Abstract
To determine the prognostic value of lymphovascular invasion (LVI) in patients with bladder cancer who underwent radical cystectomy. Total of 747 patients underwent radical cystectomy; of these, only 164 did not undergo lymph node dissection (LND). The patients were divided into 4 groups: N0, N1, LVI without LND, and non-LVI without LND. Patients in the N1 and LVI groups had significantly higher T stages and grades, as well 1.5- to 2-fold higher recurrence and mortality rates. Overall survival (OS) was significantly poorer in the N1 group, compared with the N0 and non-LVI groups (p = 0.001 and 0.012), and in the LVI group relative to the N0 and non-LVI groups (p = < 0.001 and <0.001). Recurrence-free survival (RFS) was also significantly poorer in the N1 group relative to the N0 and non-LVI groups (p = < 0.001 and <0.001), and in the LVI group relative to the N0 and non-LVI groups (p = < 0.001 and <0.001). Among patients undergoing radical cystectomy, the clinical results predicted by LVI were similar to those predicted by lymph node involvement. Therefore, the role of adjuvant chemotherapy or immunotherapy may need to be prospectively evaluated in LVI-positive patients regardless of T stage after radical cystectomy.
Similar content being viewed by others
Introduction
Bladder cancer is among the most common malignancies of the urogenital system1, and most cases are histopathologically identified as urothelial carcinoma (UC). Among patients with bladder UC, 75% present with non-muscle-invasive bladder cancer (NMIBC) at the time of diagnosis, 70% will experience a recurrence within 1 year and 20–30% will progress to muscle-invasive bladder cancer (MIBC)2,3,4. MIBC is associated with a poor prognosis and is the 13th most common cause of mortality worldwide, and its incidence is gradually increasing with population aging5,6.
A variety of treatment options for UC are available, including surgery, intravesical Bacille Calmette-Guerin (BCG) therapy, neoadjuvant/adjuvant chemotherapy, immunotherapy, and multimodal therapy. The selection of an appropriate treatment with respect to the patient and disease characteristics is prognostically important, and accordingly the tumor stage and grade are important criteria for such treatment decisions. However, several other factors can contribute to a treatment decision, including lymphovascular invasion (LVI). LVI, defined as the presence of tumor cells in the lymphatic vessels and vascular wall, can affect the characteristics of UC and may be predictive of the outcome7. In this study, we analyzed differences in prognosis according to the presence or absence of LVI after radical cystectomy without lymph node dissection (LND), which is a rare event, and discussed the clinical and prognostic value of LVI.
Methods
Study sample
The Institutional Review Board at our center approved this retrospective study (H-1707-067-869) and waived the requirement to obtain informed consent from the patients. All research and related protocols used in this study complied with the principles of the Declaration of Helsinki.
We retrospectively reviewed the medical records of 857 patients with N1 or lower UC who underwent radical cystectomy at Seoul National University Hospital from 1991 to 2016, including patients who did not undergo LND. After excluding cases for which the pathologic finding was not UC, 747 patients were included in the analysis.
Study design
We divided the included patients into four groups: N0, N1, non-LVI without LND and LVI without LND. Patients who underwent LND were divided into N0 and N1 groups according to N stage, whereas patients who did not undergo LND were divided into non-LVI and LVI groups according to LVI status.
For diagnostic accuracy, the extracted specimens were reviewed by two experienced genitourinary pathologists. The TNM stage and tumor grade were determined according to the 2010 American Joint Committee on Cancer classification and the 2004 World Health Organization/International Society of Urologic Pathology consensus classifications. We additionally collected clinicopathological information such as age, height, weight, body mass index (BMI), sex, American Society of Anesthesiologists (ASA) physical status, pathologic TNM stage, carcinoma in situ (CIS) status, LVI, margin-positive status, LND enforcement, number of removed lymph nodes, number of positive lymph nodes, and neoadjuvant chemotherapy enforcement. We also collected various oncological data, including the initial recurrence and mortality.
In the absence of any recurrence or metastasis, most patients were followed up every 3 months for 3 years after radical cystectomy, every 6 months during years 4 and 5, and annually thereafter. Each follow-up included routine laboratory and urine testing and urine cytology. Neo-bladder patients also underwent an ultrasonic bladder scan for a residual urine check. Radiological examinations such as computed tomography (CT) and bone scans were performed annually.
