Abstract
Diffuse large B-cell lymphoma (DLBCL) is an aggressive lymphoma with diverse outcomes. Concurrent translocation of MYC and BCL-2 and/or BCL-6, and concurrent immunohistochemical (IHC) high expression of MYC and BCL-2, have been linked to unfavorable treatment responses. TP53-mutated DLBCL has also been linked to worse outcome. Our aim was to evaluate the aforementioned issues in a cohort of 155 patients uniformly treated with R-CHOP-like therapies. We performed direct sequencing of TP53 exons 5, 6, 7 and 8 as well as fluorescence in-situ hybridization (FISH) of MYC, BCL-2 and BCL-6, and IHC of MYC, BCL-2 and BCL-6. In multivariate analysis, TP53 mutations in L3 and loop-sheet helix (LSH) associated with a risk ratio (RR) of disease-specific survival (DSS) of 8.779 (p = 0.022) and a RR of disease-free survival (DFS) of 10.498 (p = 0.011). In IHC analysis BCL-2 overexpression was associated with inferior DFS (p = 0.002) and DSS (p = 0.002). DLBCL with BCL-2 and MYC overexpression conferred inferior survival in all patients (DSS, p = 0.038 and DFS, p = 0.011) and in patients with non-GC phenotype (DSS (p = 0.013) and DFS (p = 0.010). Our results imply that in DLBCL, the location of TP53 mutations and IHC analysis of BCL-2 and MYC might have a role in the assessment of prognosis.
Similar content being viewed by others
Introduction
Diffuse large B-cell lymphoma (DLBCL) is the most common type of lymphoma in the western countries and is clinically heterogeneous, with subsets of patients having diverse prognoses1. Gene expression profiling (GEP) has been used to classify DLBCL into subgroups by cell of origin (COO): germinal center (GC), activated B-cell (ABC) and a third type which cannot be classified into either categories2. Owing to the high costs of GEP and the requirement of fresh tissue samples, surrogate methods to classify DLBCL into COO subgroups have been developed, e.g. Hans’s IHC algorithm that classifies DLBCLs into two subgroups, GC and non-GC, which includes ABC and the third type2. Double-hit (DH) lymphomas, defined as lymphomas with MYC translocation combined with BCL-2 or BCL6 translocation, are among the most aggressive variants. In the newly revised WHO classification, DH lymphomas were classified in a new class of high-grade B-cell lymphoma3. Double-expressor (DE) DLBCLs (DLBCLs with high protein expression of MYC and BCL-2 but without translocation) were included in the not-otherwise-specified (NOS) category, but were implied to have negative prognostic significance3. A diversity in biology and clinical outcome exists within the individual categories. DH lymphomas are usually clinically very aggressive with poor responses to first-line treatments and with short remissions.
The TP53 tumor suppressor gene located at chromosome region 17p13.1 encodes the p53 protein, which is involved in the regulation of cell cycle, DNA repair, apoptosis, and senescence after various stress signals, such as DNA damage and inflammation4. Loss of p53 function allows proliferation of cells with DNA damage and promotes neoplasia in transgenic p53-null mice5. Wild-type p53 functions as a cell-cycle checkpoint and a sensor of DNA damage in the cell6, and new functions keep emerging such as a role as a suppressor of inflammation7, and regulation of glucose metabolism8.
The TP53 gene is mutated in about 20% of cases of DLBCL9, and most of the published mutations affect p53-DNA interactions, resulting in a partial or complete loss of transactivation functions10. TP53 differs from other tumor suppressor genes in its mode of inactivation. While most tumor suppressor genes are inactivated by mutations leading to absence of protein synthesis or production of a truncated protein, more than 80% of TP53 alterations are missense mutations that lead to the synthesis of a stable full-length protein11. The location of the resulting amino-acid substitution is usually within the central DNA-binding domain (DBD) of p53, resulting in a loss of DNA-binding activity with consequent failure to transcriptionally activate target genes. The most commonly mutated areas in the DBD are loop-sheet-binding helices (LSHs) L2 and L3. Various mutations have different consequences for the function of the p53 protein12,13. Some mutations are associated with a loss of function and others with a gain of function.
