Abstract
Ventricular arrhythmias (VAs) are the leading cause of sudden cardiac death in patients with myocardial infarction (MI). We sought to compare effects of renal denervation (RDN) and metoprolol on VAs after MI. Fifty-four male Sprague-Dawley rats underwent ligation of left anterior descending coronary artery to induce MI, while 6 rats served as Control. Metoprolol was given 20 mg/kg/day for 5 weeks after MI surgery. RDN/Sham-RDN procedure was performed at 1 week after MI. At 5 weeks after MI, electrical programmed stimulation (EPS) was performed in all groups for evaluation of VAs. After EPS, heart and kidneys were harvested. Compared with MI group, RDN and metoprolol significantly decreased the incidence of VAs, and RDN is superior to metoprolol. Compared with metoprolol group, Masson staining showed that RDN significantly reduced the myocardial fibrosis. Both RDN and metoprolol decreased the protein expression of connexin43 (Cx43) compared with MI group, while only RDN lighted this decrease remarkably. Immunohistochemical staining of Tyrosine hydroxylase (TH) and growth associated protein 43 (GAP43) revealed that RDN and metoprolol had similar effect on reducing densities of sympathetic nerve in infarction border zone. According to this study, RDN is more effective in reducing VAs than metoprolol in ischemic cardiomyopathy model.
Similar content being viewed by others

Introduction
According to World Health Organization statistics, Myocardial infarction (MI) is the leading cause of death in human1. Arrhythmias, especially ventricular arrhythmias (VAs), are the major causes of sudden death in MI patients. Previous studies showed that many factors involved in the pathogenesis of VAs after MI, including the gap junction remodeling2, sympathetic neural remodeling3, cardiac fibrosis4 as well as electrical remodeling5.
Sympathetic nerve remodeling6,7 refers to a series of pathophysiological changes after MI, including myocardial denervation, nerve sprouting, sympathetic over-regeneration and high domination, ultimately developing into electrophysiological heterogeneity. This may form the basis for increased susceptibility of VAs in rats with ischemic cardiomyopathy8.
Connexin, abundant in normal cardiac tissue, plays an important role in the electrical synchronization of cardiomyocyte contraction. After MI, the expression and distribution of connexin in infarcted myocardial tissue become irregular9. Abnormal expression and distribution of connexin results in the gap junction remodeling, which is thought to be an important arrhythmogenic substrate.
Renal denervation (RDN), as a novel and safe method10, is mainly used to treat patients with resistant hypertension11. Besides, RDN also has a variety of roles such as reducing myocardial fibrosis12, promoting angiogenesis after MI13, and improving ventricular remodeling in heart failure. Several clinical studies have shown that RDN can reduce the incidence of arrhythmias14, including ventricular electrical storm15, atrial fibrillation16 and other types of arrhythmias17. Metoprolol, a classical β-blocker, has a positive effect on improving the long-term survival in patients with MI18,19. Many clinical studies showed that metoprolol can reduce the infarcted area20, decrease the incidence of recurrent myocardial ischemia21 and reduce the risk of malignant arrhythmias18. But research on comparison between RDN and metoprolol is insufficient. And the potential mechanistic evaluation remains unclear. In this study, we established MI model to investigate the effect and mechanism of RDN on VAs after MI and compared with metoprolol.
Results
Cardiac function at 1 week
At 1 week post-MI, echocardiography revealed that MI significantly decreased left ventricular ejection fraction (LVEF MI 44.77 ± 3.66% vs. Control 67.80 ± 1.14%, P = 0.0012) and left ventricular fractional shortening (LVFS MI 24.08 ± 1.24% vs. Control 38.96 ± 0.92%, P < 0.0001) compared with control group (Fig. 1). These indicated MI-induced ischemic cardiomyopathy model had been established.
Cardiac function change at 1 week. Transthoracic echocardiography evaluation of (a) EF (b) FS (c) LVDs (d) LVDd (e) IVSs (f) IVSd. (g–j) Representative tracings of echocardiography in each group. (Data were mean ± SEM. *P < 0.05 vs. Control group). LVDs = left ventricular end systolic diameter; LVDd = left ventricular end diastolic diameter; EF = ejection fraction; FS = fractional shortening; IVSs = interventricular septal thickness in systole; IVSd = interventricular septal thickness in diastole.
