea breath test, antral biopsy urease test, microbiological culture methods or histological identification of organisms, hematoxylin and eosin (HE) staining, or Giemsa staining. Reviews, letters, correspondences, editorials, and case reports were excluded from analysis. Two researchers (ZC and BT) independently evaluated the eligibility of studies using a three-step process starting with examination of titles, then paper abstracts, and ultimately full-texts. References were also reviewed to determine new qualified studies. Relevant papers were imported using the EndNote X7 software (Thomson Reuters Corporation, New York, NY, USA).
Study quality assessment
The Newcastle–Ottawa quality assessment scale (NOS) was adapted to observational studies and used to evaluate their quality25. Three factors were considered when determining a quality score: selection of the study groups; comparability of groups; and ascertainment of the exposure and outcomes. High quality studies were considered to have a score of 7 or greater out of 10 for cross-sectional and cohort studies.
Statistical analysis
Comprehensive Meta-Analysis (CMA; version 3) was used to analyze reported odds ratios (ORs) and 95% confidence intervals (CIs) for the association between ABO blood groups and H. pylori infection status. Studies with reported raw data required calculation to retrieve ORs and CIs. ABO blood group outcomes were used for primary analysis. Relative risk was measured as OR in all studies and adjusted ORs were preferred to crude ORs. A random study effects model, accounting for heterogeneity, was used to combine study individual effect estimates. Cochran Q and I2 statistics were used to evaluate heterogeneity. Cochran Q with a P value <0.10 was considered to be statistically significant for heterogeneity. A value >50% for I2 was considered to have severe heterogeneity26. Asymmetry in funnel plots of study ORs versus the standard error of logarithm of these ORs were used to assess publication/selection bias. Egger’s regression asymmetry test was used to evaluate the degree of asymmetry27. Sensitivity analyses were performed to assess the impact and influence of individual studies on overall pooled estimates28,29.
Subgroup analyses were completed subsequent to the primary analysis according to study quality (low or high), study design and study area (developed and developing). The current meta-analysis and review was performed in accordance to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA)30 and Meta-analysis of Observational Studies in Epidemiology group (MOOSE)31.
Results
Study characteristics
The comprehensive search of relevant literature yielded 2222 potentially relevant studies. Full texts of 91 papers were retrieved after title and abstract examination steps (Fig. 1). Of the 91 papers, 30 were considered eligible and presented relevant data for the meta-analysis (Fig. 1).
Of the 30 eligible studies, twenty-seven were cross-sectional in, two were cohort studies, and one used a randomized control trial design. The majority of the studies included adults aged between 18 and 74 years; only two studies were performed in children under 15 years old. The 30 studies included a total of 12,708 individuals (Table 1).
H. pylori was defined using an enzyme-linked immunosorbent assay (ELISA) in ten studies, histological analysis of hematoxylin and eosin (HE) stained gastric tissue sections in two studies, a urea breath test in four studies, and a combination of ELISA, antral biopsy urease test, and Giemsa staining of histological sections in two studies. The remaining 12 studies used various other techniques to define H. pylori. The majority of the included studies determined ABO type via serum hemagglutination methods. These methods are sufficiently standard and widely used in large-scale blood banking (Table 1).
Quality assessment
Of the 30 eligible studies, 26 were considered to be of higher methodological quality (score ≥ 7) and 3 were considered to be of lower quality due to an insufficient characterization of control populations, failure to report response rates, or lack of adjustment for confounding variables. In a range of 6–8, the median overall score was 7, which demonstrates the studies to be of generally high quality (Table 1).