Only a small number of studies combining TP53 mutation analysis, translocation data and double-expressor status in DLBCL have been published14. The results of previous studies imply that patients with combined mutation of TP53 and double-hit translocation fare poorly15. Our series is one of the largest investigated to date. In the present study, we pursue the clinical importance of TP53 mutation types combined with translocation and IHC data in patients with DLBCL.
Results
TP53 mutation
Patient characteristics are summarized in Table 1 with comparison between wild-type (WT) and mutated TP53. Out of 155 patient samples all exon sequencings were successful in 80 samples (51.6%). In 26 (16.8%) samples all but one exon were successful. Sequencing was either unsuccessful in more than one exon or totally unsuccessful in 49 samples (31.6%). Nine missense mutations with eight non-functional and one partially functional mutation in TP53 were detected in our patient material. One silent mutation with a synonymous protein product was also detected. The mutations are presented in Table 2. The total mutation frequency was detected 9.6%. In patient material with successful sequencing, 3-year DFS with mutated TP53 was 66.7%, compared with WT TP53, 75.1% (p = 0.494). When comparing 3-year DSS values, the figure for those with mutated TP53 was 66.7% versus WT TP53, 83.2% (p = 0.268). All three lymphoma-related deaths in patients with TP53 mutations were due to primary refractory disease. No relapses were detected in patients with mutated TP53 if initial treatment was successful (WT TP53, 132 patients with 26 relapses and in cases of mutated TP53, 6 patients with 0 relapses, p = 0.594). Structural analysis of mutations showed that two different mutations were present in LSH motifs, one in L3 and the other mutations were localized in β-sheets.
Mutations in LSH and L3 motifs predicted 3-year DSS and DFS (3-year DSS 33.3% versus 83.3% in WT and β-sheet-mutated TP53, p = 0.011, and 3-year DFS 33.3% versus 75.8% in WT and β-sheet-mutated TP53, p = 0.027). Survival data is shown in Fig. 1. Despite very low number of patients and events, in multivariate analysis mutation of LSH and L3 remained an independent prognostic variable as the relative risk of death from lymphoma was 8.779 (95% CI, 1.377 to 55.972, p = 0.022). LSH and L3 mutations were also independent prognostic factors for DFS (RR 10.498; 95% CI, 1.710 to 64.449, p = 0.011). Results should be considered suggestive and with caution due to low numbers in the subgroups.
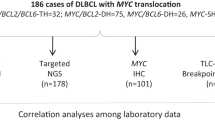
Translocations
FISH for MYC, BCL-2 and BCL-6 translocation was successful in 128/155 cases (82.6%) (Fig. 2). MYC translocations were detected in 11 (8.6%), BCL-2 translocations in 15 (11.7%), BCL-6 translocations in 22 (17.2%) and DH translocations in seven (5.5%) of the 128 cases. Three patients (2.3%) had DH with BCL-2, three patients (2.3%) DH with BCL-6 and one (0.8%) patient had triple-hit lymphoma. MYC translocation did not correlate with any clinical factor. BCL-2 translocation was associated with younger age (p = 0.05). None of the BCL-2 translocation cases were of non-GC phenotype (p = 0.0000002). DH status showed a positive correlation with extranodal disease (p = 0.014).
Gene translocations in DLBCL measured by fluorescent in situ hybridization (FISH). Composite photomicrograph with sections from representative 1 mm tissue microarray cores hybridized with dual color split FISH probes. A yellow fusion signal and red and green split signals in a cell are indicative of gene translocation (arrows). For quantitative analysis the focus must be continuously adjusted hence photographic reproduction is somewhat inaccurate. (A) CMYC. (B) BCL6. (C) BCL2.
MYC translocation predicted neither DFS nor DSS (3-year DFS 70.0% versus 73.5%, p = 0.981 and 3-year DSS 70.0% versus 81.1%, p = 0.687). The figures for BCL-6 translocation were: 3-year DFS 79.1% versus 72.1% (normal BCL-6; p = 0.480) and 3-year DSS 79.1% versus 80.2% (p = 0.845). BCL-2 translocation predicted neither DSS nor DFS (3-year DSS 73.3% versus 80.7%, p = 0.639 and 3-year DFS 60.0% versus 74.7%, p = 0.211). DH status had no prognostic value, as 3-year DFS was 83.3% versus 72.3% (p = 0.527) and 3-year DSS was 83.3% versus 79.6% (p = 0.695).
