Abstract
In order to evaluate risk factors related to the presence of extrinsic dental black stain, a total of 94 orally healthy volunteers (47 individuals with dental black stain and 47 individuals without dental black stain) were recruited from ten different dental clinics in Valencia and Castellón (Spain). Data regarding their oral hygiene, dietary habits, and oral health status were gathered by questionnaire. Samples of dental plaque, saliva and drinking water were collected for chemical analysis. Three factors were found to be statistically significantly associated with dental black stain, (i) consuming water with high iron content, (ii) consuming water with high pH, and (iii) having a high salivary pH. Other factors such as smoking, taking iron supplements or consuming caffeinated drinks were not found to be risk factors for the presence of black stain. A multivariate logistic regression analysis showed that drinking tap or osmosis-purified water and lower levels of salivary iron increase the risk of having dental black stain. Overall, several risk factors for the presence of dental black stain have been identified. The main modifiable risk factor identified in this study was the consumption of tap or osmosis drinking water.
Similar content being viewed by others
Introduction
Extrinsic dental black stain (BS) can appear as a complete or incomplete black line on the buccal and/or lingual surfaces of the teeth near the gingival margin1. These stains are firmly attached to the tooth and are difficult to remove with conventional toothbrush and toothpaste. In addition, they tend to reappear after their removal1. Published studies show prevalence from 1 to 20%2,3. This pigmentation is a relatively common phenomenon in children, where it may occur at any age, even as early as 2 years old4.
Although its development is not fully understood, early published literature suggests that BS is a black insoluble ferric compound, formed by the interaction between hydrogen sulfide produced by bacteria and iron5. A recent study published by Zhang and collaborators confirms by coupled plasma-mass spectrometry a higher level of iron in BS when compared to standard plaque6.
Regarding the bacterial species which could play a role in the formation of BS, initial hypotheses suggested the involvement of chromogenic bacteria, such as Porphyromonas gingivalis and other black-pigmented members7,8. However, several studies using PCR technology have ruled out the presence of such bacteria9, and described a reduced microbial diversity in the black stain as compared to standard plaque, with the enrichment of some bacterial genera (Actinomyces, Cardiobacterium, Haemophilus, Corynebacterium, Tannerella and Treponema) and lower levels of Campylobacter, suggesting a dysbiosis as a possible cause or contributing factor to black stain10. A recent study published by our group shows the presence of Tannerella forsythia in 83,9% of patients with dental BS11.
Currently, the main therapeutic approach is frequent dental prophylaxis upon reappearance of the BS, which can cause damage to the enamel microstructure and dental sensitivity. The objective of the present study is to identify risk factors that may influence the appearance of BS in children and adults, such as socio-demographic variables, oral hygiene and status, iron content of saliva and dental plaque, salivary pH, iron levels and pH of drinking water.
Methods
Participants
This study was carried out in accordance with the Helsinki guidelines, and approved by the Ethics Committee of CEU Cardenal Herrera University (Authorization Number CEI16/018). The research was carried out in ten private dental clinics in Valencia and Castellón from April 2014 to April 2016. A power analysis based on an expectation a 20% incidence of BS in the population (based on published data)2, an alpha value of 0.05 and a power of 0.9 indicated that a total of 90 volunteers was required12. To account for losses during to follow up, 47 patients with black plaque of bacterial origin in at least 2 teeth (according to the diagnostic criteria proposed by Koch et al.13) were recruited to participate in the study. Equal numbers of age- and sex-matched subjects without BS were selected as control group, making a total of 94 participants. All adults and legal guardians of participant children gave informed consent. The only exclusion criterion was to have taken antibiotics 15 days prior to the dental appointment.
Questionnaire
Each participant completed a questionnaire, including questions regarding socio-demographic variables such as age and sex, hygiene habits such as the type of dental brush or numbers of brushes per day, dietary habits such as snacking between meals, iron supplementation, and type of drinking water consumed. Other chemical parameters such as pH of saliva and drinking water and iron content in plaque, saliva and drinking water were also recorded.
Clinical examination
Intraoral examination of each patient was performed to evaluate the presence of black stain and to determine the degree of pigmentation, according to the classification scheme described by Koch13 and modified by Gasparetto et al.14, as reported previously by our lab11. Each patient’s BS score was assigned as follows: 1 for pigmented spots or incomplete lines parallel to the gingival margin; 2 for solid lines pigmented, readily observable and limited to the cervical third of the tooth surface; and 3 for pigmentation extending beyond the cervical third. The evaluation was always performed by the same dentist. The values obtained were analyzed by a test-retest study to assess intra-operator agreement. Briefly, ten images of participants with black staining were randomly selected and the teeth were measured twice (with an interval of ten days) by the same operator. The Kappa index obtained was 0.788, indicating good reliability of the method. Oral health status of each participant was assessed by calculating the DMFT (decay-missing-filled-teeth) Index, Periodontal Index and Hemorrhage Index15.
