Abstract
Angiopoietin-like protein 4 (ANGPTL4) is a circulating protein involved in the regulation of adipose tissue metabolism. However, its role in obesity and pregnancy is unknown. To evaluate the relationship between gestational weight gain (GWG) and circulating concentrations of ANGPTL4 in pregnant women with overweight and obesity, weight gain and fasting maternal blood samples of thirty-one pregnant women was drawn at 15, 24 and 32 weeks of gestation. ANGPTL4 concentrations continuously rose throughout gestation, whereas VEGF and leptin did not show the same trend. NEFA and glycerol concentrations remained stable during pregnancy. In contrast, total concentrations of saturated, monounsaturated and n-6 fatty acids, but not n-3 fatty acids, increased with pregnancy. In multiple regression analysis, the increase in plasma ANGPTL4 and decrease in linoleic acid concentrations were the most significant predictors of GWG, although only ANGPTL4 was significantly associated with the weight gain from early pregnancy (area under the ROC curve was 0.80 p < 0.01(95% CI 0.61–0.99)). In conclusion, in pregnant women with overweight and obesity, an increase in plasma ANGPTL4 concentrations throughout pregnancy is positively associated with GWG and could be used as an early marker of increased susceptibility to excess gestational weight gain.
Similar content being viewed by others
Introduction
Throughout normal pregnancy there are major changes in maternal lipid metabolism including maternal hyperlipidemia, but how these changes affect gain of maternal fat mass and fetal growth is not completely understood1. The early stages of pregnancy are characterized by an anabolic condition that facilitates the accumulation of lipids in maternal depots. From studies in rats it is known that maternal hyperphagia, increased concentrations of insulin in the blood and unchanged or increased insulin sensitivity during early pregnancy result in increased synthesis of fatty acids by adipose tissue2. Also an increase in adipose tissue lipoprotein lipase (LPL) activity in early pregnancy3 enables an increased uptake of circulating triacylglycerols (TAG) by adipose tissue. Both these changes also seem to take place in human pregnancies and explain the enlargement of maternal fat depots during this stage of pregnancy4,5.
LPL activity is primarily governed by complex post-translational mechanisms in response to energy requirements and hormonal changes. Angiopoietin-like 4 (ANGPTL4) protein is involved in the regulation of LPL activity, preventing dimerization and subsequent activation of the enzyme6, although the exact mechanism is still debated. In mouse models, treatment with – or over-expression of – ANGPTL4 led to an increase in circulating TAG7, while in ANGPTL4 knockout mice or in those treated with anti-ANGPTL4 antibody, the concentrations of plasma TAG are low8. It has also been proposed that ANGPTL4 is a powerful regulator of lipid metabolism and adiposity9, although its role in human adipose tissue development is not well understood. Recently, we reported that in both well-controlled gestational diabetes mellitus (GDM) and healthy control women, decreased maternal ANGPTL4 concentrations is associated with increased neonatal fat mass although its concentrations in cord blood serum were independent of neonatal fat mass10. Human studies produced inconsistent findings regarding the notion of ANGPTL4 to act as a signal preventing fat storage, and there are also studies that failed to find an association between ANGPTL4 and TAG or non-esterified fatty acid (NEFA) concentrations11,12. Moreover, serum ANGPTL4 concentrations has been found higher in obese subjects without/with type 2 diabetes mellitus relative to control subjects13, and variants of ANGPTL4 are associated with lower plasma TAG and higher waist circumference14. Recently, it has been found that ANGPTL4 is upregulated in human adipocytes in response to hypoxia15,16,17, and studies using microarray-based technology have reported that the expression of ANGPTL4 is significantly upregulated in obesity, in early18 and late phases of adipocyte differentiation19, as well as in fat samples from obese subjects20,21.