Immunohistochemistry
IHC GC and non-GC phenotyping was successful in 141 (91.0%) out of 155 samples. IHC evaluation of MYC and BCL-2 was possible in 128 (82.6%) samples and evaluation of BCL-6 in 129 (83.2%) (Fig. 3). A non-GC phenotype was associated with a trend towards worse DSS (3-year DSS 74.6% versus 83.5%, p = 0.123). High MYC expression correlated with an intermediate IPI score, compared with low- and high-risk scores (p = 0.007). High BCL-6 expression was associated with GC phenotype (p = 0.011).
Protein overexpression in DLBCL measured by immunohistochemistry. Composite photomicrograph of representative 1 mm tissue microarray cores. The MYC-, BCL6- and p53 staining patterns are nuclear whereas CD20 shows membranous - and BCL2 cytoplasmic staining patterns. (A) Hematoxylin-eosine staining. (B–F) Immunohistochemical stainings (B) CD20. (C) BCL2. (D) BCL6. (E) MYC. (F) p53.
High MYC (cut-off value 40%) or BCL-6 expression did not predict survival. High expression of BCL-2 was associated with worse DFS and DSS (3-year DFS 58.9% versus 85.9%, p = 0.002 and 3-year DSS 68.0% versus 90.6%, p = 0.002). Patients with DE lymphoma had worse 3-year DFS (57.4% versus 79.1%, p = 0.011) and worse 3-year DSS (66.5% versus 85.2%, p = 0.038). DE did not predict survival in patients with the GC phenotype, but DE status did predict both DSS and DFS in patients with the non-GC phenotype (3-year DSS 54.5% versus 85.4%, p = 0.013 and 3-year DFS 49.5% versus 76.2%, p = 0.010). When using cut-off value of 70% for MYC IHC same correlations were found albeit with better p values.
Immunohistochemical p53 expression was associated with TP53 mutation (p = 0.00017) (Table 3). The sensitivity of high p53 expression to find TP53 mutated cases was 55.6% and specifity 90.8%, respectively. Corresponding positive and negative predictive values were 31.3% and 96.4%, respectively. p53 immunohistochemical expression did not associate with traditional prognostic factors of DLBCL (performance status, IPI, stage, extranodal involvement) nor survival.
Associations between the studied parameters
Only two patients had concurrent TP53 mutation and BCL-2 translocation. TP53 mutations were located in LSH and L3 motifs (p = 0.021). These patients with concurrent BCL-2 translocation and TP53 mutation had very aggressive primary refractory DLBCL with a dismal outcome (mean DSS only 3 months, p = 0.000000002). There were no other associations between TP53 mutation and translocations. High MYC expression was associated with BCL-2 translocation (p = 0.002). MYC translocation was associated with high MYC expression (p = 0.030). MYC translocation was more common in BCL-6 translocated lymphomas (p = 0.022). High BCL-2 expression was associated with BCL-2 translocation (p = 0.011). BCL-2/MYC DE was significantly more common among patients with BCL-2 translocation, as 10 out of a total of 15 BCL-2 -translocated lymphomas had DE and 24 out of a total of 111 without BCL-2 translocation were DE (p = 0.001).
Discussion
TP53 mutations and DH with MYC and BCL-2 have been linked to inferior survival in patients with DLBCL16,17,18,19,20. Only a few studies have reported simultaneous analysis of genetic alterations and immunohistochemical protein expression of these genes21,22,23. Here we report a study describing p53 mutations, MYC, BCL-2 and BCL-6, translocations and immunohistochemical expression in a cohort of 155 newly diagnosed DLBCL cases. In the present study mutations of TP53 in LSH and L3 motifs were the only mutation types that had a strong association with poor survival. Overall, TP53 mutations were not associated with survival. High BCL-2 expression and DE status also had negative prognostic impact. DH translocation did not predict survival, nor did individual translocations. Patients were however few and results should be considered suggestive, interpreted with care and need further validation.
