Abstract
Rotavirus (RV) is an important cause of diarrheal disease particularly in children aged under 5 years. Monovalent RV vaccine (RVV) was selectively introduced in 2012 in the Philippines and in July 2014 was introduced in the public health program of a province. Two RVV doses are recommended at 6 and 10 weeks of age. We conducted a test negative case-control evaluation to assess the effectiveness of RVV when given in a routine public health program in the Philippines. From September 2014 to August 2017, 967 children aged <5 years were hospitalized with diarrhea and of these, we enrolled 600 who were eligible to have received RVV and provided stool specimens for testing. Among children ≥8 months of age who were age-eligible to have received RVV, at least one dose of RVV had an adjusted vaccine effectiveness (VE) against RV hospitalization of 60% (95% confidence interval, CI: 24%, 79%), and against severe rotavirus diarrhea, VE was 64% (95% CI: 11%, 85%). These findings support the introduction of RVV into routine public health use in the Philippines. However, other factors such as costs, cost-effectiveness and operational issues must be considered prior to adoption of the vaccine into the countries’ public immunization program.
Similar content being viewed by others
Introduction
Diarrheal disease is a significant cause of mortality and morbidity in young children in the developing world. Diarrheal diseases also adversely affect long term growth and development1 providing further impetus for the use of appropriate preventive measures, including vaccination against diarrheal diseases.
Rotavirus (RV) is the most common cause of diarrhea globally and several vaccines are now internationally licensed and prequalified by the World Health Organization (WHO)2,3. Protection afforded by rotavirus vaccine (RVV) against severe RV diarrhea has been shown to vary depending on the country’s level of development4,5,6. In Asia, few countries have introduced RVV. Earlier results from high income countries of Asia in Hong Kong7 and Japan8, where RVV are self-financed, revealed RVV effectiveness of 89% and 70%, respectively against diarrheal hospitalization. However, a cluster-randomized study conducted in Bangladesh, a low income country, revealed that the monovalent RVV effectiveness was 41.4%9.
RVV was first introduced in the Philippines’ national immunization program in 2012, targeting children who belonged to the poorest quintile. However, there were problems in identifying the children, there were questions on the economic sustainability of the program and due to the varying levels of protection provided by the vaccine, policymakers in the Philippines requested that an effectiveness evaluation be conducted to assess the RV vaccine’s relevance for inclusion in the country’s Expanded Programme on Immunization (EPI). The vaccination strategy was changed limiting RVV use in the area where an effectiveness evaluation was conducted.
Results
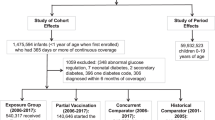
Of 967 children hospitalized with diarrhea that were screened for possible inclusion in the VE evaluation, 600 were enrolled from 1 September 2014 to 31 August 2017 and included in the analysis (Fig. 1). Of the 600 enrolled children, 203 (34%) were RV positive. The median age of enrolled children was 11 months. Most (88%) of RV positive cases were seen in children <24 months old (Fig. 2). Although statistically significant differences (median height, weight, mid-arm circumference and possession of mattress) were seen among RV positive and RV negative children, these differences were not considerable (Table 1).
RV positive children were more likely to have severe disease, i.e., more diarrhea (p < 0.001), vomiting (p = 0.01) and fever (p = 0.01) than RV negative children. Likewise, the median Vesikari score was higher among RV positive (p < 0.001) but the difference was not substantial in the two groups (Table 2). 486 (81%) of the 600 enrolled children received any vaccine. The proportion of children with no RV vaccination was significantly higher among RV positive (29%) compared to RV negative (16%) children (p = 0.004). Although the EPI schedule allowed children to receive RVV up to 2 years of age, there was no substantial difference in the age by which RV positive and RV negative children received the RVV doses (Fig. 3).
Among children ≥8 months of age who were age-eligible to receive rotavirus vaccine, the adjusted vaccine effectiveness (VE) of at least one dose of RVV against rotavirus diarrhea hospitalization was 60% (95% Confidence Interval, CI: 24%, 79%) and against severe rotavirus diarrhea hospitalization, i.e. those with Vesikari score ≥11, VE was 64% (95% CI: 11%, 85%) (Table 3). The adjusted VE of at least one dose of RVV was higher among children aged 8–11 months (85%, 95% CI: 53%, 95%), compared to children aged 12–23 months (66%, 95% CI:2%, 88%).