Maternal obesity is recognized as a major risk factor for adverse pregnancy outcomes, including pre-eclampsia, gestational diabetes, gestational hypertension, cesarean delivery and large-for gestational age infants22. Although increased adipose tissue mass can be considered physiologically normal in pregnancy, excessive weight gain can produce a dysregulation in adipose tissue metabolism. Underlying mechanisms of excessive weight gain are not fully understood. Preventing excessive weight gain during gestation is a general goal, but especially so in women with overweight or obesity prior to pregnancy. In 2009 the Institute of Medicine (IOM) guidelines recommended a total gestational weight gain (GWG) range of 7–11 kg (15–25 lbs) for women with overweight (BMI 25–30 prior to pregnancy), and 5–9 kg (11–20 lbs) for women with obesity prior to pregnancy (BMI ≥ 30)23. Currently, most pregnant women with overweight and obesity exceed the IOM GWG recommendations24. In the last decade various programs have been launched in order to prevent excessive GWG, although they have had limited success in pregnant women with overweight and obesity prior to pregnancy25,26. Moreover, to date, no early metabolic markers of increased susceptibility to excessive weight gain in pregnancy have been identified.
Because of the reported association between plasma ANGPTL4 concentrations and the regulation of lipid metabolism and adiposity, we hypothesize that ANGPTL4 could be part of the mechanism for excessive gestational weight gain in overweight women. Therefore, the purpose of this study was to determine, in a population of pregnant women with overweight and obesity, the relationships between their degree of weight gain at the three trimesters of pregnancy with plasma concentration of ANGPTL4 and different lipid variables.
Results
The characteristics of the study participants with overweight and obesity are shown in Table 1. Only 19% of the pregnant women studied showed a GWG conforming to IOM recommendations based on pre-pregnancy BMI, and more than 50% exceeded the weight that they should have gained by week 32. All neonates had appropriate weight for their gestational age, and no differences in neonatal birth weight related to maternal GWG were observed.
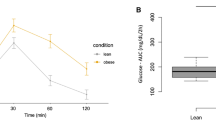
The plasma ANGPTL4 concentration progressively increased throughout gestation in all women (Fig. 1a), with significant changes between all periods. However, other plasma cytokines related to vascularization and growth of adipose tissue, as vascular endothelial growth factor (VEGF) and leptin, did not show the same trend. VEGF concentration only increased at 32 weeks of gestation (Fig. 1b), whereas plasma leptin concentration did not show significant change throughout pregnancy (Fig. 1c). Plasma glucose and RBP4 concentration (an adipokine related to insulin resistance) remained stable during pregnancy, and insulin concentration and HOMA index only increased at 32 weeks of pregnancy (Supplementary Table S1). Neither non-esterified fatty acids (NEFA) nor glycerol concentrations were altered during gestation (Table 2). In contrast, as expected, plasma concentrations of TAG and phospholipids increased with gestational age (Table 2), although the phospholipids concentrations at 24 weeks did not differ from those at 32 weeks. Plasma concentration of both total saturated fatty acids (SFA) and total monounsaturated fatty acid (MUFA) also progressively increased during pregnancy (Table 2), mainly due to rising palmitic acid (PA, 16:0) and oleic acid (OA, 18:1 n-9) concentrations, respectively. Total plasma n-6 polyunsaturated fatty acids (PUFA) and their most abundant representative, linoleic fatty acid (LA, 18:2 n-6), were significantly higher at 24 than at 15 weeks of pregnancy and this difference was maintained until 32 weeks. However, the concentrations of both γ-linolenic (GLNA, 18:3 n-6) and arachidonic (AA, 20:4 n-6) acid remained virtually unchanged throughout gestation. Also the plasma concentration of total n-3 PUFA and of the n-3 fatty acids α-linolenic (ALNA, 18:3 n-3), eicosapentaenoic (EPA, 20:5 n-3) and docosahexaenoic (DHA, 22:6 n-3) acids, remained stable during pregnancy.
Maternal plasma concentrations of (a) ANGPTL4, (b) VEGF and (c) leptin at 15, 24 and 32 weeks of pregnancy, in pregnant women with overweight and obesity. Maternal parameters were adjusted by pre-pregnancy BMI. Different superscripted upper-case letters indicate significant differences (P < 0.001) between different weeks of pregnancy. All values are mean ± SEM. (1)log-transformed for statistical comparisons.
