Abstract
This population-based cross-sectional study aims to explore the effect of China’s Rural Hospital Delivery Subsidy (RHDS) policy on the utilization of women’s hospital delivery between rural and urban areas. A total of 2398 women were drawn from the Fourth and Fifth National Health Service Surveys, from the Shaanxi province. A generalized linear mixed model was used to analyze the influence of the RHDS policy on the hospital delivery rate. Concentration index and decomposition methods were used to explore the equity of hospital delivery utilization. Prior to introduction of the RHDS policy, the difference in hospital delivery rates was −0.09 (95% CL: −0.16, −0.01) between rural and urban women when adjusting the influence of socioeconomic factors on hospital delivery; after implementation of the policy, the difference was reduced to 0.02 (95% CL: −0.01, 0.06). The horizontal inequity index was reduced from 0.084 to 0.009 for rural women and from 0.070 to 0.011 for urban women. China’s Rural Hospital Delivery Subsidy policy had some positive effect on reducing the gap between rural and urban women’s hospital delivery rate and inequity. However, there is still a pro-rich inequity of hospital delivery utilization for both rural and urban women.
Similar content being viewed by others
Introduction
Maternal mortality rate (MMR) is an important indicator to evaluate the health status in developing countries1. The World Health Organization (WHO) defines maternal death as “the death of a woman during pregnancy or within a period of 42 days after the end of the pregnancy, regardless of the pregnancy duration or location, from any cause related to or aggravated by pregnancy or by measures related to it, but not from accidental or incidental causes”2. Every day, approximately 830 women die from preventable causes related to pregnancy and childbirth, 99% of which occur in developing countries3. In Brazil, MMR is 68 deaths per 100,000 livebirths4; In Bangladesh, MMR is 194 deaths per 100,000 livebirths5; in Ghana, it is 1004 per100,000 livebirths6; in southern Nigeria, it is 1908 per 100,000 livebirths1. In China, the MMR was 27 per 100,000 livebirths7, lower than Brazil, Bangladesh, Ghana and southern Nigeria, but still higher than developed countries (12 per 100,000 livebirths)8. Hospital delivery, where pregnant women give birth to babies in hospital, is promoted as an effective strategy to prevent maternal and perinatal mortality since it is recognized that most obstetric complications occur at the time of delivery and cannot be predicted9.
The Chinese government has made many efforts to improve hospital delivery rates since 1995, such as the “Safe motherhood” and “Reducing maternal mortality and eliminating newborn tetanus” policies10,11. In 2003, three basic medical insurance schemes called “Urban Employee Basic Medical Insurance scheme”, “New Rural Cooperative Medical Scheme” and “Urban Resident Basic Medical Insurance scheme” were introduced and can cover women’s hospital delivery costs partially12. China’s latest health system reform was initiated in April 2009 and one of its aims was to ensure the safety of maternal women. As part of this, a key policy, the Rural Hospital Delivery Subsidy (RHDS) policy for rural women was introduced in September 2009 to narrow the difference between maternal mortality rates existing between urban and rural areas. The RHDS policy is to reimburse hospital delivery fees for rural women, aiming to achieve more than a 95% hospital delivery rate13. It provides 500 Ren Min Bi for each rural woman delivering at hospital and it is combined with New Rural Cooperative Medical Scheme to ease the financial burden of rural hospital delivery14.
Up to now, there have been some published studies supporting the role of the RHDS policy in influencing hospital delivery. Yang et al. found the RHDS policy promoted the hospital delivery services and reduced the regional difference14; Shen et al. observed the rate of hospital delivery increased after implementation of the RHDS policy in western China15; as did the studies of Song et al.16 and Zhang et al. in Sichuan Province17. However, these study data are based on annual reports or local surveys at the level of the county. Whilst county-level reports are valuable, the relationship between RHDS policy and hospital delivery can only be fully understood at the individual level. The data through face-to-face interview can obtain the first-hand information directly, investigators can observe the respondent’s response in a timely manner to get a more complete and accurate information18. However, there is no data available collected through face-to-face interviews to explore the relationship between RHDS policy and hospital delivery. Shaanxi Province, in the west of China, is an appropriate study area because of it’s predominantly rural character and high proportion of poor in the population, the type of area where the policy is needed most. Determining whether this policy has a positive effect on hospital delivery is important local health government strategies to promote the safe and health of maternal and newborns. Equity in healthcare has been a long-term guiding principle of health policy, and inequity remains a major challenge for health care planners and policy makers all over the world. In this study, two representative surveys based on face-to-face interviews are used firstly to explore whether the RHDS policy has made some influence on improving the hospital delivery rate in Shaanxi Province and the specific magnitude of inequity on hospital delivery utilization changes. Finally, we draw preliminary conclusions about whether the Chinese maternal health policies are progressing in the right direction.
