Abstract
The amphibian chytrid fungus Batrachochytrium salamandrivorans (Bsal) infects newts and salamanders (urodele amphibians), in which it can cause fatal disease. This pathogen has caused dramatic fire salamander population declines in Belgium, the Netherlands and Germany since its discovery in 2010. Thought to be native to Asia, it has been hypothesised that Bsal was introduced to Europe with the importation of infected amphibians for the commercial pet trade. Following the discovery of Bsal in captive amphibians in the United Kingdom in 2015, we used contact-tracing to identify epidemiologically-linked private amphibian collections in Western Europe. Of 16 linked collections identified, animals were tested from 11 and urodeles tested positive for Bsal in seven, including the identification of the pathogen in Spain for the first time. Mortality of Bsal-positive individuals was observed in five collections. Our results indicate that Bsal is likely widespread within the private amphibian trade, at least in Europe. These findings are important for informing policy regarding Bsal control strategies.
Similar content being viewed by others
Introduction
Emerging infectious diseases pose a substantial threat to global biodiversity, causing population declines, and even species extinctions, across a range of taxa1. The amphibian chytrid fungus Batrachochytrium salamandrivorans (Bsal) is a current example of this, being the putative cause of an over 99% decline in a monitored population of fire salamanders (Salamandra salamandra) in the Netherlands2. The pathogen and consequent fire salamander population declines have since expanded into Belgium and Germany3. Experimental infection trials and field observations indicate that, although Bsal can also infect anuran amphibians4,5, it is only known to cause disease in amphibians of the order Urodela (newts and salamanders)6. This is unlike its sister fungus, Batrachochytrium dendrobatidis (Bd), which can infect and cause disease in amphibians across all three amphibian orders (Anura, Urodela and Gymnophiona)7,8,9.
Infection experiments demonstrated that urodeles native to Europe were either killed by, or were resistant to, Bsal infection; however some Asian urodeles were shown to survive infection without mortality6. In three Asian species tested (Cynops cyanurus, Cynops orientalis and Paramesotriton deloustali), all individuals developed clinical disease, but some cleared infection without treatment or maintained infection for an extended period of time6. One Asian urodele species, Salamandrella keyserlingii, was shown to tolerate infection in the absence of disease6. Most of the experimentally-infected animals were captive-bred (animals for only five species tested were wild-caught)6, a factor which might influence infection outcome. These infection trials, however, provide the best available data on the response of different urodele species to exposure to Bsal.
These findings, in combination with a global surveillance effort of wild salamanders that identified Bsal only in the Netherlands, where epidemic disease was occurring, and in Asia (Thailand, Vietnam and Japan), led to the hypothesis that the fungus is endemic to Asia4. The subsequent identification of widespread Bsal infection, in the absence of disease, in wild urodeles in Vietnam and China10,11, supports the hypothesis that urodeles from this region are reservoir hosts of the pathogen. Until recently, wild-caught urodeles from Asia were routinely imported into Europe as part of the pet trade12, and this is considered to have been the likeliest route for the introduction of Bsal into Europe6. Such introduction of non-native pathogens into new geographic regions with naive host species/populations is a recognised driver of infectious disease emergence and has been termed “pathogen pollution”13.
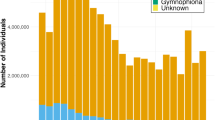
Despite difficulties in tracking and quantifying the global amphibian trade14, Europe is known to be a major importer of live amphibians15. In the United Kingdom (UK) alone, an estimated 131,000 live amphibians were imported in 2006, with approximately 98% believed to be for the pet trade16. Amphibian trade, for purposes such as research, food and the pet trade, has already been implicated in the global spread of Bd14,17, which has led to declines or extinctions of hundreds of amphibian species18,19. Thus, analysing the current state of Bsal infection in the amphibian trade is essential to understand the risk of further Bsal incursions into wild populations.
The private amphibian trade (i.e. the movement of animals between individual collectors who breed and sell amphibians on a non-commercial scale) takes place across Western Europe. Such trade is often directly between collectors or at large-scale fairs20, with little legislation governing the practice15. In the absence of sanitary regulations or practices, this trade presents a potential route of pathogen movement across international borders, particularly in animals which carry pathogens without any obvious signs of disease20. Reports of Bsal chytridiomycosis outbreaks in captive amphibian collections in the UK and Germany have shown that Bsal can cause mortality in captive animals21,22. The initial detection of Bsal in the UK was in 2015, in animals recently obtained by a zoological collection from a private amphibian breeder also in the UK21. This current study follows on from that initial detection, where using contact-tracing methods, we identified epidemiologically-linked amphibian collections across Western Europe and, where possible, we sampled urodeles in these collections to test for the presence of Bsal.