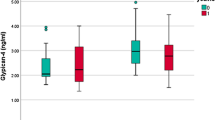
When the individual plasma concentration of these variables were correlated with GWG throughout pregnancy, only ANGPTL4 was significantly and positively associated with GWG at the three time periods of pregnancy (Table 3). At 32 weeks of pregnancy, leptin, stearic (SA,18:0), palmitoleic (POA,16:1 n-7), GLNA (18:3 n-6) and ALNA (18:3 n-3) acid concentrations were positively correlated with GWG, whereas LA (18:2 n-6) was the only variable negatively correlated with GWG in this period. ANGPTL4 was positively correlated with leptin concentration, but contrary to expectations, no association was found between ANGPTL4 and TAG or NEFA in any period studied (data not shown). Moreover, when associations of GWG with all the variables were analyzed by multiple regression, more than 67% of the variation in GWG was significantly and positively associated with the increase in both ANGPTL4 and SA (18:0), and negatively associated with the LA (18:2, n-6) concentrations (Table 4) without significant association with any of the other variables studied. Thus, women with highest GWG had higher plasma concentrations of ANGPTL4 than those with low or normal GWG at the three time periods of pregnancy (Fig. 2a). In contrast, LA (18:2, n-6), was lower in maternal plasma of pregnant women with the highest GWG versus the two other subgroups, although it only reached statistical significance at 15 and 24 weeks (Fig. 2b). Curiously, pregnant women who showed disturbances in GWG (those with low and highest GWG), at early pregnancy had significant lower concentration of glucose, insulin and RBP4, as well as HOMA-IR values than those with the recommended GWG (Supplementary Fig. S1), but these differences disappeared as pregnancy progressed. Only insulin (Supplementary Fig. S1B) and HOMA-IR (Supplementary Fig. S1C) were significantly higher at 32 weeks than those found at earlier times of pregnancy, in pregnant women whose GWG was higher than recommended. Finally, the ability of ANGPTL4, stearic and linoleic acid to predict excessive weight gain was assessed by receiver operating characteristic (ROC) analysis. Plasma ANGPTL4 concentration at week 15 was identified as the only predictor of highest GWG (Fig. 3). This was reflected by the area under the ROC curve (AUC) of 0.80 (standard error = 0.10; 95% CI = 0.61 to 0.99; P < 0.01), indicating a satisfactory discriminatory capacity for ANGPTL4.
Maternal plasma concentrations of (a) ANGPTL4 and (b) linoleic acid (LA, 18:2 n-6) at 15, 24 and 32 weeks of pregnancy, in pregnant women with overweight and obesity classified by GWG conformed to the recommended rate of weight gain during such interval of pregnancy made by the IOM for their particular pre-pregnancy BMI: between 3.4 and 5.5 kg for women with overweight and between 3 and 4.6 kg for women with obesity. Open bars, data pregnant women with GWG < IOM recommendation; filled grey bars, data from pregnant women with GWG within IOM recommendation; filled black bars, data from pregnant women with GWG > IOM recommendation. For each subgroup, different superscripted upper-case letters indicate significant differences (P < 0.001) between different weeks of pregnancy, whereas different superscripted lower-case letters indicate significant differences (P < 0.001) between subgroups at each stage of gestation analyzed (i.e. 15, 24 and 32 weeks of pregnancy). Maternal parameters were adjusted by pre-pregnancy BMI. All values are mean ± SEM. (1)log-transformed for statistical comparisons.
Discussion
Obesity among pregnant women has increased alarmingly in recent years, as has the prevalence of obesity in the general population, and most pregnant women with overweight and obesity in developed countries exceed the IOM recommendations for GWG26. Therefore, an early metabolic marker for increased susceptibility to GWG is highly desirable. This would allow for targeted intervention for the prevention of excessive GWG. Our study shows for the first time that plasma ANGPTL4 concentrations measured in early pregnancy may serve as such a marker in pregnant women with overweight and obesity. Indeed, higher ANGPTL4 concentrations were found as early as 15 weeks of pregnancy in those pregnant women with overweight and obesity that had the highest GWG compared with those with low or appropriate GWG. This result appears against the known role of ANGPTL4 decreasing adipose tissue LPL activity27, but it may be a consequence of the dysregulation of adipose tissue in pregnant women with overweight and obesity, having excessive GWG mediated by the effect of ANGPTL4. Since neither the plasma concentrations of TAG or phospholipids were related with GWG, ANGPTL4 nor leptin, a mechanistic contribution of ANGPTL4 to adipose tissue accretion mediated by LPL in these women appears unlikely. Under non-pregnant conditions such as fasting28, exercise29 and diabetic insulin-resistance10,30, ANGPTL4 has been related to their active adipose tissue lipolysis. However, in agreement with previous studies11, we did not find here any relationship between the plasma concentration of NEFAs with ANGPTL4. In addition, plasma concentrations of NEFAs and glycerol were independent of GWG, not supporting the contention that alterations in lipolysis caused by the changes in ANGPTL4 concentration, could be responsible for the differences observed in GWG.
