Abstract
We evaluated the performance of 3 different left ventricular leads (LV) for resynchronization therapy: bipolar (BL), quadripolar (QL) and active fixation leads (AFL). We enrolled 290 consecutive CRTD candidates implanted with BL (n = 136) or QL (n = 97) or AFL (n = 57). Over a minimum 10 months follow-up, we assessed: (a) composite technical endpoint (TE) (phrenic nerve stimulation at 8 V@0.4 ms, safety margin between myocardial and phrenic threshold <2V, LV dislodgement and failure to achieve the target pacing site), (b) composite clinical endpoint (CE) (death, hospitalization for heart failure, heart transplantation, lead extraction for infection), (c) reverse remodeling (RR) (reduction of end systolic volume >15%). Baseline characteristics of the 3 groups were similar. At follow-up the incidence of TE was 36.3%, 14.3% and 19.9% in BL, AFL and QL, respectively (p < 0.01). Moreover, the incidence of RR was 56%, 64% and 68% in BL, AFL and QL respectively (p = 0.02). There were no significant differences in CE (p = 0.380). On a multivariable analysis, “non-BL leads” was the single predictor of an improved clinical outcome. QL and AFL are superior to conventional BL by enhancing pacing of the target site: AFL through prevention of lead dislodgement while QL through improved management of phrenic nerve stimulation.
Similar content being viewed by others
Introduction
Cardiac resynchronization (CRT) is a proven heart failure therapy, but a minority of patients (pts) have no clinical benefit1. The lack of improvement is multi-faceted, owing both to pts selection and technical CRT issues. Phrenic nerve stimulation (PNS), high myocardial threshold (HMT), left ventricular lead dislodgement (LD) and failure to achieve the target pacing site are the most frequent technical issues1,2, that were aimed at by the introduction of new left ventricular leads such as the quadripolar (QL) and the bipolar active fixation leads (AFL)3,4,5,6. This is the first study comparing 3 different LV lead platforms for CRT with defibrillator: bipolar passive fixation lead (BL), QL and AFL. The purpose was to evaluate at long term the performance of these 3 different LV leads from both the technical and clinical outcome standpoint.
Methods
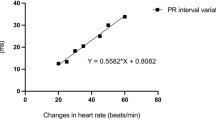
This was a single center observational study carried out on pts consecutively implanted with a CRT with defibrillator (D) and 3 different LV lead platforms: BL, QL and AFL. The study of LV performance was approved by the local Ethic Committee of the University Hospital S.Orsola-Malpighi (Bologna, Italy) and complies with the principles outlined in the Declaration of Helsinki. Pts provided informed consent for data collection and analysis. All the 4 implanting physicians have ≥10 years experience in CRT implantation, hence a learning-curve effect was excluded. The study enrolled all the pts implanted with CRT-D from January 2012 to June 2015. Pts with life expectancy <12 months were excluded. BL were implanted from January 2012 to December 2013; QL from June 2012 to June 2015, bipolar AFL were implanted from September 2013 to June 2015 (when they became available). Since December 2013 onward any bipolar lead implanted was an AFL. During the implant procedure an angiogram (obtained with an occlusive catheter) was taken in 45° left anterior oblique view (LAO) and in 30° right anterior oblique view (RAO). The target pacing site (TPS) was defined as the site with the longer Q-LV among all accessible veins7 sized at least 5 F. Preoperative imaging helped the selection process: areas of scarred tissue as detected by history of previous MI, echocardiography, SPECT, MR scan, were avoided to ensure stimulation of viable LV tissue, that predisposes to CRT non-response8. Q-LV was firstly measured at the great cardiac vein placement, then in the other coronary veins that had a minimum 5 F diameter (as showed by the angiogram), starting from the easiest accessible and ending with the more challenging one. Only coronary veins having a ratio Q-LV/total QRS duration ≥0.7 were considered suitable for the TPS. Thus, a TPS was achieved when this ratio was obtained by any available LV electrode7. When it became available, an AFL was preferred in the presence of a suitable coronary vein leading to posterior or lateral or antero-lateral site whose length was not exceeding 4 cm, whereas a QL was chosen for longer veins. LV leads location is shown in Fig. 1. Pacing configuration (LV-only vs Biventricular), atrioventricular and interventricular delay optimization occurred before discharge in all patients. “LV only” pacing configuration means LV stimulation avoiding right ventricle stimulation in the event of a normal intrinsic PR interval. The atrioventricular and interventricular optimization was guided by ECHO with the iterative method.
