Abstract
Adhesion is a significant concern after surgery. Many researchers studied the anti-adhesive effect of statin, of which results were inconsistent. Thus, we purposed to perform a systematic review and meta-analysis to evaluate the effect of statins on postoperative adhesion in an experimental study. A comprehensive search was conducted using MEDLINE, EMBASE, and Google Scholar to identify animal studies that investigated the postoperative anti-adhesive effect of statins applied at the surgical area. Primary outcome measure was gross adhesion score. Secondary outcomes included microscopic adhesion score and tissue plasminogen activator (t-PA) activity. Totally, 298 rats from 9 animal studies (172 rats received statin therapy and 126 rats received placebo or no treatment) were included in the final analysis. The combined results showed that gross and microscopic adhesion scores were significantly lower in the statin group in comparison to the control group (standardized mean difference [SMD] = 1.65, 95% confidence interval [CI]: 1.02 to 2.28, Pchi2 < 0.001, I2 = 77.9%; SMD = 1.90, 95% CI: 1.10 to 2.79, Pchi2 < 0.001, I2 = 84.5%, respectively). However, there was no evidence of a difference in t-PA activity (SMD = −3.43, 95% CI: −7.95 to 1.09, Pchi2 < 0.001, I2 = 95.5%). In conclusion, statins were effective in preventing postoperative adhesion, as assessed based on gross and microscopic adhesion scores in rats.
Similar content being viewed by others
Introduction
Postoperative adhesion formation remains a major cause of morbidities such as bowel obstruction, infertility, and subsequent persistent pain1,2,3,4. Furthermore, subsequent adhesion-related hospital readmissions and reoperations impose a significant social and economic burden5.
Various strategies have been employed for the prevention of postoperative adhesion formation including abdominal tissue manipulation and irritation reduction5, mechanical barriers such as different film types6, solutions or different gel types7, chemical barriers such as heparin8, non-steroidal anti-inflammatory agents9, fibrinolytic agents10, thrombin-activated fibrinolysis inhibitors11, and a combination of mechanical and chemical barriers12. However, no method has proven to prevent adhesion consistently and completely.
Despite the use of anti-adhesive agents, postoperative adhesion rates remain high13.
Adhesion formation is triggered by trauma to the surgery area. Surgical trauma induces an inflammatory response that leads to activation of the extrinsic pathway of the coagulation cascade, resulting in fibrosis14. Under normal conditions, fibrosis is resolved by fibrinolysis. The process of fibrinolysis is mediated by the enzyme plasmin, which is derived from its inactive substrate plasminogen via tissue-type plasminogen activator (t-PA). t-PA is inhibited by plasminogen activator inhibitor-1 (PAI-1)15,16. However, under ischemic or inflammatory conditions such as surgery, the fibrinolytic system is suppressed and fibroblasts assemble into dense adhesions17. This, in turn, disturbs the balance between t-PA and PAI-1, resulting in increased adhesion formation18.
The family of statins, 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors, has largely been used in patients with atherosclerotic disease and hyperlipidemia. Various experimental studies have shown that statins also have antioxidant, anti-inflammatory, and pro-fibrinolytic properties19, all of which may play a role in the process of adhesion formation and prevention. Thus, statins theoretically have the potential to prevent postoperative adhesion.
Though several studies have investigated the anti-adhesive effect of statins following surgery, the results have been inconsistent. There are currently no systematic review and meta-analysis on the postoperative anti-adhesive effects of statins. Therefore, our objective was to identify and summarize the currently available data from animal studies investigating the anti-adhesive effects of statins after surgery.
Results
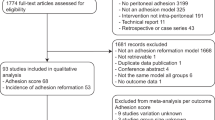
Sixty-eight records were found using OVID-MEDLINE, EMBASE, and Google Scholar and 6 were identified through manual searches. After adjusting for duplicates, 71 studies remained. Of these, 58 studies that did not align with the aim of our meta-analysis were excluded following a review of the titles and abstracts. The full texts of the remaining 13 studies were reviewed in detail, and 4 studies were excluded for the following reasons: oral use of statins (n = 3)20,21,22 and use in clinical setting (n = 1)23.