The results of this study suggest that excessive, i.e. higher than recommended by IOM, weight gain during pregnancy is related to disturbances in maternal adipose tissue. In women with overweight and obesity in pre-pregnancy, the rate at which maternal weight and fat mass increase during gestation is normally lower than in women without obesity31. As is the case in normal pregnancy, GWG in pregnant women with overweight and obesity is known to correlate with maternal fat deposition32. In our study, the concentration of leptin, a marker of adipose tissue accretion in both pregnant and nonpregnant conditions33,34,35 did not change significantly throughout pregnancy, in keeping with the lower tendency for fat mass accumulation of these pregnant women. However, at 32 weeks of gestation leptin concentration was significantly correlated with GWG, indicating that some of the GWG at late pregnancy corresponds to adipose tissue accretion. We found here that it is in pregnant women with GWG higher than recommended where ANGPTL4 concentration was higher already at week 15 of pregnancy. Different from its role in lipid and adipose tissue metabolism, ANGPTL4 can also act as an early pro-angiogenic cytokine inducing adipocyte differentiation and endothelial cell growth necessary for adipose tissue expansion20,36. The effect of ANGPTL4 on adipose tissue accretion would later be reinforced by the synthesis of other cytokines such as VEGF, whose concentration we found to increase in the last trimester of pregnancy. These results are in accordance with other studies reporting that ANGPTL4 expression is significantly upregulated in obesity, in the early18 and the later phases of adipocyte differentiation19,37, and also in adipose tissue cells from subjects with obesity21,36.
In addition to the changes in the plasma concentration of ANGPTL4, we found that GWG in pregnant women with obesity was related negatively to LA (18:2, n-6) and positively to saturated fatty acids, especially SA (18:0), concentrations in plasma. No differences were observed in the plasma concentrations of n-3 fatty acids. Although these results are consistent with other studies that found low plasma LA, but higher concentrations of other n-6 PUFAs, in adults with overweight and obesity (reviewed in38), only few studies have examined the relationship between the fatty acid profile and obesity during pregnancy. In accordance with our results, lower plasma LA but higher arachidonic and palmitic acid concentrations at 20 weeks of pregnancy were previously found in pregnant women with obesity with higher GWG39. However, the mechanistic link between these changes in fatty acid profile and obesity is unclear.
In conclusion, our results support the possibility that plasma ANGPTL4 concentrations could be used as an early indicator of future excessive weight gain during pregnancy. We propose that an early increase in ANGPTL4 production in response to a decrease in linoleic acid concentration and an increased stearic acid concentration could induce angiogenesis and adipogenesis in pregnant women with overweight and obesity, making them more susceptible to excessive GWG during pregnancy.
Research Design and Methods
Study subjects
The sample studied consisted of 31 pregnant women with overweight (pre-pregnancy 25 ≤ BMI < 30) and obesity (pre-pregnancy BMI ≥ 30), who were at increased risk of GDM. The women were recruited in midwife practices and hospitals in Amsterdam, the Netherlands, between January 2007 and January 2011, as has been described in detail previously40. Women were considered to be at increased risk of GDM if they had overweight or obesity and had at least one of the following characteristics: (1) history of macrosomia (offspring with a birth weight above the 97th percentile for a given gestational age); (2) history of GDM; or (3) a first-degree relative with type 2 diabetes mellitus. Exclusion criteria included recruitment after 20 weeks of gestation; under 18 years or age; inadequate knowledge of the Dutch language; diagnosis of GDM at baseline; hypertension; pulmonary, cardiac, hepatic or renal impairment; alcohol or drugs abuse and use of medication that affects insulin secretion or insulin sensitivity. For the purpose of this study women with GDM diagnosed during the course of pregnancy were also excluded. All participating mothers gave informed written consent after having received verbal and written information on the study. The study protocol was approved by the Medical Ethics Committee of VU University Center in Amsterdam (2007/133).