DH status has been established as a major survival predictor in DLBCL, and in the recently revised WHO classification DH DLBCL is categorized as an entity of its own among high-grade lymphomas (HGL)18,22. Many studies have shown that patients with BCL-2 and MYC DH translocation show poor responses to treatment. However, some recent reports have not been able to confirm the very poor prognosis of this group. These discrepancies have been recently presented in a comprehensive review of the literature published by Rosenthal & Yunes24. Moreover, to describe further the biological impact of these translocations it been suggested that patients with MYC translocations should be substratified according to translocation partner23,25,26,27,28. The issue is further complicated by the fact that MYC/BCL-2 and MYC/BCL-6 double hit lymphomas seems to be biologically distinct and probably should be addressed separately24. One study has shown that IHC analysis of BCL-2 and MYC expression might have more prognostic impact than FISH alone18. This implies that mechanisms other than translocation affect protein expression, which is also supported by the fact more patients have high MYC protein expression than translocation. In the present material, DH status and translocations did not predict survival. This might be due to the rarity of these cases. In the present series limited number of patients with DH lymphoma did not allow for substratification according to MYC translocation partner gene. In contrast to this, IHC predicted worse survival in the BCL-2 expression group and in the DE group using cut-off values established in the previous studies of DE29.
In this study we used cut-off value of 40% for MYC positivity, which is used in most previous studies. Work by Ambrosio et al. including a large series of 753 patients with aggressive B-cell lymphoma suggested that cut-off value of 70% might be able to better define the true poor prognosis group of DE lymphomas30. We repeated our analyses with this higher cut-off value also. This change increased the statistical power of established correlations but still we did not find correlations with survival. This discrepancy with the results of Ambrosio et al. may be explained by our smaller cohort.
The mutation frequency of TP53 is considered to be about 20% in de novo DLBCL19,20. Earlier studies of DLBCL have shown that most mutations occur in hot-spot regions, and mutations in LSH and L3 are associated with worse prognosis, while patients with L2 mutations show survival similar to those in WT groups. In a study by Young et al. in the pre-rituximab era concerning a cohort of 477 patients, 102 of the DLBCL cases were TP53-mutated. Mutations in LSH and L3 were associated with worse survival and TP53 mutations in the DBD region were considered markers of poor prognosis19. In a later study by Xu-Monette et al. a rituximab-treated cohort of 506 patients was studied. Of these, 112 patients with mutation of TP53 were detected and mutation was associated with worse prognosis. The study also established IHC-detected p53 as a suitable surrogate marker of mutation. A cut-off value of 50% quantified patients into a probable TP53 mutation group and IHC of p53 was shown to have prognostic potential. Deletion of TP53 was not associated with poor prognosis, only point mutations20. These studies, as well as other studies performed at rituximab era, established that mutations at the DBD region of TP53 were prognostic in regards to survival in DLBCL, regardless of treatment14,21,22.
In the present study, LSH and L3 mutations of TP53 were associated with poor survival. The other TP53 mutations were located in β-sheets (in non-DNA-binding domains) and did not predict survival. LSH and L3 mutations of TP53 mutations were however only detected in three patients and the statistical analysis should be considered with care. Moreover, while the value of p53 pathway in carcinogenesis is evident, the big picture seems to be much more complicated and cover a broader issue than just p53 gene mutations. p53 pathway is a complexed one with over 50 genes and proteins affected. Several genetic events commonly discovered in DLBCL, like ATM (Ataxia telangiectasia mutated) mutations and deletions, MDM2 (murine double minute 2) deletions and ARF (alternate reading frame of CDKN2A locus) loss may induce p53 dysfunction despite unaltered gene31. To add more complexity to the issue, it has been shown in CLL, that patients harboring bi-allelic loss of p53 function have a dismal prognosis32. Recently a large comprehensive study revealing the molecular subtypes of DLBCL, verified the same phenomena in DLBCL as well33. Together these facts imply that a broader approach discovering the genetic landscape of the disease should be preferred in the future.
Patients with TP53 mutations had a high frequency of primary refractory diseases. An interesting finding in our data was, however that among patients with mutated TP53 (n = 10), in whom primary treatment was successful, no relapses were detected. This might imply that these patients would possibly benefit from more intensive primary treatments or from different treatment strategies such as new targeted therapies, e.g. kinase inhibitors idelalisib or ibrutinib. In chronic lymphocytic leukemia, an effect of these drugs has been shown to be independent of functional TP53 genes34,35. In DLBCL ibrutinib has shown promise in treatment of ABC subtypes in a phase-2 trial36. These arising therapies warrant new studies to discover their therapeutic potential in high-risk DLBCL.