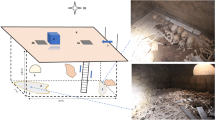
Analysis of dental plaque, saliva and drinking water samples
Supragingival dental plaque samples were collected by scraping with a plastic scaler from tooth surfaces taking care to avoid unnecessary removal of enamel16. A total of 1 mg of each collected plaque sample was transferred to sterile endodontic paper points and stored in sterile 0.5 ml DNA- and RNA-free Eppendorf tubes, and store at −20 °C until processed, as described previously11 (Fig. 1). Unstimulated whole saliva samples were collected as described elsewhere17. Each participant provided a sample of drinking water (for those drinking tap water) or specified the brand of mineral water consumed. Supragingival dental plaque samples were subject to digestion with 65% nitric acid (JT Baker®, Fisher Scientific, Madrid, Spain) for 24 hours prior to iron determination18. Iron determination in all samples (saliva, drinking water and digested supragingival plaque) was performed using Spin 200E equipment (Spinreact®, Girona, Spain), following the manufacturer instructions, and as described elsewhere19. Salivary and drinking water pH was analyzed with a pH-meter Basic 20 with glass electrode for microsamples (Crison instruments®, Barcelona, Spain).
Statistical analysis
Pearson’s chi-squared test was used to analyze the distribution of black stain amongst participants and the assessment of risk factors such as hygiene and dietary habits, smoking or type of drinking water. The Mann-Whitney test was used to test for differences between the BS and control groups with regard to the oral health status (DMFT index, bleeding index, periodontal index) and chemical variables (salivary and drinking water pH, iron levels in saliva, dental plaque and drinking water). Spearman’s coefficient was used to analyze correlations. Logistic regression was used to perform a multivariate analysis of the different risk factors assessed.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Ethics Committee of CEU Cardenal Herrera University (Authorization Number CEI16/018).
Informed consent
Prior informed consent was obtained from all individual participants included in the study.
Results
A total of 94 volunteers participated in the study. The mean age of the control group was 39.8 ± 18.1 years, and 39.9 ± 18.3 years for volunteers with BS (Table 1). Age showed no association with the presence of black stain (P = 0.982). The ratio of female to male volunteers was calculated as 1.69: 1. No statistically significant differences was found between males and females with BS, ruling out sex as a risk factor (P = 0.831; Table 1). The mean number of stained teeth for participants with BS was 17.68 ± 6.47, with 25 surfaces ± 11.01 stained on average, with a higher number of lingual surfaces stained (63.9% of lingual surfaces were stained surfaces whilst 35.2% of vestibular surfaces showed presence of BS; data not shown). Age was found to be inversely related to the percentage of stained surfaces. As age increases, the percentage of stained surfaces decreases, with a Spearman’s rho of −0.381 (P = 0.029).
Risk factors related to oral hygiene, dietary and social habits
Participants were asked about their oral hygiene habits, such as frequency of tooth brushing and type of dental brush employed. No significant differences were found amongst participants brushing three or more times when compared to participants brushing twice or once per day (P = 0.321). Similarly, the type of dental brush used (manual or rotatory, or combination of both) did not show an impact upon the presence of BS (P = 0.553; Table 2). Participants were asked about several dietary habits. The BS group showed a significantly lower number of participants who snacked between meals when compared to the control group (31.9% vs 53.2%, P = 0.037; Table 2). The majority of participants in the control group consumed mineral water (93.6%) whilst in the BS group 57.4% of participants consumed mineral water, 27.7% consumed tap water, and 14.9% consumed osmosis-purified water (Table 2). Only 6.4% of participants in the control group drank osmosis-purified water and none of them referred to drinking tap water. When asked about the consumption of iron supplements, 8.5% and 6.4% of control and BS participants, respectively, indicated that they consumed regularly iron supplements (Table 2). Pearson’s chi-squared test was applied to the above dietary factors, resulting in a P value of 0.037 for snacking between meals (being these a protective factor) and a P < 0.001 for the type of drinking water consumed (with consumption of tap or osmosis water being a risk factor for the presence of BS).