Results
Epidemiological tracing
Sixteen private amphibian collections were identified as being epidemiologically linked to the index (first) case of Bsal infection in the UK21. We identified Collection A as the source of the Bsal infected urodeles in the index zoological collection21. Further epidemiological links between private collections were established either through the sale, purchase or swapping of urodeles during the previous 24 months (Fig. 1). Of the 16 linked collections, 11 collectors granted access to sample amphibians for Bsal infection (Collections A-K), and five collectors denied access (Collections L-P). Summary information on Collections A-K, including the total numbers of urodeles and numbers of species held at the time of testing, is provided in Table 1. Access to each collection was allowed on the condition of anonymity. As details of the actual numbers of each species held in each location could identify some of the collections, these data have not been shown, but a list of the total number of each species examined is listed in Supplementary Tables S1 and S2.
Epidemiological links between all sixteen contact-traced private collections. Access was granted to Collections (A-K) with all urodeles swabbed for Bsal infection. Access was not granted to Collections (L-P). Arrows indicate the direction of transit of animals, including those subsequently identified as Bsal-positive. Numbers and percentages indicate the number of Bsal-positive/total number of urodeles tested.
Collectors reported mostly trading urodeles in person, meeting either privately or at large-scale fairs, where both commercial breeders and private collectors bring urodeles to trade with other collectors. Some collectors reported sending or receiving urodeles via postal and courier services. Trading often occurred in small numbers (less than ten urodeles), primarily to provide collections with a new species or to supplement currently held animals and to form breeding pairs. Trading at large-scale fairs was reported as common. Private hobbyist trade deals were often pre-agreed using social media, with collectors advertising which species they had available for sale or swap, and those species they wished to buy or swap in return.
Bsal prevalence in private collections
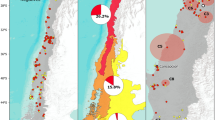
At least one urodele tested positive for Bsal using qPCR in seven of the 11 tested collections: four in the UK, two in the Netherlands and one in Spain. Infection prevalences ranged from 1.6% (1/62) to 91.3% (21/23) across the collections at the time of testing (Table 1; Fig. 1). In accordance with the owner’s wishes, samples from live urodeles in Collection K were grouped by species (five animals per swab), so the prevalence of infection in this collection could not be ascertained. All 84 Bsal-positive urodeles across all collections were adults, 74 of which were captive-bred and ten were wild-caught. None of the 58 anurans of 21 species sampled in Collection A tested positive for Bsal using qPCR (Supplementary Table S2).
A comparison of Bsal prevalence in Asian (0/79) versus non-Asian (64/738) urodeles in Collections A-J showed a statistically significant difference (χ2 = 5.6651, p = 0.01731) with non-Asian urodeles having a higher prevalence of Bsal infection (Supplementary Table S1). Fisher’s exact tests showed no association between the presence of Asian species in a collection and higher than usual levels of mortality (p = 0.5671), or between the presence of Asian species and the presence of Bsal in a collection (p = 0.5455) (Table 1).
Pathological examinations
Unusually high mortalities were reported from five of the tested collections (A, C, F, J and K; Table 1), all of which had mortalities associated with Bsal-positive urodeles.
The owner of Collection A donated 11 dead urodeles and two sick Lissotriton boscai (which were then euthanased) for pathological examination. No gross skin lesions were observed in any of the dead urodeles examined, however cachexia and ataxia, two non-specific signs associated with Bsal chytridiomycosis2, were observed in both L. boscai prior to euthanasia. Eleven of the 13 donated urodeles from Collection A tested positive for Bsal on qPCR, with infection intensities available for ten ranging from 1.2 to 2,836.92 genome equivalents (GE) swab−1 (Table 2). Of these, six (2 Salamandra corsica, 2 S. salamandra and both euthanased L. boscai) were suitable for post-mortem examination. All six necropsied animals were in a thin or emaciated body condition, with reduction or complete absence of coelomic fat bodies.
Samples were taken for histological examination from one L. boscai, one S. salamandra and two S. corsica. On histological examination of a forelimb and a hindlimb from the L. boscai, multiple areas of epidermal erosion associated with intracellular zoosporangia consistent with those of a chytrid fungus were identified (Fig. 2). Bsal chytridiomycosis was confirmed in this individual (Table 2), which had been captive-bred in Collection E and traded to Collection A in March 2013. No lesions consistent with Bsal chytridiomycosis were identified on histological examination of samples taken from the other three animals.
One S. salamandra was found dead in its enclosure in Collection C at the time of swabbing. This animal had a Bsal infection intensity of 8,402.64 GE swab−1. The two remaining live S. salamandra in this enclosure also tested positive for Bsal on qPCR; both had higher infection intensities than the dead individual (9,752.76 and 45,250.68 GE swab−1). The individual with the higher infection intensity was reported dead approximately one week later; the outcome of the other is unknown. The owner of Collection C also reported that four other known Bsal-positive animals, three Lissotriton helveticus and one Triturus cristatus, died approximately one week after swabbing. However, as these animals were not individually identifiable and were in an enclosure with conspecifics, we are unable to determine their infection intensities at the time of swabbing. Although these six dead urodeles were Bsal-positive, none were made available for pathological examination, so chytridiomycosis could not be confirmed as the cause of death.