Pre-pregnancy weight was self-reported, but maternal body weight throughout gestation was measured by calibrated electronic scales while participants were only wearing indoor clothing and no shoes. Maternal height was measured (in bare feet) by a wall-mounted height scale to calculate the body mass index.
Gestational weight gain was defined as the weight gained between the measurements at 15 and 32 weeks. Conforming with the IOM recommendations23, an adequate gestational weight during this interval was between 3.4 and 5.5 kg for overweight women and between 3 and 4.6 kg for women with obesity.
Blood samples
Maternal blood samples were drawn in heparinized tubes from the antecubital vein after the participant had fasted for at least 10 h. Maternal blood samples were centrifuged (1500 × g at 4C for 25 min) and aliquots of plasma were immediately stored at −80C until analysis. None of the samples used in the study showed hemolysis.
Analytical determinations
Plasma ANGPTL4 (USCN Life Science, Wuhan, China; intra-assay variations of <10% and inter-assay variation of <12%), leptin (eBioscience, San Diego CA, USA; intra-assay variation 5.7% and inter-assay variation 6.9%), retinol binding protein-4 (RBP4) (AdipoGen, Seoul, Korea; intra-assay variation 3.4% and inter-assay variation 7.1%), and VEGF (IBL-Clontech, Gunma, Japan; intra-assay variation 5.9% and inter-assay variation 9.4%) were determined using sandwich ELISA kits. Plasma insulin was measured by an immunometric assay (Luminescence, Advia Centaur; Siemens Medical Solutions Diagnostics, Deesfield, Illinois); insulin sensitivity was calculated from the homeostasis model assessment (HOMA). Plasma glucose, TAG (Roche Diagnostics GmbH, Germany), NEFA (Wako Chemicals GmbH, Neuss, Germany) and glycerol (Sigma, St. Louis, MO) were determined enzymatically using commercial kits.
For the analysis of fatty acid profiles, plasma lipids were extracted in chloroform/methanol (2:1 by volume) containing 0.005 % BHT and an internal standard of nonodecenoic acid (19:1). Dried lipid extracts were subjected to methanolysis for 2.5 h at 80 °C in methanol:toluene (4:1 by volume) containing acetyl chloride and the methyl esters were analyzed on a Perkin Elmer gas chromatograph (Autosystem; Norwalk, CT) in the presence of methyl-heptadecanoate (17:0) as a reference standard, as previously reported41.
All methods were performed in accordance with the relevant guidelines and regulations.
Statistics
Results are expressed as means ± SEM. Statistical difference between subgroups was determined by ANOVA, after adjustment for pre-gestational BMI as a possible confounding factor; when differences were statistically significant, multiple comparisons were performed using the Tukey post hoc test. Given their skewed distributions, concentrations of ANGPTL4, VEGF, leptin, TAG, NEFA and glycerol were log-transformed before statistical comparison. Correlations were tested using Pearson’s method with the log-transformed data. To ascertain the independent predictors of gestational weight gain, stepwise multiple regressions with backward selection were performed. To determine the association between the early ANGPTL4 concentration and gestational weight gain higher than recommended, a receiver operating characteristic (ROC) curve was generated. All statistical analyses were performed using a computer software package (SPSS Statistics 24, Chicago, IL, USA). The statistics at p-value < 0.05 was considered significant.
References
Herrera, E. & Ortega-Senovilla, H. Lipid metabolism during pregnancy and its implications for fetal growth. Curr Pharm Biotechnol 15, 24–31, https://doi.org/10.2174/1389201015666140330192345 (2014).