Regarding social habits, 19.1% of control participants were smokers, whilst 85.1% of control participants consumed regularly caffeinated drinks (tea, coffee and/or soft drinks). In the BS group 10.6% of participants consumed tobacco, whilst 76.6% of participants drank caffeinated drinks habitually. No statistically significant differences were found regarding the consumption of iron supplements, smoking or caffeine consumption (P = 0.500; P = 0.247; P = 0.294, respectively).
Risk factors related to oral health status
Oral health status of the participants was assessed with the DMFT index and the bleeding and periodontal indexes. The control group showed a median DMFT index of 7 whilst the BS group showed a median DMFT value of 5 (Interquartile range 9 and 8 respectively; Table 3). BS patients showed an increased bleeding index (median of 4.3 in the BS group versus 3.4 in the control group). The periodontal index was obtained for all adult participants, with similar results in both groups (median 16.8 in both groups, with interquartile ranges of 1.20 and 1.00 (control and patients respectively).
Mann-Whitney test was applied, since the above mention parameters showed non-normal distribution. No statistically significant results were found when comparing the control and the BS groups, with P values of 0.298, 0.416 and 0.574 respectively for DMFT, periodontal and bleeding indexes (Table 3).
Risk factors associated with salivary iron and pH, the iron in dental plaque and the pH and iron levels of drinking water
Salivary pH was measured in all study participants, with an average value of 7.2 ± 0.7 in the control group versus an average value of 8.0 ± 0.5 in the participants with BS (Table 4). The Mann-Whitney test demonstrated a highly significant difference in these salivary pH values (P < 0.001). Iron levels were also quantified in saliva of the volunteers; control participants carried an average of 63.9 ± 93 µg/dl, whilst the BS participants showed lower levels of salivary iron, with an average value of 5.4 ± 11.1 µg/dl. A similar trend was detected in the iron levels in dental plaque, BS participants showed a lower level of iron (77.0 ± 67.5 µg/dl) than control participants (116.4 ± 91.4 µg/dl). Both iron levels in saliva and dental plaque were found not to be statistically significant (P = 0.066; P = 0.153; Mann-Whitney test).
Levels of pH and iron were analyzed in the drinking water consumed by the participants. We found that pH was lower in the control group (6.9 ± 1.0) when compared to the average pH of drinking water in the BS group (7.4 ± 1.4; P = 0.003). Iron levels were also lower in the drinking water consumed by the control participants (20.7 ± 51.7 µg/dl control group vs 70.8 ± 77.6 µg/dl BS group, P = 0.028).
Multivariate analysis
Multivariate logistic regression analysis revealed that BS was statistically significantly associated with the type of drinking water (tap/osmosis) and the presence of iron in saliva (lower quantity; Table 5). The odds of having BS was 13 times higher in participants consuming tap or osmosis water, and salivary iron consistently influenced the tendency for BS with an odds ratio of about 2.25% for each unitary increase in iron levels (Table 5).
Discussion
This study aimed to identify significant risk factors for the presence of dental black stain. According to previous published studies, several factors were investigated such as demographic characteristics20, oral hygiene and oral health status3,21, dietary factors such as snacking between meals and type of drinking water3,22, intake of iron supplements and iron levels of saliva and dental plaque6, and pH and iron contents of saliva23,24. Our study included adult participants; hence factors such as smoking or caffeine consumption were also included as potential risk factors for the presence of black stain in adults.
We found no association between sex and the presence of BS, in agreement with the majority of published work13,20,22,25. Similarly, we did not find association between age and the presence of BS, coinciding with previous reports13,22,25. One study by Chen and coworkers showed a correlation (although not statistically significant) between age and BS20, reporting also that the number of stained teeth increased with age, contradicting our findings. This could be due to the different population analyzed, since the mean age of the participants in the Chen study was 4.55 years and our study included adult participants with a mean age of 39.85 years.
Several studies have indicated in past years that BS could be associated with lower caries3. Our results also found that DMTF indexes were slightly lower in BS participants, although the difference was not found to be statistically significant. Early studies of BS suggested a role for chromogenic bacteria as possible causative factor of this extrinsic tooth discoloration7,8. Since some of these bacteria also related to periodontal disease, it has been suggested that gingival bleeding stimulated by the presence of the bacteria could be the source of iron necessary for the formation of the black pigment26. Even though bleeding indexes were elevated in the BS group, no substantial differences amongst participant groups were detected, ruling out periodontal bleeding as a risk factor for BS, in agreement with recent literature attributing better oral health to individuals with BS3,8,20,22. Some authors have pointed out that individuals with BS might demonstrate better oral hygiene, in an attempt to control BS extension, which in turn will lead to improved oral health. Although there is conflicting evidence about the influence of oral hygiene in BS, oral hygiene habits were not found significantly different amongst participant groups in our study.