Discussion
Our findings confirm that RV is an important cause of diarrhea in the Philippines, responsible for 34% of hospitalized diarrheal cases, predominantly affecting young children. Further, we found that the monovalent RVV is effective against RV diarrhea in the Philippines, a lower middle income country in Asia. This supports our earlier findings of the substantial decline of RV diarrheal diseases in Agusan del Sur, where RVV was introduced10. Although lower VE was identified in older children in our study and may suggest waning effectiveness, it is also possible that unvaccinated children acquire infection earlier and are no longer susceptible to clinically significant infection because of natural acquired immunity11.
However, there are limitations that may have affected our results. First, RVV was not consistently available. After selective RVV introduction in September 2012 to infants from the poorest quintile, RVV was not available for nine months from October 2013 to June 2014 and then again for 11 months from June 2016 to April 2017. These prolonged periods may have precluded the identification of additional benefits such as indirect protection, which has been seen in other countries12,13,14. Furthermore, other findings such as changes in the rotavirus cyclical activity and age of RV infection were not identified. Coincidentally, during the period when vaccine stockouts in 2016 to 2017 occurred, a rise in the proportion of RV positive cases subsequently followed. This coincidental finding adds support to our results. Second, the health care system in the Philippines allows patients to access care anywhere, including the private healthcare system. Hence, it is likely that we were not able to capture all cases of diarrhea in Agusan del Sur. However, patients who go to the private health sector for management of diarrhea would also most likely obtain vaccine from the private sector. Third, unequal ascertainment of vaccination status may impact our results. Because immunization records in the Philippines are maintained in immunization registries that are kept in the public health centers, we had to visit all health centers to confirm all immunization information (obtained by review of cards or by recall). We had to exclude 20 children whose immunizations were unconfirmed to avoid misclassification. Stool test results were unknown to the study staff who collected vaccination information and it is unlikely that RV stool positivity influenced ascertainment of vaccination. Fourth, testing was not available locally so specimens had to be brought to RITM for testing. Fourteen specimens were lost in transit and could not be traced. Fifth, 298 children were unable to provide a stool specimen for testing, either because they were admitted on a weekend or they no longer had considerable stool output at the time of presentation. As these may have equally affected RV positive and RV negative children, it is unlikely that this resulted in bias. Sixth, since this is a hospital-based study, we did not detect cases and deaths due to RV that may have occurred in the community. Few deaths were identified in the study; all occurred among RV negative cases. A previous records review that we conducted was unable to quantify diarrheal deaths due to limitations in civil registration in the area where the study was conducted10. Lastly, observational studies are subject to limitations primarily due to the non-random allocation of vaccines resulting in possible differences in the health-care seeking behavior of the cases from the controls15. However, the controls used in the study have similar health-seeking behavior as the cases. The test negative design applied in our evaluation has been shown to be an efficient design useful particularly in countries with limited resources16 with comparable results to traditional case-control studies16 and has been validated against Phase 3 clinical trial results of RVV17.
The results of our study support the inclusion of RVV in the Philippines’ EPI. Aside from being provided in two regions in the Philippines, RVV is also available in the private sector. The EPI estimates that children who are brought to the private sector for immunization constitute less than 10% of the population. A decision on nationwide vaccine introduction should consider evidence of disease burden, cost and cost-effectiveness, and operational factors.
Methods
Study site
The vaccine effectiveness evaluation was conducted in D.O. Plaza Hospital (DOPH), one of the rotavirus sentinel surveillance hospitals in the Philippines. DOPH is a secondary hospital with a 100-bed capacity, located in Prosperidad, Agusan del Sur. In 2011, Agusan del Sur’s population was 808,500 with 15,946 births. The infant death rate was 8.78 infant deaths per 1000 live births and under 5 mortality rate was 1.10 per 100,000.
In the EPI schedule, children at least 6 weeks of age were eligible to receive the first dose of RVV. The second dose was given at least 4 weeks after the first RVV dose or at the same time as the Pentavalent vaccine, pneumococcal conjugate vaccine (PCV) and oral polio vaccine (OPV), as long as the child is not over 2 years old. RVV was provided to infants in the poorest quintile in Agusan del Sur starting in September 2012. In January 2013, RVV availability was expanded to all age-eligible children in two municipalities in Agusan del Sur, San Francisco and Prosperidad, regardless of socioeconomic status. In July 2014 vaccination was further expanded to all age-eligible children in the whole province. Vaccine stock-outs occurred in October 2013 to June 2014 and from June 2016 to April 2017.