Ramos, P. & Herrera, E. Reversion of insulin resistance in the rat during late pregnancy by 72-h glucose infusion. Am J Physiol 269, E858–863, https://doi.org/10.1152/ajpendo.1995.269.5.E858 (1995).
Knopp, R. H., Boroush, M. A. & O'Sullivan, J. B. Lipid metabolism in pregnancy. II. Postheparin lipolytic acitivity and hypertriglyceridemia in the pregnant rat. Metabolism 24, 481–493, https://doi.org/10.1016/0026-0495(75)90073-6 (1975).
Alvarez, J. J., Montelongo, A., Iglesias, A., Lasuncion, M. A. & Herrera, E. Longitudinal study on lipoprotein profile, high density lipoprotein subclass, and postheparin lipases during gestation in women. J Lipid Res 37, 299–308 (1996).
Kinoshita, T., Shirai, K. & Itoh, M. The level of pre-heparin serum lipoprotein lipase mass at different stages of pregnancy. Clin Chim Acta 337, 153–156, https://doi.org/10.1016/j.cccn.2003.08.002 (2003).
Yau, M. H. et al. A highly conserved motif within the NH2-terminal coiled-coil domain of angiopoietin-like protein 4 confers its inhibitory effects on lipoprotein lipase by disrupting the enzyme dimerization. J Biol Chem 284, 11942–11952, https://doi.org/10.1074/jbc.M809802200 (2009).
Yoshida, K., Shimizugawa, T., Ono, M. & Furukawa, H. Angiopoietin-like protein 4 is a potent hyperlipidemia-inducing factor in mice and inhibitor of lipoprotein lipase. J Lipid Res 43, 1770–1772, https://doi.org/10.1194/jlr.C200010-JLR200 (2002).
Koster, A. et al. Transgenic angiopoietin-like (angptl)4 overexpression and targeted disruption of angptl4 and angptl3: regulation of triglyceride metabolism. Endocrinology 146, 4943–4950, https://doi.org/10.1210/en.2005-0476 (2005).
Mandard, S. et al. The fasting-induced adipose factor/angiopoietin-like protein 4 is physically associated with lipoproteins and governs plasma lipid levels and adiposity. J Biol Chem 281, 934–944, https://doi.org/10.1074/jbc.M506519200 (2006).
Ortega-Senovilla, H., Schaefer-Graf, U., Meitzner, K., Abou-Dakn, M. & Herrera, E. Decreased concentrations of the lipoprotein lipase inhibitor angiopoietin-like protein 4 and increased serum triacylglycerol are associated with increased neonatal fat mass in pregnant women with gestational diabetes mellitus. J Clin Endocrinol Metab 98, 3430–3437, https://doi.org/10.1210/jc.2013-1614 (2013).
Ortega-Senovilla, H. et al. Lack of relationship between cord serum angiopoietin-like protein 4 (ANGPTL4) and lipolytic activity in human neonates born by spontaneous delivery. PloS one 8, e81201 (2013).
Blaedel, T. et al. A randomised, controlled, crossover study of the effect of diet on angiopoietin-like protein 4 (ANGPTL4) through modification of the gut microbiome. J Nutr Sci 5, e45, https://doi.org/10.1017/jns.2016.38 (2016).
Cinkajzlova, A. et al. Angiopoietin-like protein 3 and 4 in obesity, type 2 diabetes mellitus, and malnutrition: the effect of weight reduction and realimentation. Nutr Diabetes 8, 21, https://doi.org/10.1038/s41387-018-0032-2 (2018).
Smart-Halajko, M. C. et al. ANGPTL4 variants E40K and T266M are associated with lower fasting triglyceride levels in Non-Hispanic White Americans from the Look AHEAD Clinical Trial. BMC Med Genet 12, 89–95, https://doi.org/10.1186/1471-2350-12-89 (2011).
Mazzatti, D., Lim, F. L., O'Hara, A., Wood, I. S. & Trayhurn, P. A microarray analysis of the hypoxia-induced modulation of gene expression in human adipocytes. Arch Physiol Biochem 118, 112–120, https://doi.org/10.3109/13813455.2012.654611 (2012).