Association between O Blood groups and H. pylori infection
The meta-analysis of findings from 30 studies on the association between O blood group and H. pylori infection (Fig. 2) demonstrated an increased odds of H. pylori infection compared to non-O blood group (OR; 1.163; 95% CI; 1.074–1.259, P < 0.001). Sixteen of the 30 studies independently reported an OR greater than or equal to 1. Although most of the studies found a positive association between O blood group and H. pylori (Fig. 2), there was substantial heterogeneity (I2 = 85.52%) in estimated effect size between the studies suggesting that systematic effect size variability was unaccounted for. Thus, factors associated with the studies themselves (e.g., quality of the study, study design) and participant characteristics (e.g. place of residence or age) may have moderated the overall results. We therefore conducted subgroup analyses to determine the extent to which these variables moderated the overall results. In a subgroup analysis, O blood group was also significantly associated with H. pylori infection (OR = 1.268: 95% CI 1.141–1.409, P < 0.001) when the data pool was restricted to seventeen studies that were conducted in a developing country, whilst the pooled OR for the twelve studies conducted in a developed country was weaker and not statistically significant (OR = 1.071, 95% CI; 0.944–1.214, P = 0.984; Fig. S1). Findings did not substantially change when the analysis was concentrated on the 26 high-quality studies (OR = 1.157, 95% CI 1.067–1.254; P < 0.01; Fig. S2).
Meta-analysis of the association between O blood group and H. pylori infection. For each study, the box represents the fixed and random effects odds ratio and the line the 95% confidence intervals. The size of each box indicates the relative weight of each study in the meta-analysis. Test for overall fixed and random effects: z = 3.731, P < 0.001, I2 = 85.52, P < 0.001; z = 1.818, P = 0.069, respectively.
The 27 cross-sectional studies resulted in a pooled OR of 1.185 (95% CI; 1.091–1.286; P < 0.01), Fig. S3). Publication bias did not appear to play a role in the association between blood group O and H. pylori infection since no clear deviations from symmetry was observed in the funnel plot (Fig. 3). The Egger regression asymmetry test also demonstrated no statistically significant publication biases (Egger’s test; b = 0.802, P = 0.486). Furthermore; robustness of the observed outcome was investigated by sequentially removing each study and re-analyzing the data sets and no study was shown substantially alter the pooled OR estimate (Supplement Fig. S4).
Association between B Blood group and H. pylori infection
The meta-analysis of findings from 27 studies on the association between B blood group and H. pylori infection (Fig. 4) demonstrated a slightly decreased odds of H. pylori infection (OR = 0.831 (95% CI; 0.738–0.935, p = 0.002). Eighteen of the 27 studies independently reported an OR less than 1, and evidence of substantial heterogeneity was observed (I2 = 62.31). A subgroup analysis of sixteen studies from a developing country produced a summary risk estimate of 0.741 (95% CI 0.633–0.868, P < 0.001, Fig. S5). Further stratified analysis by study quality and study design did not materially alter the size of pooled estimate: with 23 high-quality studies (OR = 0.850, 95% CI 0.752–0.959; P = 0.009; Fig. S6), and 24 cross-sectional studies (OR of 0.819 (95% CI; 0.723–0.927; P = 0.002; Fig. S7). There was no evidence of publication bias on both visual inspections of the funnel plot (Fig. 5) and from the result of Egger’s test (Egger’s test; b = −0.221, P = 0.792). Furthermore, a sensitivity analyses was completed by sequentially removing each study and re-analyzing the data sets provided a nearly identical risk estimate (Supplement Fig. S8).
Association between AB Blood group and H. pylori infection
The meta-analysis of findings from 27 studies on the association between AB blood group and H. pylori infection (Fig. 6) demonstrated decreased odds of H. pylori infection (OR:0.709; 95% CI; 0.605–0.832, p < 0.000), and there was moderate heterogeneity across studies (I2 = 49.2%). The findings from the subgroup analyses based on different methodological criteria did not materially alter the size of pooled estimates (OR:0. 601 (95% CI 0.492–0.735, P < 0.001; 16 studies from developing country; Fig. S9, OR = 0.692, 95% CI 0.586–0.816; P < 0.01 in 23 high quality studies; Fig. S10, and OR = 0.697; 95% CI; 0.591–0.822; P < 0.01 in 24 cross sectional studies Fig. S11). No significant deviations from symmetry were observed in the funnel plot that might suggest evidence of publication bias (Fig. 7). No statistical significant publication bias was also shown by the Egger regression asymmetry test (Egger’s test; b = 0.775, P = 0.172). Robustness of the observed outcome was investigated by sequentially removing each study and re-analyzing the data sets leading to no substantial alteration to the pooled OR estimate by any single study (Fig. S12).