LV myocardial threshold, pacing impedance and phrenic nerve threshold were evaluated before discharge and at follow-up (in all pacing vector configurations). All the pts were evaluated clinically before implantation, at hospital discharge, and after at least 10 months of continuous resynchronization therapy.
We assessed composite technical endpoint (TE), clinical endpoint (CE), and LV reverse remodeling (RR) by Echocardiography.
Definition of the composite TE
PNS at 8 V@0.4 ms in at least one pacing configuration (all the programmable LV pacing configuration were tested); safety margin between myocardial and phrenic threshold <2 V in the chosen pacing configuration not correctable with pacing vector reprogramming; left ventricular lead dislodgement requiring a re-operation and correctable with pacing vector reprogramming (variation of myocardial threshold >1.5 V suggested a possible LV lead dislodgement that need to be confirmed with an X-ray in antero-postero and latero-lateral view); failure to achieve the TPS.
Definition of composite CE
death for any cause, hospitalization for heart failure and heart transplantation after at least 10 months of resynchronization therapy; infection leading to lead extraction.
RR (reduction of end systolic volume >15% compared to the value before the implant) was evaluated by the echocardiography according to Ypenburg classification9 after 10 months of continuous CRT (percentage of pacing >99%). The reproducibility of measurements in our center has been previously reported10.
Statistical Analysis
Descriptive statistics are reported as mean ± standard deviation (SD) for normally distributed variables
Categorical variables are reported as percentages and were statistically tested by means of the χ2. Freedom from clinical and technical endpoints was studied by means of the Kaplan–Meier method. Univariate Cox proportional hazards models were used to investigate the predictors of clinical outcome. Variables that showed an effect on the clinical outcome with a significance level <0.2 in the univariate analysis were entered into the multivariate Cox proportional hazards models. Cox model findings are presented as hazard ratios (HRs) and 95% confidence intervals (CIs). A two-tailed p-value of <0.05 was considered statistically significant.SAS 9.3, SAS Institute Inc., Cary, NC, USA was used for statistical analysis.
Results
Population
Table 1 reports clinical characteristics according to the implanted lead. BL group had a slightly lower EF owing to implantation before the 2013 guidelines11 release (NYHA 3–4 patients more represented), whereas the AFL patients were on average older, with higher prevalence of old females, AF, diuretic use and comorbidities. All the patients were on optimized medical therapy for heart failure therapy. The leads used in the study period are reported in Table 2. During follow up, CRT delivery was not significantly different across the groups, 97.8% (BL) vs 99% (QL) vs 100% (AFL).
Technical composite endpoint
The incidence of composite technical endpoint at long term follow up is reported in Table 3 and Fig. 2; overall TE occurred in 27.5%, but did not prevent CRT delivery in any patient during follow-up. Dislodgment requiring re-operation occurred in 10 (7.4%) BL patients, in 4 (4.1%) QL patients (2 with a Quartet St. Jude Medical leads and 2 with Performa Medtronic leads), and in no AFL patient. Five of these patients (4 with a BL and 1 with a QL) could no longer be paced in the same targeted site because of coronary vein occlusion (after the LV lead dislodgement).
Significant differences in the composite TE were observed amongst the 3 LV lead groups: QL enabled superior management of PN, whereas AFL proved superior for LV targeting and prevention of dislodgment (Table 3, Fig. 2) regardless of a difficult coronary vein anatomy and right atrial enlargement (Fig. 3).
