Abstract
Cardiovascular events in hypertensives are associated with elevated average blood pressure (BP) and higher short-term BP variability (V), but little is known on treatment effects on BPV and on how to assess changes in short-term BPV. Aim of our study was to address the methodology of short-term BPV assessment and its reduction by Lercanidipine (L) or Enalapril (E) and their combination, through analysis of 24-hour ambulatory BP recordings from two studies including subjects of different age. Study-1: 64 middle-age hypertensives (52.9 ± 9.5 yrs) received L and E s.i.d. at 10 mg (L10, E10) or 20 mg doses (L20, E20) for 8 weeks. Study-2: 66 elderly hypertensives (65.5 ± 4.7 yrs) received placebo, L10, E20 and L10 + E20 s.i.d. for 4 weeks. In middle-age subjects, both L and E decreased mean BP and, at the highest dose, also short-term BPV. In elderly subjects, L10 alone or in combination with E20 reduced BPV. Treatment-induced reductions in BP levels and BPV were uncorrelated. Different methods for short-term BPV assessment did not always provide superimposable results in the elderly. Our study supports a better reduction of BPV by L in the elderly and by E + L combination at any age, suggesting BPV reduction to be independent from reduction in average BP.
Similar content being viewed by others
Introduction
Evidence is available from observational studies and trials meta-analyses that cardiovascular events in hypertensive patients are associated not only with elevated average blood pressure (BP) levels but also with increased BP variability (V), in particular with an increased short-term BPV over 24 hours. 24 h BPV is a complex phenomenon, including BP fluctuations at different frequency, ranging from day-night BP changes to reading–to-reading BP variations, the former being associated with favorable, and the latter with unfavourable effects on organ damage and prognosis in hypertensive patients1. Thus, when quantifying BPV over 24 hours, it has been recommended to separately assess the degree of day-night BP reduction (dipping), whose occurrence is associated with a favorable impact on organ damage and prognosis, and the magnitude of faster BP fluctuations (short-term BPV), an increase of which is on the contrary associated with increased severity of organ damage and higher rate of cardiovascular events and cardiovascular mortality1. For this reason, recent methods for estimating 24 hour BPV have been proposed which allow assessment of short-term BPV while excluding the contribution of day-night BP changes1,2. Furthermore, on such a background, it has been suggested that anti-hypertensive treatment should be aimed at reducing not only BP levels, but also short-term BPV, while preserving nocturnal BP dipping1. The actual ability of antihypertensive treatment to reduce short-term BPV is still a matter of debate, however, as previous studies suggested that a reduction in BP standard deviation by treatment could be only the consequence of concomitant reduction in BP mean, without evidence of any direct and specific effect by antihypertensive drugs on BPV3. Moreover, limited information is available also on whether there is any difference among drug classes in this regard.
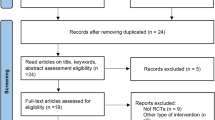
Therefore, aim of this work was to address the methods for assessing short-term 24 h BPV and to explore the effects on short-term BPV, measured over 24 hours by ambulatory BP monitoring (ABPM), of monotherapy with two commonly used antihypertensive drugs, targeting different mechanisms of cardiovascular regulation, i.e., a dihydropyridine calcium channel blocker (CCB) and an angiotensin converting enzyme inhibitor (ACEI), as well as of their combination. This was done by re-analyzing ABPM recordings, obtained in two previous studies aimed at exploring the 24-hour antihypertensive effect of the CCB Lercanidipine (L), the ACEI Enalapril (E) and their combination in essentially hypertensive patients of different ages: in middle-age subjects and in elderly subjects (Fig. 1).
Results
Middle-age patients (study 1)
Figure 2 shows the effects of treatments with L and E at 10 mg (L10, E10) and 20 mg (L20, E20) dosages separately on Systolic (S)BP, Mean Arterial Pressure (MAP) and Diastolic (D)BP mean levels and on two short-term BPV indices: the weighted standard deviation (SDW) and the average real variability (ARV). All treatments decreased significantly BP means over 24 hours. Short-term BPV indices were not influenced by low dose treatments, neither L10 nor E10, while high-dose treatments, L20 and E20, decreased significantly both indices. Reductions of short-term variability for MAP and DBP were more significant when quantified by ARV than by SDW.
