Abstract
CD80, which regulates T cell activation, may provide a differential diagnostic marker between minimal change disease (MCD) and other renal diseases, including focal segmental glomerular sclerosis (FSGS). However, recent reports show contrasting results. Therefore, we evaluated the utility of urinary CD80 as a diagnostic biomarker. We collected 65 urine samples from 55 patients with MCD (n = 31), FSGS (n = 4), inherited nephrotic syndrome (n = 4), Alport syndrome (n = 5) and other glomerular diseases (n = 11), and control samples (n = 30). We measured urinary CD80 levels by ELISA. Urinary CD80 (ng/gCr) (median, interquartile range) levels were significantly higher in patients with MCD in relapse (91.5, 31.1–356.0), FSGS (376.2, 62.7–1916.0), and inherited nephrotic syndrome (220.1, 62.9–865.3), than in patients with MCD in remission (29.5, 21.7–52.8) (p < 0.05). Elevation of urinary CD80 was observed, even in patients with inherited nephrotic syndrome unrelated to T cell activation. Additionally, urinary CD80 was positively correlated with urinary protein levels. Our results suggest that urinary CD80 is unreliable as a differential diagnostic marker between MCD in relapse and FSGS or inherited kidney diseases. Increased urinary CD80 excretion was present in all patients with active kidney disease.
Similar content being viewed by others
Introduction
Nephrotic syndrome (NS) is clinically characterized by massive proteinuria with hypoalbuminemia, accompanied by systemic oedema. These clinical changes are correlated with specific structural changes in the foot processes of glomerular visceral epithelial cells, podocytes, which form the glomerular filtration barrier1,2. NS is categorized into primary diseases of idiopathic NS, such as Minimal Change Disease (MCD) and Focal Glomerulosclerosis (FSGS), and secondary diseases associated with drugs, infection or genetic defects, i.e., inherited NS3.
In MCD, the most common cause of NS in children, the activation of T cells may be related to injuries of the glomerular filtration barrier, including podocytes, for the following reasons:4 (i) remission of MCD is caused by diseases and drugs leading to the inactivation of T cells, such as measles, steroids, and cyclosporine; (ii) Hodgkin’s diseases associated with T-cell activation often cause secondary MCD.
However, in inherited NS, variants of podocyte-related genes are linked, directly or indirectly, to specific defects of podocytes5; most patients with deleterious variants of these genes show significantly lower response to immunosuppressive therapy, or entirely lack a response to such therapy6,7. This suggests that inherited NS is not associated with T-cell activation.
CD80 is a transmembrane protein which is expressed on antigen-presenting cells or natural killer cells. It works as a ligand, playing important roles in T-cell activation and inactivation by binding to CD28 on T cells or cytotoxic T-lymphocyte-associated-4 (CTLA-4) on Tregs8. Gene expression of CD80 is upregulated by allergens and irritants in human keratinocytes, or by oxidative stress in mastocytoma tumour cells9,10. Recently, some groups reported CD80 expression in glomerular podocytes in MCD patients in relapse, as well as in podocytes cultured with serum in the relapse phase of MCD. In addition, CD80 was not present in podocytes from patients with MCD in remission, or patients with FSGS11,12. Notably, urinary CD80 was elevated in patients with MCD in relapse, but not in patients in remission or with FSGS13. From these results, it was hypothesized that the level of urinary CD80 was useful as a biomarker to distinguish between MCD patients in relapse and other renal diseases, including FSGS13.
However, more recent reports have shown different results for the expression of CD80 on podocytes. Reiser et al. reported that CD80 was expressed on podocytes in patients with various diseases: MCD in relapse, FSGS, SLE, and even inherited diseases14. In contrast to this report, Larsen et al. and Novelli et al. reported that CD80 was not found on podocytes in either MCD in relapse or FSGS15,16. Thus, the specificity of expression of CD80 on podocytes in MCD remains controversial15,17. Moreover, the usefulness of urinary CD80 levels as a differential diagnostic marker for patients with MCD has not been fully examined.