When dietary and social habits were investigated, we found no association between habits such as smoking, intake of caffeinated drinks or iron supplements. A recent report by Prskalo and coworkers highlights the consumption of beets as risk factor for BS27 whilst intake of collard greens and wine were more frequent in participants without BS. Prskalo’s results also showed no association between intake of iron supplements and BS27. Our control group showed higher frequency of snacking between meals when compared to the BS group. One dietary factor was identified as a strong risk factor, the type of drinking water. In agreement with one previous study published in Brazil22, we found that in our study population, consuming tap or osmosis water increased the odds of having BS by 13 times.
Levels of pH and iron concentration in saliva have been reported to differ between the subjects with and without caries, with a significant negative relationship between the salivary pH and iron concentration28. Lower salivary pH and higher iron levels have been postulated as increasing caries risk28. Since BS is traditionally associated with reduced caries formation, we decided to investigate pH levels and iron concentration in saliva and dental plaque, to find out if any of the above factors could play a role in promoting BS formation and maintenance. Our BS participants showed increased salivary pH and lower salivary and plaque iron levels, as reported previously23,24. Snacking decreases salivary pH regularly, so this could explain our finding that snacking between meals could play a protective role against BS, due to the effect on salivary pH, promoting acidification.
Both pH and iron levels were analyzed in drinking water, aiming to identify if different levels of pH or iron could be the underlying reason for the increased BS risk detected in participants consuming this type of water. We found higher pH levels, but also, higher iron content in tap/osmosis water than in mineral water. One explanation for this discrepancy between salivary and drinking water iron levels could be that lower pH could enhance iron solubility and higher pH will have the opposite effect29. Even though tap/osmosis water provides a higher iron content, elevated salivary pH would reduce the availability of this iron to bacteria in the gingival sulcus, hence modifying the normal microbiota, leading to the dysbiosis observed in BS10.
The main limitations of our study are related to the in-depth analysis of dietary factors involved in BS. More cohort studies following participants with substantially different diets would be necessary to address this lack of information with respect to the role of diet in BS. Major strengths of our study are the inclusion of adult participants (only one previous study included volunteers up to 50 years old)30 and the identification of one preventable risk factor for the presence of black stain; the consumption of tap/osmosis water.
Three factors were found to independently influence the presence of BS (consuming water with high iron content, consuming water with high pH, and having a high salivary pH). The two main factors associated with the presence of BS were low levels of salivary iron and consuming tap/osmosis water. Patients with BS should be advised to switch to mineral water to reduce the risk of BS reappearance following dental prophylaxis.
References
Hattab, F. N., Qudeimat, M. A. & al-Rimawi, H. S. Dental discoloration: an overview. J. Esthet. Dent. 11, 291–310 (1999).
Ronay, V. & Attin, T. Black Stain- A review. Oral Health Prev. Dent. 9(1), 37–45 (2011).
Zyla, T., Kawala, B., Antoszewska-Smith, J. & Kawala, M. Black stain and dental caries: a review of the literature. Biomed. Res. Int. 2015, 469392, https://doi.org/10.1155/2015/469392 (2015).
Paredes, V. & Paredes, C. Tinción cromógena: un problema habitual en la clínica pediátrica. An. Pediatr. 62, 258–260 (2005).
Reid, J. S., Beeley, J. A. & MacDonald, D. G. Investigations into black extrinsic tooth stain. J. Dent. Res. 56(8), 895–899 (1977).
Zhang, F., Li, Y., Xun, Z., Liu, H. & Chen, F. A preliminary study on the relationship between iron and black extrinsic tooth stain in children. Lett. Applied Microbiol. 64, 424–429 (2017).
Pessoa, L., Galvão, V., Damante, C. & Sant’Ana, A. Removal of black stains from teeth by photodynamic therapy: clinical and microbiological analysis. BMJ Case Reports bcr2015212276. https://doi.org/10.1136/bcr-2015-212276 (2015).
Heinrich-Weltzien, R., Bartsch, B. & Eick, S. Dental caries and microbiota in children with black stain and non-discoloured dental plaque. Caries Res. 48, 118–125 (2014).
Saba, C. et al. Black stains in the mixed dentition: A PCR microbiological study of the etiopathogenic bacteria. J. Clin. Pediatr. Dent. 30(3), 219–224 (2006).
