Abstract
Multiple in vitro and mice model studies suggest statins may attenuate dengue severity. However, little is known about statin use and dengue severity in adult dengue patients with hyperlipidemia. We conducted a retrospective cohort study from 2004–2008 and 2012–2013 in Tan Tock Seng Hospital, Singapore on adult dengue patients with hyperlipidemia, comparing those with and without statin usage at hospitalization in terms of primary outcome of dengue hemorrhagic fever (DHF) or shock syndrome (DSS), and severe dengue (SD). Of 13,975 subjects screened, 257 dengue patients were included; 191 (74.3%) were statin users and 66 (25.7%) were non-users. Compared with non-users, statin use was not associated with decreased risk of DHF/DSS (adjusted risk ratio [aRR] = 0.66, 95%confidence interval [CI]: 0.41–1.08, P = 0.10) and SD (aRR = 1.43, 95%CI: 0.84–2.43, P = 0.19). Therefore, statin usage had minimal effect on dengue severity in our study population in Singapore.
Similar content being viewed by others
Introduction
Dengue is an arboviral disease of global importance, with increase in incidence attributed to globalization, changing climates, and geographical expansion1. It is caused by dengue virus (DENV) which has four serotypes. While majority of dengue patients recover uneventfully, a proportion will progress to severe illness which has no specific treatment available to date. The immune system plays an important role in dengue pathogenesis. It has been demonstrated that the peak in symptoms as well as progression to the critical phase of dengue occurs with viremia clearance and a rise in proinflammatory cytokines2. The pathogenesis of dengue hemorrhagic fever (DHF) or dengue shock syndrome (DSS) as defined in the World Health Organization (WHO) 1997 dengue guideline3, and severe dengue (SD) as defined in the WHO 2009 guideline4, involves vascular leakage which is associated with higher levels of various cytokines5,6.
Obesity, a non-communicable disease on the rise worldwide7, has been described as a risk factor for poorer outcomes in dengue8. Obesity is part of the metabolic syndrome which includes hyperlipidemia and is associated with an increased pro-inflammatory state9. Metabolic syndrome, obesity and hyperlipidemia are associated with various conditions such as nonalcoholic fatty liver disease, cardiovascular and cerebrovascular diseases, for which the treatment commonly includes statins. Statins are inhibitors of 3-hydroxy-3-methylglutaryl coenzyme A reductase, an enzyme necessary for cholesterol synthesis. With its pleiotropic effects, statins have been shown to reduce cytokines in various non-infective diseases10,11,12 and may potentially exert an immunomodulatory effect on the development of DHF/DSS and SD. Several retrospective and observational studies have documented better outcomes for patients already on statin therapy in various infectious such as pneumonia and bacteremia13. A few studies on in vitro and animal models for dengue infection also suggested that statin usage may improve disease outcomes14,15,16,17.
A common side effect of statins is a rise in transaminases, thus there is concern that continued use of statins in dengue infection can worsen clinical outcomes. Liver complications with raised transaminases of >1000 IU/L is one criterion for SD in the WHO 2009 dengue guideline4. Consequently, most clinicians discontinue statins upon suspicion of dengue infection and restart them only after recovery. A recent randomized controlled trial of Vietnamese adult dengue patients compared lovastatin versus placebo and did not find an increase in adverse events. However, the trial recruited relatively young adults who were unlikely to have comorbidities and was inadequately powered for dengue severity which was part of its secondary outcomes18. Thus, currently it is still unclear if preceding statin use influences the risk of dengue severity in adults with hyperlipidemia.
We embarked on this retrospective cohort study to investigate the association between preceding statin usage and dengue severity in adults with known hyperlipidemia presenting with dengue. We hypothesized that patients on statins had a decreased risk of plasma leakage with no increase risk in liver inflammation.