Drager, L. F. et al. Intermittent hypoxia inhibits clearance of triglyceride-rich lipoproteins and inactivates adipose lipoprotein lipase in a mouse model of sleep apnoea. Eur Heart J 33, 783–790, https://doi.org/10.1093/eurheartj/ehr097 (2012).
Wang, B., Wood, I. S. & Trayhurn, P. Dysregulation of the expression and secretion of inflammation-related adipokines by hypoxia in human adipocytes. Pflugers Arch-Eur J Physiol 455, 479–492, https://doi.org/10.1007/s00424-007-0301-8 (2007).
Yoon, J. C. et al. Peroxisome proliferator-activated receptor gamma target gene encoding a novel angiopoietin-related protein associated with adipose differentiation. Mol Cell Biol 20, 5343–5349, https://doi.org/10.1128/MCB.20.14.5343-5349.2000 (2000).
Yin, C. et al. DNA microarray analysis of genes differentially expressed in adipocyte differentiation. J Biosci. 39, 415–423, https://doi.org/10.1007/s12038-014-9412-5 (2014).
Gealekman, O. et al. Enhanced angiogenesis in obesity and in response to PPARgamma activators through adipocyte VEGF and ANGPTL4 production. Am J Physiol Endocrinol Metab 295, E1056–1064, https://doi.org/10.1152/ajpendo.90345.2008 (2008).
Rodriguez-Acebes, S. et al. Gene expression profiling of subcutaneous adipose tissue in morbid obesity using a focused microarray: distinct expression of cell-cycle- and differentiation-related genes. BMC Med Genomics. 3, 61, https://doi.org/10.1186/1755-8794-3-61 (2010).
Marchi, J., Berg, M., Dencker, A., Olander, E. K. & Begley, C. Risks associated with obesity in pregnancy, for the mother and baby: a systematic review of reviews. Obes Rev 16, 621–638, https://doi.org/10.1111/obr.12288 (2015).
Rasmussen, K. M. & Yaktine, A. L. Weight Gain During Pregnancy: Reexamining the Guidelines. Institute of Medicine (U.S.). Committee to reexamine IOM pregnancy weight guidelines Weight Gain During Pregnancy: Reexamining the Guidelines. xiv, 854–858, https://doi.org/10.17226/12584 (2009).
Deputy, N. P., Sharma, A. J., Kim, S. Y. & Hinkle, S. N. Prevalence and characteristics associated with gestational weight gain adequacy. Obstet Gynecol 125, 773–781, https://doi.org/10.1097/AOG.0000000000000739 (2015).
Skouteris, H. et al. Preventing excessive gestational weight gain: a systematic review of interventions. Obes Rev 11, 757–768, https://doi.org/10.1111/j.1467-789X.2010.00806.x (2010).
Artal, R., Lockwood, C. J. & Brown, H. L. Weight gain recommendations in pregnancy and the obesity epidemic. Obstet Gynecol 115, 152–155, https://doi.org/10.1097/AOG.0b013e3181c51908 (2010).
Dijk, W. & Kersten, S. Regulation of lipoprotein lipase by Angptl4. Trends Endocrinol Metab 25, 146–155, https://doi.org/10.1016/j.tem.2013.12.005 (2014).
Kersten, S. et al. Caloric restriction and exercise increase plasma ANGPTL4 levels in humans via elevated free fatty acids. Arterioscler Thromb Vasc Biol 29, 969–974, https://doi.org/10.1161/ATVBAHA.108.182147 (2009).
Catoire, M. et al. Fatty acid-inducible ANGPTL4 governs lipid metabolic response to exercise. Proc Natl Acad Sci USA 111, E1043–1052, https://doi.org/10.1073/pnas.1400889111 (2014).
Mizutani, N. et al. Reduction of insulin signaling upregulates angiopoietin-like protein 4 through elevated free fatty acids in diabetic mice. Exp Clin Endocrinol Diabetes 120, 139–144, https://doi.org/10.1055/s-0031-1291258 (2012).
Straughen, J. K., Trudeau, S. & Misra, V. K. Changes in adipose tissue distribution during pregnancy in overweight and obese compared with normal weight women. Nutr Diabetes 3, e84, https://doi.org/10.1038/nutd.2013.25 (2013).