Vaccine effectiveness case-control evaluation
We conducted a test-negative case-control evaluation within the rotavirus surveillance platform of DOPH. Children aged <5 years who underwent treatment for acute diarrhea in DOPH were included in the surveillance. Acute diarrhea was defined as the passage of three or more loose or watery stools within a 24-hour period for ≤14 days. Case-patients were children who were enrolled in the active surveillance platform, tested positive for RV by ELISA, and were age-eligible to have received RVV. Controls were children who were enrolled in the active surveillance platform, tested negative for RV by ELISA, and were age-eligible to have received RVV. Stool specimens were collected and shipped frozen to the Department of Virology of the Research Institute for Tropical Medicine (RITM), where specimens were tested. Information on receipt of RVV from the immunization cards and from parents’ recall were confirmed in the public health centers’ immunization registries. If the child was not in the immunization registry and may not have received vaccine, this information was confirmed by a visit to the child’s domicile, if known, by the health worker. Children whose identity could not be confirmed by the community health workers were excluded.
Sample size calculation
We assumed that 30% of diarrhea cases were due to RV, to detect a 60% vaccine effectiveness (VE), 90% vaccine coverage, at a 1 case to 2 controls ratio, power of 80% and 5% significance, at least 327 children were required, including 109 case-patients and 218 test-negative controls.
Data management and statistical analysis
Data were collected from the patient’s medical charts and caregiver and provider interviews and were recorded in paper forms. Aside from surveillance information (age, RV vaccination history, address), socioeconomic status, receipt of other EPI vaccines and disease severity indicators were collected. To assess the severity of the diarrheal illness, Vesikari scoring was performed by one researcher (JET). These were then transcribed into the web-based Rotavirus Surveillance Reporting System (RvSRS ver 1.0), developed by the WHO Regional Office for the Western Pacific.
Analyses were performed using SAS version 9.4. Age, receipt of RVV doses and other vaccines as well as clinical and socio-economic characteristics were tabulated and compared between test-positive cases and test-negative controls using chi-square or Fischer’s exact test, for sparse data. Like other analyses of RV effectiveness, calculation of VE was limited to children ≥8 months of age to exclude very young children not age-eligible for the vaccine or those children whose RV vaccination may have been delayed. Unconditional logistic regression controlling for month and year of birth, month and year of admission, and district where child lived was used to calculate the odd ratio for rotavirus vaccination for rotavirus-positive cases vs. rotavirus-test negative controls. VE was calculated using the formula:
where the odds ratio is the adjusted odds ratio for the rotavirus immunization rate among case-patients compared with controls. All p values and 95% confidence intervals (CI) were interpreted in a two-tailed manner and statistical significance was set at p < 0.05.
Ethics and Informed Consent
The evaluation was reviewed and approved by the University of the Philippines Manila Research Ethics Board (UPMREB 2014-167-01). Additional ethical approval was obtained from the WHO Regional Office for the Western Pacific Ethical Review Committee (2014.9.PHL.1.EPI). The study was conducted in accordance with the Philippines’ National Ethical Guidelines for Health and Health Related Research. Informed consents were obtained from all guardians of study participants.
Data Availability Statement
Datasets analysed in this study are available from the corresponding author on reasonable request.
References
Troeger, C. et al. Global disability-adjusted life-year estimates of long-term health burden and undernutrition attributable to diarrhoeal diseases in children younger than 5 years. Lancet Glob Health 6, e255–e269, https://doi.org/10.1016/S2214-109X(18)30045-7 (2018).
Deen, J. et al. Improving rotavirus vaccine coverage: Can newer-generation and locally produced vaccines help? Human vaccines & immunotherapeutics, 00–00, https://doi.org/10.1080/21645515.2017.1403705 (2017).
PATH. India-made rotavirus vaccine achieves World Health Organization prequalification, http://www.path.org/news/press-room/860/ Accessed 13 March 2018 (2018).
Fischer Walker, C. L. & Black, R. E. Rotavirus vaccine and diarrhea mortality: quantifying regional variation in effect size. BMC Public Health 11(Suppl 3), S16, https://doi.org/10.1186/1471-2458-11-S3-S16 (2011).
Lamberti, L. M., Ashraf, S., Walker, C. L. & Black, R. E. A Systematic Review of the Effect of Rotavirus Vaccination on Diarrhea Outcomes Among Children Younger Than 5 Years. Pediatr Infect Dis J 35, 992–998, https://doi.org/10.1097/INF.0000000000001232 (2016).