BP levels and indices of short-term BP variability (SDW and ARV) over 24 hours in middle-age hypertensives (Study 1) as mean and standard error of the mean before (full symbols) and after (open symbols) each of four treatments (circle: L10; square: E 10; downward arrow: L20; upward arrow: E 20); the *and **indicate differences after vs. before treatment significant at 0.05 and 0.01 statistical levels. See text for abbreviations.
Before treatment, patients who received 20 mg doses (L20 and E20) had higher BP than those receiving 10 mg doses: this is likely due to a bias introduced by dose adjustment from 10 mg to 20 mg for those hypertensive individuals that did not normalize DBP after one month of the low dose treatment (see methods). However, the dose-adjustment procedure did not affect short-term BPV indices, being baseline values of ARV or of SDW similar for all treatments.
No significant associations were found between decreases in 24 hour levels of SBP, MAP or DBP, and decreases in their corresponding weighted standard deviation (SDW) for any of the four treatments (Table 1), with the exception of the effect of the E20 treatment on SBP. This association, however, was characterized by a negative slope which means that larger decreases in mean level were not associated with larger, but with smaller decreases of SDW.
Elderly patients (study 2)
Monotherapies with active compounds as well as their combination significantly decreased the 24-hour BP means compared to placebo in elderly hypertensive patients (Fig. 3). The decrease was more pronounced for E20 than for L10 (p < 0.01) and for the combined treatment L10 + E20 than for E20 (p < 0.01).
BP levels and indices of short-term BP variability over 24 hours (SDW and ARV) in elderly hypertensives (study 2) for each of four treatments (mean and standard error of the mean); the *and **indicate differences vs. placebo (P) significant at 0.05 and 0.01 statistical levels. See text for abbreviations.
Considering monotherapies, L10 decreased ARV significantly for MAP and DBP, while E20 did not have significant effects on short-term BPV. The combined treatment, L10 + E20 had marked effects on ARV, which decreased significantly for SBP, DBP and MAP. The combination treatment decreased also SDW, but for DBP only.
No significant associations were found between changes vs. placebo in 24-hour mean levels and changes vs. placebo in SDW of MAP and DBP for any active treatment (Table 1). As to SBP, a significant positive relationship between decreases in SBP level and decreases in SDW of SBP was found for the L10 + E20 treatment only. However, the fraction of change in SDW explained by the linear model was less than 5%.
Discussion
On the background of the accumulating evidence that cardiovascular events in hypertensive patients are associated not only with higher BP mean levels but also with increased BPV, in particular when focusing on short-term BPV over 24 hours1, our study contributes to the debate on the possibility that antihypertensive treatments have a direct effect in buffering BPV, by investigating a few issues of practical relevance. In particular, our study addresses three aspects: (1) the possible difference in the effects on BPV exerted by two classes of drugs (ACEI and CCB) and by their combination; (2) the possible influence of ageing on the effects of these drugs on BPV; and (3) whether a drug-induced reduction in BP standard deviation might be consequence of the concomitant drug-induced reduction in mean BP level, or whether it might rather reflect a specific drug action on BPV. To address the first two issues, we have compared the effects of an ACEI, of a CCB and of their combination on short-term BPV over 24 hours, by considering different drug dosages and their administration to individuals of different age. To address the third issue, in both studies we have investigated whether the degree of reduction in mean is or is not correlated to the degree of reduction in standard deviation.
Results of study 1 show that in middle age individuals both the CCB Lercanidipine and the ACEI Enalapril are effective in reducing 24-hour BP levels either at the dose of 10 and of 20 mg given once a day. They are also effective in reducing short-term BPV, but only at their higher dose of 20 mg. These findings suggest that low dose treatments, capable of reducing 24-hour BP levels, might not be powerful enough to also reduce BPV, i.e. the dynamic component of BP reflecting the interaction between environmental stimuli and the cardiovascular control mechanisms of a given subject.