In our series TP53 mutation frequency was lower than previously reported, i.e. 12.5% versus 20%, and this difference might be explained by selection bias, because small samples were excluded from the study20. Although difficulties were expected with sequencing of paraffin-embedded samples, the total success rate of sequencing was not optimal. To improve the success ratio, we excluded small biopsy samples, e.g. core needle samples, and only selected the exons that harbour most of the functional mutations. In addition, we divided exons 5 and 8 into two parts to improve the output.
Because gene sequencing is a challenging method to apply to routine clinical practice, it would be attractive to use IHC as a surrogate marker to find the mutated cases. We found that high p53 protein expression correlated with TP53 gene mutations. However, it did not have statistically significant prognostic value, and half of the cases with strong expression had wild type p53 gene. These findings imply that p53 immunohistochemistry might be used for screening of the mutations but is not able to substitute sequencing20.
Here we report results of p53 gene sequencing, MYC, BCL-2 and BCL-6 FISH as well as MYC, BCL-2, BCL-6 and p53 immunohistochemistry in a moderate group of 155 DLBCL cases. Our data suggest that TP53 mutations in LSH and L3, and IHC high expression of BCL-2 and MYC are each independently associated with poor prognosis in patients with DLBCL. The impact of p53 mutations was limited. Together with other existing data, this implies, that in the future studies also the existence of other wild type gene should be taken into account. Although we had a moderate patient population, considering the excellent prognosis of these patients, few events; relapses and disease related deaths occurred. Combining this fact with the rarity of studied molecular features we could not do detailed subgroup analysis and the results should be addressed with caution. However, most of the published studies face this same problem, which should therefore be addressed in a meta-analysis combining several studies. Despite all these limitations we found our study adds knowledge to this field of prognostic impact of molecular events in DLBCL.
Methods
Patients and samples
Paraffin-embedded tissue blocks from diagnostic lymph nodes or extralymphatic tumor-site samples were available from 155 untreated patients with histologically confirmed de novo DLBCL, not otherwise specified. Core needle biopsy samples were excluded on the basis of sample size. Detailed patient information was collected retrospectively in each case. Patients were diagnosed and treated at Oulu and Kuopio University Hospitals and Central Hospital of Central Finland between the years 2003–2011. The patient material was collected from three primary treatment facilities in Finland and overall treatment was uniform in all hospitals. Diagnoses were reviewed by experienced hematopathologists (KMH, YS and JB). Hans’ IHC algorithm was used to stratify DLBCL cases into GC and non-GC phenotypes2. The diagnostic work-up included medical history, physical examination, blood chemistry, bone marrow biopsy, and whole body computed tomography. Primary treatment for all patients was CHOP-like therapy combined with rituximab. The Ethics Committee of the Northern Ostrobothnia Hospital District approved the study design (Approval Number 42/2010, date 23 June 2010). The ethics committee waived the need to obtain informed consent. All experiments were performed in accordance with relevant guidelines and regulations.
Microdissection and DNA isolation
DNA was obtained from paraffin-embedded tissue sections. Sections were cut into 10 µm-thick slices and mounted on polyethylene naphthalate (PEN) membrane-coated slides (P.A.L.M. Microlaser Technologies, Germany). Tissues sections were analyzed by experienced hematopathologists (KMH and JB) and areas with tumor tissue were marked and cut out using the P.A.L.M. Robot-microlaser system (P.A.L.M. Microlaser Technologies) with assistance of pressure catapulting according to the instructions of the manufacturer.
TP53 mutation analysis
Direct sequencing (ABI3130 Genetic Analyzer, Applied Biosystems, CA, USA) of tumor-derived DNA was performed for TP53 exons 5, 6, 7 and 8 based on the sequence information (NG_017013.2, NM_000546.5) obtained from the NCBI public database. Six primer pairs (Table 4) were used in the PCR amplification with AmpliTaq-Gold® (Applied Biosystems) and in BigDye terminator v.1.1 cycle sequencing reactions (Applied Biosystems). For exons 5 and 8, two sets of primers were used in order to keep the PCR product sizes small (<200 bp) and thus suitable for sequence analysis of fragmented DNA. The PCR and sequencing reaction conditions are available upon request. All the sequencing reactions were carried out in both forward and reverse directions and any unclear results were confirmed by re-sequencing of the sample. PCR products were purified using ExoSAP-IT® (Affymetrix) or ExoStar™ (Illustra) one-step cleanup reactions. The sequencing reaction cleanup was performed with basic ethanol/EDTA precipitation. All the sequence data was analyzed with CodonCodeAligner v4.1.1 (CodoneCode Corporation) and Sequence Scanner v1.0 (Applied Biosystems) software. IARC database version R18, April 2016 was used to analyze the mutational data37.