Coronary sinus angiogram and target pacing site evaluation. Panel A: coronary sinus angiogram that showed a lateral short vein; panel B: Q-LV methods for the electrical delay evaluation9; panel C: final left ventricular lead position in right anterior oblique (RAO) view; panel D: final left ventricular lead position in left anterior oblique (LAO) view.
Composite clinical endpoint
The incidence of composite clinical endpoint at 12 months follow up was 10.3% without significant differences between the 3 groups (p = 0.38) (Table 3, Fig. 4). Infections leading to system removal occurred in 2 pts (one in BL group and the other in the QL group) after respectively 8 and 6 months from implantation (Table 3).
Reverse remodeling
At follow up 170/270 (63%) living patients had reverse remodeling (reduction of ESV > 15%), but there were differences in the 3 LV lead groups (Fig. 5): responders were 56%, 68%, 64% respectively in BL, QL and AFL (p = 0.02). No significant differences occurred between QL and AFL. On a multivariable regression analysis, only “non-BL leads” were associated to an improved clinical outcome (reverse remodeling + free from heart failure related hospitalizations/death/heart transplantation; see Table 4).
Reverse remodeling and quality of response11 by 10-months Echocardiography.
Discussion
This is an observational cohort, not a randomized clinical trial with the inherent limitation (as described in the dedicated section) but representing the real world. Our study highlights that QL and mostly AFL enable an easier targeted LV lead placement compared to traditional BL, with a trend in favor to less heart failure-related hospitalizations. Owing to superior stability coupled with small size, trackability along tortuous veins and steroid elution on either tip or ring electrode, the Attain StabilityTM proved superior in overcoming the main challenges to LV lead implantation at a targeted placement site regardless of coronary vein anatomy and risk of dislodgement. In fact, short and thin veins as long as 3 cm could be considered for LV lead stimulation (Figs 1 and 3). Targeted LV stimulation has indeed demonstrated to increase the chances of RR and clinical improvement following CRT implantation12.
Technical Endpoint and LV leads
PN, LV lead dislodgement and high LVT prevent a stable and targeted CRT delivery along follow up, thus creating the background for CRT-nonresponse2,3,4,5,6,13,14. New multipolar leads enable an easier management of PN and broader possibilities to reach the target stimulation site. Despite this, the LVT threshold at the target location may not differ from one lead platform to the other, being dependent on local tissue properties, electrode technology, and stabilization strategy2,3,4,5,6,13,15. Whereas QL leads ensure an easier management of PN and fewer lead dislodgments compared to conventional BL leads in comparative studies16, the dislodgement rate of QL was 3.5% at 3 months in Tomassoni multicenter study5, and very similar at one year in this study (with some differences across manufacturers). Enhanced stability portends improved clinical outcome: Forleo et al.16 observed a reduction of heart failure-related hospitalizations and of LV lead dislodgements by QL compared to conventional BL, although the study was not randomized and no strategy for coronary vein selection was used for both type of leads. Being RR data not reported in that study16, it is likely that the clinical outcome has been influenced also by factors other than the QL technology, that is the TE may not be related to the CE. In our study, the strategy aimed at the latest activated site of the accessible veins at least 5 F in size in all the patients, CRT delivery was optimized and delivered at the same extent in all the patients, hence the incidence of TE, the RR extent and the CE can be associated to lead technology.