Results of study 2, on elderly hypertensive patients, partly differ in terms of BPV from those of study 1 carried out in middle aged individuals. In fact, no reduction in short-term BPV could be seen under treatment with ACEI Enalapril 20 mg, while short-term variability of DBP and MAP as quantified by ARV were significantly reduced by CCB Lercanidipine even at the low dose of 10 mg. These results could be partly explained by the tendency towards a reduced efficacy of ACE inhibitors in elderly individuals4,5, in whom these drugs may be effective enough in reducing mean BP levels6, but may be less effective than CCBs in buffering short-term BPV. Even if the relatively low dose of CCB Lercanidipine tended to decrease ARV also for SBP, the reduction did not reach the statistical significance as for MAP and DBP. This may be due to the fact that DBP fluctuations reflect modulations of peripheral resistance better than SBP fluctuations. Therefore, they can be more effectively reduced by a CCB than by an ACEI in the elderly, in whom baroreflex modulation of peripheral resistance is known to be impaired7 and arterial stiffness increased. Combination treatment with an ACEI and a CCB was more effective not only in reducing 24-hour BP levels, but also in reducing most indices of BPV in this elderly cohort.
To evaluate whether an association exists between the reduction in BP level and the reduction in BP variability, we calculated a total of 21 regressions between BP mean and SDW (Table 1). The only significant association with a positive slope regards the effect of L10 + E20 vs. placebo on SBP. However, the percentage of explained variability is less than 5%, indicating that even if the association were real (and not due to chance) the possible direct effect of the reduction of SBP mean on the reduction of SBP SDW is minimal. This excludes that a reduction in BPV is just a consequence of the concomitant reduction in BP level due to a relation between central value and dispersion for the statistical distribution of BP measures. This lack of correlation makes also unlikely that treatments may have activated one single mechanism which deterministically reduced the BP level and the BP variability simultaneously. It may also explain why SDW and ARV from 24-hour ambulatory BP monitoring were associated with highly significant hazard ratios for total mortality even after adjustment for the 24-hour BP level, which is expected to have a greater prognostic value8. Furthermore, it may explain the significant risk reclassification of BP variability (particularly during nighttime) when added to fully-adjusted models9.
A merit of our study is the assessment of 24-hour BPV with indices that specifically quantify short-term BP fluctuations (reported to carry an increased risk of cardiovascular complications), while excluding the contribution to 24-hour BPV of nocturnal BP fall (which in contrast is known to have a favourable prognostic meaning)1,10. In this regard, we employed two indices that quantify the effects of treatments on BPV with a different sensitivity, and this is probably due to the different weight that slower and faster components of short-term BPV have in determining ARV and SDW values (see methods). To the best of our knowledge, our study is the first addressing these methodological issues in a clinical perspective, offering indications for a better standardization of methods for assessing short-term BPV in clinical trials. This is an important issue, given that proper comparison of data from previous studies exploring the clinical relevance of BPV has been so far made difficult by the diverse methods used by different investigators1. Therefore, our study also underlines the utility to decompose short-term BPV into faster and slower components, in order to more precisely evaluate the effects of treatments or to better stratify the cardiovascular risk associated to short-term BPV.
Our study offers information also on the possibility that some antihypertensive agents might reduce BPV independently from a reduction in mean BP levels, which is yet a debated issue3. The demonstration of uncorrelated changes in BP mean and standard deviation supports the usefulness of focusing on the reduction of both BP and BPV. Indeed, our results should be interpreted on the background of previous studies on this issue. In rats, BPV is an independent determinant of end-organ damage11 and CCB may reduce BPV and protect against end-organ damage, independently from the reduction in mean BP12. Also in a clinical setting CCB treatment reduced daytime and nighttime variability of SBP and improved arterial baroreflex modulation of heart rate in diabetic hypertensive patients, although this demonstration was provided through BP recordings at the finger artery level, where pulse waveforms may be differently amplified in different individuals, as a function of differences in stroke volume and arterial stiffness13. A more recent study evaluated the antihypertensive effects of an ACEI alone or associated with CCB or with a diuretic, and showed that BPV decreased when the ACEI was combined with a CCB, and that conversely it did not change when ACEI was combined with a diuretic14.
Evidence that CCBs might be superior to other drug classes in reducing BPV, probably because of their effects on arterial wall properties1, has also been provided by studies focusing on mid-term (day-by-day) and long-term (visit-to-visit) BPV. In particular, in a study by Matsui et al., mid-term BPV was quantified from day-by-day changes of home BP in patients initially treated with an angiotensin antagonist (olmesartan) and then randomly assigned to receive additionally either a CCB (azelnidipine) or a diuretic (hydrochlorothiazide)14. The addition of azelnidipine led to a significantly larger reduction in mid-term BPV than the addition of hydrochlorothiazide, with similar reductions in mean BP in both groups. Moreover, the BPV reduction in the azelnidipine group was independently related to a reduction in aortic stiffness (assessed through carotid-femoral pulse wave velocity)14,15.