Cardiac function at 5 weeks
At 5 weeks post-MI, there were 6, 8, 12 and 14 rats survived in control, MI, Met and RDN groups respectively. Compared with MI group, RDN and metoprolol significantly increased LVEF (RDN 56.99 ± 1.50% vs. MI, P < 0.0001; Met 51.36 ± 3.49% vs. MI, P = 0.0468; MI 41.34 ± 2.31%) and LVFS (RDN 32.08 ± 1.65% vs. MI, P = 0.0019; Met 29.10 ± 2.21% vs. MI, P = 0.0551; MI 22.62 ± 1.98% Fig. 2a,b). No significant difference was observed between RDN group and metoprolol group in LVEF (P = 0.1321) and LVFS (P = 0.2815). Furthermore, both RDN and metoprolol significantly decreased left ventricular end diastolic dimension (LVDd RDN 8.12 ± 0.71 mm vs. MI, P < 0.05; Met 8.23 ± 0.42 mm vs. MI, P < 0.05; MI 10.54 ± 0.82 mm) and left ventricular end systolic diameter (LVDs RDN 6.70 ± 0.39 mm vs. MI, P < 0.05; Met 6.69 ± 0.20 mm vs. MI, P < 0.05; MI 8.32 ± 0.49 mm) in comparison with MI group (Fig. 2c,d).
RDN and metoprolol partly restored cardiac function at 5 weeks. Transthoracic echocardiography evaluation of (a) EF (b) FS (c) LVDs (d) LVDd (e) IVSs (f) IVSd. (g–j) Representative tracings of echocardiography in control group, MI group, RDN group and Metoprolol group. (Data were mean ± SEM. *P < 0.05 vs. Control group; &P < 0.05 vs. Met group). LVDs = left ventricular end systolic diameter; LVDd = left ventricular end diastolic diameter; EF = ejection fraction; FS = fractional shortening; IVSs = interventricular septal thickness in systole; IVSd = interventricular septal thickness in diastole.
Effectiveness of RDN
At the end of the study period, Renal tyrosine hydroxylase (TH) staining was analyzed for the effectiveness of RDN. Compared with MI group, both RDN and metoprolol significantly reduced the densities of TH positive regions (RDN vs. MI, P < 0.01; Met vs. MI, P < 0.01). Besides, RDN significantly decreased the level of renal TH expression than metoprolol (Fig. 3). These confirmed the effectiveness of RDN.
RDN significantly reduced renal expression of TH. (a–d) Representative images of immunohistochemical staining of renal TH protein expression in the control group, MI group, Met group and RDN group (magnification ×200). (e) Quantitative analysis suggested that TH expression in RDN group was significantly lower than that in MI group and Met group. (Data were mean ± SEM. *P < 0.05 vs. Control group; #P < 0.05 vs. MI group; &P < 0.05 vs. Met group).
Effects of RDN on incidence of VAs
At 5 weeks post-MI, electrical programmed stimulation (EPS) was performed in all groups. Compared with MI group, RDN and metoprolol significantly decreased the VA inducibility (RDN 3/14 vs. MI 7/8, P < 0.05; Met 6/12 vs. MI 7/8, P < 0.05; Control 1/6). Furthermore, the incidence of VAs was significantly decreased in RDN than Metoprolol group (RDN 3/14 vs. Met 6/12, P < 0.05) (Fig. 4).
RDN significantly reduced the incidence of ventricular arrhythmias. Representative ECG of electrical stimulation, including sinus rhythm (a), ventricular arrhythmias (b) and (c). Ventricular arrhythmias were less easily induced in RDN group rather than in MI group and Met group (d). (*P < 0.05 vs. Control group; #P < 0.05 vs. MI group; &P < 0.05 vs. Met group).
Effects of RDN on fibrosis in ventricle
Masson staining showed that both RDN and metoprolol group significantly reduced the collagen volume fraction (CVF) of left ventricle compared with the MI group (RDN 18.35 ± 1.06% vs. MI 66.21 ± 5.01%, P < 0.0001; Met 33.42 ± 1.47% vs. MI 66.21 ± 5.01%, P < 0.0001). Besides, RDN remarkably decreased CVF than metoprolol (RDN vs. Met, P < 0.0001, Fig. 5).
Both RDN and metoprolol significantly attenuated cardiac fibrosis. (a–d) Representative ventricular fibrosis (in blue) by Masson’s staining of samples from the control group, MI group, Met group and RDN group. (e) Quantitative analysis suggested that CVF in RDN group was significantly lower than that in MI group and Met group. (Data were mean ± SEM. *P < 0.05 vs. Control group; #P < 0.05 vs. MI group; &P < 0.05 vs. Met group).