The present study was performed to determine the utility of urinary CD80 measurement for the differential diagnosis of patients with various renal diseases. We recruited patients with MCD, FSGS, and other glomerular diseases, including inherited renal diseases that are not associated with T-cell activation.
Results
Patient characteristics
The clinical characteristics of each group are shown in Table 1. There were statistically significant differences in urinary protein/creatinine between MCD in remission and MCD in relapse, FSGS, or inherited NS.
Precision of our ELISA
We produced a standard curve for CD80 with commercially quantified CD80 protein (Cat. No. 10698-H08H, Sino Biological Inc.) (Supplemental Fig. 1). In addition, we also produced a standard curve with an ELISA kit (Bender MedSystems, Burlingame, CA, USA) used in previous reports13,18, as a comparison with our ELISA method. Both ELISAs displayed a linear correlation between CD80 concentration and OD450; the correlation coefficient of our ELISA was higher than that of the established ELISA kit.
Urinary CD80 excretion
The CD80 (ng/gCr) levels in urine were significantly higher in patients with MCD in relapse (91.5, 31.1–356.0), FSGS (376.2, 62.7–1916.0) or inherited NS (220.1, 62.9–865.3) than in patients with MCD in remission (29.5, 21.7–52.8) (p < 0.05) (Fig. 1). Two of four patients with FSGS and one of four patients with inherited NS showed much higher urinary CD80 than 75th percentile of CD80 in patients with MCD in relapse (2337.6, 651.5, and 1038.1 ng/gCr, respectively). There was no significant difference in urinary CD80 level between patients with MCD in remission and controls (59.9, 48.6–72.5). There were no significant differences in urinary CD80 levels among patients with MCD in relapse, FSGS, or inherited NS. To investigate whether elevated urinary CD80 in MCD in relapse has specificity for other renal diseases, we compared urinary CD80 values between MCD in relapse and all renal diseases other than MCD. Notably, no differences in urinary CD80 were found between MCD in relapse and other renal diseases (Supplemental Fig. 2).
Correlation between CD80 values in serum and urine
The relationship between serum CD80 and urinary CD80 was examined in 15 patients, but no correlation was found (r = 0.07, p = 0.80) (Fig. 2). Serum CD80 remained at a normal value (20–320 pg/ml)19, even in patients who exhibited high values, such as urinary CD80 exceeding 1000 ng/gCr.
Correlation between serum and urinary CD80. Serum and urine samples collected at the same time points were measured in 15 patients, including 11 with MCD in relapse, one with FSGS, and three with other renal diseases. Most samples remained in the normal range (155, 70–197 pg/ml); no correlation was found between serum and urinary CD80 (r = 0.07, p = 0.80).
Correlation between urinary CD80 and urinary protein
A positive correlation was found between urinary CD80 levels and the urine protein/creatinine ratio in total subjects (r = 0.57, p < 0.0001) (Fig. 3).
In each group, there were wide variations in urinary CD80 concentration, reflected by wide error bars (Fig. 1). Therefore, we studied the correlation between urinary CD80 and urinary protein in each group. First, we calculated the 97.5th percentile of the control group and determined that the normal range of urinary CD80 lies below 105.1 ng/gCr. Values greater than the 97.5th percentile of control were defined as high. The remaining subjects in each group were defined to exhibit normal CD80 levels. Then, we compared the amounts of urinary protein in these two groups, according to each renal disease. There were significant differences between the high and low groups in MCD in relapse, and for the group of all renal diseases (Supplemental Fig. 2). Although the same tendency was observed between inherited NS and FSGS, a significant difference was not detected because of the small sample size.
Discussion
In this study, we evaluated the concentration of urinary CD80 of 65 samples from 55 patients with various renal diseases, including inherited diseases, to determine the utility of urinary CD80 as a diagnostic biomarker. Among these 65 samples, 20 were collected from 10 patients at different two points of NS (remission and relapse). The remaining 45 samples were collected from different patients.