Thus, 9 studies with a total of 298 rats (172 rats received statin therapy and 126 rats received placebo or no treatment) met the inclusion criteria and were included in this systematic review and meta-analysis (Fig. 1).
Study characteristics
The characteristics of the included studies are shown in Table 1. The studies investigated the effects of simvastatin24,25,26, atorvastatin27,28,29, rosuvastatin30,31, and lovastatin and atorvastatin17. The surgeries performed included laparotomy (cecum)17,24,26,28,29, laparotomy (uterine)27, femoral condyle surgery30, and laminectomy25,31. Male Wistar rats17,24,26,28,29,31, female Wistar rats27, and male Sprague-Dawley rats25,30 were used.
Three studies with multiple groups had two eligible groups for comparison25,26,31 and two studies with multiple groups had three eligible groups for comparison27,28, in which only eligible groups were selected and included in our meta-analysis. In one study with four groups29, we produced two sub-studies having two each groups depending on whether a sodium hyaluronate/carboxymethylcellulose membrane was applied to both statin and control groups, or not. In two sub-studies, two independent investigations were performed. In four studies17,27,28,30, there were two eligible statin groups comparing control group, respectively. We combined the two statin groups to create a single pair-wise comparison to avoid the unit-of-analysis error.
Gross adhesion score
Gross adhesion scores were reported in all studies. These scores were reported on a 5-point scale24,26,28, 4-point scale25,30, or 4-point and 5-point scales27,29 and number of ischemic buttons with attached adhesions17. The definitions for gross adhesion score in each study are described in Table 2. The combined results showed that gross adhesion score was significantly lower in the statin group (SMD = 1.65, 95% CI: 1.02 to 2.28, Pchi2 < 0.001, I2 = 77.9%; Fig. 2).
As the result of subgroup analysis according to the surgery type, gross adhesion score was significantly lower in statin group for laparotomy (SMD 1.32, 95% CI: 0.74 to 1.90, Pchi2 = 0.001, I2 = 73.8%). For laminectomy, there was no significant difference (SMD 3.70, 95% CI: −1.33 to 8.72, Pchi2 < 0.001, I2 = 90%), but the values of effect size and I2 increased. Sensitivity analyses through the sequential removal of one study at a time did not alter the significance (Fig. 3).
Fibrosis microscopic adhesion score
Fibrosis microscopic adhesion scores were reported in 6 studies24,25,27,28,30,31. The definitions for microscopic adhesion score used in each study are described in Table 2. The combined results showed that microscopic adhesion score was significantly lower in the statin group than in the placebo group (SMD = 1.90, 95% CI: 1.01 to 2.79, Pchi2 = 0.001, I2 = 76.6%; Fig. 4).
As a result of subgroup analysis according to the surgery type, microscopic adhesion score was significantly lower in statin group for both laparotomy and laminectomy, respectively (SMD 2.07, 95% CI: 0.57 to 2.80, Pchi2 = 0.122, I2 = 52.4% in laparotomy; SMD 2.14, 95% CI: 0.48 to 3.81, Pchi2 = 0.110, I2 = 61% in laminectomy). Sensitivity analyses by removing one study at a time did not change the significance of the results.
t-PA activity
t-PA activity was reported in two studies17,26. The combined results showed no evidence of a difference (SMD = −3.43, 95% CI: −7.95 to 1.09, Pchi2 < 0.001, I2 = 95.5%; Fig. 5).
Methodological quality and publication bias
A summary of the methodological quality assessment for each study is shown in Table 3. The methodological quality scores ranged from 3 to 5, with 5 studies scoring 4 or 5 points. Publication bias was not analyzed since the number of included studies was less than 10.
Discussion
In the present study, statins applied at the surgical area reduced postoperative adhesion with respect to the evaluation of macroscopic adhesion and microscopic fibrosis scores. t-PA activity during the postoperative period was lower in the statin group, although this difference was not statistically significant.