Association between A Blood groups and H. pylori infection
Figure 8 shows an overall pooled OR for the association between A blood group and H. pylori infection. No evidence was found suggesting that individuals with A blood group significantly associated with risk of H. pylori infection (OR = 1.041; 95% CI; 0.958–1.132, p = 0.340). There was also evidence of substantial heterogeneity (I2 = 74.68), however, symmetry was observed in the funnel plot, indicating no publication bias (Fig. 8). Furthermore, No statistical significant publication bias was also shown by the Egger regression asymmetry test (Egger’s test; b = 0.80198, P = 0.486). A subgroup analysis analyses based on different methodological criteria did not materially alter the size of pooled estimates (Data not shown). No single study substantially altered the pooled OR estimates in the sensitivity analysis (Data not shown).
Association between Rh Blood group and H. pylori infection
Figure 9 shows an overall pooled OR for the association between Rh blood group and H. pylori infection. Overall, Rh positive was associated with non-significant reduction risk in H. pylori infection (pooled OR 0.804 (95% CI 0.614–1.053). There was evidence of heterogeneity (P < 0.0001), with a moderate proportion of the total variation in the estimated effect due to between-study heterogeneity (I2 = 31.9%).
Association between secretor status and H. pylori infection
Nine studies reported secretor status (secretors belong to Lewis (Le)(a-b+) and those who are non- secretors to Le (a-b−) histo-blood group phonotype). The pooled analysis showed a slightly higher odds of H. pylori infection among secretors compared to non-secretors (OR = 1.140 (95% CI; 0.882–1.472, p = 0.317) (Fig. 10). Five of the 9 studies individually reported an OR greater than 1, and evidence of minimum heterogeneity was observed (I2 = 18.157, P = 0.184.). There was no evidence of publication bias on both visual inspections of the funnel plot (Fig. S13) and from the result of Egger’s test (Egger’s test; b = 1.0672, P = 0.441). Sensitivity analyses indicated that there was little evidence to suggest that the pooled odds ratio was influenced by any single study (Data not shown).
Discussion
We believe that this is the first meta-analysis that investigates the association between ABO blood group and H. pylori infection. Our meta-analysis of 30 eligible studies consisting of more than 12,000 individuals showed O blood group to be associated with an estimated 16.3% increase in probability of H. pylori infection than non-O blood group, which was highly statistically significant. Whilst, blood group B and AB were found to be associated with an estimated 17% and 29% reduction in odds of H. pylori infection compared with non-B, non-AB, respectively, also highly statistically significant. The results did not vary much from the overall association when observing study area (developing and developed countries), study quality, or study design. No evidence of publication bias was found on both visual inspections of the funnel plot and from the result of Egger’s test. However, there was moderate to substantial heterogeneity in the estimated effect size between studies suggesting that systematic effect size variability was unaccounted for. Thus, factors associated with the studies themselves (e.g. quality of the study, study design) and participant characteristics (e.g. place of residence, age) may have moderated the overall results. Our subgroup analysis, however, did not materially alter the size of pooled estimates. We observed a limited change in association regardless of study quality, study design or study area. Our meta-analysis found no evidence that A and Rh blood group groups significantly associated with risk of H. pylori infection. We attempted to perform potential disease subgroup analyses, however there was an insufficient number of epidemiological papers to see the relationship between H. pylori and ABO amongst PUD or gastric cancer compared to NUD. Further studies are needed in this area in order to clarify the impact of blood groups on disease risk.