IHC staining and FISH
Immunostaining and fluorescence in situ hybridization (FISH) analyses were performed as previously described25,38,39. For these stainings, tissue microarrays were constructed40.
For IHC the following monoclonal antibodies were used in accordance with the manufacturer’s instructions. Monoclonal Rabbit Anti-Human c-MYC, clone EP121, dilution 1:100, Epitomics, CA, USA; Monoclonal Mouse Anti-Human BCL-2, clone124, dilution 1:100, Flex, Dako, Denmark; Monoclonal Mouse Anti-Human BCL-6, clone PG-B6p, RTU, Flex+, Dako, Denmark: Monoclonal Mouse Anti-Human p53 protein, clone DO-7, Flex, Dako, Denmark.
MYC, BCL-2 and BCL-6 protein expression was evaluated as a percentage of cells stained in 10-unit intervals. Previously described cut-off values were used for regards BCL-6 (50%), MYC (40%), BCL2 (70%)29 and p53 (50%)39.
Cut-off values were used to divide patients into high- and low-expression groups. Double-expressor (DE) lymphomas were defined as lymphomas with high expression irrespectively to the existence of gene translocations. The cut-off value used were BCL-6 staining over 50%, BCL-2 staining over 70% of the cells positive. For MYC IHC we performed analyses with both the cut-off value of 70% and 40%. The results are given mainly with the latter one.
The following FISH probes were used in accordance with the instructions of the manufacturer. BCL2 FISH DNA Probe, Split Signal, Code Y5407, Dako, Denmark; BCL6 Breakapart probe, LPH 035, Cytocell, United Kingdom; MYC FISH DNA Probe, Split Signal, Code Y5410, Dako, Denmark.
DH lymphomas were defined as those with concurrent MYC and BCL-2 or BCL-6 translocation. Triple-hit lymphomas were defined as lymphomas with MYC translocation combined with both BCL-2 and BCL-6 translocation.
Statistical analysis
Associations between the different variables and clinical parameters were assessed by using Pearson’s 2-sided chi-square test. Kaplan–Meier analyses were used to assess survival rates and log-rank tests were used to determine the statistical significance. Disease-specific survival (DSS) was calculated from the date of diagnosis to the date of lymphoma-related death or the last follow-up date. Overall survival (OS) was calculated from the date of diagnosis to death from any cause or last follow-up. Disease-free survival (DFS) was calculated from the date of diagnosis to the date of relapse or date of death from any cause, or last follow-up date, whichever occurred first. p-values < 0.05 were considered significant. To evaluate the independent prognostic potential, all significant associations with survival in univariate analysis were analyzed by means of Cox regression using the enter method. The model included International Prognosis Index (IPI) divided into three categories according to risk, lactate dehydrogenase, Eastern Cooperative Oncology Group (ECOG) performance status, Ann Arbor stage, age, B-symptoms and extranodal involvement. The three IPI categories were as follows: low 0–1, intermediate, 2–3 and high risk, 4–5. Lactate dehydrogenase categories were normal and high. ECOG performance status categories were 0 or 1 and 2, 3 or 4. Ann Arbor-stage categories were Stages I–II and III–IV. Age categories were under 60 and 60 or more. B-symptom categories were no and yes. Extranodal involvement was divided to no extranodal disease or extranodal involvement. All statistical analyses were performed using the Statistical Package for the Social Sciences, v. 22.0 (IBM SPSS, Chicago, IL, USA).
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Nogai, H. et al. Pathogenesis of non-Hodgkin’s lymphoma. J. Clin. Oncol. 29, 1803–1811 (2011).
Hans, C. P. et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood 103, 275–282 (2004).
Swerdlow, S. H. et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood 127, 2375–2390 (2016).