Results
Changes of hospital delivery rate
Table 1 presents the basic characteristics between urban women and rural women before and after the introduction of the RHDS policy. Before the policy, the difference in proportion between rural women who had a hospital delivery was 18.57% points (95% CL: 10.75%, 26.40%) lower than that of urban women [46.00% (95% CL: 41.32%, 50.67%) vs. 64.57% (95%CL: 58.30%, 70.85%); χ2 = 20.43, P < 0.001]. After the policy, the difference in rate was reduced to 1.47% (95% CL: 0, 3.98%) between rural and urban women [91.63% (95% CL: 89.94%, 93.33%) vs 93.10% (95%CL: 91.23%, 94.96%); χ2 = 1.26, P = 0.262]. Table 2 shows the results of the differences of Rural Hospital Delivery Subsidy policy on hospital delivery rate before and after RHDS policy by two GLMMs. When adjusting for the influence of women’s age, health score, prenatal visits, chronic disease, health insurance, annual personal expenditure, parity, education and work status on hospital delivery rate in model 2, the difference in hospital delivery rates was −0.09 (95%CL: −0.16, −0.01) between rural and urban women before the policy. After the policy, there was no difference in hospital delivery rates between them (mean difference: 0.02; 95%CL: −0.01, 0.06). This suggests the intervention of RHDS policy had some influence on reducing the gap in hospital delivery rate between rural and urban women.
Equity of hospital delivery utilization
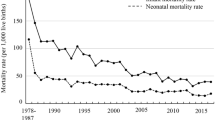
Figure 1 shows that before the RHDS policy, concentration curves both in rural and urban women lay below the line of equality significantly, indicating that hospital delivery was more concentrated among the rich. However, the concentration curves were closer to the line of equality after the policy and the difference in concentration index between urban and rural women was reduced from 0.012 to −0.001 (Table 3). In addition, the concentration index of occurring hospital delivery in rural women decreased significantly (P = 0.020) from 0.082 (95% CL: 0.038, 0.156) to 0.009 (95% CL: −0.001, 0.022). This decreasing trend remains for urban women (P = 0.003): 0.070 (95% CL: 0.020, 0.172) before the policy, and after 0.010 (95% CL: −0.002, 0.024, Table 3). Therefore, the differences in inequality of hospital delivery were reduced after the policy but still favoring the rich both in rural and urban women.
By decomposing the concentration index of the hospital delivery, the socioeconomic-related inequalities were decomposed into relative contributions of each determinant (see Supplementary Tables S1 and S2). Quantifying the corresponding contributions expressed as a percentage of each determinant before and after China’s Rural Hospital Delivery Subsidy policy, most of the socioeconomic inequality in hospital delivery was attributable to annual personal expenditure, at 73.39 and 90.84 for rural women, 61.42 and 85.31 for urban women. Finally, it was computed that horizontal inequity indexes of occurring hospital delivery after the policy are 0.009 for rural women and 0.011 for urban women, evidencing a pro-rich inequity of hospital delivery utilization. In addition, the difference in horizontal inequity indexes of hospital delivery utilization between rural and urban women reduced from 0.014 (0.084 vs 0.070) before the policy to −0.002 (0.009 vs 0.011) after the policy, indicating the inequity gap of hospital delivery utilization had been reduced after the policy (Table 4).