Effects of RDN on Cx43 and p-Cx43
The localization of connexin was evaluated by immunofluorescence technique. Both RDN and metoprolol could significantly attenuate the chaos of connexin43 (Cx43), while metoprolol was less effective than RDN (Fig. 6a). The protein level of Cx43 and phosphorylated connexin43 (p-Cx43) were examined through western blotting. Compared with the MI group, both RDN and metoprolol significantly increased the relative expression of Cx43 (RDN vs. MI, P < 0.0001; Met vs. MI, P = 0.0001) and p-Cx43 (RDN vs. MI, P = 0.0015; Met vs. MI, P = 0.0018), Moreover, RDN is more effective than metoprolol in the expression of Cx43 (P = 0.039) but not p-Cx43 (P = 0.1577, Fig. 6).
RDN and metoprolol significantly improved distribution and expression of Cx43 and p-Cx43 in the infarcted border zone compared with MI group. The distribution of Cx43 was disrupted in the border-zone of the infarcted area and the chaos of Cx43 was attenuated by RDN and metoprolol. (b) Representative cropped Western blot of Cx43, p-CX43 and ACTIN in heart. (c,d) Quantitative analysis of Cx43 and p-CX43 in heart by Western blot (Data were mean ± SEM. *P < 0.05 vs. Control group; #P < 0.05 vs. MI group; &P < 0.05 vs. Met group).
Effects of RDN on sympathetic neural remodeling
The sympathetic activity in infarcted border zone (IBZ) was evaluated by immunostaining technique. Compared with the control group, MI significantly increased the densities of TH- (MI vs. Control, P < 0.0001) and growth associated protein 43 (GAP43) - (MI vs. Control, P < 0.0001) positive regions. Both RDN and metoprolol could significantly decrease the densities of TH- (RDN vs. MI, P < 0.0001; Met vs. MI, P < 0.0001) and GAP43- (RDN vs. MI, P < 0.0001; Met vs. MI, P < 0.0001) positive regions in comparison with MI group. However, no significant difference was observed between RDN and metoprolol in reducing densities of TH- (RDN vs. Met, P = 0.3532) and GAP43- (RDN vs. Met, P = 0.1221) positive regions (Figs 7 and 8).
Both RDN and metoprolol significantly reduced cardiac expression of TH. (a–d) Representative images of immunohistochemical staining of cardiac TH protein expression in the control group, MI group, Met group and RDN group (magnification ×400). (e) Quantitative analysis suggested that TH expression in RDN group and metoprolol group were significantly lower than that in MI group. (Data were mean ± SEM. *P < 0.05 vs. Control group; #P < 0.05 vs. MI group).
Both RDN and metoprolol significantly reduced cardiac expression of GAP. (a–d) Representative images of immunohistochemical staining of cardiac GAP protein expression in the control group, MI group, Met group and RDN group (magnification ×400). (e) Quantitative analysis suggested that GAP expression in RDN group and metoprolol group was significantly lower than that in MI group. (Data were mean ± SEM. *P < 0.05 vs. Control group; #P < 0.05 vs. MI group).
Discussion
The main findings of this study are as follows: (1) RDN and metoprolol significantly reduced VAs inducibility; (2) RDN and metoprolol decreased myocardial fibrosis; (3) RDN and metoprolol improved Cx43 expression and distribution, as well as sympathetic neural remodeling. RDN effects were not inferior to metoprolol in this ischemic cardiomyopathy model.
Myocardial fibrosis is an important substrate for reentry VAs genesis. In fact, many clinical studies showed that the level of fibrosis is an independent predictive factor for VAs both in ischemic and non-ischemic cardiomyopathy22,23. Our previous study demonstrated that RDN reduced electrical storm in cardiomyopathy patient with ICD, which may be associated with fibrosis24. In patients with Brugada syndrome, VAs are associated to epicardial fibrosis in right ventricular outflow tract, and catheter ablation in this fibrosis area could significantly reduce VAs events25. Fibrosis is a critical pathway in organ injury26. In response to MI, structural remodeling happens in the infarcted regions, with massive deposition of extracellular matrix. After that, cytokines such as TGF-β1 are released and fibroblasts are activated, which could ultimately develop into myocardial scar and cardiac fibrosis26. Myocardial fibrosis is an important substrate for VAs genesis27. Firstly, fibrous tissue could develop into regions of conduction block and form nonuniform anisotropy and slow conduction, which may finally results in reentry substrate for sustained VAs28. Secondly, the abnormal myocytes in regions of interstitial fibrosis might develop spontaneous diastolic depolarization, leading to abnormal automaticity29. Furthermore, fibroblasts also play a direct role in modulating the electrophysiology by acting as obstacles and depolarizing myocytes. Thus, when the fibroblast further increases, the electrical conduction slows down and finally leads to conduction failure27. In our previous studies, we had demonstrated that RDN could significantly attenuate organ fibrosis. In this study, we found that RDN is superior to metoprolol in reducing cardiac fibrosis12,30, which may explain the lower incidence of VAs.