Moreover, retrospective analyses of the ASCOT BPL and the UK-TIA trials focusing on visit-to-visit BPV provided evidence of a superior reduction of BPV by the CCB amlodipine as compared to other drug classes, in particular to the beta blocker Atenolol16,17,18. More recently, when focusing on 24-hour BPV in the X-CELLENT study, treatment with amlodipine, a long lasting CCB, was associated with a greater reduction in different measures of 24-hour BPV than treatment with Indapamide, Candesartan and placebo19. Our study offers novel information on the role of dihydropyridine CCBs in reducing short-term BPV by comparing different doses, with and without combined administration of a drug blocking the renin-angiotensin system, in patients of different age.
We should acknowledge some limitations of our work. First, it is based on the retrospective analysis of studies previously performed for other purposes, although the methodology used for ABPM did allow for an accurate assessment of parameters measuring BPV. Moreover, the number of patients investigated was not high, limitation, however, counteracted by the crossover design of these studies. Therefore, some negative results might be due to the limited sample size of these investigations.
In spite of the above limitations, our study does support the possible advantages offered by antihypertensive treatment based on a CCB or on its combination with an ACEI in reducing not only BP levels, but also short-term BPV. These findings, and their possible impact on cardiovascular prognosis, pave thus the way for additional longitudinal intervention studies of adequate size, which are needed to definitely clarify these issues. In particular, they may have practical implications for planning larger intervention trials targeting BPV and for improving cardiovascular risk reduction in hypertensive patients of different age. Finally, the methodological information provided by our study on different indices quantifying short-term 24 h BPV might help in achieving a better standardization of BPV assessment in clinical trials.
Methods
Subjects and studies design
We considered ABPM data recorded in two previous cross-over studies that involved 1) middle-age hypertensive patients receiving monotherapy with an ACEI and a CCB (Study 1), and 2) elderly hypertensive patients treated with the same ACEI and the same CCB as monotherapy or in combination (Study 2), see Fig. 1. Details are reported hereafter.
Both study protocols were approved by the local Ethics Committee of the centers involved (TUKIJA – Lääketieteellinen tutkimuseettinen jaosto, Helsinki, Finland; HUS – Sisatautien eettinen komitea HYKS Meilahden Sairaala, Helsinki, Finland; Comité Ético de Investigación Clínica, Santiago de Compostela, Spain; Comité Ético de Investigación Clínica, Madrid, Spain) and were conducted in accordance with the Declaration of Helsinki and Good Clinical Practice. All subjects gave written informed consent to participate.
Study 1 (middle-age patients)
This was a single-blind cross-over study conducted on 64 patients with essential hypertension (27 females, 37 males; age 52.9 ± 9.5 yrs, mean ± SD), that received the calcium antagonist Lercanidipine (Zanidip, Recordati, Italy) and the ACEI Enalapril (Renitec, MSD, Belgium) in a random sequential order. Each patient was also randomly assigned to receive L at doses of 10 mg or 20 mg once-a-day, and E at doses of 10 mg or 20 mg once-a-day.
Each treatment lasted 8 weeks and was preceded by 3 weeks of wash out. Initial E10 mg and L10 mg doses could be increased to E20 mg and L20 mg, if clinic DBP remained higher than 90 mmHg or decreased by less than 10 mmHg after one month of treatment. Each subject underwent a 24-hour ABPM immediately before and after each treatment. The ABPM device was set to obtain readings of systolic SBP, DBP and MAP every 15 minutes from 6 am to 10 pm and every 30 minutes from 10 pm to 6 am.
Study 2 (elderly patients)
This was a four-way, balanced, crossover study conducted on elderly hypertensive patients. Inclusion criteria were: age between 60 and 85 years, baseline clinic SBP between 160 and 179 mmHg and clinic DBP lower than 110 mmHg in sitting position, combined with a mean daytime SBP ≥ 135 mmHg at baseline, measured by ABPM. Patients with history of cerebrovascular or cardiac complications were excluded.