Statistical analysis
Regarding the statistical analysis, continuous variables are presented as mean values with standard deviations (SDs) or as median values with interquartile ranges (IQRs). Categorical variables are presented as frequencies of events (%). The primary and secondary endpoints of the study were overall survival (OS) and recurrence-free survival (RFS), respectively, and all survival outcomes were estimated using the Kaplan–Meier method and compared using the log-rank test. A Cox proportional hazard regression analysis was used to identify the predictors of various oncological outcomes. All statistical tests were performed using IBM SPSS Statistics, version 22.0 (IBM, Armonk, NY, USA), and a p-value of <0.05 was considered to indicate statistical significance.
Results
Clinicopathological characteristics of the patients
Table 1 lists the clinicopathological characteristics and oncologic results of the 747 patients included in this study during a median follow-up duration of 41.5 (IQR: 6–311) months. The median age of the patients was 66.0 (IQR: 21–95), and >80% of the subjects were male. The four groups differed with respect to T stage, tumor grade and CIS status. The N1 and LVI groups had a higher frequency of stage T2 and higher cases and a higher tumor grade, compared with the other groups (p = < 0.001 and <0.001, respectively), whereas the LVI group had a significantly lower frequency of CIS cases relative to the other groups (p = 0.007). Additionally, the N1 and LVI groups had significantly higher recurrence and mortality rates, compared with the other groups (p = < 0.001 and <0.001, respectively).
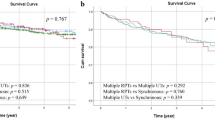
Inter-group comparison of the association of LVI with OS
Figure 1A presents a graph of OS in each of the groups. OS was relatively better in the non-LVI and N0 groups, compared with the LVI and N1 groups. A log-rank comparison confirmed that the N0 and non-LVI groups had significantly better OS outcomes, when compared with the N1 and LVI groups (p = 0.001 and <0.001, and p = 0.012 and <0.001, respectively). However, no significant differences in OS were observed between the N0 and non-LVI groups, or between the N1 and LVI groups.
Intergroup comparison of the association of LVI with RFS
Figure 1B presents a graph of RFS in each of the groups. The results obtained for RFS are similar to those for OS. Specifically, the N0 and non-LVI groups appeared to have better RFS outcomes when compared with the N1 and LVI groups, and a log-rank test confirmed both groups achieved a significantly better RFS than did the N1 and LVI groups (p = < 0.001 and <0.001, and p = < 0.001 and <0.001, respectively). Again, no significant differences in RFS were observed between the N0 and non-LVI groups or between the N1 and LVI groups.
Multivariate regression analysis of significant predictors of OS and RFS in the overall study population
We also performed a multivariate Cox regression analysis to identify significant predictors of OS and RFS after radical cystectomy. Regarding OS, age (hazard ratio [HR]: 1.05; 95% confidence interval [CI]: 1.03–1.06), LVI (HR: 2.50; 95% CI: 1.68–3.70), stage N1 disease (HR: 1.72; 95% CI: 1.11–2.56) and stage T3 (HR: 3.37; 95% CI: 1.30–5.54) or T4 disease (HR: 4.92; 95% CI: 1.38–8.18) were identified as significant predictors. These parameters were also identified as significant predictors of RFS (age, HR: 1.02, 95% CI: 1.00–1.03; LVI, HR: 2.22, 95% CI: 0.343–3.685 N1, HR: 2.07, 95% CI: 1.20–3.58; T3, HR: 3.03, 95% CI: 1.41–6.50 and T4, HR: 4.25, 95% CI: 1.65–10.92) (Table 2).
Significant predictors of OS and RFS in the Nx subgroup population
We finally performed a Cox regression analysis to identify the significant predictors of oncological outcomes (e.g., OS and RFS) in the Nx subgroup without LND. Here, age (HR: 1.04; 95% CI: 1.02–1.06) and LVI (HR: 2.42; 95% CI: 1.51–3.90) were identified as predictors of OS, whereas LVI (HR: 2.04; 95% CI: 0.14–3.66) was the only identified predictor of RFS (Table 3).