Li, Y. et al. Analysis of the microbiota of black stain in the primary dentition. PLoS One 10, e0137030, https://doi.org/10.1371/journal.pone.0137030 (2015).
Albelda-Bernardo, M. A., Jovani-Sancho, M. M., Veses, V. & Sheth, C. C. Remediation of adult black dental stains by phototherapy. BDJ Open 4, 17035, https://doi.org/10.1038/s41405-018-0001-9 (2018).
Rosner, B. Fundamentals of Biostatistics (ed. Brooks/Cole) (Boston, 2011).
Koch, M. J. et al. Black stain and dental caries in schoolchildren in Potenza, Italy. J. Dent. Child. 68(3), 353–355 (2010).
Gasparetto, A. Prevalence of black tooth stains and dental caries in Brazilian schoolchildren. Braz. Dent. J. 14, 157–161 (2003).
WHO. Oral Health Surveys. Basic Methods. 5ª ed., Geneva: World Health Organization, 2013, http://www.who.int/oral_health/publications/9789241548649/en/ [last accessed on 9th July 2018].
Parnas, L., Chevion, M., Berenshtein, E., Faibis, S. & Moskovitz, M. Are there metallic traces in black extrinsic dental stain? Quintessence Int. 44(5), 427–432 (2013).
Norris, H. L. et al. Salivary metals, age, and gender correlate with cultivable oral Candida carriage levels. J. Oral Microbiol. 10, 1447216, https://doi.org/10.1080/20002297.2018.1447216 (2018).
Perrotta, G. Iron and iron-binding capacity. (eds Pesce, A. J. & Kaplan, L. A., Methods in clinical chemistry) 1258–1261 (CV Mosby, 1987).
Sánchez-González, C. et al. Exposure to bis(maltolato)oxovanadium (IV) increases levels of hepcidin mRNA and impairs the homeostasis of iron but not that of manganese. Food Chem. Toxicol. 73, 113–118 (2014).
Chen, X. et al. Factors associated with black tooth stain in Chinese preschool children. Clin. Oral Invest. 18, 2059–2066 (2014).
Boka, V., Trikaliotis, N., Kotsanos, N. & Karagiannis, V. Dental caries and oral health related factors in a sample of greek preschool children. Eur. Arch. Paediatr. Dent. 14, 363–368 (2013).
França-Pinto, C. et al. Association between black stains and dental caries in primary teeth: findings from a brazilian population based birth cohort. Caries Res. 46(2), 170–176 (2012).
Surdacka, A. Chemical composition of the saliva in children and adolescents with black tartar. Czas Stomatol. 42, 525–533 (1989).
Surdacka, A. Amount and pH of the saliva in children and adolescents with black tartar. Czas Stomatol. 42, 381–386 (1989).
Martin, J. M. G. et al. Prevalence of black stain and associated risk factors in preschool Spanish children. Pediatrics International 55, 355–359 (2013).
Zambon, J. J., Reynolds, H. S. & Slots, J. Black-pigmented Bacteroides spp. In the human oral cavity. Infect. Immun. 32, 198–203 (1981).
Prskalo, K. et al. Risk factors associated with black tooth stain. Acta Clin. Croat. 56(1), 28–35 (2017).
Zhou, J. et al. Influences of pH and iron concentration on the salivary microbiome in individual humans with and without caries. Appl. Environ. Microbiol. 83, e02412–16, https://doi.org/10.1128/AEM.02412-16 (2017).
Andrews, S. C., Robinson, A. K. & Rodriguez-Quinones, F. Bacterial iron homeostasis. FEMS Microbiol. Rev. 27, 215–237 (2003).
Costa, M. T., Dorta, M. L., Ribeiro-Dias, F. & Pimenta, F. C. Biofilms of black tooth stains: PCR analysis reveals presence of Streptococcus mutans. Braz. Dent. J. 23(5), 555–558 (2012).
Author information
Authors and Affiliations
Contributions
C.S.O.-L. performed the clinical examinations, data and sample collection. V.V. participated in the experimental design and wrote the manuscript. J.A.G.B. participated in the experimental design and supervised the chemical analysis. M.M.J.-S. participated in the experimental design and supervised the clinical examinations. All authors reviewed the data and the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ortiz-López, C.S., Veses, V., Garcia-Bautista, J.A. et al. Risk factors for the presence of dental black plaque. Sci Rep 8, 16752 (2018). https://doi.org/10.1038/s41598-018-35240-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-35240-7
Keywords
This article is cited by
-
Dental black plaque: metagenomic characterization and comparative analysis with white-plaque
Scientific Reports (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.