Discussion
China bears some burden of global maternal mortality, the largest part being in the poor western provinces19. Hospital delivery should be completely covered because it has been recognized as an effective strategy in reducing maternal mortality. Although previous studies show women’s higher socioeconomic characteristics (including age, education, work or not, parity and so on) may increase the hospital delivery rate, there is still a gap between urban and rural women20. In this study, we focused on China’s Rural Hospital Delivery Subsidy policy and explored its influence on reducing the gap between rural and urban women’s hospital delivery rate when adjusting for their socioeconomic characteristics. According to these two representative samples of health service surveys, the evidence supports the positive effect of the policy in reducing the difference in hospital delivery rate between rural and urban women. This finding is consistent with the evaluation of RHDS policy studies made by Song et al., Zhang et al., Shen et al. and Yang et al.14,15,16,17. It is the first study based on two representative surveys to explore the relationship between RHDS policy and hospital delivery in Shaanxi Province. A positive direction of the RHDS policy in improving the safe and health of maternal and newborns has been concluded and provides a strong evidence base to inform health policy. Now, the hospital delivery rate for rural women is at a similar level to that of urban women (91.63% vs 93.10%) in Shaanxi Province. Besides, the hospital delivery rate for rural women in Shaanxi was 91.63% in 2013 which, whilst still higher than the rate of 86.3% reported by Liu et al. in 201121, is still lower than the rates in Zhejiang (99.98%)22 and other regions (97.8%) in China16. It is higher than for many developing countries though. In Pakistan, the rate of hospital delivery was 40% for rural areas23 in 2012–2013, and among Indian rural women it was 69.7%, as reported through the Sample Registration System, Registrar General of India24. So, whilst the status of rural and urban hospital delivery rate in Shaanxi was not low, and it had increased in recent years.
China is a huge country with significant rural-urban differences, and rural areas are usually recognized as having a lower quality of health care25. The government conducted the health system reform and introduced a basic health insurance system in order to eliminate the rural-urban disparity in health care. These two policies helped redistribute health resources towards rural areas. However, substantial rural-urban inequality in delivery still exists with more hospital deliveries in urban than in rural areas26,27. One of the encouraging findings in this study is that the difference in rural hospital delivery inequality was also reduced after the introduction of the RHDS policy, demonstrating that implementation of maternal policies since 2009 has led the rural health service utilization development in a positive direction28. However, the concentration indexes of hospital delivery utilization between rural and urban were positive, showing that obvious pro-rich inequalities of hospital delivery utilization still remain, and indicating that a disproportionate share of hospital delivery resources is utilized by wealthier people despite lower need. These results are consistent with findings of many other studies in different parts of the world26,29,30. Therefore, the focus of public health policy still needs to remain on the expansion of the maternal health utilization with an emphasis among poor women.
The study has a few limitations. First, this is an observational study and the determinants of hospital delivery included in this study are limited by the pre-specified questions in the surveys. There could be some potential unobserved confounding factors we did not control for. Second, the imbalanced data before (660) and after (1738) the policy may have two potential impacts on the results and conclusions. One potential impact is the smaller data before the policy are less representative of the study population than that of the larger one after the policy, introducing possible more selection bias into the statistical results related to the data before the policy; another potential impact is the imbalanced data may generate results with less statistical efficiency (eg, larger standard error and less statistical significance) compared with the balanced one. Last but not the least, all the data were collected by a self-report approach, and there may be recall bias. However, it is suggested that, as pregnancy and childbirth are prominent life events, the associated heightened attention is likely to reduce effects of recall bias.
In summary, the evidence supports the positive effect of China’s Rural Hospital Delivery Subsidy policy in reducing the gap in hospital delivery rate and inequity between rural and urban women. However, there is still a pro-rich inequity of hospital delivery utilization for both rural and urban women and efforts should still be made to increase utilization of maternal health services in order to realize the full coverage of hospital delivery and eliminate the rural-urban inequity in health care.
Methods
Study setting and data source
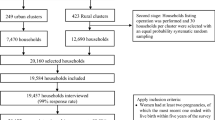
Data were drawn from the 4th (in 2008) and 5th (in 2013) National Health Service Surveys (NHSS) conducted in Shaanxi Province before and after the introduction in 2009 of China’s Rural Hospital Delivery Subsidy (RHDS) policy. The NHSS is a national representative survey conducted by the National Health and Family Planning Commission of China every five years31. Considering the hierarchical structure of Chinese administrative districts and the imbalanced population distributions among the different provinces, a multistage stratified sampling method was used to ensure the samples were representative of the whole population of each province. The structured strategy for sampling in Shaanxi in the 4th and 5th NHSS was introduced by Zhou et al. and Yang et al.32,33.