Results
A total of 13,975 subjects were screened and 257 dengue patients with history of hyperlipidemia were included, including 191 (74.3%) statin users and 66 (25.7%) non-users. Of the 191 statin users, majority were on simvastatin, at 132 users (69.1%), followed by lovastatin at 33 users (17.3%), atorvastatin at 16 users (8.4%), rosuvastatin at 8 users (4.2%) and pravastatin at 2 users (1.0%). The mean age was 61.6 years with standard deviation (SD) of 12.0 years for users and 60.5 years with SD of 11.9 years for non-users, with 93 (48.7%) and 33 (50.0%) males respectively (Table 1). Statin users were significantly more likely to be overweight or obese, have a higher CCI index, and a history of hypertension in keeping with metabolic syndrome compared with non-users. A higher proportion of users were observed to have chronic liver disease (P = 0.07), but not other comorbidities (Supplementary Table 1). Similarly, users had more concurrent medications, and a statistically significant higher proportion was also on sulfonylurea, metformin, insulin, antiplatelet agents, ACEI and ARB.
Statistically significant differences were noted in proportion of total cholesterol, LDL cholesterol, HDL cholesterol and triglyceride between users and non-users, with non-users having higher values. There was no statistically significant difference in ALT or AST levels at the end of hospitalization between the two groups, with a median ALT of 65IU/L (interquartile range [IQR]: 34–117 IU/L) in users and 68IU/L (IQR: 31–116 IU/L) in non-users (P = 0.69), and median AST of 94IU/L (IQR: 53–163 IU/L) in users and non-users 104 IU/L (IQR: 50–174 IU/L) (P = 0.78). There was no significant difference in proportion of patients with ALT ≥ 1000IU/L and AST ≥ 1000IU/L (Table 1).
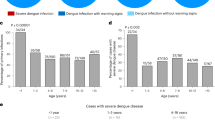
Statin users were more likely to develop tachycardia (91 [47.6%] statin users versus 13 [19.7%] non-users, P = < 0.001) and fluid accumulation (41 [21.5%] statin users versus 4 [6.1%] non-users, P = 0.01) than non-users (Supplementary Table 1). There was however no difference between platelet nadir between the two groups (Supplementary Table 1). With regards to disease severity, there was no significant difference in occurrence of overall DHF/DSS (56 [29.3%] statin users versus 24 [36.4%] non-users, P = 0.29) and SD (64 [33.5%] statin users versus 17 [25.8%] non-users, P = 0.24) (Table 1). Interestingly, a higher proportion of users (33.5%) were more likely to have severe plasma leakage as defined by WHO 2009 guidelines, compared to non-users (25.8%) (P = 0.04).
Compared with non-users, usage of statins prior to admission was not associated with a reduced risk of DHF/DSS on multivariate analysis, after adjusting for potential confounders including age, gender, year of presentation, BMI, CCI, hypertension, and other medications including antiplatelet drugs, ARB, ACEI, insulin, metformin and sulfonylurea. There was no statistically significant risk reduction for both DHF/DSS (aRR = 0.73 95%CI 0.46–1.16, P = 0.18) and SD (aRR 1.52, 95%CI: 0.91–2.53, P = 0.11) (Table 2). There was also no significant difference in clinical outcomes, including length of stay, ICU admission and mortality between the two groups (Supplementary Table 1).
Discussion
In this retrospective cohort study of laboratory confirmed adult dengue patients with hyperlipidemia, use of statins prior to hospital presentation was not associated with lower risk of DHF/DSS and SD. There was also no evidence of increased liver function abnormalities between dengue patients with or without statin use. A significantly higher proportion of users were more likely to develop severe plasma leakage as defined by WHO 2009 guidelines, compared to non-users. In our study, users of statin compared to non-users, had lower values of total cholesterol, LDL cholesterol, HDL cholesterol and triglyceride which may account for our findings. A similar phenomenon has also been reported in children, wherein lower levels of total cholesterol, LDL cholesterol and HDL cholesterol were observed in children with severe dengue when compared with children with mild dengue19,20, suggesting that cholesterol plays an important role in dengue pathophysiology, which needs to be further delineated.
DENV can infect a wide range of cells ranging from monocytes to endothelial cells in vitro21. T cells are activated, resulting in production of inflammatory cytokines and chemokines2. Statins may potentially exert immunomodulatory effects on the innate and adaptive immune response, as well as the vascular system. Briefly, higher levels of certain cytokines and chemokines such as interleukin (IL) 2, IL4, IL6, IL8, IL10, interferon (IFN)–γ, IFN-γ–induced protein 10 (IP-10), matrix metalloproteinases (MMP) 2 and MMP9 are associated with poorer prognosis5,22,23,24. In vitro non-dengue studies using murine cells, human bronchial epithelial cells and human monocytes showed a decrease in production of IL2, IL4, IL6, IL8, IFN- γ, MMP2 and MMP6 in the presence of statins25,26,27. In patients with various underlying medical conditions, ranging from autoimmune disease to cardiac disease, use of statins resulted in decreased IL6, IL10, IP10, MMP2 and MMP610,11,12. Inhibition of cholesterol synthesis by statins has been shown to directly reduce virion assembly and regulate DENV replication in vitro16,17, and this may result in shortened viremia and better outcomes. In murine models however, use of statins had increased viremia and yet improved survival thus there is conflicting data on the impact statins has on viremia15.