Postoperative adhesions remain a significant problem for patients and surgeons as they can cause bowel obstruction, infertility, subsequent persistent pain, reoperation, and hospital readmissions1,2,3,4. The presence of adhesions has also been reported to be the greatest risk factor for bowel resection in patients with small bowel obstruction32. Furthermore, postoperative adhesion imposes a significant social and economic burden5; costs reportedly exceed $1 billion in the United States alone annually33.
To prevent or reduce postoperative adhesion, various strategies have been investigated: (1) techniques to reduce tissue manipulation and irritation5, (2) mechanical barriers6,7, (3) chemical barriers8,9,10,11, and (4) a combination of mechanical and chemical barriers12. However, none of these strategies have proven to be consistently and completely effective. One study reported that despite the use of anti-adhesive agent and improvement in surgical techniques, the overall incidence of adhesion-related readmissions has not diminished13. In this study, despite the use of Seprafilm, postoperative adhesion was prevented in only 51% of patients, and dense adhesions formed in 15% of patients13. Further, the cumulative risk of adhesive small bowel obstruction following abdominal surgery and readmission risk due to adhesion following colorectal surgery remain high (approximately 30%)34,35.
Adhesion formation is induced by trauma to the surgical area, initiating an inflammatory response. This inflammatory response activates the extrinsic pathway of the coagulation cascade via up-regulation of the expression of tissue factors by macrophages and mesothelial cells, resulting in the formation of a fibrin-rich inflammatory exudate14. Although fibrinolysis can resolve these fibrin bands under normal conditions, fibrinolysis is reduced under the ischemic or inflammatory conditions that accompany local damage to the surgically injured area. The suppression of fibrinolysis facilitates the infiltration of inflammatory cells and fibroblasts into the fibrin bands, causing the bands to organize into persistent dense adhesions17. The process of fibrinolysis, primarily the degradation of fibrin bands, is driven by the enzyme plasmin, which is converted from its inactive substrate plasminogen by t-PA and urokinase-type plasminogen activator (u-PA). Of those, tPA is the primary plasminogen activator synthesized in the abdomen by mesothelial cells and is responsible for 95% of the plasminogen conversion. tPA is inactivated by PAI-1 and PAI-215,16. Intra-abdominal surgery can cause local damage to the peritoneum and induce inflammatory and ischemic conditions. It has also been observed to decrease t-PA and increase PAI-1 and PAI-2, resulting in inadequate peritoneal fibrinolysis and increase in fibrin exudates and adhesion formation18.
The family of statins, 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors, which catalyze the rate-limiting step in hepatic cholesterol, has been largely used in patients with atherosclerotic disease and hyperlipidemia. They also reportedly possess antioxidant, anti-inflammatory, and pro-fibrinolytic properties19, all of which may play a role in the process of adhesion formation and prevention. Further, statins have been shown to be potent modulators of fibrinolysis under both normal and inflammatory conditions36.
The fibrinolytic effects of statins have been demonstrated in human peritoneal mesotheslial cells36,37, human vascular smooth muscle cells38, and rabbit renal mesangial cells39. Statins were reported to stimulate fibrinolytic activity by significantly increasing t-PA levels and reducing PAI-1 levels37. Thus, statins theoretically have the potential to prevent postoperative adhesion. The findings in our meta-analysis confirmed the favorable effect of statins with regard to gross adhesion and microscopic fibrosis scores. However, inconsistent results exist in the literature regarding the oral administration of statins for the prevention of adhesion formation. Some experimental studies reported that oral simvastatin or fluvastatin reduced fibrosis in rotator cuff tears or laparotomy, respectively21,22, whereas there was studies reporting that oral simvastatin did show no effect on the fibrinolytic pathway in rats and human20,40.