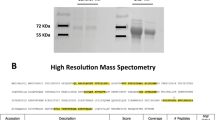
Since Garin et al. reported the utility of urinary CD80 as a differential biomarker between the relapse phase of MCD and other renal diseases in 200913, five other reports have been published concerning the use of this biomarker12,18,20,21,22. All these reports showed elevation of urinary CD80 only in patients with MCD in relapse, with levels remaining normal in controls, patients with MCD in remission, FSGS or other renal diseases. Specific elevation of urinary CD80 in MCD in relapse was supported by the following reports: (1) The expression of CD80 on podocytes was strongly enhanced in MCD patients in relapse, measured by immunostaining, compared with patients with MCD in remission or those with FSGS12. (2) The source of urinary CD80 is the podocytes because the molecular weight of urinary CD80 (53 kDa) is close to that of CD80 derived from cell membrane, rather than that of serum CD80 (23 kDa)12. (3) The serum level of CD80 is normal in MCD in relapse although it is elevated in urine13. However, some other studies have recently reported that the immunostaining assay of CD80 on podocytes is not a reliable diagnostic marker for MCD in relapse15,16.
Although previous reports maintain that urinary CD80 levels clearly differentiate between MCD in relapse and FSGS12,13,18,23, our study did not (Fig. 1) (Supplemental Fig. 2). There was some uncertainty, in that previous studies involved FSGS cases derived from genetic defects, whereas our cases with FSGS were derived from immunological mechanisms. To remove this concern, we measured urinary CD80 levels in patients with inherited NS; these patients also exhibited elevated CD80. This result supports our conclusion that urinary CD80 is not a reliable marker for MCD in relapse.
In our study, the concentration of CD80 in urine was higher in patients with FSGS and inherited NS in addition to MCD in relapse than MCD in remission. This might mean that excretion of urinary CD80 may increase in patients with active renal disease, rather than upon activation of T cells. CD80 has been previously measured in patients with inherited renal diseases14,23. Cara-Fuentes et al. reported a patient with an NPHS2 defect who showed elevation of urinary CD80. Reiser et al. reported that nephrin or α3 integrin knockout mice showed expression of CD80 on podocytes; they hypothesized that various stresses, including genetic defects, might lead to podocyte CD80 induction.
Our study showed that urinary CD80 is not affected by serum CD80 (Fig. 3). Importantly, we examined the correlation between serum and urine CD80 levels; we found that serum CD80 was within the reference range, even for serum samples from patients that simultaneously exhibited very high urinary CD80 values, suggesting that urinary CD80 is not derived from serum CD80.
We focused on the relationship between urinary protein and urinary CD80 and found a positive correlation (Fig. 2), which was observed in MCD in relapse, FSGS, and inherited NS (Supplemental Fig. 3). These results indicated that the elevation of urinary CD80 was not specific to patients with MCD in relapse, and it was correlated with urinary protein levels that might rather reflect the severity of glomerular damage, i.e., podocyte injuries. In contrast, in some samples, the correlation between urinary protein and CD80 was poor; this suggests that other factors may influence urinary CD80 excretion.
The current study has limitations. We did not perform Western blotting analysis of urinary CD80 or measure CD80 expression in kidney tissue. When examining urinary CD80, it is important to determine whether that urinary CD80 is blood-derived or kidney-derived; it is an important limitation that we did not perform these analyses. However, the method for measuring CD80 in renal tissues has been reported as low quality15,16; moreover, we showed that serum CD80 levels in our patients were not correlated with urinary CD80. The second limitation is that the sample sizes remain small in our study. The number of patients with FSGS or inherited NS was only four; however, 50% or 25% of these patients showed much higher levels of urinary CD80. Therefore, we judged that urinary CD80 might not be a useful diagnostic marker for renal diseases, and we decided not to collect more samples.
In conclusion, our results showed that urinary CD80 was not a reliable differential diagnostic marker between MCD in relapse and FSGS or other kidney diseases, including inherited kidney diseases, in contrast to previous reports. The level of CD80 was elevated in all patients with active kidney disease. We suggest that measuring urinary CD80 levels is not a reliable marker for the differential diagnosis of MCD in relapse and other kidney diseases.