Currently, only one randomized controlled trial on the use of statin in 300 dengue patients has been conducted18, comparing lovastatin versus placebo. While the trial demonstrated that concurrent use of lovastatin was safe with ongoing dengue infection as its primary outcome, there was no statistically significant difference in outcomes either in duration of fever or viremia, or disease severity. Only 3 patients out of 300 developed DHF/DSS or SD; thus, the study was inadequately powered to study statin effect on disease severity in dengue. There is also no other literature on the use of statins in other flaviviruses or arboviruses. While there is literature on influenza and statin use, the differences between the viruses and diseases precludes extrapolation.
Interestingly, our data showed a significant increased plasma leakage by the WHO 2009 definition in users versus non-users, however this was not seen when the definition in the WHO 1997 guideline was used. The difference in outcome analysis was driven by the inclusion of hypoproteinemia in the 1997 definition and a higher proportion of non-users having hypoproteinemia. Nevertheless, overall our data suggests that discontinuation of statins may not be necessary at the onset of dengue infection, and clinicians may adopt a watchful approach of continuing statins, supporting results shown by the Vietnam group18. Discontinuation of statins may not be harmless even for short periods of time28. Abrupt statin withdrawal was shown to cause impaired endothelial function via nitric oxide release and higher C-reactive protein levels resulting in a pro-inflammatory state28. In high risk patients with angina, discontinuation of statins resulted in a three-fold increase in cardiac risk compared with patients who continued statin treatment and 1.7 times increase in cardiac risk compared with patients who were statin-naïve29. With an ageing population compounded by a rise in obesity and associated comorbidities in Singapore, it is not uncommon that patients can present with dengue on a background of multiple medical problems that may pose a therapeutic challenge.
Our study has several strengths. Firstly, we used DHF/DSS and SD in our analysis as these classifications are internationally established as clinically relevant endpoints of dengue severity. Secondly, the dengue outcome documented has minimal risk of outcome information bias as a standardized dengue care path was used by all clinicians to assess dengue patients in our hospital. Thirdly, risk of statin usage misclassification was low because statin usage was ascertained from medication prescription database as well as medication reconciliation records performed on hospital admission by a hospital pharmacist. Lastly, clinical data was collected by two trained research assistants, minimizing error in data extraction and standardizing data collection. Data audit was conducted to ensure data accuracy.
Limitations of our study include the relatively small study population, the lack of evaluation of patient’s compliance to statin use, and missing lipid profiles for about 30% of our study population. Although some patients may not be compliant with medications after the onset of dengue symptoms prior to hospital admission, these patients were still nonetheless recorded as users. This would make it more challenging to determine the effects of the duration and dosage of statin and its potential immuno-modulatory effects in dengue infection. Nevertheless, in the analysis of patients with available lipid profile, patients in the statin arm were more likely to have optimal LDL-C and triglyceride levels. It is thus reasonable to assume that therapeutic concentrations for lipid-lowering effects were achieved in users. Although it is unclear if this is the same dosage required for an immuno-modulatory effect, prior observational reports on improved clinical outcomes in sepsis were with the routine dosages of statins30,31. Other limitations include the lack of data to adjust for the effect of different dengue serotypes on disease severity. The potential effect of prior dengue infection on disease severity also could not be adjusted as serostatus was not available in clinical practice. There is a risk of channeling bias, namely statin prescription is dependent on patient’s characteristics such as age, gender, ethnicity and comorbidities, but this was mitigated by adjustment in multivariable analysis. Finally, the study was not sufficiently powered to examine the interactions and effects statin might exert as a whole and differentially on different subgroups of patients.