The precise mechanism of postoperative adhesion is not clear yet. One of the suggested mechanism by which statins function to prevent intra-abdominal adhesion is increased t-PA and reduced PAI-1 levels. Aarons et al. reported that the intraperitoneal administration of atorvastatin and lovastatin significantly increased t-PA and mRNA levels and t-PA activity in the peritoneum17. Additionally, Kucke et al. reported that reduced adhesion was associated with increase in t-PA levels in the abdominal cavity26. Haslinger et al. demonstrated that simvastatin enhanced the fibrinolytic capacity of the human mesothelial cells at peritoneum where t-PA was activated and PAI-1 production was inhibited37. They reported that geranylgeranyl-modified intermediates and actin skeleton perturbation were mediated in this mechanism37. However, our meta-analysis could not confirm the association between t-PA activity and statins. This might be due to the lack of studies, since only two studies reported on t-PA activity. However, it is also possible that t-PA was not involved or bypassed the mechanism by which statins operate to prevent adhesion. Although the role of t-PA has been strongly implicated, in clinical practice, fibrinolytic agents and thrombin-activated fibrinolysis inhibitors continue to be suggested as chemical barriers, resulting in inconsistent outcomes11,41.
In terms of pathophysiology of epidural adhesion after laminectomy, there is a bit different point from abdominal adhesion. Songer et al. suggested that the replacement of epidural fat by a hematoma would cause epidural fibrosis4. Some researchers reported that a posterior invasion of fibroblast from the erector spinal muscle would cause peridural and epidural adhesion after laminectomy42. Most surgery type was laparotomy in included studies in our meta-analysis, but laminectomy also was performed in two studies. Hence, we conducted subgroup analysis according to surgery type, laparotomy and laminectomy. The significance of the results from macroscopic and microscopic adhesion scores did not change for laparotomy. On the other hand, macroscopic score was comparable for laminectomy although microscopic score was still higher in statin group. Epidural fibrosis after laminectomy should be based on both gross and microscopic evaluation, while macroscopic evaluation for intra-abdominal fibrosis after laparotomy may have a larger portion compared to microscopic evaluation. Given this, we suggest that statin can be beneficial for the adhesion following laminectomy as well as laparotomy.
We expect that our findings from this meta-analysis of animal studies will present the possibility and necessity of clinical research regarding anti-adhesive effect of statin, especially application of statin to the surgical site. Indeed, there are many trials to develop materials containing statin applying surgical site43, which would be actually beneficial for the prevention of postoperative adhesion. It can provide the valuable evidence to research the effect of statin on postoperative adhesion for patients having statin due to dyslipidemia. There was a pilot clinical study investigating the effect of oral simvastatin after colorectal surgery40. There was no anti-adhesive effect of statin in this study, but further and more clinical trials are required.
The present meta-analysis has several limitations. First, we could not include human clinical studies. The postoperative macroscopic adhesion score, which is the primary end point of this study, cannot be confirmed without operation except in special cases. Thus, for ethical reasons, randomized controlled studies are not possible. Only one study of retrospective data, which examined 419 patients admitted with intraperitoneal adhesion in one institution, reported that history of statin use significantly reduced the need for reoperation23.
Secondly, significant heterogeneity was observed between the included studies. Therefore, although our meta-analysis showed that statins are effective for the prevention of postoperative adhesion with respect to gross and microscopic adhesion scores, these results should be cautiously interpreted. However, sensitivity analyses, conducted through the removal of one study at a time, suggest that this had no impact on the statistical significance. Finally, the present meta-analysis included only a small number of available studies. Additional well-designed, large studies will provide the information necessary to further elucidate the issues presented here. Nevertheless, notwithstanding these limitations, we applied rigorous methodology to provide the first systematic review to examine the anti-adhesive effects of statins.
In conclusion, although this meta-analysis does have some limitations, our study demonstrates that statins applied at the surgical area may be effective for the prevention of postoperative adhesion with respect to gross and microscopic adhesion scores. However, clinical studies performed in large patient populations and well-designed large animal studies are required to determine the impact of statins on postoperative adhesion.
Methods
The present systematic review and meta-analysis was conducted according to the protocol recommended by the Cochrane Collaboration44 and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines45.
Literature search
Two authors (GJ Choi and D Lee) independently carried out database searches using OVID-MEDLINE, EMBASE, and Google Scholar in March 2017, which was updated in September 2017. There were no language restrictions in the search criteria. The reference lists of the eligible publications were also searched manually to further identify relevant publications. The search strategy, which included a combination of free text, Medical Subject Headings, and EMTREE terms, is given in detail in the Appendix.