Our findings should be interpreted in light of the following limitations. First, caution is warranted in the overall estimates provided in this meta-analysis, as there was significant heterogeneity. The lack of any explanation for this heterogeneity, apart from method of exposure and outcome assessments and possibly variation in the populations studied, suggests that methodological variations that we were not able to test may have been important. An alternative approach would be individual participant meta-analysis, as it would provide some consistency across the potentially mediating characteristics. Although, a high statistical heterogeneity across the studies still limiting the interpretation of the pooled estimate, the subgroup analysis, as well as sensitivity analysis, showed that results from our meta-analysis was robust. Second, because this meta-analysis was based on observational studies, our results were prone to selection bias inherent in the included studies. In addition, the potential confounding from other risk factors could not be ruled out, especially when considering that some studies only reported crude risk estimated without adjustments. Third, by narrowing our studies to only those of the English language, it is possible that some suitable studies published other languages may have been missed. Although, we did not find evidence of publication bias on both visual inspections of the funnel plot and from the result of Egger’s test, it might still be possible that some unpublished studies may have been missed.
A major strength of this review was the comprehensive search strategy in the PubMed database used to identify relevant studies. Furthermore, to reduce the possibility of missing eligible studies, reference lists of retrieved papers were checked. Additionally, study eligibility was meticulously assessed by an independent reviewer and further evaluated by an additional independent reviewer when necessary. Most of the eligible studies were considered of high methodological quality and outcomes were consistent after excluding studies of lower quality. Specific inclusion criteria were used regarding the method of ascertainment and other facets, effectively reducing reporting bias that may emerge from use of a subjective self-reported method. Our eligibility criteria required that the outcome of interest, H. pylori infection, be objectively measured. The majority of studies used ELISA tests to inexpensively and noninvasively detect anti-H. pylori IgG antibodies to define H. pylori infection. For ABO phenotype determination, most of the included studies used standard hemagglutination methods that have been in clinical use for the major blood types for a century32 and on which blood banking relies. Furthermore, the meta-analysis exhibits high statistical power through its use of 30 studies and over 12,000 individuals.
The underlying mechanism for the relationship between ABO blood group and H. pylori infection has been proposed from previous biochemical studies in ABO, Lewis and Secretor histo-blood system17,33. Individuals from O blood group carrying the secretor phenotype converts the precursor oligosaccharide type 1 into H antigen type 1 but due to the absence of GTA and or GTB glycosyltransferases they are unable to synthesize A or B antigens. Therefore, they convert H type 1 antigen into Leb antigen in Lewis positive individuals (90% of the population). The high quantitative expression of this antigen in the gastric and duodenal mucosae of O blood group individuals carrying the secretor phenotype seems to increase the susceptibility to infection by H. pylori by providing a greater number of receptors for this microorganism17. The increase risk of H. pylori infection among individuals with O blood group, but not in non-O blood group (A, B, AB) in this meta-analysis fit with the aforementioned proposed biological mechanisms. Furthermore, the tendency of higher risk of H. pylori infection among secretor compared to non-secretor in our study fits with the early hypothesis proposed by Borén et al.17 in which bacteria choose to attach itself to the Lewis b antigen (Leb), which is rich in fucose and is expressed on the surface of the epithelial cells of the gastric mucosa17. Most of the included studies in our analysis did not provide secretor frequencies in each A, B, O individuals, however studies documented that O and Le (a-b+) phenotypes express a greater quantity of these fucosylated antigens in comparison with other groups which in turn predispose these carriers to H. pylori infection17,34, and influence the development of H. pylori associated complication. Although most epidemiological studies failed to report data on specific strains of H. pylori in relation to ABO group, experimental evidence has shown strain-dependent preference of BabA adhesin(s) in binding to MUC5AC glycoforms substituted with Leb which may contribute interindividual variability in host-microbe interactions35.