Conclusion
In adult dengue patients, statin usage at hospital admission did not reduce dengue severity in subjects with hyperlipidemia presenting with dengue. However, prior use of statins is not a risk factor for increased liver inflammation and supports the safety of continuing statins in patients with dengue.
Methods
We conducted a retrospective cohort study using patients from previous studies with similar study designs from 2004–2008 and 2012–2013 in Tan Tock Seng Hospital, a 1600-bed teaching hospital in Singapore. Data collected included baseline demographic data (age, gender and ethnicity), year of illness, comorbidities (including Charlson’s comorbidity index (CCI), hypertension and other immunocompromising status), weight and height, smoking, daily symptoms and signs of illness, laboratory investigations (full blood count, renal panel, liver panel and lipid profile), radiology, and prescribed medications from hospital admission to discharge. Lipid profile up to 1 year prior to admission were screened and included total cholesterol, low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C) and triglyceride. The most recent record for lipid profile was documented. Clinical data from hospital admission to discharge date for inpatients, or to the end of acute follow-up for outpatients were documented using a standardized dengue care path for all dengue patients and data were extracted by trained research assistants. We selected a cohort of laboratory-confirmed hospitalized dengue patients with hyperlipidemia. Laboratory confirmation of dengue was based on positive non-structural protein 1 (SD BIOLINE Dengue Duo Standard Diagnostics, Republic of Korea) or polymerase chain reaction (PCR) results32. Study exposure was current use of any statin and subjects were classified as ‘users’ if they were on statin treatment at the time of hospital admission for dengue. The study outcome was dengue categorized as DHF/DSS or SD as per WHO 1997 and 2009 guidelines respectively3,4. Briefly, DHF requires the presence of fever, thrombocytopenia, any bleeding and evidence of plasma leakage. Patients with DHF who experienced shock were classified as DSS3. Patients with severe plasma leakage (respiratory compromise or shock), severe bleeding and severe organ impairment (renal impairment, aspartate aminotransaminase (AST) or alanine aminotransaminase (ALT) > 1000 units/L, encephalopathy, myocarditis) were classified as SD4.
Potential confounders
Covariates likely to be associated with dengue severity and likelihood of receiving statin treatment were identified. Potential confounders include age, gender, comorbidities, obesity (body mass index (BMI) ≥ 30 kg/m2), smoking, and concurrent medications (sulfonylureas, metformin, insulin, anti-platelet agents, angiotensin-converting-enzyme inhibitors [ACEI], angiotensin-receptor blockers [ARB], anti-arrhythmic drugs and other lipid-lowering agents). DENV serotype is a known risk factor for disease severity33. As majority of the retrospective cohorts did not have PCR performed, the year of presentation was used as a surrogate marker for dengue serotype, postulating the serotype will be the predominant circulating dengue virus serotype of the epidemic year. Based on the Singapore communicable disease surveillance data from Ministry of Health Singapore, DENV-1 was the predominant serotype during 2004–2006 and 2013(61–82% of all circulating serotypes), and DENV-2 was the predominant serotype during 2007–2008 and 2012 (66–87%)34.
Statistical methods
In order to investigate the association between statin use and severe dengue manifestations, we used univariate and multivariate Poisson regression with robust error variance35 to estimate crude and adjusted risk ratio (cRR and aRR) respectively with 95% confidence interval (CI). Multivariable models were built by adding a priori defined clinically important variables including age, gender, chronic liver disease, year of presentation and variables with P < 0.20 between the two groups. The best fit model was compared against nested model with Akaike information criterion (AIC)36. All statistical analyses were carried out with Stata 13.1 (College Station, TX: StataCorp LP). Statistical significance was set at P < 0.05 and all reported P values were two-tailed. The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics consideration
The study was approved by Singapore National Healthcare Group Domain Specific Review Board (NHG DSRB – 2015/01053) with waiver of informed consent. All subject identifiers were anonymized for analysis.
Data Availability
All data supporting the findings of this study are available within the article or from the corresponding author upon reasonable request.
References
Messina, J. P. et al. Global spread of dengue virus types: mapping the 70 year history. Trends in microbiology 22, 138–146, https://doi.org/10.1016/j.tim.2013.12.011 (2014).
Screaton, G., Mongkolsapaya, J., Yacoub, S. & Roberts, C. New insights into the immunopathology and control of dengue virus infection. Nature reviews. Immunology 15, 745–759, https://doi.org/10.1038/nri3916 (2015).