Clinical Endpoint
Resynchronization therapy is a customized therapy, targeted pacing site being a key point for LV reverse remodeling and long-term outcome12. LV lead placement at a scar-free site8,17 possibly mechanically12 or electrically delayed (Fig. 3 panel B) improve RR up to 70% of patients. Avoidance of LV dislodgement over the first year after implantation is hence of pivotal importance, since displacement has been reported to reach a ceiling after 10 months11,14,15. Under this perspective, the use of AFL enhances the capability of targeted LV lead placement4 while ensuring stability over the long term (Table 3), possibly improving the clinical outcome (Table 3). This is particularly important as only 35% of patients have more than a single coronary vein suitable to LV lead placement6, and QL leads may not be successfully implanted in up to 7% of patients17,18. Despite these considerations in our study the “novel technologies”, while significantly increasing RR, failed to show an improvement in clinical composite score. The reason for this result presumably lay in study design which compared three active strategies for CRT (and not a placebo/drug-only arm) that may require longer follow-up time to show superiority in terms of survival/hospitalization. However, in view of the close relationship between RR and clinical outcomes we believe that future studies with larger cohorts and longer follow-up will obtain positive results also in terms of hospitalization reduction and even survival. One possible limitation of bipolar AFL could be the impossibility to elicit multi-point LV stimulation at inter-electrode intervals broader than 20 mm; this novel technology awaits to prove superiority in non-responders to single site LV stimulation in the randomized More-CRT MPP study (Clinical Trials.gov Identifier NCT02006069), and has been shown to have a highly individual efficacy on acute hemodynamic measurements, when a strictly pathophysiologic approach is applied19. Some concern could be raised about AFL extractability in the event of CIED infection: the conception of the Attain StabilityTM lead is such to minimize the labor of lead extraction, and although leads being in place for several years have to be challenged, we previously reported an uneventful extraction procedure in a patient (not included in this population being a CRTP recipient) with a device infection implanted with an AFL lead20.
Limitations
This is a single center, retrospective non-randomized study that reflects the clinical practice in CRT at an experienced teaching hospital in consecutively implanted patients. The population is outnumbered for mortality endpoints, and a longer follow up could strengthen our argumentation. Moreover, the potential confounders in the assessment of CE were even among the study groups owing to a similar care in device tailoring and CRT delivery along follow up. Finally we must remember that measuring RR with echocardiography is challenging and shows important inter-observer variability even if our inter-observer variability is quite good10.
Conclusions
Left ventricular QL and AFL enable a superior RR compared to conventional BL, owing to a decreased dislodgement rate from the targeted stimulation site and freedom from other technical challenges21. AFL and QL solve the same technical issues, but in different way, the first one with the active fixation and the second one with electronic repositioning. Both new technologies permit a targeted pacing, then AFL is the best lead to prevent dislodgement instead QL is the best for the PN management.
Data Availability Statement
The datasets generated during the current study are not publicly available due to restrictions claimed by the ethical committee but are available from the corresponding author on reasonable request and formal request to the local ethical committee.
References
Auricchio, A. & Prinzen, F. W. Non-responders to cardiac resynchronization therapy: the magnitude of the problem and the issues. Circ J 75, 521–7 (2011).
Biffi, M. et al. Occurrence of phrenic nerve stimulation in cardiac resynchronization therapy patients: the role of left ventricular lead type and placement site. Europace 15, 77–82 (2013).
Crossley, G. H. et al. Performance of a novel left ventricular lead with short bipolar spacing for cardiac resynchronization therapy: primary results of the Attain Performa quadripolar left ventricular lead study. Heart Rhythm 12, 751–8 (2015).
Keilegavlen, H., Hovstad, T. & Faerestrand, S. Active fixation of a thin transvenous left-ventricular lead by a side helix facilitates targeted and stable placement in cardiac resynchronization therapy. Europace 18, 1235–40 (2016).
Tomassoni, G. et al. Postoperative performance of the Quartet(R) left ventricular heart lead. J Cardiovasc Electrophysiol 24, 449–56 (2013).
Ziacchi, M. et al. Left Ventricular Reverse Remodeling Elicited by a Quadripolar Lead: Results from the Multicenter Per4mer Study. Pacing Clin Electrophysiol 39, 250–60 (2016).
D’Onofrio, A. et al. The interventricular conduction time is associated with response to cardiac resynchronization therapy: interventricular electrical delay. Int J Cardiol 168, 5067–8 (2013).
Leyva, F. et al. Cardiac resynchronization therapy guided by late gadolinium-enhancement cardiovascular magnetic resonance. J Cardiovasc Magn Reson 13, 29 (2011).