During the survey, all household members were interviewed face to face individually using a structured household questionnaire (see Supplementary Questionnaire S1 and S2). A total of 18,290 household members in the 4th NHSS and 57,529 household members in the 5th NHSS were collected. For our study, only women who had at least one delivery were selected as the sampling unit of interest in the 4th NHSS. From the 5th NHSS, only women whose last delivery occurred after January 2010 were selected considering the publishing time of RHDS policy (September 2009) and the consistencies in implementation among hospitals and related departments (for example, the health insurance department). Finally, data from 660 women in the 4th NHSS and 1,738 women in the 5th NHSS were utilized for this analysis. Given the hospital delivery rate (88.8%) in rural area of China before the 4th National Health Services Survey34, the sample size was calculated as 510 with a permissible error of 3%, a type I error of 0.05 and an expected 20% non-response rate. Thus, the number of the women from these two cross-sectional studies met the requirement of hospital delivery analysis.
Ethics
This study protocol was approved by the Ethics Committee of Xi’an Jiaotong University Health Science Center (the 4th NHSS Approval No. 2014–204 and the 5th NHSS Approval No. 2015-644). In addition, the study was in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Verbal informed consent was obtained by NHSS surveyors from each participant before the original survey.
Main outcome and predictor variables
In the household questionnaire of the 4th and 5th NHSS, women were asked to describe the type of delivery institution from six category options: county hospital and above, maternal and child health care institution, township health center, community health center, village clinic and at home. According to China’s status for medical institutions after December 2009, we divided them into two groups: ≥secondary institution (including county hospital and above, maternal and child health care institution) and ≤primary institution (including township health center, community health center, village clinic and at home). Women who had a delivery at ≥secondary institution were identified as having hospital delivery. The settings characterized as primary institutions were considered to lack sufficient equipment, doctors and, or nurses to ensure a safe delivery. The indicator used to measure the effect of the Rural Hospital Delivery Subsidy policy for rural maternal women was the occurrence of hospital delivery (a binary outcome variable). According to the RHDS policy that only rural women could receive a subsidy after a hospital delivery, rural women were selected to be the intervention group. The policy had not yet been implemented among urban women from the 4th NHSS to the 5th NHSS, making the urban women to be an excellent control for this study. It is hypothesized that the occurrence of hospital delivery in rural areas would be increased after implementing the RHDS.
Statistical analysis
Generalized linear mixed models (GLMM) are an extension of generalized linear models and include both fixed and random effects35. The response variable can come from different distributions. In this study, GLMM was employed to analyze the effect of the RHDS policy on hospital delivery after controlling a number of confounding factors. These variables were selected based on previous studies but constrained by the variables collected in the survey16,36,37. The characteristics of the whole variables used are shown in Table 1. The variables policy, site, and interaction between policy and site were specified as fixed effects, and the village where women lived as a random effect. Health insurance, health score, annual personal expenditure, parity, chronic disease, prenatal visits, age, education, work were covariates. In a GLMM, the linear prediction η is the combination of the fixed and random effects excluding the residuals.
g(⋅) is the link function which relates the outcome y to the linear predictor η. The equation is as follow:
Here, we use the multiple generalized linear mixed model:
In equation (3), yij is the hospital delivery takes the value of 0 and 1. β0,j is a constant, βpj represent the effects of xpi on y, and εij is a random error. The link function is identity. In this study, interaction effect may exist between RHDS policy and site (urban, rural) when β3,j ≠ 038.
Methods to measure hospital delivery inequality
Concentration index (CI) was employed to measure the extent of income-related inequality of healthcare utilization39. It is defined as twice the area between the concentration curve and the line of equality and ranges from −1 to +140. The formula for computing the concentration index is as follows:
where C stands for concentration index, yi is the hospital delivery status of the ith individual, and Ri is the fractional rank of the ith individual (for weighted data) in terms of the index of annual personal economic status. μ is the (weighted) mean of hospital delivery index and covw denotes the weighted covariance. If C is positive, it means high-income people utilize more hospital delivery than their low-income counterparts. Meanwhile, the C is negative if the low-income group utilizes more hospital delivery than their rich counterparts. When all hospital delivery resources are utilized by low-income group the concentration index will be −1 and it will be +1 when the high-income group are favored in hospital delivery utilization. Hospital delivery is equitably utilized by the poor and the rich when the index is 041.