WHO. Dengue haemorrhagic fever. Diagnosis, treatment, prevention and control. Second Edition (1997).
WHO. Dengue Guidelines for Diagnosis, Treatment, Prevention and Control. Third Edition (2009).
Her, Z. et al. Severity of Plasma Leakage Is Associated With High Levels of Interferon gamma-Inducible Protein 10, Hepatocyte Growth Factor, Matrix Metalloproteinase 2 (MMP-2), and MMP-9 During Dengue Virus Infection. The Journal of infectious diseases 215, 42–51, https://doi.org/10.1093/infdis/jiw494 (2017).
Tramontini Gomes de Sousa Cardozo, F. et al. Serum from dengue virus-infected patients with and without plasma leakage differentially affects endothelial cells barrier function in vitro. PloS one 12, e0178820, https://doi.org/10.1371/journal.pone.0178820 (2017).
Ford, N. D., Patel, S. A. & Narayan, K. M. Obesity in Low- and Middle-Income Countries: Burden, Drivers, and Emerging Challenges. Annual review of public health 38, 145–164, https://doi.org/10.1146/annurev-publhealth-031816-044604 (2017).
Zulkipli, M. S. et al. The association between obesity and dengue severity among pediatric patients: A systematic review and meta-analysis. PLoS neglected tropical diseases 12, e0006263, https://doi.org/10.1371/journal.pntd.0006263 (2018).
Kim, D., Touros, A. & Kim, W. R. Nonalcoholic Fatty Liver Disease and Metabolic Syndrome. Clinics in liver disease 22, 133–140, https://doi.org/10.1016/j.cld.2017.08.010 (2018).
van der Meij, E. et al. A clinical evaluation of statin pleiotropy: statins selectively and dose-dependently reduce vascular inflammation. PloS one 8, e53882, https://doi.org/10.1371/journal.pone.0053882 (2013).
Duan, H. Y. et al. Effect of atorvastatin on plasma NT-proBNP and inflammatory cytokine expression in patients with heart failure. Genetics and molecular research: GMR 14, 15739–15748, https://doi.org/10.4238/2015.December.1.25 (2015).
Erkan, D. et al. A prospective open-label pilot study of fluvastatin on proinflammatory and prothrombotic biomarkers in antiphospholipid antibody positive patients. Annals of the rheumatic diseases 73, 1176–1180, https://doi.org/10.1136/annrheumdis-2013-203622 (2014).
Hennessy, E., Adams, C., Reen, F. J. & O’Gara, F. Is There Potential for Repurposing Statins as Novel Antimicrobials? Antimicrobial agents and chemotherapy 60, 5111–5121, https://doi.org/10.1128/aac.00192-16 (2016).
Bryan-Marrugo, O. L. et al. The antidengue virus properties of statins may be associated with alterations in the cellular antiviral profile expression. Molecular medicine reports 14, 2155–2163, https://doi.org/10.3892/mmr.2016.5519 (2016).
Martinez-Gutierrez, M., Correa-Londono, L. A., Castellanos, J. E., Gallego-Gomez, J. C. & Osorio, J. E. Lovastatin delays infection and increases survival rates in AG129 mice infected with dengue virus serotype 2. PloS one 9, e87412, https://doi.org/10.1371/journal.pone.0087412 (2014).
Rothwell, C. et al. Cholesterol biosynthesis modulation regulates dengue viral replication. Virology 389, 8–19, https://doi.org/10.1016/j.virol.2009.03.025 (2009).
Martinez-Gutierrez, M., Castellanos, J. E. & Gallego-Gomez, J. C. Statins reduce dengue virus production via decreased virion assembly. Intervirology 54, 202–216, https://doi.org/10.1159/000321892 (2011).
Whitehorn, J. et al. Lovastatin for the Treatment of Adult Patients With Dengue: A Randomized, Double-Blind, Placebo-Controlled Trial. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America 62, 468–476, https://doi.org/10.1093/cid/civ949 (2016).
Biswas, H. H. et al. Lower Low-Density Lipoprotein Cholesterol Levels Are Associated with Severe Dengue Outcome. PLoS neglected tropical diseases 9, e0003904, https://doi.org/10.1371/journal.pntd.0003904 (2015).
van Gorp, E. C. et al. Changes in the plasma lipid profile as a potential predictor of clinical outcome in dengue hemorrhagic fever. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America 34, 1150–1153, https://doi.org/10.1086/339539 (2002).