In Collection F, two Triturus marmoratus were found dead in their enclosure at the time of swabbing. Four apparently-healthy individuals of the same species shared the enclosure. The two dead animals had substantially higher infection intensities (8,045.28 and 9,259.80 GE swab−1) (Table 2) than the four that remained alive (146.16, 348.60, 382.80 and 1,132.32 GE swab−1), but these four animals were reported to have died approximately two weeks after the swabbing took place. None of the six T. marmoratus were made available for pathological examination, so chytridiomycosis could not be confirmed as the cause of death.
Collection J experienced the complete loss of 160 animals of nine species from the genera Lissotriton, Neurergus, Notophthalmus and Triturus over the course of 2015. The collector submitted six captive-bred urodeles (three Neurergus strauchii and three Notophthalmus viridescens) that died during this period for pathological examination. All six tested positive for Bsal on qPCR, but the infection intensities are not available, and all had multiple skin erosions observed on histological examination. Bsal chytridiomycosis was confirmed in all six cases (Table 2).
Collection K reported the complete loss of 12 urodelan breeding groups in a period of three months, including fully-aquatic newts of species from the genera Euproctus, Neurergus, Ommatotriton and Triturus. The collector submitted two Triturus macedonicus that died during these mortality events for pathological examination. Both T. macedonicus were captive-bred and were in the aquatic breeding stage at the time of death. Bsal chytridiomycosis was confirmed in both cases using a combination of histopathological examination and qPCR (Table 2)23. Skin swabs taken from the two dead T. macedonicus had infection intensities of 40,900.00 and 115,400.00 GE swab−1.
Bsal genotyping
Sequencing of amplicons obtained following PCR2 of DNA extracted from skin-swabs from three Bsal-positive S. salamandra from Collection A and from Bsal isolates cultured from one diseased Neurergus strauchii from Collection J and one Salamandra corsica from Collection K all showed 100% identity to the type strain, AMFP13/1, in the Netherlands and Belgium2.
Discussion
We identified Bsal-positive urodeles in seven of 11 tested private amphibian collections across Western Europe that were epidemiologically linked to the index case in the UK21, including the first identification of Bsal in Spain. In addition to apparent subclinical infection of urodeles, both clinical disease and fatal chytridiomycosis were diagnosed in several collections. None of the anurans tested were positive for this pathogen despite being in a Bsal-positive collection with an absence of biosecurity, such as shared tools, water, plants and other matter being transferred between enclosures. Whilst the tested collections only form a small proportion of the number of private amphibian collections in Europe, a high percentage of those tested were found to be Bsal-positive. It is likely, therefore, that Bsal is widespread within the European private amphibian trade. This is in contrast to the situation in the United States of America, where surveys have not identified Bsal either in the private amphibian trade24, or in the wild25,26.
Fatal Bsal chytridiomycosis was confirmed using histological examination and qPCR in nine dead urodeles from three collections: one in the UK and two in the Netherlands. These deaths and diagnoses all occurred during multiple mortality events affecting a range of urodele species native to Europe, North America and the Middle East. There was a wide range of infection intensities observed in animals that died with confirmed Bsal chytridiomycosis (523.20–115,400.00 GE swab−1) (Table 2). Further research into the pathogenesis of Bsal will help to identify possible links between infection intensity and the likelihood of mortality, and whether any link between infection intensity and mortality is species- or life-history-specific.
The spectrum of species we found to be affected by fatal Bsal infection in private collections largely corroborates results of experimental infection trials6. Here, however, we also show mass mortality in aquatic newts, with complete eradication of the breeding groups, whereas wild urodele declines due to Bsal chytridiomycosis have so far only been detected in terrestrial Salamandra salamandra2,3. Although the situation in captivity might not be representative of that in the wild, it clearly shows that Bsal transmission and disease in newts during the aquatic life stage is possible. Also, this study expands the spectrum of susceptible host species (Supplementary Table S1), with the inclusion of the genera Ambystoma (A. mexicanum) and Ommatotriton (O. ophryticus) and further species in the genera Neurergus (N. strauchii), Triturus (T. dobrogicus, T. ivanbureschi, T. karelinii, T. marmoratus), Salamandra (S. atra) and Lissotriton (L. boscai). These additions to the list of species susceptible to Bsal infection confirm the potential threat of Bsal to western Palearctic and Nearctic urodele diversity.