Horizontal inequity of hospital delivery
Horizontal inequity index (HI) is a summary measure of the magnitude of inequity in the dependent variable, used to measure whether the extent of deviation in the use of healthcare for people is equal for healthcare irrespective of their income42,43. HI is computed by subtracting the contribution of need variables (such as age, health score and having chronic disease or not) from the concentration index of hospital delivery, which is used to measure the equity of hospital delivery. Decomposition methods enable researchers to quantify each determinant’s true contribution to measured income-related inequality with the controlling of other determinants44. Since the outcome variable, hospital delivery, was binary with the range of (0, 1), Probit regression model was used to indirectly standardize the healthcare service utilization. As the standardization of health utilization holds for a linear model of healthcare, we applied the linear approximation to the Probit model to extract marginal effects of each determinant on observed probabilities of the outcome variable. The formula can be written as follows39,45:
G is functional transformation, y is the dependent variable, xji are needs variables, and zki are control variables. Then the standardized need was estimated using the following equation:
where \({\hat{y}}_{i}^{IS}\) is standardized hospital delivery utilization, n is sample size. The more hospital delivery allocated to the needed, the less inequity of hospital delivery utilization.
All questionnaires had been checked for missing data and outliers, then cleaned prior to data analysis. Continuous variables were summarized as means with standard deviations, and categorical variables as number and percentages. Differences in variables between rural and urban areas were compared by either t test or chi-squared test. The statistical analyses were performed using SAS 9.4 (SAS Institute, Cary, NC, USA) and STATA statistical software version 12.0 (StataCorp LP, College station 77845, USA). A two-tailed P value < 0.05 was considered statistically significant.
Availability of materials and data
The datasets analyzed during the current study are not publicly available due to confidential data only be available from the Shaanxi Health and Family Planning Commission for researchers who meet the criteria but are available from the corresponding author on reasonable request. Researchers who want to use these data should contact Jianmin Gao (gaojm@mail.xjtu.edu.cn).
References
Mbachu, I. I. et al. A cross sectional study of maternal near miss and mortality at a rural tertiary centre in southern nigeria. BMC Pregnancy and Childbirth 17, 251, https://doi.org/10.1186/s12884-12017-11436-z. (2017).
Alkema, L. et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet 387, 462–474 (2016).
Tuncalp, O., Hindin, M. J., Adu-Bonsaffoh, K. & Adanu, R. M. Assessment of maternal near-miss and quality of care in a hospital-based study in Accra, Ghana. Int J Gynaecol Obstet 123, https://doi.org/10.1016/j.ijgo.2013.06.003 (2013).
Moreira, D. D. S. & Gubert, M. B. Healthcare and sociodemographic conditions related to severe maternal morbidity in a state representative population, Federal District, Brazil: A cross-sectional study. PLOS ONE 12, e0180849, doi:10.0181371/journal.pone.0180849.eCollection0182017 (2017).
Arifeen, S. E. et al. Maternal mortality in Bangladesh: a Countdown to 2015 country case study. Lancet 384, 1366–1374 (2014).
QY, L., At, O., H, O.-A. & ET, D. Maternal mortality in Ghana: a hospital-based review. Acta Obstet Gynecol Scand 91, 87–92 (2012).
WHO. Maternal and reproductive health, http://gamapserver.who.int/gho/interactive_charts/mdg5_mm/atlas.html (2015).
WHO, Unicef, Unfpa, World Bank Group & United Nations Population Division. Trends in maternal mortality: 1990 to 2015. Estimates by WHO UNICEF UNFPA World Bank Group and the United Nations Population Division (2015).
Pardeshi, G. S., Dalvi, S. S., Pergulwar, C. R., Gite, R. N. & Wanje, S. D. Trends in Choosing Place of Delivery and Assistance during Delivery in Nanded District, Maharashtra, India. Journal of Health Population & Nutrition 29, 71–76 (2011).
United Nations Children’s Fund. Maternal and neonatal tetanus eliminated in China, http://www.unicef.cn/en/index.php?m=content&c=index&a=show&catid=53&id=3653 (2012).