After a wash-out period of 2 weeks, each patient was randomized according to a double-blind design to receive for 4 weeks placebo, L10, E20, and the combination of the two active treatments (L10 + E20) once/day, all administered according to randomized sequences, for a total therapy duration of 16 weeks. At the end of each treatment, patients performed a 24-hour ABPM. As in study 1, the ABPM device was set to obtain readings every 15 minutes from 6 am to 10 pm and every 30 minutes from 10 pm to 6 am. Seventy-five patients were randomized (see20 for details). In the present study we considered the 66 of them (31 females, 35 males; age 65.5 + 4.7 yrs) that completed at least three treatments with a valid ABPM recording after each treatment.
For both studies, 24-hour ABPM recordings were performed with a validate device applied to the non-dominant arm (Spacelabs Healthcare, Issaquah, WA).
Short-term BPV Indices
For each recording, mean values of SBP, MAP and DBP were computed over the whole 24-hour tracing. Two indices of short-term BPV were estimated: the weighted 24 h standard deviation and the Average Real Variability.
Night-time sleep period (SLEEP) and day-time wake period (WAKE) were identified based on the “wake up” and “go to bed” times that patients reported in their diary, and SDW was calculated for SBP, MAP and DBP separately as:
where nSLEEP and nWAKE are the number of ABPM measures for each BP series during SLEEP and WAKE periods, SDSLEEP and SDWAKE are the corresponding standard deviations10.
The Average Real Variability (ARV) was calculated as:
with \({w}_{k}={t}_{k+1}-{t}_{k}\) being the time interval between the k + 1 and k consecutive measures, and n the total number of BP measures (SBP, MAP or DBP) in 24 hours8.
The SDW and ARV indices offer a somewhat different quantification of short-term BPV. SDW is a measure of BP dispersion around the mean, like the traditional standard deviation; however, at variance from the conventional 24-hour standard deviation, it removes the difference between day and night BP levels from the measure of BP values dispersion. By contrast, ARV is not a measure of dispersion of BP values, but a measure of dispersion of the differences between consecutive BP readings. The paragraph “SDW vs. ARV” illustrates how SDW and ARV weight differently faster and slower components of short-term BPV.
Statistical Analysis
Normality of distributions of BP mean values and of short-term BPV indices was tested in each condition and for each treatment separately by the Shapiro-Wilks test. Short-term BPV indices passed the normality test after log-transformation. Differences between BEFORE and AFTER conditions for the four treatments (L10, L20, E10 and E20) of study 1 and comparison among the four treatments (placebo, L10, E20 and L10 + E20) of study 2 were performed by applying Linear Mixed-Effects Models with a posteriori contrasts accounting for repeated measurements and compound symmetry covariance structure, fitting the models by maximizing the restricted log-likelihood. For multiple post-hoc comparisons, the expected rate of false-positive results for all positive results was controlled by the false discovery rate algorithm21.
For some theoretical probability distributions (like the exponential distribution), mean and standard deviation are not independent quantities, but any decrease (or increase) of the mean is mathematically associated with a decrease (or increase) of standard deviation. To exclude that a similar mechanism, possibly caused by a particular data distribution, may be responsible for observing a reduction of BPV after a treatment that reduced the mean BP, we evaluated the associations between decreases in 24 hour BP mean and short-term standard deviation. This was done by calculating differences in the 24 hour BP mean (ΔMEAN24H) and in SDW of BP(ΔSDW) between the BEFORE-treatment and the AFTER-treatment conditions (study 1) or between placebo and each active treatment (study 2). Then, linear regressions between ΔMEAN24H and ΔSDW were calculated for each treatment. An association between decreases in mean and in standard deviation is revealed by a statistically significant correlation and a positive slope (β1 coefficient). The threshold for statistical significance was set at 0.05; all analyses were performed using R Core Team software (2015), Vienna, Austria.
SDW vs. ARV
ARV and SDW indices assess the effects of treatments on short-term BPV with different sensitivity. The reason lies in the different nature of the variability components they quantify. SDW measures the standard deviation of BP residuals after removal of nighttime and daytime levels, quantifying all the variability components of BP residuals with the same weight, regardless of their oscillation periods. By contrast, ARV measures the amplitude of the difference between consecutive BP samples, in this way giving a greater weight to the faster components.