It is thought that Bsal initially reached Europe via the import of Asian urodeles and that these species are key in the movement of the pathogen6. Our study shows that the movement of non-Asian urodeles can also present a biosecurity risk to captive amphibian collections. We failed to detect an association between the presence of Asian urodeles and the presence of Bsal or unusually high mortality in collections. The movement of non-Asian urodeles appears to have introduced the pathogen into at least three of the Bsal-positive collections with higher than usual levels of mortality (Collections A, C and J; Table 1). These results, coupled with the significantly higher Bsal infection prevalence in non-Asian vs Asian urodeles in Collections A-J, indicate that non-Asian urodeles should be considered potential vectors of Bsal in the private amphibian trade.
Following the emergence of Bsal in wild amphibians in Western Europe, there is a danger that this pathogen will cause a second amphibian chytridiomycosis panzootic, similar to the Bd panzootic but with a greater impact on urodeles. Once established in the wild, the disease is likely to be extremely difficult to eradicate or otherwise mitigate27 if its epidemiology is similar to that of Bd28. Bd is now established in wild amphibian populations on a global scale29,30 and, despite best efforts, strategies to mitigate the effect of Bd in the wild have only had small-scale, short-term success31,32,33. Preventing such an outcome with Bsal is a high priority, but the best methods by which to do this vary depending on location and are still being debated34,35,36. One area of agreement is that reducing the risk of spread to, and establishment in, wild populations is a primary objective28,30,36,37,38. The amphibian trade has been identified as the likeliest route of Bsal introduction to the wild in Europe6. We identify the widespread presence of Bsal in captive amphibian collections, providing further evidence that the amphibian trade may spread this pathogen both within countries and internationally. Thus, both the commercial and the private trade in amphibians need to be considered when developing measures to mitigate the spread of Bsal. In addition to posing a threat to the health and welfare of captive urodeles, the presence of Bsal in amphibian collections increases the risk of Bsal infection transmitting to nearby wild populations, for example via contaminated wastewater or released or escaped animals, in a similar manner to Bd16.
Further work is required to reduce the disease risks presented by the amphibian trade to wild amphibian health and conservation. This includes engagement of policy makers, conservationists and veterinarians with the commercial amphibian trade and hobbyists to develop and promote appropriate biosecurity protocols in a collaborative manner34,35,36. Such an engagement was conducted in the UK by conservation charities, government and the amphibian trade following the discovery of Bsal in captive amphibians21. Although it was well-received by the target sectors, the degree and duration of uptake was not quantified39. The European Food Safety Authority identified that screening captive collections, treating Bsal positive individuals40,41 and engaging with collectors to improve sanitary protocols are likely to be the most effective and feasible measures to protect captive urodeles from Bsal42.
Increasing the general levels of hygiene and biosecurity in captive collections and the amphibian trade has the additional benefits of increasing the health, welfare and longevity of captive animals while also minimising disease threats to native wild animals43. Such sanitary measures include the disinfection of equipment after each use44, the appropriate disinfection and disposal of waste and dead animals42, and the quarantine and pathogen screening45 of new arrivals before being placed into a collection. The development of best-practice sanitary protocols to be shared with the private and commercial trade is considered an important future step in Bsal mitigation42.
The management of wildlife diseases and mitigating their potential impacts on wild populations is a complex issue. The critical control point is the prevention of pathogen introduction28,30,36,37,38, although historically, international trade controls have not been implemented in response to diseases that solely affect wildlife46. This appears to be changing, with the United States of America, Canada and Switzerland all recently banning the importation of urodeles, citing the threat of Bsal to native amphibian biodiversity47. Also, the European Union (EU) recently announced regulation of the movement of captive urodeles in response to Bsal48. Due to concerns that blanket bans could lead to an increase in unregulated “black market” trade42,49,50, the EU regulations focus on developing a clean trade in Bsal-free animals. This decision affects both the import into the EU and the intra-EU movement of urodeles across national borders, with veterinarians required to certify that urodeles have been examined, and are negative, for clinical signs of Bsal infection, that they come from a population where no Bsal chytridiomycosis has been observed and that the urodeles have undergone mandatory pre-import pathogen screening and quarantine, with treatment of infected amphibians where required48.
In addition to these regulations, the development and dissemination of biosecurity guidance for the owners of captive amphibians is required to increase awareness of the risks of Bsal to native amphibian biodiversity and to prevent its spread into the wild. In parallel, surveillance for Bsal infection and disease in wild amphibians should be increased across Europe in order to identify and eradicate any incursions into the wild as quickly as possible, and before the infection can become established.
Methods
Ethics
All procedures performed in this study involving animals were in accordance with the laws of the UK and with the institutional guidelines of the Zoological Society of London (ZSL). Informed consent was obtained from the owner of each amphibian collection tested. This consent was given under the condition that each collection would remain anonymous. No charge was made for visiting any collection or for testing any animals included in this study for Bsal infection. Ethical approval for this study was provided by the ZSL Ethics Committee (ref. WAB17).