Liu, X., Yan, H. & Wang, D. The evaluation of “Safe Motherhood” program on maternal care utilization in rural western China: a difference in difference approach. Bmc Public Health 10, 1–6 (2010).
Gao, Y., Barclay, L., Kildea, S., Hao, M. & Belton, S. Barriers to increasing hospital birth rates in rural Shanxi Province, China. Reprod Health Matters 18, 35–45 (2010).
National Health and Family Planning Commission of the People’s Republic of China. Announcement on Rural Maternal Hospital Childbirth Subsidy Project by the Ministry of Health, http://www.moh.gov.cn/mohbgt/s9513/200909/42975.shtml (2009).
Yang, Z. & Wang, Z. Status Analysis of the Design and Implementation of Hospital Delivery Subsidy Policy of Rural Pregnant and Lying -in Women. Chinese Health Economics 32, 64–67 (2013).
Shen, J., Xie, Z., Jian, W. & Guo, Y. Evaluation of institutional delivery subsidy program in rural China. Chinese Journal of Health Plicy 5, 54–59 (2012).
Song, P. et al. Barriers to Hospital Deliveries among Ethnic Minority Women with Religious Beliefs in China: A Descriptive Study Using Interviews and Survey Data. International Journal of Environmental Research and Public Health 13, 815, doi:D-NLM: PMC4997501 OTO-NOTNLM (2016).
Zhang, Y. et al. Evaluation of institutional delivery subsidy program in rural Sichuan province. Chinese Journal of Family Planning & Gynecotokology 6, 74–78 (2014).
Yang, M. Research on Questionnaire-based Data Collection and Analysis Master thesis, Shandong Normal University (2011).
Du, Q. et al. The trends in maternal mortality between 1996 and 2009 in Guizhou, China: ethnic differences and associated factors. Journal of Huazhong University of Science and Technology [Medical Sciences] 35, 140–146 (2015).
Gabrysch, S. & Campbell, O. M. Still too far to walk: Literature review of the determinants of delivery service use. Bmc Pregnancy & Childbirth 9, 34 (2009).
Liu, X., Zhou, X., Yan, H. & Wang, D. Use of maternal healthcare services in 10 provinces of rural western China. Int J Gynaecol Obstet 114, 260–264 (2011).
Zhang, W. F., Xu, Y. H., Yang, R. L. & Zhao, Z. Y. Indicators of child health, service utilization and mortality in Zhejiang Province of China, 1998–2011. PLOS ONE 8, e62854, https://doi.org/10.61371/journal.pone.0062854 (2013).
Parveen, Z., Sadiq, M., Abbas, F. & Amir-ud-Din, R. Correlates of home and hospital delivery in Pakistan. J Pak Med Assoc 67, 1166–1172 (2017).
Singh, S. K., Kaur, R., Prabhakar, P., Gupta, M. & Kumar, R. Improving Perinatal Health: Are Indian Health Policies Progressing In The Right Direction? Indian Journal of Community Medicine Official Publication of Indian Association of Preventive & Social Medicine 42, 116–119 (2017).
Meng, Q., Zhang, J., Yan, F., Hoekstra, E. J. & Zhuo, J. One country, two worlds - the health disparity in China. Glob Public Health 7, 124–136 (2012).
Liu, X., Gao, W. & Yan, H. Measuring and decomposing the inequality of maternal health services utilization in western rural China. BMC Health Serv Res 14, 102 (2014).
Phiri, S. Na, Fylkesnes, K., Moland, K. M., Byskov, J. & Kiserud, T. Rural-Urban Inequity in Unmet Obstetric Needs and Functionality of Emergency Obstetric Care Services in a Zambian District. PLOS ONE 11, e0145196, https://doi.org/10.1371/journal.pone.0145196 (2016).
Tian, M. et al. China’s rural public health system performance: a cross-sectional study. PLOS ONE 8, e83822, https://doi.org/10.1371/journal.pone.0083822 (2013).
Mehata, S. et al. Trends and Inequalities in Use of Maternal Health Care Services in Nepal: Strategy in the Search for Improvements. Biomed Res Int 2017, https://doi.org/10.1155/2017/5079234. (2017).
Haider, M. R. et al. Impact of maternal and neonatal health initiatives on inequity in maternal health care utilization in Bangladesh. PLOS ONE 12, e0181408, doi:10.0181371/journal.pone.0181408 (2017).