Martina, B. E. E., Koraka, P. & Osterhaus, A. D. M. E. Dengue Virus Pathogenesis: an Integrated View. Clinical Microbiology Reviews 22, 564–581, https://doi.org/10.1128/CMR.00035-09 (2009).
Abhishek, K. S. et al. Association of interleukin-2, -4 and -10 with dengue severity. Indian journal of pathology & microbiology 60, 66–69, https://doi.org/10.4103/0377-4929.200027 (2017).
Mehta, V. K. et al. Study of interleukin-6 and interleukin-8 levels in patients with neurological manifestations of dengue. Journal of postgraduate medicine 63, 11–15, https://doi.org/10.4103/0022-3859.188545 (2017).
Lee, Y. H., Leong, W. Y. & Wilder-Smith, A. Markers of dengue severity: a systematic review of cytokines and chemokines. The Journal of general virology 97, 3103–3119, https://doi.org/10.1099/jgv.0.000637 (2016).
Zhang, J. et al. Statins directly suppress cytokine production in murine intraepithelial lymphocytes. Cytokine 61, 540–545, https://doi.org/10.1016/j.cyto.2012.12.006 (2013).
Iwata, A. et al. Inhibitory effect of statins on inflammatory cytokine production from human bronchial epithelial cells. Clinical and Experimental Immunology 168, 234–240, https://doi.org/10.1111/j.1365-2249.2012.04564.x (2012).
Sasidhar, M. V., Chevooru, S. K., Eickelberg, O., Hartung, H. P. & Neuhaus, O. Downregulation of monocytic differentiation via modulation of CD147 by 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors. 12, e0189701, https://doi.org/10.1371/journal.pone.0189701 (2017).
Reidenberg, M. M. Drug discontinuation effects are part of the pharmacology of a drug. The Journal of pharmacology and experimental therapeutics 339, 324–328, https://doi.org/10.1124/jpet.111.183285 (2011).
Heeschen, C. et al. Withdrawal of statins increases event rates in patients with acute coronary syndromes. Circulation 105, 1446–1452 (2002).
Liappis, A. P., Kan, V. L., Rochester, C. G. & Simon, G. L. The Effect of Statins on Mortality in Patients with Bacteremia. Clinical Infectious Diseases 33, 1352–1357, https://doi.org/10.1086/323334 (2001).
Ma, Y. et al. Systematic Review and Meta-Analysis on the Association between Outpatient Statins Use and Infectious Disease-Related Mortality. PloS one 7, e51548, https://doi.org/10.1371/journal.pone.0051548 (2012).
Barkham, T. M., Chung, Y. K., Tang, K. F. & Ooi, E. E. The performance of RT-PCR compared with a rapid serological assay for acute dengue fever in a diagnostic laboratory. Transactions of the Royal Society of Tropical Medicine and Hygiene 100, 142–148, https://doi.org/10.1016/j.trstmh.2005.05.015 (2006).
Yung, C.-F. et al. Dengue serotype-specific differences in clinical manifestation, laboratory parameters and risk of severe disease in adults, Singapore. The American journal of tropical medicine and hygiene 92, 999–1005 (2015).
Htun, H. L. et al. Metformin Use and Severe Dengue in Diabetic Adults. Scientific Reports 8, 3344 (2018).
Zou, G. A modified poisson regression approach to prospective studies with binary data. American journal of epidemiology 159, 702–706 (2004).
Posada, D. & Buckley, T. R. Model selection and model averaging in phylogenetics: advantages of Akaike information criterion and Bayesian approaches over likelihood ratio tests. Systematic biology 53, 793–808 (2004).
Author information
Authors and Affiliations
Contributions
Chia P.Y., Htun H.L., Yeo T.W. and Lye D.C. had been involved in drafting the manuscript or revising it critically for important intellectual content. Ling W.P., Htun H.L., Leo Y.S. and Lye D.C. made substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chia, P.Y., Htun, H.L., Ling, W.P. et al. Hyperlipidemia, statin use and dengue severity. Sci Rep 8, 17147 (2018). https://doi.org/10.1038/s41598-018-35334-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-35334-2
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.