Bensaad, K. et al. P53: New roles in metabolism. Trends Cell. Biol. 17, 286–291 (2007).
Donehower, L. A. et al. Mice deficient for p53 are developmentally normal but susceptible to spontaneous tumours. Nature 356, 215–221 (1992).
Sengupta, S. et al. p53: Traffic cop at the crossroads of DNA repair and recombination. Nat. Rev. Mol. Cell. Biol. 6, 44–55 (2005).
Xue, W. et al. Senescence and tumour clearance is triggered by p53 restoration in murine liver carcinomas. Nature 445, 656–660 (2007).
Gottlieb, E. et al. P53 regulation of metabolic pathways. Cold. Spring. Harbor. Perspect. Biol. 2, a001040 (2010).
Young, K. H. et al. Mutations in the DNA-binding codons of TP53, which are associated with decreased expression of TRAILreceptor-2, predict for poor survival in diffuse large B-cell lymphoma. Blood 110, 4396–4405 (2007).
Haupt, S. et al. Mutant p53 drives cancer by subverting multiple tumor suppression pathways. Front. Oncol. 6, 12 (2016).
Soussi, T. et al. Assessing TP53 status in human tumours to evaluate clinical outcome. Nat. Rev. Cancer 1, 233–240 (2001).
Soussi, T. et al. P53 mutation heterogeneity in cancer. Biochem. Biophys. Res. Commun. 331, 834–842 (2005).
Kato, S. et al. Understanding the function-structure and function-mutation relationships of p53 tumor suppressor protein by high-resolution missense mutation analysis. Proc. Natl. Acad. Sci. USA 100, 8424–8429 (2003).
Clipson, A. et al. The prognosis of MYC translocation positive diffuse large B-cell lymphoma depends on the second hit. J. Pathol. Clin. Res. 1, 125–133 (2015).
Wang, X. J. et al. 53 expression correlates with poorer survival and augments the negative prognostic effect of MYC rearrangement, expression or concurrent MYC/BCL2 expression in diffuse large B-cell lymphoma. Mod. Pathol. 30, 194–203 (2017).
Johnson, N. A. et al. Lymphomas with concurrent BCL2 and MYC translocations: The critical factors associated with survival. Blood 114, 2273–2279 (2009).
Cheung, K. J. et al. The significance of TP53 in lymphoid malignancies: Mutation prevalence, regulation, prognostic impact and potential as a therapeutic target. Br. J. Haematol. 146, 257–269 (2009).
Horn, H. et al. MYC status in concert with BCL2 and BCL6 expression predicts outcome in diffuse large B-cell lymphoma. Blood 121, 2253–2263 (2013).
Young, K. H. et al. Structural profiles of TP53 gene mutations predict clinical outcome in diffuse large B-cell lymphoma: An international collaborative study. Blood 112, 3088–3098 (2008).
Xu-Monette, Z. Y. et al. Mutational profile and prognostic significance of TP53 in diffuse large B-cell lymphoma patients treated with R-CHOP: Report from an international DLBCL rituximab-CHOP consortium program study. Blood 120, 3986–3996 (2012).
Schiefer, A. I. et al. Impact of single or combined genomic alterations of TP53, MYC, and BCL2 on survival of patients with diffuse large B-cell lymphomas: A retrospective cohort study. Medicine (Baltimore) 94, e2388 (2015).
Fiskvik, I. et al. Combining MYC, BCL2 and TP53 gene and protein expression alterations improves risk stratification in diffuse large B-cell lymphoma. Leuk. Lymphoma 56, 1742–1749 (2015).
Sarkozy, C. et al. Double-hit and double-protein-expression lymphomas: aggressive and refractory lymphomas. Lancet Oncol. 16, e555–e567 (2015).
Rosenthal, A. & Younes, A. High grade B-cell lymphoma with rearrangements of MYC and BCL2 and/or BCL6: Double hit and triple hit lymphomas and double expressing lymphoma. Blood Rev. 31, 37–42 (2017).
Pedersen, M. Ø. et al. MYC translocation partner gene determines survival of patients with large B-cell lymphoma with MYC- or double-hit MYC/BCL2 translocations. Eur. J. Haematol. 92, 42–48 (2014).