Berggren, E. K., Groh-Wargo, S., Presley, L., Hauguel-de Mouzon, S. & Catalano, P. M. Maternal fat, but not lean, mass is increased among overweight/obese women with excess gestational weight gain. Am J Obstet Gynecol. 214(745), e741–745, https://doi.org/10.1016/j.ajog.2015.12.026 (2016).
Sattar, N., Greer, I. A., Pirwani, I., Gibson, J. & Wallace, A. M. Leptin levels in pregnancy: marker for fat accumulation and mobilization? Acta Obstet Gynecol Scand. 77, 278–283, https://doi.org/10.1034/j.1600-0412.1998.770304.x (1998).
Harris, R. B. Direct and indirect effects of leptin on adipocyte metabolism. Biochim Biophys Acta 1842, 414–423, https://doi.org/10.1016/j.bbadis.2013.05.009 (2014).
Okereke, N. C., Huston-Presley, L., Amini, S. B., Kalhan, S. & Catalano, P. M. Longitudinal changes in energy expenditure and body composition in obese women with normal and impaired glucose tolerance. Am J Physiol Endocrinol Metab 287, E472–479, https://doi.org/10.1152/ajpendo.00589.2003 (2004).
Gealekman, O. et al. Depot-specific differences and insufficient subcutaneous adipose tissue angiogenesis in human obesity. Circulation 123, 186–194, https://doi.org/10.1161/CIRCULATIONAHA.110.970145 (2011).
Zhu, S., Cheng, G., Zhu, H. & Guan, G. A study of genes involved in adipocyte differentiation. J Pediatr Endocrinol Metab 28, 93–99, https://doi.org/10.1515/jpem-2014-0002 (2015).
Fekete, K. et al. Long-chain polyunsaturated fatty acid status in obesity: a systematic review and meta-analysis. Obes Rev 16, 488–497, https://doi.org/10.1111/obr.12280 (2015).
Vidakovic, A. J. et al. Body mass index, gestational weight gain and fatty acid concentrations during pregnancy: the Generation R Study. Eur J Epidemiol 30, 1175–1185, https://doi.org/10.1007/s10654-015-0106-6 (2015).
van Poppel, M. N. et al. Longitudinal relationship of physical activity with insulin sensitivity in overweight and obese pregnant women. J Clin Endocrinol Metab 98, 2929–2935, https://doi.org/10.1210/jc.2013-1570 (2013).
Amusquivar, E., Schiffner, S. & Herrera, E. Evaluation of two methods for plasma fatty acid analysis by GC. Eur J Lipid Sci Technol, 711–716, https://doi.org/10.1002/ejlt.201000476 (2011).
Acknowledgements
The authors wish to thank Milagros Morante of Universidad CEU San Pablo for her excellent technical assistance, Nicolette Oostdam for recruitment and collection of the samples, and pp-science-editing.com for editing and linguistic revision of the manuscript. This work has been carried out with the financial support of the Spanish Ministry of Economy and Competitiveness (SAF2012-39273) and Universidad San Pablo-CEU (USPBS APP32016 and MBS08C05).
Author information
Authors and Affiliations
Contributions
H.O.-S. performed analysis and interpretation of data, statistical study and wrote the article; M.N.M.v.P. performed the experimental design, and undertook supervision and critical review of the manuscript; G.D. reviewed the manuscript critically; E.H. also collaborated in the experimental design, and revising the article critically.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ortega-Senovilla, H., van Poppel, M.N.M., Desoye, G. et al. Angiopoietin-like protein 4 (ANGPTL4) is related to gestational weight gain in pregnant women with obesity. Sci Rep 8, 12428 (2018). https://doi.org/10.1038/s41598-018-29731-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-29731-w
This article is cited by
-
Short-chain fatty acids as a link between diet and cardiometabolic risk: a narrative review
Lipids in Health and Disease (2023)
-
Cross-talk between ANGPTL4 gene SNP Rs1044250 and weight management is a risk factor of metabolic syndrome
Journal of Translational Medicine (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.