Discussion
Whereas previous studies focused on the prognosis and significance of LVI in any subgroup, our study analyzed the prognostic risk of N0 and N1 in the presence of LVI. Accordingly, we analyzed differences in oncological prognosis according to the presence or absence of LVI in the patients who underwent radical cystectomy without LND, as well as differences among pathologically confirmed N0 and N1 patients who underwent radical cystectomy with LND. Furthermore, we evaluated the effects of LVI on the oncological prognosis with respect to lymph node invasion by comparing patients with LVI in the Nx group to those in the N0 and N1 groups. Here, we did not identify the exact difference in oncological prognosis between the LVI and N1 groups and the survival curves of the two groups were similar, with both exhibiting significantly poorer RFS and OS outcomes relative to the N0 group. Similarly, the non-LVI group, which did not differ significantly from the N0 group, had better RFS and OS outcomes when compared with the N1 group. Furthermore, our overall population multivariate Cox regression analysis identified N1, LVI, T stage and age as significant predictors of the oncological prognosis of patients undergoing radical cystectomy. However, in the Nx subgroup multivariate Cox regression analysis, LVI was the only significant predictor of oncological prognosis.
LVI, defined as the presence of tumor cells in small vessels. This process increases the frequency of lymph node metastasis and is an important step in the processes of metastatic spread and cancer cell microcirculation, as8,9,10 cancer cells migrate through the local lymphatics after invading and proliferating the lymphovascular space11. LVI is observed in many types of cancer, and has been identified as an important predictor of poor prognosis in patients with liver, testicular and penile cancer12,13. By contrast, the reported outcomes of LVI in patients with bladder cancer are varied, although the positive outcomes are not yet generally accepted14,15,16,17,18,19.
Previous studies have identified LVI as an independent predictor of OS, CSS and RFS in patients who have undergone radical cystectomy. Bolenz et al. determined that LVI is a significant predictor of OS and RFS in node-negative patients, and that the tumor stage and grade are significant predictors20. In a comparison of node-positive and -negative subgroups, Shariat et al. found that LVI correlated with OS, CSS and RFS in all subgroups and observed that the tumor stage and LN involvement were risk factors for survival14. Hermann et al. also reported that LVI, tumor stage and LN status were important prognostic factors for OS21. However, some studies have reported that LVI only affects the prognosis of patients with N0 disease, and not all radical cystectomy patients. Lotan et al. reported that LVI is an important risk factor for local, distant and overall recurrence in node-negative patients, but not in node-positive patients22. Tilki et al. reported that LVI is associated with recurrence and survival only in patients with pT1N0 disease. Still other studies observed no significant correlation between LVI and survival23,24.
We note that our current research had some limitations. First, this study featured a retrospective design, and the surgeries were performed by four surgeons. Second, although we considered neoadjuvant chemotherapy, we did not consider previous repeated transurethral resection of bladder tumor (TURBT) or intravesical treatment, although these may have affected the outcomes. Third, there may be potential interoperability variability or limitations in setting up a single center. Fourth, the small sample size of patients who did not undergo LND. Fifth, there is variability in follow-up and at the time of test. Sixth, when cystectomy is performed in UC, LND is performed with cystectomy as standard treatment. The absence of LND can be a confounding bias. Seventh, regimens and time from neoadjuvant chemotherapy completion to surgery was not consistent
Conclusion
LVI is an independent predictor of prognosis in patients with bladder UC who have undergone radical cystectomy. Relatively speaking, LVI and N1 are prognostically similar, and both are associated with a poorer prognosis when compared with N0. Therefore, the role of adjuvant chemotherapy or immunotherapy may need to be prospectively evaluated in LVI-positive patients regardless of T stage after radical cystectomy.
References
Torre, L. A. et al. Global cancer statistics, 2012. CA Cancer J Clin. 65, 87 (2015).
Babjuk, M. et al. Reply to Harry Herr’s Letter to the Editor re: Marko Babjuk, Andreas Bohle, Maximilian Burger et al. EAU Guidelines on Non-muscle-invasive Urothelial Carcinoma of the Bladder: Update 2016. Eur Urol 71, E173 2017.
Burger, M. et al. Epidemiology and risk factors of urothelial bladder Cancer. Eur Urol 63, 234 (2013).
Sylvester, R. J. et al. Predicting recurrence and progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: a combined analysis of 2596 patients from seven EORTC trials. Eur Urol 49, 466, discussion: 75 (2006).
Advanced Bladder Cancer Meta-analysis C. Adjuvant chemotherapy in invasive bladder cancer: a systematic review and meta-analysis of individual patient data Advanced Bladder Cancer (ABC) Meta-analysis Collaboration. Eur Urol 48, 189, discussion: 99 (2005).
Yin, M. et al. Neoadjuvant chemotherapy for muscle-invasive bladder cancer: a systematic review and two-step meta-analysis. Oncologist 21, 708 (2016).