Vitolo, U. et al. Obinutuzumab or Rituximab Plus CHOP in Patients with Previously Untreated Diffuse Large B-Cell Lymphoma: Final Results from an Open-Label, Randomized Phase 3 Study (GOYA). Blood 128, 470 (2016).
Copie-Bergman, C. et al. MYC-IG rearrangements are negative predictors of survival in DLBCL patients treated with immunochemotherapy: A GELA/LYSA study. Blood 126, 2466–2474 (2015).
Campo, E. MYC in DLBCL: Partners matter. Blood 126, 2439–2440 (2015).
Johnson, N. A. et al. Concurrent expression of MYC and BCL2 in diffuse large B-cell lymphoma treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone. J. Clin. Oncol. 30, 3452–3459 (2012).
Ambrosio, M. A. et al. MYC protein expression scoring and its impact on the prognosis of aggressive B-cell lymphoma patients. Haematologica In press (2018).
Tessoulin, B. et al. p53 dysregulation in B-cell malignancies: More than a single gene in the pathway to hell. Blood Rev. 31, 251–259 (2017).
Marinelli, M. et al. Identification of molecular and functional patterns of p53 alterations in chronic lymphocytic leukemia patients in different phases of the disease. Haematologica. 98, 371–375 (2013).
Chapuy, B. et al. Molecular subtypes of diffuse large B cell lymphoma are associated with distinct pathogenic mechanisms and outcomes. Nat. Med. 24, 679–690 (2018).
Farooqui, M. Z. et al. Ibrutinib for previously untreated and relapsed or refractory chronic lymphocytic leukaemia with TP53 aberrations: A phase 2, single-arm trial. Lancet Oncol. 16, 169–176 (2015).
Thijssen, R. et al. The pan phosphoinositide 3-kinase/mammalian target of rapamycin inhibitor SAR245409 (voxtalisib/XL765) blocks survival, adhesion and proliferation of primary chronic lymphocytic leukemia cells. Leukemia 30, 337–345 (2016).
Wilson, W. H. et al. Targeting B cell receptor signaling with ibrutinib in diffuse large B cell lymphoma. Nat. Med. 21, 922–926 (2015).
Bouaoun, L. et al. TP53 variations in human cancers: New lessons from the IARC TP53 database and genomics data. Hum. Mutat. 37, 865–876 (2016).
Pedersen, M. Ø. et al. Real world data on young patients with high-risk diffuse large B-cell lymphoma treated with R-CHOP or R-CHOEP - MYC, BCL2 and BCL6 as prognostic biomarkers. PLoS. One 12, e0186983 (2017).
Pedersen, M. Ø. et al. Double-hit BCL2/MYC translocations in a consecutive cohort of patients with large B-cell lymphoma - a single centre’s experience. Eur. J. Haematol. 89, 63–71 (2012).
Kononen, J. et al. Tissue microarrays for high-throughput molecular profiling of tumor specimens. Nat. Med. 4, 844–847 (1998).
Acknowledgements
The financial support of the Finnish Anti-tuberculous association is greatly appreciated. The authors are grateful to the Immunohistochemistry and FISH labs at the Pathology Dept., Herlev Hospital for performing IHC and FISH analyses.
Author information
Authors and Affiliations
Contributions
P.P., E.J. and K.V. were responsible for patient data collection. P.P., M.P., P.N., T.M., K.M.H. and K.R. carried out experiments. P.P. and O.K. drafted the manuscript. P.P., P.K., M.P., P.N. and O.K. analysed data. All authors were involved in planning and writing the paper and had approval of the submitted manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Peroja, P., Pedersen, M., Mantere, T. et al. Mutation of TP53, translocation analysis and immunohistochemical expression of MYC, BCL-2 and BCL-6 in patients with DLBCL treated with R-CHOP. Sci Rep 8, 14814 (2018). https://doi.org/10.1038/s41598-018-33230-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-33230-3
Keywords
This article is cited by
-
Follicular lymphoma and marginal zone lymphoma: how many diseases?
Virchows Archiv (2023)
-
Real-world routine diagnostic molecular analysis for TP53 mutational status is recommended over p53 immunohistochemistry in B-cell lymphomas
Virchows Archiv (2023)
-
The Role of Immunohistochemical Overexpression of p53 as Adverse Prognostic Factor in Primary Testicular Diffuse Large B Cell Lymphoma
Pathology & Oncology Research (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.