Burnett, E., Jonesteller, C. L., Tate, J. E., Yen, C. & Parashar, U. D. Global Impact of Rotavirus Vaccination on Childhood Hospitalizations and Mortality From Diarrhea. The Journal of infectious diseases 215, 1666–1672, https://doi.org/10.1093/infdis/jix186 (2017).
Yeung, K. H. T. et al. Rotavirus vaccine effectiveness in Hong Kong children. Vaccine 34, 4935–4942, https://doi.org/10.1016/j.vaccine.2016.08.047 (2016).
Fujii, Y. et al. Effectiveness of rotavirus vaccines against hospitalisations in Japan. BMC Pediatr 17, 156, https://doi.org/10.1186/s12887-017-0916-7 (2017).
Zaman, K. et al. Effectiveness of a live oral human rotavirus vaccine after programmatic introduction in Bangladesh: A cluster-randomized trial. PLoS Med 14, e1002282, https://doi.org/10.1371/journal.pmed.1002282 (2017).
Lopez, A. L. et al. Impact of rotavirus vaccine on diarrheal hospitalization and outpatient consultations in the Philippines: First evidence from a middle-income Asian country. Vaccine, https://doi.org/10.1016/j.vaccine.2018.04.058.
Wu, Y., Marsh, J. A., McBryde, E. S. & Snelling, T. L. The influence of incomplete case ascertainment on measures of vaccine efficacy. Vaccine 36, 2946–2952, https://doi.org/10.1016/j.vaccine.2018.04.046 (2018).
Diop, A. et al. Impact of rotavirus vaccine on acute gastroenteritis in children under 5 years in Senegal: Experience of sentinel site of the Albert Royer Children’s Hospital in Dakar. Vaccine, https://doi.org/10.1016/j.vaccine.2017.10.061 (2017).
Thomas, S. L. et al. Impact of the national rotavirus vaccination programme on acute gastroenteritis in England and associated costs averted. Vaccine 35, 680–686, https://doi.org/10.1016/j.vaccine.2016.11.057 (2017).
Bennett, A., Bar-Zeev, N. & Cunliffe, N. A. Measuring indirect effects of rotavirus vaccine in low income countries. Vaccine 34, 4351–4353, https://doi.org/10.1016/j.vaccine.2016.07.001 (2016).
Smith, P. G., Rodrigues, L. C. & Fine, P. E. Assessment of the protective efficacy of vaccines against common diseases using case-control and cohort studies. International journal of epidemiology 13, 87–93 (1984).
Tate, J. E. et al. Use of Patients With Diarrhea Who Test Negative for Rotavirus as Controls to Estimate Rotavirus Vaccine Effectiveness Through Case-Control Studies. Clin Infect Dis 62(Suppl 2), S106–114, https://doi.org/10.1093/cid/civ1014 (2016).
Schwartz, L. M., Halloran, M. E., Rowhani-Rahbar, A., Neuzil, K. M. & Victor, J. C. Rotavirus vaccine effectiveness in low-income settings: An evaluation of the test-negative design. Vaccine 35, 184–190, https://doi.org/10.1016/j.vaccine.2016.10.077 (2017).
Acknowledgements
The authors would like to thank the following: staff of the Philippines’ Department of Health (DOH) Expanded Programme on Immunization, staff of DOH Office in CARAGA Region and staff of the D.O. Plaza Hospital for assisting the authors in coordinating the study and Ms. Josephine Logronio (WHO-WPRO) for assisting us in Data Management. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention (US CDC). This study was funded by the World Health Organization.
Author information
Authors and Affiliations
Contributions
A.L.L., J.E.T. and U.D.P. prepared the protocol. A.L.L., J.V.D., J.E. and M.J.D. supervised and implemented the study. J.B. conducted the laboratory testing. A.L.L., J.V.D. and J.E.T. cleaned the data for analysis. J.E.T. and U.D.P. analysed the data. B.N. and K.F. contributed to the supervision of the study. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lopez, A.L., Daag, J.V., Esparagoza, J. et al. Effectiveness of monovalent rotavirus vaccine in the Philippines. Sci Rep 8, 14291 (2018). https://doi.org/10.1038/s41598-018-32595-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-32595-9
Keywords
This article is cited by
-
Rotavirus infection in children in Southeast Asia 2008–2018: disease burden, genotype distribution, seasonality, and vaccination
Journal of Biomedical Science (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.