Private collection identification
The index case of Bsal infection in the UK occurred in recently-purchased animals under quarantine in a zoological collection, as previously reported21. The animals had been purchased from a private hobbyist in the UK, from here on termed Collection A. We used contact-tracing methods to identify other private collections that could be contaminated with Bsal. For each private collection that had Bsal positive animals, we identified the source of all the animals currently held at the collection using the collector’s records. We determined that collections were epidemiologically linked if there had been movement of any animals between collections in the previous two years, either through the sale, purchase or swapping of urodeles. Epidemiologically linked collections were then approached to test their urodeles, and the process repeated. In total, during the course of this study, 16 epidemiologically linked collections were identified and approached, 11 of which granted access.
Samples were obtained between 11th March 2015 and 26th February 2016 by skin-swabbing urodeles at 11 private amphibian collections across Western Europe; five in the United Kingdom, three in the Netherlands, two in Spain, and one in Germany. At all collections, all non-larval (i.e. neotenic, juvenile and adult) urodeles of all species were tested, as current evidence indicates that larval urodeles are not able to be infected with Bsal51. At Collection A, all anurans were also tested. At the time of this study, it was thought that anurans could not be infected with Bsal6. Anuran amphibians were tested in Collection A as this Bsal-positive collection held a large number of both urodeles and anurans, with opportunity for cross-taxon transmission. As no anurans in this collection were Bsal-positive, and as sampling anurans added time and cost burdens, including to collection owners and could thus impact compliance, only urodeles were tested in subsequent collections visited.
Access to the collections, samples and records were obtained with the full knowledge and permission of the owner of each collection, which was given on the grounds on anonymity. Results were provided to the owners, so they could act on this information and seek veterinary advice, if required. In addition, we requested that carcasses of any amphibians that died during the course of this study were made available for pathological examination.
During each visit, each collection owner was asked how they sold/bought/exchanged animals, their rationale for doing so and the numbers of animals involved. This was done in an informal, conversational way to maximise the likelihood of obtaining the required information.
Skin-swabbing
Skin swab samples were taken from all non-larval urodeles in each collection visited, whether they were live or dead, using a dry rayon-tipped swab (MW100, Medical Wire & Equipment, UK). We followed a well-established protocol of comprehensively swabbing the underside of the legs, feet (including between digits) and ventral surface (five swab strokes over each area) before replacing the swab into its plastic sleeve52. One swab was used per animal apart from in Collection K, where – at the owner’s request – five animals from within the same enclosure were sampled with each swab. Animals for which swabs were pooled always coinhabited the same enclosure. During swabbing, animals were visually examined for the presence of gross lesions and were observed for signs of Bsal chytridiomycosis, such as cachexia, lethargy or ataxia2.
Quantitative PCR
DNA was extracted in 60 µl PrepMan Ultra following the manufacturer’s guidelines (Applied Biosystems, Foster City, CA). Samples were analysed for the presence of Bd and Bsal DNA using a duplex quantitative polymerase chain reaction (qPCR), targeting the ITS1 rRNA gene of Bd and 5.8S rRNA gene of Bsal, as described by Blooi et al.45. Each sample was run in duplicate; where a sample produced contradictory results in the duplicates, the qPCR was repeated until the duplicates gave a consistent result. Positive controls, comprising known quantities of both Bd and Bsal DNA (100, 10, 1 and 0.1 GE – zoospore genomic equivalents) and a negative control were included in each qPCR run. Infection intensity results from qPCR plates where the R2 value of the standard curves generated by the positive controls was less than 0.9 were determined to be inaccurate and were re-run. Infection intensities, measured in zoospore genomic equivalents per swab (GE swab−1), were calculated by multiplying the mean quantity output of Bsal positive qPCRs by 120, to account for the dilution between swab and PCR, as described by Hudson et al.31.
Pathological investigations and diagnosis
Two sick urodeles submitted by collectors were euthanased with an overdose of the anaesthetic tricaine methanesulphonate (MS222) followed by destruction of the brain and spinal cord by pithing.
Urodele carcasses were examined for the presence of macroscopic skin lesions consistent with Bd or Bsal chytridiomycosis. Full necropsies were conducted following published guidelines53. Tissue samples, including forelimb, hindlimb, tail, 1 cm2 patch of dorsal skin and 1 cm2 patch of ventral skin, were taken for histological examination. These samples were fixed in neutral buffered 10% formalin, embedded in paraffin and sectioned, before being stained with haematoxylin and eosin using routine methods54.
For this study, animals which tested positive for Bsal on qPCR, whether or not gross or microscopic lesions were observed, are termed ‘Bsal-positive’. Following the case definition and diagnostic criteria for Bsal chytridiomycosis23, this disease was confirmed in dead animals when lesions consistent with Bsal infection were seen on histopathological examination and positive Bsal qPCR results were obtained.