Methods
Ethical considerations
All procedures were reviewed and approved by the Institutional Review Board of Kobe University Graduate School of Medicine (No_1770), with all study subjects providing written informed consent. All methods were performed in accordance with the relevant guidelines and regulations.
Patients
We retrospectively analysed 30 subjects in the healthy control group (Cat. No. OH2000, OH2010, Sunfco Ltd., Tokyo, Japan) and 65 samples from 55 patients with MCD (n = 31), FSGS (n = 4), inherited NS (n = 4), Alport syndrome (n = 5), and other glomerular diseases (n = 11), including Henoch-Schönlein Purpura Nephritis (HSPN), IgA Nephropathy (IgAN), Hemolytic Uremic Syndrome (HUS), and oligomeganephronia (Table 1). Renal biopsies were performed on all patients with MCD, FSGS, Alport syndrome, and other glomerular diseases except for the case with HUS. These patients were diagnosed using established criteria24,25,26,27,28. Pathogenic mutations were proven in all patients of inherited NS (NPHS1 p.Pro368Ser and p.Gln839Argfs*8, Ref:NM_004646, compound heterozygote) (WT1 p.Cys393Tyr, Ref:NM_024426, heterozygote) (ADCK4 p.Ser246Asn, Ref:NM_024876, homozygote) (ACTN4 p.Leu224Pro, Ref:NM_004924, heterozygote) and Alport syndrome by genetic tests. Thirty-one patients with MCD provided 41 urine samples, including 10 patients who provided samples at both relapse and remission. They were divided into two groups, including a group in remission (n = 17), whose urinary protein creatinine ratio was <2.0 g/gCre, and a group in relapse (n = 24), whose urinary creatinine ratio was >2.0 g/gCre. Immunosuppressive therapy was introduced for all patients with MCD in relapse, or FSGS, and for some patients with IgAN and HSPN. This led to a reduction in proteinuria for all treated patients.
CD80 measurement
The value of CD80 were measured by using urine and serum samples that had been stored at -80 °C. The sandwich ELISA method was used for measurement of urinary CD80. Nunc-Immuno module 96-well plates (Cat. No. 468667, Thermo Fisher Scientific, Waltham, MA, USA) were coated with 100 µl capture anti-CD80 antibody (Cat. No. 11-221-C100, Exbio, Vestec, Czech Republic). After the plates were incubated at 4 °C overnight for adhesion, the coating solution was removed completely. The coated wells were blocked with 300 µl of 1% BSA per well at 4 °C overnight. The urine and serum samples, standards of CD80 protein (Cat. No. 10698-H08H, Sino Biological Inc., Peking, China), and anti-CD80 antibody labelled with HRP (Cat. No. 37711 MAB140, R&D Systems Inc., Minneapolis, MN, USA) were diluted in PBS containing 1% BSA and were applied to wells with room temperature incubation for 90 min, followed by washing three times with PBS containing 0.05% Tween 20. The chemiluminescent substrate (Cat. No 37070, Thermo Fisher Scientific) was added and incubated for 15 min; then, absorbance values were read by using a microplate reader (FLUOstar OPTIMA, BMG Labtech).
Statistical analysis
All results were described as median with interquartile range. Kruskal-Wallis and Dunn’s multiple comparison tests were used for analyses of differences among groups. The Mann-Whitney U test was used for comparisons between high and low CD80 groups in each renal disease, and for comparison of urinary CD80 between MCD in relapse and renal diseases other than MCD. Spearman rank correlation coefficient was used to calculate the correlation between urinary protein and urinary CD80. The level of statistical significance was set as p < 0.05. Data graphics and statistical analysis were described with GraphPad Prism7 software.
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Caulfield, J. P. & Farquhar, R. J. MG. Alterations of the glomerular epithelium in acute aminonucleoside nephrosis. Evidence for formation of occluding junctions and epithelial cell detachment. Lab Invest 34, 43–59 (1976).
Ryan, G. B. & Karnovsky, M. J. An ultrastructural study of the mechanisms of proteinuria in aminonucleoside nephrosis. Kidney International 8, 219–232, https://doi.org/10.1038/ki.1975.105 (1975).