Study selection
The inclusion and exclusion criteria of this study were determined before conducting the systematic search. All animal studies that compared statins applied to the surgical site (statin group) with control group for the prevention of adhesion following surgery were included. Review articles, case reports, case series, letters to the editor, commentaries, proceedings, laboratory science studies, and any other non-relevant studies were excluded. Two authors (HK Park and DS Kim) independently reviewed the titles and abstracts of the reports identified in the search described above. If a report was determined eligible from the title or abstract, the full paper was retrieved. Potentially relevant studies chosen by at least one author were retrieved, and the full-text versions were evaluated. Two authors (HK Park and DS Kim) held discussions to reach consensus on which studies to include. Disagreements over inclusion or exclusion were settled through discussion with the third investigator (H Kang).
Methodological quality and publication bias
Methodological quality of the selected studies was assessed based on statements of (1) random allocation into treatment and control groups, (2) husbandry conditions (e.g., light/dark cycle, temperature, access to water, and environmental enrichment), (3) compliance with animal welfare regulations, and (4) potential conflicts of interests and whether the study appeared in a peer-reviewed publication. Two authors (GJ Choi and D Lee) independently evaluated the studies and scored each on a scale from 0 to 5. Conflicting evaluations were resolved through the third investigator (H Kang). Publication bias was assessed but not analyzed when the number of included studies was less than 10.
Outcome measure
We recorded outcomes according to intention to treat analysis where available. The primary outcome measure of this meta-analysis was the severity of adhesion under macroscopic evaluation (gross adhesion). The secondary outcome measure was the severity of fibrosis under microscopic evaluation and t-PA activity.
Data extraction
All interrelated data from the included studies were independently extracted and entered into standardized forms by two authors (HK Park and DS Kim), and then cross-checked. Discrepancies were resolved through discussion. If an agreement could not be reached, issues were resolved with the aid of a third investigator (D Lee).
We treated the administration of statin at the surgical site as the statin group regardless of its type, dose, or administered method, and we did the administration of placebo and nothing as the control group. We combined all of the statin groups if a given study had more than one statin group which are eligible for comparison46. We extracted data from partial groups that were eligible in a study with multiple groups if the groups were comparable. When a material such as film, membrane, and sponge was equally applied or not applied to both statin and control group in a single study with multiple groups more than four, data were extracted to effectively yield to sub-studies of whether the material was used or not. The standardized form included the following items: (1) title, (2) name of first author, (3) name of journal, (4) year of publication, (5) type of animal studied, (6) type of surgery performed, (7) interventions in control group, (8) interventions in experimental group, (9) definition of gross adhesion score, (10) definition of microscopic adhesion score (11) severity and extent of gross adhesion, (12) severity of fibrosis, and (13) t-PA activity.
The data were initially extracted from tables or text. In cases involving missing or incomplete data, an attempt was made to contact the study authors to obtain the relevant information.
Statistical analysis
We conducted this meta-analysis using the Comprehensive Meta-Analysis software (version 2.0; Biostat, Englewood, NJ, USA). Two authors (GJ Choi and H Kang) independently inputted all data into the software. The standardized mean differences (SMDs) and their 95% confidence intervals (CIs) were calculated for each outcome. We used the chi-squared test for homogeneity and the I2 test for heterogeneity. A P < 0.1 for the chi-squared statistic was used to indicate statistical significance. An I2 greater than 50% was considered to indicate significant heterogeneity. For P-values < 0.10 and the I2 values < 50%, fixed effects models were used, and for I2 values > 50%, random effects models were used47.
Since the combined number of studies that showed substantial heterogeneity were less than 10, t-statistics (Hartung-Knapp-Sidik-Jonkman method) were used instead of Z-tests in all random effects analysis in order to lower the error rate48.
We conducted subgroup analysis according to the surgery type. We also conducted sensitivity analysis on outcomes with significant heterogeneity. If the reported data were medians (P25–P75), medians (ranges) or means (standard error of means), means and standard deviations were calculated from these values49.
Data Availability
All data generated or analysed during this study are included in this published article (and its Supplementary Information files).