Ypenburg, C. et al. Long-term prognosis after cardiac resynchronization therapy is related to the extent of left ventricular reverse remodeling at midterm follow-up. J Am Coll Cardiol 53, 483–90 (2009).
Rocchi, G. et al. Exercise stress echocardiography is superior to rest echocardiography in predicting left ventricular reverse remodelling and functional improvement after cardiac resynchronization therapy. Eur Heart J 30, 89–97 (2009).
Brignole, M. et al. ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: the Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Eur Heart J 34, 2281–329 (2013).
Kydd, A. C. et al. Prognostic benefit of optimum left ventricular lead position in cardiac resynchronization therapy: follow-up of the TARGET Study Cohort (Targeted Left Ventricular Lead Placement to guide Cardiac Resynchronization Therapy). JACC Heart Fail 2, 205–12 (2014).
Geller, L. et al. Long-term experience with coronary sinus side branch stenting to stabilize left ventricular electrode position. Heart Rhythm 8, 845–50 (2011).
van Rees, J. B. et al. Implantation-related complications of implantable cardioverter-defibrillators and cardiac resynchronization therapy devices: a systematic review of randomized clinical trials. J Am Coll Cardiol 58, 995–1000 (2011).
Biffi, M. et al. Left ventricular lead stabilization to retain cardiac resynchronization therapy at long term: when is it advisable? Europace 16, 533–40 (2014).
Forleo, G. B. et al. Hospitalization rates and associated cost analysis of cardiac resynchronization therapy with an implantable defibrillator and quadripolar vs. bipolar left ventricular leads: a comparative effectiveness study. Europace 17, 101–7 (2015).
Taylor, R. J., Umar, F., Panting, J. R., Stegemann, B. & Leyva, F. Left ventricular lead position, mechanical activation, and myocardial scar in relation to left ventricular reverse remodeling and clinical outcomes after cardiac resynchronization therapy: A feature-tracking and contrast-enhanced cardiovascular magnetic resonance study. Heart Rhythm 13, 481–9 (2016).
Sperzel, J. et al. First prospective, multi-centre clinical experience with a novel left ventricular quadripolar lead. Europace 14, 365–72 (2012).
Umar, F. et al. Haemodynamic effects of cardiac resynchronization therapy using single-vein, three-pole, multipoint left ventricular pacing in patients with ischaemic cardiomyopathy and a left ventricular free wall scar: the MAESTRO study. Europace 18, 1227–34 (2016).
Ziacchi, M., Diemberger, I., Martignani, C., Boriani, G. & Biffi, M. New left ventricular active fixation lead: The experience of lead extraction. Indian Heart J 67(Suppl 3), S97–9 (2015).
Ziacchi, M. et al. Cardiac resynchronization therapy: a comparison among left ventricular bipolar, quadripolar and active fixation leads. Europace June 2017 P1505.
Author information
Authors and Affiliations
Contributions
Ziacchi and Biffi conceived the study design. Corzani, Martignani, Mazzotti, Massaro and Valzania performed all the evaluations. Ziacchi, Biffi and Diemberger wrote the main manuscript text. Ziacchi, Corzani, Massaro prepared figures and tables. Rapezzi and Boriani scientifically reviewed the manuscript. All the authors read and approved the final version.
Corresponding author
Ethics declarations
Competing Interests
M.Z. received speaker’s fees from Medtronic and Boston Scientific; G.B. received speaker’s fees from Boston Scientific, Medtronic and St.Jude and Boehringer Ingelheim; M.B. received speaker’s fees from Medtronic and Biotronik. I.D. received speaker’s fees from Boston Scientific, Biotronik.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ziacchi, M., Diemberger, I., Corzani, A. et al. Cardiac resynchronization therapy: a comparison among left ventricular bipolar, quadripolar and active fixation leads. Sci Rep 8, 13262 (2018). https://doi.org/10.1038/s41598-018-31692-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-31692-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.