Genotyping
A subset of DNA extracts that were positive for Bsal on qPCR were further analysed using standard PCR with the STerF and STerR primers to target the ITS1–5.8S-ITS2 region of the Bsal 5.8 S rRNA gene2. PCR amplicons of approximately 160 base pairs45 were sequenced in-house at Ghent University and compared to the type strain (GenBank accession no. KC762295)2. This was conducted to determine whether the strain of Bsal in the captive collections was the same as the strain implicated in the epizootic in the Netherlands2.
Statistical analysis
Bsal prevalence in each collection was calculated (number of animals that tested positive divided by the total population size tested). We then used the Clopper-Pearson test (also known as an exact binomial distribution confidence interval test) to determine the 95% confidence intervals for Bsal prevalence in each collection. Comparisons of Bsal prevalence in Asian versus non-Asian urodeles was conducted using a Pearson’s Chi-squared Test. For each of these tests, Collection K was excluded from the analyses, as swabs were pooled by five animals so results for individuals were not available. Fisher’s exact tests were used to examine if there was an association between the presence of Asian species of urodele in a collection and either (1) the presence of Bsal or (2) the presence of unusually high levels of mortality. All statistical analyses were conducted using R version 3.4.1.55.
Data Availability
All materials, data and associated protocols have been made available in the manuscript and supplementary information. We sampled animals under the condition that each collection/owner would be anonymous. We are, therefore, unable to provide details of the species and numbers sampled for individual collections as doing so could identify the collections sampled. This will not affect the ability to replicate this work: information about the number of each species sampled has been provided pooled across all collections.
References
Daszak, P., Cunningham, A. A. & Hyatt, A. D. Emerging infectious diseases of wildlife–threats to biodiversity and human health. Science 287, 443–449 (2000).
Martel, A. et al. Batrachochytrium salamandrivorans sp. nov. causes lethal chytridiomycosis in amphibians. Proc. Natl. Acad. Sci. 110, 15325–15329 (2013).
Spitzen-van der Sluijs, A. et al. Expanding distribution of lethal amphibian fungus Batrachochytrium salamandrivorans in Europe. Emerg. Infect. Dis. 22, 1286–1288 (2016).
Stegen, G. et al. Drivers of salamander extirpation mediated by Batrachochytrium salamandrivorans. Nature 544, 353–356 (2017).
Nguyen, T. T. et al. Trade in wild anurans vectors the urodelan pathogen Batrachochytrium salamandrivorans into Europe. Amphibia-Reptilia 4–6, https://doi.org/10.1038/srep44443.Martel (2017).
Martel, A. et al. Recent introduction of a chytrid fungus endangers Western Palearctic salamanders. Science 346, 630–631 (2014).
Berger, L. et al. Chytridiomycosis causes amphibian mortality associated with population declines in the rain forests of Australia and Central America. Proc. Natl. Acad. Sci. USA 95, 9031–9036 (1998).
Davidson, E. W. et al. Pathogenicity and transmission of chytridiomycosis in tiger salamanders (Ambystoma tigrinum). Copeia 2003, 601–607 (2003).
Gower, D. J. et al. Batrachochytrium dendrobatidis infection and lethal chytridiomycosis in caecilian amphibians (Gymnophiona). Ecohealth 10, 173–183 (2013).
Laking, A. E., Ngo, H. N., Pasmans, F., Martel, A. & Nguyen, T. T. Batrachochytrium salamandrivorans is the predominant chytrid fungus in Vietnamese salamanders. Sci. Rep. 7, 44443 (2017).
Yuan, Z. et al. Widespread occurrence of an emerging fungal pathogen in heavily traded Chinese urodelan species. Conserv. Lett. e12436 (2018).
UNEP-WCMC. Review of the risk posed by importing Asiatic species of Caudata amphibians (salamanders and newts) into the EU. (2016).
Cunningham, A. A., Daszak, P. & Rodriguez, J. P. Pathogen pollution: defining a parasitological threat to biodiversity conservation. J. Parasitol. 89, 78–83 (2003).
Schloegel, L. M., Daszak, P., Cunningham, A. A., Speare, R. & Hill, B. Two amphibian diseases, chytridiomycosis and ranaviral disease, are now globally notifiable to the World Organization for Animal Health (OIE): an assessment. Dis. Aquat. Organ. 92, 101–108 (2010).
Auliya, M. et al. The global amphibian trade flows through Europe: the need for enforcing and improving legislation. Biodivers. Conserv. 25, 2581–2595 (2016).
Peel, A. J., Hartley, M. & Cunningham, A. A. Qualitative risk analysis of introducing Batrachochytrium dendrobatidis to the UK through the importation of live amphibians. Dis. Aquat. Organ. 98, 95–112 (2012).
O’Hanlon, S. J. et al. Recent Asian origin of chytrid fungi causing global amphibian declines. Science 360, 621–627 (2018).