In conclusion, this meta-analysis provides evidence that O blood group is associated with increased risk of H. pylori infection compared to non-O blood group. However, high quality cohort studies are necessary to ascertain causality, which may significantly aid in understanding the pathogenesis of H. pylori infection and discover potential preventative strategies. For instance, if the association between O blood type and H. pylori infection is confirmed by further controlled studies, O blood group status may be listed as one of H. pylori risk factors, and ABO blood typing may hence become part of a multifaceted strategy for H. pylori risk assessment.
References
Megraud, F., Brassens-Rabbe, M. P., Denis, F., Belbouri, A. & Hoa, D. Q. Seroepidemiology of Campylobacter pylori infection in various populations. J Clin Microbiol. 27(8), 1870–3 (1989).
Go, M. F. Review article: natural history and epidemiology of Helicobacter pylori infection. Alimentary pharmacology & therapeutics. 16(Suppl 1), 3–15 (2002).
Ernst, P. B. & Gold, B. D. The disease spectrum of Helicobacter pylori: the immunopathogenesis of gastroduodenal ulcer and gastric cancer. Annu Rev Microbiol. 54, 615–40 (2000).
Uemura, N. et al. Helicobacter pylori infection and the development of gastric cancer. N Engl J Med. 345(11), 784–9 (2001).
Schistosomes, liver flukes and Helicobacter pylori. IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Lyon, 7–14 June 1994. IARC monographs on the evaluation of carcinogenic risks to humans. 61, 1–241 (1994).
Safavi, M., Sabourian, R. & Foroumadi, A. Treatment of Helicobacter pylori infection: Current and future insights. World journal of clinical cases. 4(1), 5–19 (2016).
Graham, D. Y. et al. Epidemiology of Helicobacter pylori in an asymptomatic population in the United States. Effect of age, race, and socioeconomic status. Gastroenterology. 100(6), 1495–501 (1991).
Malaty, H. M., Evans, D. G., Evans, D. J. Jr. & Graham, D. Y. Helicobacter pylori in Hispanics: comparison with blacks and whites of similar age and socioeconomic class. Gastroenterology. 103(3), 813–6 (1992).
Sgambato, D. et al. Prevalence of Helicobacter pylori infection in sexual partners of H. pylori-infected subjects: Role of gastroesophageal reflux. United European Gastroenterology Journal. 0(0), 2050640618800628.
Hamajima, N. Persistent Helicobacter pylori infection and genetic polymorphisms of the host. Nagoya journal of medical science. 66(3-4), 103–17 (2003).
Malaty, H. M., Engstrand, L., Pedersen, N. L. & Graham, D. Y. Helicobacter pylori infection: genetic and environmental influences. A study of twins. Annals of internal medicine. 120(12), 982–6 (1994).
Rossez, Y. et al. Almost all human gastric mucin O-glycans harbor blood group A, B or H antigens and are potential binding sites for Helicobacter pylori. Glycobiology. 22(9), 1193–206 (2012).
Clarke, C. A. et al. ABO blood groups and secretor character in duodenal ulcer; population and sibship studies. British medical journal. 2(4995), 725–31 (1956).
Oh, S. et al. Effect of Helicobacter pylori Eradication and ABO Genotype on Gastric Cancer Development. Helicobacter. 21(6), 596–605 (2016).
Cooling, L. Blood Groups in Infection and Host Susceptibility. Clinical microbiology reviews. 28(3), 801–70 (2015).
Boren, T., Normark, S. & Falk, P. Helicobacter pylori: molecular basis for host recognition and bacterial adherence. Trends in microbiology. 2(7), 221–8 (1994).
Boren, T., Falk, P., Roth, K. A., Larson, G. & Normark, S. Attachment of Helicobacter pylori to human gastric epithelium mediated by blood group antigens. Science (New York, NY). 262(5141), 1892–5 (1993).
Kanbay, M., Gur, G., Arslan, H., Yilmaz, U. & Boyacioglu, S. The relationship of ABO blood group, age, gender, smoking, and Helicobacter pylori infection. Digestive diseases and sciences. 50(7), 1214–7 (2005).
Niv, Y. et al. Helicobacter pylori infection and blood groups. The American journal of gastroenterology. 91(1), 101–4 (1996).