References
Menzies, D. Postoperative adhesions: their treatment and relevance in clinical practice. Annals of the Royal College of Surgeons of England 75, 147–153 (1993).
Ellis, H. The clinical significance of adhesions: focus on intestinal obstruction. The European journal of surgery. Supplement.: = Acta chirurgica. Supplement, 5–9 (1997).
Ellis, H. et al. Adhesion-related hospital readmissions after abdominal and pelvic surgery: a retrospective cohort study. Lancet (London, England) 353, 1476–1480, https://doi.org/10.1016/s0140-6736(98)09337-4 (1999).
Songer, M. N., Rauschning, W., Carson, E. W. & Pandit, S. M. Analysis of peridural scar formation and its prevention after lumbar laminotomy and discectomy in dogs. Spine 20, 571–580; discussion 579–580 (1995).
Fortin, C. N., Saed, G. M. & Diamond, M. P. Predisposing factors to post-operative adhesion development. Human reproduction update 21, 536–551, https://doi.org/10.1093/humupd/dmv021 (2015).
Kelekci, S. et al. The efficacy of a hyaluronate/carboxymethylcellulose membrane in prevention of postoperative adhesion in a rat uterine horn model. The Tohoku journal of experimental medicine 204, 189–194 (2004).
Hong, J. H. et al. The effects of barrier materials on reduction of pericardial adhesion formation in rabbits: a comparative study of a hyaluronan-based solution and a temperature sensitive poloxamer solution/gel material. The Journal of surgical research 166, 206–213, https://doi.org/10.1016/j.jss.2010.09.034 (2011).
Al-Chalabi, H. A. & Otubo, J. A. Value of a single intraperitoneal dose of heparin in prevention of adhesion formation: an experimental evaluation in rats. International journal of fertility 32, 332–335 (1987).
Golan, A., Maymon, R., Winograd, I. & Bukovsky, I. Prevention of post-surgical adhesion formation using aspirin in a rodent model: a preliminary report. Human reproduction (Oxford, England) 10, 1797–1800 (1995).
Hellebrekers, B. W., Trimbos-Kemper, T. C., Trimbos, J. B., Emeis, J. J. & Kooistra, T. Use of fibrinolytic agents in the prevention of postoperative adhesion formation. Fertility and sterility 74, 203–212 (2000).
Kim, T. H., Park, J. S., An, S. S. & Kang, H. Inhibition of thrombin-activated fibrinolysis inhibitor decreases postoperative adhesion. The Journal of surgical research 193, 560–566, https://doi.org/10.1016/j.jss.2014.07.056 (2015).
Choi, G. J. et al. Effects of a Lidocaine-Loaded Poloxamer/Alginate/CaCl2 Mixture on Postoperative Pain and Adhesion in a Rat Model of Incisional Pain. Anesthesia and analgesia, https://doi.org/10.1213/ane.0000000000001934 (2017).
Becker, J. M. et al. Prevention of postoperative abdominal adhesions by a sodium hyaluronate-based bioresorbable membrane: a prospective, randomized, double-blind multicenter study. Journal of the American College of Surgeons 183, 297–306 (1996).
van der Wal, J. B. & Jeekel, J. The use of statins in postoperative adhesion prevention. Annals of surgery 245, 185–186, https://doi.org/10.1097/01.sla.0000253071.06793.e6 (2007).
Falk, K., Bjorquist, P., Stromqvist, M. & Holmdahl, L. Reduction of experimental adhesion formation by inhibition of plasminogen activator inhibitor type 1. The British journal of surgery 88, 286–289, https://doi.org/10.1046/j.1365-2168.2001.01647.x (2001).
Liakakos, T., Thomakos, N., Fine, P. M., Dervenis, C. & Young, R. L. Peritoneal adhesions: etiology, pathophysiology, and clinical significance. Recent advances in prevention and management. Digestive surgery 18 260-273 50149 (2001).
Aarons, C. B. et al. Statins (HMG-CoA reductase inhibitors) decrease postoperative adhesions by increasing peritoneal fibrinolytic activity. Annals of surgery 245, 176–184, https://doi.org/10.1097/01.sla.0000236627.07927.7c (2007).