Eddy, A. A. & Symons, J. M. Nephrotic syndrome in childhood. The Lancet 362, 629–639, https://doi.org/10.1016/s0140-6736(03)14184-0 (2003).
Shalhoub, R. J. Pathogenesis of lipoid nephrosis- A disorder of T-cell function. Lancet 2, 556–603 (1974).
Mace, C. & Chugh, S. S. Nephrotic syndrome: components, connections, and angiopoietin-like 4-related therapeutics. J Am Soc Nephrol 25, 2393–2398, https://doi.org/10.1681/ASN.2014030267 (2014).
Buscher, A. K. et al. Immunosuppression and renal outcome in congenital and pediatric steroid-resistant nephrotic syndrome. Clin J Am Soc Nephrol 5, 2075–2084, https://doi.org/10.2215/CJN.01190210 (2010).
Buscher, A. K. et al. Rapid Response to Cyclosporin A and Favorable Renal Outcome in Nongenetic Versus Genetic Steroid-Resistant Nephrotic Syndrome. Clin J Am Soc Nephrol 11, 245–253, https://doi.org/10.2215/CJN.07370715 (2016).
Alegre, Maria-Luisa, Frauwirth, K. A. & Thompson, C. B. T-CELL REGULATION BY CD28 AND CTLA-4. Nature Reviews Immunology 1, 220–228 (2001).
Wakem, P. et al. Allergens and irritants transcriptionally upregulate CD80 gene expression in human keratinocytes. J Invest Dermatol 114, 1085–1092, https://doi.org/10.1046/j.1523-1747.2000.00997.x (2000).
Donepudi, M., Raychaudhuri, P., Bluestone, J. A. & Mokyr, M. B. Mechanism of Melphalan-Induced B7-1 Gene Expression in P815 Tumor Cells. The Journal of Immunology 166, 6491–6499, https://doi.org/10.4049/jimmunol.166.11.6491 (2001).
Ishimoto, T. et al. Toll-like receptor 3 ligand, polyIC, induces proteinuria and glomerular CD80, and increases urinary CD80 in mice. Nephrol Dial Transplant 28, 1439–1446, https://doi.org/10.1093/ndt/gfs543 (2013).
Garin, E. H. et al. Urinary CD80 is elevated in minimal change disease but not in focal segmental glomerulosclerosis. Kidney Int 78, 296–302, https://doi.org/10.1038/ki.2010.143 (2010).
Garin, E. H. et al. Urinary CD80 excretion increases in idiopathic minimal-change disease. J Am Soc Nephrol 20, 260–266, https://doi.org/10.1681/ASN.2007080836 (2009).
Reiser, J. et al. Induction of B7-1 in podocytes is associated with nephrotic syndrome. J Clin Invest 113, 1390–1397, https://doi.org/10.1172/jci20402 (2004).
Novelli, R., Gagliardini, E., Ruggiero, B., Benigni, A. & Remuzzi, G. Any value of podocyte B7-1 as a biomarker in human MCD and FSGS? Am J Physiol Renal Physiol 310, F335–341, https://doi.org/10.1152/ajprenal.00510.2015 (2016).
Larsen, C. P., Messias, N. C. & Walker, P. D. B7-1 immunostaining in proteinuric kidney disease. Am J Kidney Dis 64, 1001–1003, https://doi.org/10.1053/j.ajkd.2014.07.023 (2014).
Salant, D. J. Podocyte Expression of B7-1/CD80: Is it a Reliable Biomarker for the Treatment of Proteinuric Kidney Diseases with Abatacept? J Am Soc Nephrol 27, 963–965, https://doi.org/10.1681/ASN.2015080947 (2016).
Ling, C. et al. Urinary CD80 levels as a diagnostic biomarker of minimal change disease. Pediatr Nephrol 30, 309–316, https://doi.org/10.1007/s00467-014-2915-3 (2015).
Hock, B. D. et al. Identification of a circulating soluble form of CD80: levels in patients with hematological malignancies. Leuk Lymphoma 45, 2111–2118 (2004).