In fact, let’s consider a hypothetical sinusoidal component, BPi(t), of amplitude Ai and period Ti:
and assume that BP is measured every Δt seconds, so that the k-th sample corresponds to the time instant tk = kΔt seconds. The difference between two successive samples, tk+1 and tk, is:
By applying the sum-to-product trigonometric identity, Equation (4) can be rewritten as:
with
and
Therefore also the series of differences between consecutive BP samples is a sinusoid with period Ti, as BPi(t), but with different phase and different amplitude. In particular, the amplitude depends on the Δt/Ti ratio, and lower is this ratio, lower is Di. This means that BP oscillations with different period contribute differently to ARV.
Discrepancies between SDW and ARV can be understood simulating a BP(t) series sampled every 15 minutes as sum of three components (Fig. 4). First component, BPF, is a fast sinusoidal oscillation with 10-mmHg amplitude and 90-minute period (TF = 3600 s). Second component, BPS, is a slow sinusoidal oscillation with the same amplitude (10 mmHg) and 5-hour period (TS = 14400 s). Third component, BPN/D, represents the night/day modulation by a square wave between 110 mmHg during daytime (from 7:30 to 21:30) and 90 mmHg during nighttime (from 21:30 to 7:30). The SDW of the night/day modulation is clearly null. The fast and slow oscillations have the same SDW (7.1 mmHg) because SDW depends on the amplitude and not on the period of the oscillation. The SDW of the resulting simulated BP series, BPTOT, is 10.0 mmHg, value that coincides with the square root of the sum of SDW’s squared of the three components (we recall that the power of the sum of sinusoids with different frequencies equals the sum of the power of each sinusoid). Therefore, fast and slow oscillations contribute equally to the SDW of BPTOT.
BPTOT (lower panel) is a synthesized BP continuous signal obtained by summing a fast (BPF) and a slow (BPS) sinusoidal oscillation to a night/day modulation with square-wave shape (BPN/D). The dot symbols indicate simulated measures obtained with an ABPM device that samples the BP signals every 15 minutes; SDW is the weighted standard deviation of each sampled BP series.
This is not the case for ARV. To evaluate ARV, we should first calculate the difference between consecutive BP samples. By applying Equation (4), with Δt/TF = 900/5400 and Δt/TS = 900/21600, we obtain that the amplitude of the differentiated fast component is DF = 10.0 and of the differentiated slow component is DS = 2.6. Figure 5 shows clearly the lower amplitude of the slow oscillation, and therefore ARV is higher for the faster oscillation. The differentiated night/day component is zero at all times except two instants with the fast transition from night to day and from day to night, which contribute minimally to the overall ARV.
Synthesized BP signals of Fig. 4 after differentiation; ARV is the average real variability of time series obtained by simulating the sampling of an ABPM device every 15 minutes.
Table 2 quantifies how the fast and the slow components contribute to the overall short term variability. It compares SDW and ARV of BPTOT, considered as the 100% reference, with the values estimated by excluding from BPTOT only the fast components (BPTOT-BPFAST), or only the slow component (BPTOT-BPSLOW). Table 2 points out that the contribution to ARV of BPTOT of the slow component is much smaller than the contribution of the fast component, while these two components contribute similarly to the SDW of BPTOT.
Considering the frequency of readings of the ABPM devices used in study 1 and 2, the slow components that affect SDW without influencing ARV importantly are those with time scales of hours. These could be the BP changes associated with the circulatory long-term control of the renin-angiotensin-aldosterone system over the 24-hour period and, during sleep, the possible long-term BP modulations associated with the 100-minute alternation of REM and NREM sleep. By contrast, the faster BP changes that are expected to influence ARV more than SDW could be the BP fluctuations associated with sleep related breathing disorders during night-time, or the BP changes associated with postural changes or with everyday activities during daytime.
References
Parati, G., Ochoa, J. E., Lombardi, C. & Bilo, G. Assessment and management of blood-pressure variability. Nat. Rev. Cardiol. 10, 143–155 (2013).
Mancia, G. et al. Long-term prognostic value of blood pressure variability in the general population: results of the Pressioni Arteriose Monitorate e Loro Associazioni Study. Hypertension 49, 1265–1270 (2007).