Gao, J., Tang, S., Tolhurst, R. & Rao, K. Changing access to health services in urban China: implications for equity. Health Policy Plan 16, 302–312 (2001).
Zhou, Z. et al. The effect of urban basic medical insurance on health service utilisation in Shaanxi Province, China: a comparison of two schemes. Plos One 9, e94909, https://doi.org/10.1371/journal.pone.0094909 (2014).
Yang, X. et al. Assessing the Effects of the New Cooperative Medical Scheme on Alleviating the Health Payment-Induced Poverty in Shaanxi Province, China. Plos One 11, e0157918, https://doi.org/10.1371/journal.pone.0157918 (2016).
Zhang, Y. et al. Secular trends of institutional delivery rate in China from1996 to 2015. Zhonghua yi xue za zhi 97, 1337–1342 (2017).
Wang, D. In Interaction. Clinical Trials: A Practical Guide to Design, Analysis and Reporting (ed. A Bakhai) 496pp (ReMEDICA, 2006).
Friedman, A. M., Ananth, C. V., Huang, Y., D’Alton, M. E. & Wright, J. D. Hospital delivery volume, severe obstetrical morbidity, and failure to rescue. American Journal of Obstetrics and Gynecology 215, 795.e791–795.e714, https://doi.org/10.1016/j.ajog.2016.07.039 (2016).
Seraphin, M. N. et al. Determinants of institutional delivery among women of childbearing age in rural Haiti. Matern Child Health J 19, 1400–1407 (2015).
Gen, Z. & Hu, Y. Statistical inference of interaction. Zhong Hua Liu Xing Bing Xue Za Zhi 23, 221–224 (2002).
Zhou, Z. et al. Assessing equity of healthcare utilization in rural China: results from nationally representative surveys from 1993 to 2008. International Journal for Equity in Health 12, 34 (2013).
Wagstaff, A. The bounds of the concentration index when the variable of interest is binary, with an application to immunization inequality. Health Economics 14, 429–432 (2005).
Pathak, P. K., Singh, A. & Subramanian, S. V. Economic Inequalities in Maternal Health Care: Prenatal Care and Skilled Birth Attendance in India, 1992–2006. PLOS ONE 5, e13593 (2010).
Almeida, G. & Sarti, F. M. Measuring income related inequality in health: standardisation and the partial concentration index. Revista Panamericana De Salud Pública 33, 83–89 (2013).
Wagstaff, A. & Doorslaer, E. V. Measuring and Testing for Inequity in the Delivery of Health Care. Journal of Human Resources 35, 716–733 (2000).
Wagstaff, A., Van, D. E. & Watanabe, N. On decomposing the causes of health sector inequalities with an application to malnutrition inequalities in Vietnam. Washington D 112, 207–223 (2001).
Kien, V. D., Van Minh, H., Giang, K. B., Weinehall, L. & Ng, N. Horizontal inequity in public health care service utilization for non-communicable diseases in urban Vietnam. Global Health Action 7, 24919, https://doi.org/10.3402/gha.v7.24919 (2014).
Acknowledgements
This study was funded by the Project of Shaanxi Social Science Foundation (2017S024), Research Program of Shaanxi Soft Science (2015KRM117), Shaanxi provincial youth star of science and technology and China Medical Board (15–227). We express our appreciation to all participants in this study for their participation and co-operation, to the leaders and staffs of Shaanxi Health and Family Planning Commission, to the guiders from the sample counties for their co-operation and organization in the data collection.
Author information
Authors and Affiliations
Contributions
Conceived and designed the study: X.F., Y.X. and Z.Z. Collected the data: J.G. and Z.Z. Conducted the data analysis and prepared the manuscript: X.F., W.D., M.S. and S.D. All authors critically reviewed and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fan, X., Xu, Y., Stewart, M. et al. Effect of China’s maternal health policy on improving rural hospital delivery: Evidence from two cross-sectional surveys. Sci Rep 8, 12326 (2018). https://doi.org/10.1038/s41598-018-29830-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-29830-8
This article is cited by
-
Comparison of inequity in health-related quality of life among unemployed and employed individuals in China
BMC Public Health (2021)
-
Maternal mortality ratio in China from 1990 to 2019: trends, causes and correlations
BMC Public Health (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.