Cara-Fuentes, G. et al. CD80 and suPAR in patients with minimal change disease and focal segmental glomerulosclerosis: diagnostic and pathogenic significance. Pediatr Nephrol 29, 1363–1371, https://doi.org/10.1007/s00467-013-2679-1 (2014).
Cara-Fuentes, G., Wasserfall, C. H., Wang, H., Johnson, R. J. & Garin, E. H. Minimal change disease: a dysregulation of the podocyte CD80-CTLA-4 axis? Pediatr Nephrol 29, 2333–2340, https://doi.org/10.1007/s00467-014-2874-8 (2014).
Mishra, O. P. et al. Toll-like receptor 3 (TLR-3), TLR-4 and CD80 expression in peripheral blood mononuclear cells and urinary CD80 levels in children with idiopathic nephrotic syndrome. Pediatr Nephrol 32, 1355–1361, https://doi.org/10.1007/s00467-017-3613-8 (2017).
Cara-Fuentes, G. et al. CD80, suPAR and nephrotic syndrome in a case of NPHS2 mutation. Nefrologia 33, 727–731, https://doi.org/10.3265/Nefrologia.pre2013.Jun.12085 (2013).
John, A. & Mills, M. D. et al. The American College of Rheumatology 1990 criteria for the classification of henoch-schönlein purpura Authors. Arthritis Rheum. 33, 1068–1073 (1990).
Royer, P., Courtecuisse, H. R. & Leclerc, V. F. Bilateral renal hypoplasia with oligonephronia. (Study of 21 cases). Arch Fr Pediatr. 24, 249–268 (1967).
White, R. H. R., Glasgow, E. F. & Mills R. J. Clinicopathological study of nephrotic syndrome in childhood. Lancet 295, 1353–1359 (1970).
Igarashi, T. et al. Guidelines for the management and investigation of hemolytic uremic syndrome. Clin Exp Nephrol 18, 525–557, https://doi.org/10.1007/s10157-014-0995-9 (2014).
Magistroni, R., D’Agati, V. D., Appel, G. B. & Kiryluk, K. New developments in the genetics, pathogenesis, and therapy of IgA nephropathy. Kidney Int 88, 974–989, https://doi.org/10.1038/ki.2015.252 (2015).
Acknowledgements
The authors gratefully acknowledge the cooperation of the attending patients and physicians in this study. All phases of this study were supported by a grant from the Ministry of Health, Labour and Welfare (Japan) for Research on Rare Intractable Diseases in Kidney and Urinary Tract (H24-nanchitou (nan)-ippan-041 to Kazumoto Iijima) in the “Research on Measures for Intractable Diseases” Project and a Grant-in-Aid, Culture, Sports, Science and Technology [KAKENHI] (Subject ID: 15K09691 to Kandai Nozu, 17H04189to Kazumoto Iijima and 17K16087 to Shogo Minamikawa). This study was also funded by Sysmex corporation. We thank Colleen Elso, PhD, and Ryan Chastain-Gross, PhD, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript. Funding for this study was received from Sysmex Corporation.
Author information
Authors and Affiliations
Contributions
S.M. and K.I. designed the study concept and wrote the manuscript. K. Nozu interpreted the data and wrote the manuscript. S.M. H.S., and K. Noda established the ELISA assay for CD80. T.Y., K. Nakanishi., J.F., T.H., C.N., N.S., H.N., T.N. and H.K. collected and interpreted the data. T.N. and H.K., critically reviewed the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Minamikawa, S., Nozu, K., Maeta, S. et al. The utility of urinary CD80 as a diagnostic marker in patients with renal diseases. Sci Rep 8, 17322 (2018). https://doi.org/10.1038/s41598-018-35798-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-35798-2
Keywords
This article is cited by
-
Attogram-level light-induced antigen-antibody binding confined in microflow
Communications Biology (2022)
-
An updated view of the pathogenesis of steroid-sensitive nephrotic syndrome
Pediatric Nephrology (2022)
-
Biomarkers in pediatric glomerulonephritis and nephrotic syndrome
Pediatric Nephrology (2021)
-
Nephrotisches Syndrom im Kindesalter
Monatsschrift Kinderheilkunde (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.