Scott-Coombes, D., Whawell, S., Vipond, M. N. & Thompson, J. Human intraperitoneal fibrinolytic response to elective surgery. The British journal of surgery 82, 414–417 (1995).
Schonbeck, U. & Libby, P. Inflammation, immunity, and HMG-CoA reductase inhibitors: statins as antiinflammatory agents? Circulation 109, Ii18–26, https://doi.org/10.1161/01.cir.0000129505.34151.23 (2004).
Yildiz, M. K. et al. Effect of orally administered simvastatin on prevention of postoperative adhesion in rats. International journal of clinical and experimental medicine 7, 405–410 (2014).
Davis, M. E. et al. Simvastatin reduces fibrosis and protects against muscle weakness after massive rotator cuff tear. Journal of shoulder and elbow surgery 24, 280–287, https://doi.org/10.1016/j.jse.2014.06.048 (2015).
Hoscan, Y. et al. Oral fluvastatin reduces the severity of peritoneal adhesions in rats. Acta chirurgica Belgica 110, 66–70 (2010).
Srinivasa, S. et al. Use of statins in adhesive small bowel obstruction. The Journal of surgical research 162, 17–21, https://doi.org/10.1016/j.jss.2010.02.028 (2010).
Javaherzadeh, M. et al. Effects of intraperitoneal administration of simvastatin in prevention of postoperative intra-abdominal adhesion formation in animal model of rat. Bulletin of Emergency and Trauma 4, 156–160 (2016).
Sun, Y. et al. Reduction of epidural scar adhesion by topical application of simvastatin after laminectomy in rats. European Review for Medical and Pharmacological Sciences 19, 3–8 (2015).
Kucuk, H. F. et al. The role of simvastatin on postoperative peritoneal adhesion formation in an animal model. European Surgical Research 39, 98-102.
Yilmaz, B. et al. Metformin and atorvastatin reduce adhesion formation in a rat uterine horn model. Reproductive Biomedicine Online 18, 436–442.
Lalountas, M. et al. Postoperative adhesion prevention using a statin-containing cellulose film in an experimental model. British Journal of Surgery 99, 423–429 (2012).
Lalountas, M. A. et al. Preventing intraperitoneal adhesions with atorvastatin and sodium hyaluronate/carboxymethylcellulose: a comparative study in rats. American Journal of Surgery 200, 118–123 (2010).
Wu, H. et al. The Topical Application of Rosuvastatin in Preventing Knee Intra-Articular Adhesion in Rats. Medical science monitor: international medical journal of experimental and clinical research 22, 1403–1409 (2016).
Gurer, B. et al. Evaluation of topical application and systemic administration of rosuvastatin in preventing epidural fibrosis in rats. The spine journal: official journal of the North American Spine Society 15, 522–529, https://doi.org/10.1016/j.spinee.2014.10.018 (2015).
Bickell, N. A., Federman, A. D. & Aufses, A. H. Jr. Influence of time on risk of bowel resection in complete small bowel obstruction. Journal of the American College of Surgeons 201, 847–854, https://doi.org/10.1016/j.jamcollsurg.2005.07.005 (2005).
Ray, N. F., Larsen, J. W. Jr., Stillman, R. J. & Jacobs, R. J. Economic impact of hospitalizations for lower abdominal adhesiolysis in the United States in 1988. Surgery, gynecology & obstetrics 176, 271–276 (1993).
Parker, M. C. et al. The SCAR-3 study: 5-year adhesion-related readmission risk following lower abdominal surgical procedures. Colorectal disease: the official journal of the Association of Coloproctology of Great Britain and Ireland 7, 551–558, https://doi.org/10.1111/j.1463-1318.2005.00857.x (2005).
Fevang, B. T. et al. Long-term prognosis after operation for adhesive small bowel obstruction. Annals of surgery 240, 193–201 (2004).