Loffeld, R. J. & Stobberingh, E. Helicobacter pylori and ABO blood groups. Journal of clinical pathology. 44(6), 516–7 (1991).
Henriksson, K., Uribe, A., Sandstedt, B. & Nord, C. E. Helicobacter pylori infection, ABO blood group, and effect of misoprostol on gastroduodenal mucosa in NSAID-treated patients with rheumatoid arthritis. Digestive diseases and sciences. 38(9), 1688–96 (1993).
Dickey, W., Collins, J. S., Watson, R. G., Sloan, J. M. & Porter, K. G. Secretor status and Helicobacter pylori infection are independent risk factors for gastroduodenal disease. Gut. 34(3), 351–3 (1993).
Ayalew, F., Tilahun, B. & Taye, B. Performance evaluation of laboratory professionals on malaria microscopy in Hawassa Town, Southern Ethiopia. BMC Res Notes. 7, 839 (2014).
Louis, T. A., Fineberg, H. V. & Mosteller, F. Findings for public health from meta-analyses. Annual review of public health. 6, 1–20 (1985).
Wells, G. S. B. et al. Newcastle-Ottawa scale (NOS) for assessing the quality of non randomised studies in meta-analysis Available from, http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm.
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. Bmj. 327(7414), 557–60 (2003).
Egger, M., Davey Smith, G., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. Bmj. 315(7109), 629–34 (1997).
Steichen, T. Tests for publication bias in meta-analysis. Stata Tech Bull. 41(sbe19), 9–15 (1998).
Steichen, T., Egger, M. & Sterne, J. Tests for publication bias in meta-analysis. Stata Tech Bull. 44(sbe19.1), 3–4 (1998).
Moher, D., Liberati, A., Tetzlaff, J. & Altman, D. G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. International journal of surgery (London, England). 8(5), 336–41 (2010).
Stroup, D. F. et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. Jama. 283(15), 2008–12 (2000).
Bond, C. J. On auto-haemagglutination: a contribution to the physiology and pathology of the blood. British medical journal. 2(3129), 925–7 (1920).
Aspholm-Hurtig, M. et al. Functional Adaptation of BabA, the H. pylori ABO Blood Group Antigen Binding Adhesin: American Association for the Advancement of Science. 519–22 p.
Jaff, M. S. Higher frequency of secretor phenotype in O blood group - its benefits in prevention and/or treatment of some diseases. International journal of nanomedicine. 5, 901–5 (2010).
Linden, S. et al. Strain- and blood group-dependent binding of Helicobacter pylori to human gastric MUC5AC glycoforms. Gastroenterology. 123(6), 1923–30 (2002).
Acknowledgements
We thank Colgate University library system for all of their help and resources.
Author information
Authors and Affiliations
Contributions
B.T. conceived and designed the study and wrote this manuscript. Z.C. and B.T. searched database and reviewed studies. Z.C. performed data analysis and prepare the initial draft of the manuscript. K.R. participated in interpretation of data, helped in drafting the manuscript and critically reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chakrani, Z., Robinson, K. & Taye, B. Association Between ABO Blood Groups and Helicobacter pylori Infection: A Meta-Analysis. Sci Rep 8, 17604 (2018). https://doi.org/10.1038/s41598-018-36006-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-36006-x
Keywords
This article is cited by
-
ABO, Lewis blood group systems and secretory status with H.pylori infection in yemeni dyspeptic patients: a cross- sectional study
BMC Infectious Diseases (2023)
-
The immune microenvironment in gastric adenocarcinoma
Nature Reviews Gastroenterology & Hepatology (2022)
-
Correlation between CT chest severity score (CT-SS) and ABO blood group system in Egyptian patients with COVID-19
Egyptian Journal of Radiology and Nuclear Medicine (2021)
-
Blood group AB increases risk for surgical necrotizing enterocolitis and focal intestinal perforation in preterm infants with very low birth weight
Scientific Reports (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.