Mancia, G., Omboni, S., Ravogli, A., Parati, G. & Zanchetti, A. Ambulatory blood pressure monitoring in the evaluation of antihypertensive treatment: additional information from a large data base. Blood Press 4, 148–156 (1995).
Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 288, 2981–2997 (2002).
Wing, L. M. et al. A comparison of outcomes with angiotensin-converting–enzyme inhibitors and diuretics for hypertension in the elderly. N. Engl. J. Med. 348, 583–592 (2003).
Mancia, G. et al. ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur. Heart J. 34, 2159–2219 (2013).
Mancia, G. & Mark, A. L. Handbook of Physiology, The Cardiovascular System, Peripheral Circulation and Organ Blood Flow., pp. 755–793 (2011).
Hansen, T. W. et al. Prognostic value of reading-to-reading blood pressure variability over 24 hours in 8938 subjects from 11 populations. Hypertension 55, 1049–1057 (2010).
Palatini, P. et al. Added predictive value of night-time blood pressure variability for cardiovascular events and mortality: the Ambulatory Blood Pressure-International Study. Hypertension 64, 487–493 (2014).
Bilo, G. et al. A new method for assessing 24-h blood pressure variability after excluding the contribution of nocturnal blood pressure fall. J. Hypertens. 25, 2058–2066 (2007).
Miao, C. Y., Xie, H. H., Zhan, L. S. & Su, D. F. Blood pressure variability is more important than blood pressure level in determination of end-organ damage in rats. J. Hypertens. 24, 1125–1135 (2006).
Liu, J. G., Xu, L. P., Chu, Z. X., Miao, C. Y. & Su, D. F. Contribution of blood pressure variability to the effect of nitrendipine on end-organ damage in spontaneously hypertensive rats. J. Hypertens. 21, 1961–1967 (2003).
Frattola, A. et al. Lacidipine and blood pressure variability in diabetic hypertensive patients. Hypertension 36, 622–628 (2000).
Matsui, Y. et al. Combined effect of angiotensin II receptor blocker and either a calcium channel blocker or diuretic on day-by-day variability of home blood pressure: the Japan Combined Treatment With Olmesartan and a Calcium-Channel Blocker Versus Olmesartan and Diuretics Randomized Efficacy Study. Hypertension 59, 1132–1138 (2012).
Parati, G. & Bilo, G. Calcium antagonist added to angiotensin receptor blocker: a recipe for reducing blood pressure variability? Evidence from day-by-day home blood pressure monitoring. Hypertension 59, 1091–1093 (2012).
Rothwell, P. M. et al. Effects of beta blockers and calcium-channel blockers on within-individual variability in blood pressure and risk of stroke. Lancet Neurol. 9, 469–480 (2010).
Rothwell, P. M. et al. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet 375, 895–905 (2010).
Webb, A. J. & Rothwell, P. M. Effect of dose and combination of antihypertensives on interindividual blood pressure variability: a systematic review. Stroke 42, 2860–2865 (2011).
Zhang, Y., Agnoletti, D., Safar, M. E. & Blacher, J. Effect of antihypertensive agents on blood pressure variability: the Natrilix SR versus candesartan and amlodipine in the reduction of systolic blood pressure in hypertensive patients (X-CELLENT) study. Hypertension 58, 155–160 (2011).
Puig, J. G. et al. Lercanidipine, enalapril and their combination in the treatment of elderly hypertensive patients: placebo-controlled, randomized, crossover study with four ABPM. J Hum. Hypertens. 21, 917–924 (2007).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society, Series B 57, 289–300 (1995).
Acknowledgements
The authors wish to thank Recordati S.p.A. for kindly making the ABPM data available for our analysis free of charge.
Author information
Authors and Affiliations
Contributions
G.P. conceived the study. A.F. performed the statistical analysis. A.F., G.P., S.O. and P.C. fulfilled data interpretation and wrote the manuscript. P.C. elaborated the theoretical analysis. All authors critically revised the manuscript.
Corresponding author
Ethics declarations
Competing Interests
G.P. and S.O. received an unrestricted grant by Recordati S.p.A. for educational activities on BPV.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Parati, G., Castiglioni, P., Omboni, S. et al. Effects on 24-hour blood pressure variability of ace-inhibition and calcium channel blockade as monotherapy or in combination. Sci Rep 8, 13779 (2018). https://doi.org/10.1038/s41598-018-31746-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-31746-2
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.