Haslinger, B., Kleemann, R., Toet, K. H. & Kooistra, T. Simvastatin suppresses tissue factor expression and increases fibrinolytic activity in tumor necrosis factor-alpha-activated human peritoneal mesothelial cells. Kidney international 63, 2065–2074, https://doi.org/10.1046/j.1523-1755.2003.t01-2-00004.x (2003).
Haslinger, B., Goedde, M. F., Toet, K. H. & Kooistra, T. Simvastatin increases fibrinolytic activity in human peritoneal mesothelial cells independent of cholesterol lowering. Kidney international 62, 1611–1619, https://doi.org/10.1046/j.1523-1755.2002.00601.x (2002).
Wiesbauer, F. et al. HMG CoA reductase inhibitors affect the fibrinolytic system of human vascular cells in vitro: a comparative study using different statins. British journal of pharmacology 135, 284–292, https://doi.org/10.1038/sj.bjp.0704454 (2002).
Wei, J., Ma, C. & Wang, X. Simvastatin inhibits tissue factor and plasminogen activator inhibitor-1 expression of glomerular mesangial cells in hypercholesterolemic rabbits. Biomedical research (Tokyo, Japan) 27, 149–155 (2006).
Alexander, Z. E. et al. The effect of oral simvastatin on fibrinolytic activity after colorectal surgery-a pilot study. The Journal of surgical research 205, 28–32, https://doi.org/10.1016/j.jss.2016.05.037 (2016).
Diamond, M. P. & Decherney, A. H. Pathogenesis of adhesion formation/reformation: application to reproductive pelvic surgery. Microsurgery 8, 103–107 (1987).
LaRocca, H. & Macnab, I. The laminectomy membrane. Studies in its evolution, characteristics, effects and prophylaxis in dogs. The Journal of bone and joint surgery. British volume 56b, 545–550 (1974).
Moris, D. et al. Postoperative Abdominal Adhesions: Clinical Significance and Advances in Prevention and Management. Journal of gastrointestinal surgery: official journal of the Society for Surgery of the Alimentary Tract 21, 1713–1722, https://doi.org/10.1007/s11605-017-3488-9 (2017).
Higgins J. P. T. & Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration Available from, www.handbook.cochrane.org (2011).
Liberati, A. et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Journal of clinical epidemiology 62, e1–34, https://doi.org/10.1016/j.jclinepi.2009.06.006 (2009).
Altman, D. G. & Bland, J. M. Statistics notes. Units of analysis. BMJ (Clinical research ed.) 314, 1874 (1997).
Hasin, T. et al. Attenuation in peripheral endothelial function after continuous flow left ventricular assist device therapy is associated with cardiovascular adverse events. Circulation Journal 79, 770–777 (2015).
IntHout, J., Ioannidis, J. P. & Borm, G. F. The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC medical research methodology 14, 25, https://doi.org/10.1186/1471-2288-14-25 (2014).
Hozo, S. P., Djulbegovic, B. & Hozo, I. Estimating the mean and variance from the median, range, and the size of a sample. BMC medical research methodology 5, 13, https://doi.org/10.1186/1471-2288-5-13 (2005).
Acknowledgements
This research was supported by the Basic Science Research Program through the National Research Foundation (NRF) of Korea funded by: the Ministry of Education, Science and Technology (NRF-2018R1A2A2A05021467); the Ministry of Science, ICT & Future Planning (NRF-2015R1A1A1A05027868). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
G.J.C. designed the study, conducted the study (searched literature and assessed methodological quality), analysed and interpreted the data, and wrote the manuscript; H.K.P. designed the study, conducted study (selected study and extracted data) and wrote the manuscript; D.S.K. designed the study, conducted study (selected study and extracted data) and wrote the manuscript; D.L. designed the study, conducted the study (searched literature, assessed methodological quality, and helped to extract data) and provided critical revision of the manuscript; H.K. designed the study, conducted the study (helped to select study and assess methodological quality), analysed and interpreted the data, and wrote the manuscript; all authors approved the final manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Choi, G.J., Park, H.K., Kim, D.S. et al. Effect of statins on experimental postoperative adhesion: a systematic review and meta-analysis. Sci Rep 8, 14754 (2018). https://doi.org/10.1038/s41598-018-33145-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-33145-z
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.