Stuart, S. N. et al. Status and trends of amphibian declines and extinctions worldwide. Science 306, 1783–1786 (2004).
Alroy, J. Current extinction rates of reptiles and amphibians. Proc. Natl. Acad. Sci. 112, 13003–13008 (2015).
Spitzen-van der Sluijs, A. et al. Clinically healthy amphibians in captive collections and at pet fairs: a reservoir of Batrachochytrium dendrobatidis. Amphibia-Reptilia 32, 419–423 (2011).
Cunningham, A. A. et al. Emerging disease in UK amphibians. Vet. Rec. 176, 468 (2015).
Sabino-Pinto, J. et al. First detection of the emerging fungal pathogen Batrachochytrium salamandrivorans in Germany. Amphibia-Reptilia 36, 411–416 (2015).
White, C. L. et al. Amphibian: a case definition and diagnostic criteria for Batrachochytrium salamandrivorans chytridiomycosis. Herpetol. Rev. 47, 207–209 (2016).
Klocke, B. et al. Batrachochytrium salamandrivorans not detected in U.S. survey of pet salamanders. Sci. Rep. 7, 13132 (2017).
Bales, E. K. et al. Pathogenic chytrid fungus Batrachochytrium dendrobatidis, but not B. salamandrivorans, detected on Eastern hellbenders. PLoS One 10, 1–9 (2015).
Parrott, J. C. et al. Survey of pathogenic chytrid fungi (Batrachochytrium dendrobatidis and B. salamandrivorans) in salamanders from three mountain ranges in Europe and the Americas. Ecohealth 14, 296–302 (2017).
Canessa, S. et al. Decision-making for mitigating wildlife diseases: from theory to practice for an emerging fungal pathogen of amphibians. J. Appl. Ecol. 1–10, https://doi.org/10.1111/1365-2664.13089 (2018).
Garner, T. W. J. et al. Mitigating amphibian chytridiomycoses in nature. Philos. Trans. R. Soc. B Biol. Sci. 371 (2016).
Olson, D. H. et al. Mapping the global emergence of Batrachochytrium dendrobatidis, the amphibian chytrid fungus. PLoS One 8, e56802 (2013).
Bower, D. S., Lips, K. R., Schwarzkopf, L., Georges, A. & Clulow, S. Amphibians on the brink. Science 357, 454–456 (2017).
Hudson, M. A. et al. In-situ itraconazole treatment improves survival rate during an amphibian chytridiomycosis epidemic. Biol. Conserv. 195, 37–45 (2016).
Bosch, J. et al. Successful elimination of a lethal wildlife infectious disease in nature. Biol. Lett. 11, 20150874 (2015).
Clulow, S. et al. Elevated salinity blocks pathogen transmission and improves host survival from the global amphibian chytrid pandemic: implications for translocations. J. Appl. Ecol. 55, 830–840 (2018).
Yap, T. A., Koo, M. S., Ambrose, R. F., Wake, D. B. & Vredenburg, V. T. Averting a North American biodiversity crisis. Science 349, 481–482 (2015).
Gray, M. J. et al. Batrachochytrium salamandrivorans: the North American response and a call for action. PLoS Pathog. 11, 1–9 (2015).
Grant, E. H. C. et al. Using decision analysis to support proactive management of emerging infectious wildlife diseases. Front. Ecol. Environ. https://doi.org/10.1002/fee.1481 (2017).
Langwig, K. E. et al. Context-dependent conservation responses to emerging wildlife diseases. Front. Ecol. Environ. 13, 195–202 (2015).
Schmidt, B. R., Bozzuto, C., Lötters, S. & Steinfartz, S. Dynamics of host populations affected by the emerging fungal pathogen Batrachochytrium salamandrivorans. R. Soc. Open Sci. 4, 160801 (2017).
Disease alert - Reducing the risks in captive amphibians and protecting our wild native amphibians from invasive disease. (2015). Available at: http://www.gardenwildlifehealth.org/files/2013/06/Amphibian-disease-alert_June-2015.pdf.
Blooi, M. et al. Successful treatment of Batrachochytrium salamandrivorans infections in salamanders requires synergy between voriconazole, polymyxin E and temperature. Sci. Rep. 5, 11788 (2015).
Blooi, M. et al. Treatment of urodelans based on temperature dependent infection dynamics of Batrachochytrium salamandrivorans. Sci. Rep. 5, 8037 (2015).
EFSA Panel on Animal Health and Welfare (AHAW) et al. Risk of survival, establishment and spread of Batrachochytrium salamandrivorans (Bsal) in the EU. EFSA J. 16 (2018).
Pasmans, F. et al. Future of keeping pet reptiles and amphibians: towards integrating animal welfare, human health and environmental sustainability. Vet. Rec. 1–8, https://doi.org/10.1136/vr.104296 (2017).