Muppa, P. et al. Prognostic significance of lymphatic, vascular and perineural invasion for bladder cancer patients treated by radical cystectomy. Pathology 49, 259 (2017).
Abdel-Latif, M. et al. Nodal involvement in bladder cancer cases treated with radical cystectomy: incidence and prognosis. J Urol 172, 85 (2004).
Alitalo, K., Mohla, S. & Ruoslahti, E. Lymphangiogenesis and cancer: meeting report. Cancer Res 64, 9225 (2004).
Padera, T. P. et al. Lymphatic metastasis in the absence of functional intratumor lymphatics. Science 296, 1883 (2002).
Alexander-Sefre, F. et al. Detection of tumour lymphovascular space invasion using dual cytokeratin and CD31 immunohistochemistry. J Clin Pathol 56, 786 (2003).
Vauthey, J. N. et al. Simplified staging for hepatocellular carcinoma. J Clin Oncol 20, 1527 (2002).
Albers, P. et al. Risk factors for relapse in clinical stage I nonseminomatous testicular germ cell tumors: results of the German Testicular Cancer Study Group Trial. J Clin Oncol 21, 1505 (2003).
Shariat, S. F. et al. International validation of the prognostic value of lymphovascular invasion in patients treated with radical cystectomy. BJU Int 105, 1402 (2010).
Leissner, J., Koeppen, C. & Wolf, H. K. Prognostic significance of vascular and perineural invasion in urothelial bladder cancer treated with radical cystectomy. J Urol 169, 955 (2003).
Ku, J. H. et al. Lymphovascular invasion as a prognostic factor in the upper urinary tract urothelial carcinoma: a systematic review and meta-analysis. Eur J Cancer 49, 2665 (2013).
Kim, H. S. et al. Presence of lymphovascular invasion in urothelial bladder cancer specimens after transurethral resections correlates with risk of upstaging and survival: a systematic review and meta-analysis. Urol Oncol 32, 1191 (2014).
Kim, H. et al. Prognostic significance of lymphovascular invasion in radical cystectomy on patients with bladder cancer: a systematic review and meta-analysis. PLoS One 9, e89259 (2014).
Gondo, T. et al. Risk stratification of survival by lymphovascular invasion, pathological stage, and surgical margin in patients with bladder cancer treated with radical cystectomy. Int J Clin Oncol 17, 456 (2012).
Bolenz, C. et al. Lymphovascular invasion is an independent predictor of oncological outcomes in patients with lymph node-negative urothelial bladder cancer treated by radical cystectomy: a multicentre validation trial. BJU Int 106, 493 (2010).
Herrmann, E. et al. The prognostic impact of pelvic lymph node metastasis and lymphovascular invasion on bladder cancer. Int J Urol 15, 607 (2008).
Lotan, Y. et al. Lymphovascular invasion is independently associated with overall survival, cause-specific survival, and local and distant recurrence in patients with negative lymph nodes at radical cystectomy. J Clin Oncol 23, 6533 (2005).
Hara, S. et al. Prognostic variables in patients who have undergone radical cystectomy for transitional cell carcinoma of the bladder. Jpn J Clin Oncol 31, 399 (2001).
Bassi, P. et al. Prognostic factors of outcome after radical cystectomy for bladder cancer: a retrospective study of a homogeneous patient cohort. J Urol 161, 1494 (1999).
Acknowledgements
This study was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIP) (Grant number: 2016R1A2B4011623). No funders had any role in study concept and design, experiments, analysis of data, writing manuscript, or the decision for publication.
Author information
Authors and Affiliations
Contributions
Hyeong Dong Yuk, Ja Hyeon Ku, Chang Wook Jeong and Hyeon Hoe Kim wrote the main manuscript text and Hyeong Dong Yuk, Cheol Kwak prepared figures and table. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yuk, H.D., Jeong, C.W., Kwak, C. et al. Lymphovascular invasion have a similar prognostic value as lymph node involvement in patients undergoing radical cystectomy with urothelial carcinoma. Sci Rep 8, 15928 (2018). https://doi.org/10.1038/s41598-018-34299-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-34299-6
Keywords
This article is cited by
-
Feasibility analysis of arterial CT radiomics model to predict the risk of local and metastatic recurrence after radical cystectomy for bladder cancer
Discover Oncology (2024)
-
Tumor cell invasion in blood vessels assessed by immunohistochemistry is related to decreased survival in patients with bladder cancer treated with radical cystectomy
Diagnostic Pathology (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.