Van Rooij, P., Pasmans, F., Coen, Y. & Martel, A. Efficacy of chemical disinfectants for the containment of the salamander chytrid fungus Batrachochytrium salamandrivorans. PLoS One doi:0186269 (2017).
Blooi, M. et al. Duplex real-time PCR for rapid simultaneous detection of Batrachochytrium dendrobatidis and Batrachochytrium salamandrivorans in amphibian samples. J. Clin. Microbiol. 51, 4173–4177 (2013).
Cunningham, A. A., Daszak, P. & Wood, J. L. N. One Health, emerging infectious diseases and wildlife: two decades of progress? Philos. Trans. R. Soc. B Biol. Sci. 372, 1–8 (2017).
Yap, T. A., Nguyen, N. T., Serr, M., Shepack, A. & Vredenburg, V. T. Batrachochytrium salamandrivorans and the risk of a second amphibian pandemic. Ecohealth 1–14, https://doi.org/10.1007/s10393-017-1278-1 (2017).
Official Journal of the European Union. Commission Implementing Decision (EU) 2018/320 on certain animal health protection measures for intra-Union trade in salamanders and the introduction into the Union of such animals in relation to the fungus Batrachochytrium salamandrivorans. 15 (2018).
Garner, T. W. J., Stephen, I., Wombwell, E. & Fisher, M. C. The amphibian trade: bans or best practice? Ecohealth 6, 148–151 (2009).
EFSA Panel on Animal Health and Welfare (AHAW) et al. Assessment of listing and categorisation of animal diseases within the framework of the Animal Health Law (Regulation (EU) No 2016/429): Batrachochytrium salamandrivorans. EFSA J. 15 1–34 (2017).
Van Rooij, P., Martel, A., Haesebrouck, F. & Pasmans, F. Amphibian chytridiomycosis: a review with focus on fungus-host interactions. Vet. Res. 46, 137 (2015).
Hyatt, A. D. et al. Diagnostic assays and sampling protocols for the detection of Batrachochytrium dendrobatidis. Diseases of Aquatic Organisms 73, 175–192 (2007).
Nichols, D. K. N. In Amphibian Medicine and Captive Husbandry (eds Wright, K. & Whitaker, B.) 53, 555 (Krieger Publishing Company, 2001).
Bancroft, J. D. & Layton, C. The hematoxylins and eosin. In Bancroft’s Theory and Practice of Histological Techniques (eds Bancroft, J. D. & Gamble, M.) 173–186, https://doi.org/10.1016/B978-0-7020-4226-3.00010-X (Churchill Livingstone, 2013).
R Core Team. R: a language and environment for statistical computing. (2017).
Acknowledgements
We thank all the private amphibian hobbyists who provided access to, and information about, their collections. Matthew Perkins assisted with the qPCR laboratory analysis. Julia Rodriguez-Ramos Fernandez assisted with urodele necropsies, histology preparation and examination. This work was funded by the Department for Environment, Food and Rural Affairs (UK), the Animal and Plant Health Agency (UK), the Royal Veterinary College, the Zoological Society of London (ZSL) and the Research Foundation – Flanders (GOF3816N). A component of this study was carried out in fulfilment of the Wild Animal Biology MSc degree (L.D.F.) at the Royal Veterinary College and the Zoological Society of London.
Author information
Authors and Affiliations
Contributions
The study was conceived by A.A.C. Sample collection and laboratory analyses were conducted by L.D.F., A.A.C., F.P. and A.M. Analysis and interpretation of the data were conducted by all authors. L.D.F. was the main author of the manuscript with input from A.A.C., F.P. and A.M.
Corresponding author
Ethics declarations
Competing Interests
A.M. is an advisor to the European Food Safety Authority on the control of Bsal in Europe. L.D.F., A.A.C. and F.P. declare they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fitzpatrick, L.D., Pasmans, F., Martel, A. et al. Epidemiological tracing of Batrachochytrium salamandrivorans identifies widespread infection and associated mortalities in private amphibian collections. Sci Rep 8, 13845 (2018). https://doi.org/10.1038/s41598-018-31800-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-31800-z
Keywords
This article is cited by
-
United States amphibian imports pose a disease risk to salamanders despite Lacey Act regulations
Communications Earth & Environment (2023)
-
Broad host susceptibility of North American amphibian species to Batrachochytrium salamandrivorans suggests high invasion potential and biodiversity risk
Nature Communications (2023)
-
Batrachochytrium salamandrivorans’ Amphibian Host Species and Invasion Range
EcoHealth (2022)
-
Diversity, multifaceted evolution, and facultative saprotrophism in the European Batrachochytrium salamandrivorans epidemic
Nature Communications (2021)
-
Population structure, gene flow and relatedness of Natterer’s bats in Northern England
Mammalian Biology (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.