Cx43 is the predominant ventricular gap junction protein with the function of rapidly spreading and coordinating excitation signals for an effective heart contraction31,32. Thus, it is critical for maintaining normal cardiac electrical conduction33. After MI, the de-phosphorylation of Cx43, the reduced expression and the disarrayed distribution of Cx43 act synergistically on conduction abnormalities and reentrant arrhythmias34,35,36. Firstly, the expression of Cx43 influences the susceptibility to VAs37 after MI and the down-regulation of CX43 alter the spread of the impulse of ventricular myocardium. Roell et al.38 reported that engraftment of connexin43-expressing cells can prevent post-infarct arrhythmia. On the contrary, Lerner et al.39 demonstrated that in Cx43-deficient mice, the incidence of VAs increased markedly when coronary artery occluded. Secondly, abnormal distribution of Cx43 in infarct-related myocardium can cause abnormal conduction. After MI, Cx43 arrayed longitudinally along the lateral surfaces of the myocardial cells while normally distributed in intercalated disc40. Those changes not only reduce electrical conductance, but also decrease permeability of chemicals between cardiomyocytes41. Thus, changes of gap junction protein are the basis of arrhythmia after MI42. According to our study, we confirmed that RDN can increase the expression of Cx43 in the IBZ and ameliorate the distribution of Cx43 in the intercalated disc, which led to better coordination and synchronization of electrical activity and restored conduction and contractile function, Thus, RDN can effectively inhibit formation of arrhythmias. The level of Cx43 in the metoprolol-treated group was also partially ameliorated, but inferior to RDN group.
Sympathetic neural remodeling also account for the occurrence of arrhythmias after MI. Firstly, it has been widely recognized that MI could result in degeneration and death of sympathetic fibers in both infarcted area43 and the viable myocardium44. Due to excessive express of nerve growth factor (NGF)45, the degenerative sympathetic nerve could ultimately develop into sympathetic neural remodeling which manifests as cardiac nerve sprouting and sympathetic hyperinnervation46. Secondly, it has been demonstrated that excessive sympathetic activity in heart can directly lead to arrhythmias in both post-MI patients and animal models47. The potential mechanisms may be as follows: On one hand, the heterogeneous of sympathetic transmission after MI contributes to a nonuniform electrophysiologic response, which could create a substrate for VAs48. On the other hand, symptomatic hyperinnervation can also lead to lower ventricular tachycardia (VT) and ventricular fibrillation (VF) threshold, thus contributing to the occurrence of arrhythmias by altering the electrophysiological properties of the innervated myocardium49. In addition, Gu et al.50 also demonstrated that increased sympathetic tone promoted the degradation and de-phosphorylation of Cx43, which may work together and contribute to VAs. The present study found that both RDN and metoprolol can significantly inhibit the densities of TH and GAP43 positive nerve fibers in IBZ, indicating that RDN and metoprolol can effectively inhibit sympathetic neural remodeling in post-MI rats. This may be another potential mechanism to reduce arrhythmias.
Nowadays, the potential of RDN for arrhythmias and the mechanistic evaluation is ongoing. Jackson et al.51 reported that RDN reduces spontaneous VAs in the subacute period after acute MI by inhibiting sympathetic neural remodeling. They demonstrated that in a relatively small infarct size (mean LVEF at 55%), abnormal automaticity in response of increased cardiac sympathetic activity might be the major mechanism. In our study, where infarct size was big and sustained VAs were induced by EPS, the distribution of Cx43 and the formation of scarring may have been another prominent mechanism. After a wide range of infarct size, a large number of gap junction channels close and a region of electrical conduction block forms, leading to delayed arrhythmias52. Chang et al.53 showed that RDN could improve calcium dynamic and decrease susceptibility to arrhythmogenic cardiac alternans by inhibiting sympathetic nerve activity, thereby reducing the incidence of VAs after heart failure. In addition to the sympathetic activity mentioned by Chang et al., intracellular calcium handling is more relevant to cardiac contractile function. Previous study showed that HF destroyed calcium cycling in sarcoplasmic reticulum, further influenced amplitude and duration of calcium transients, resulting in calcium transient alternans and action potential duration alternans54. In the present study, we found that RDN can effectively improve cardiac function after MI and may further modify calcium regulation abnormalities and reduce the incidence of conduction block and VAs, which also supports the findings reported by Chang et al. In addition to these conventional mechanisms, the natriuretic peptide system has become a new target for cardiovascular events. Polhemus et al.55 found that RDN can protect the failing heart via inhibition of neprilysin activity. Diego et al.56 demonstrated that neprilysin inhibition decreased VAs in patients with reduced ejection fraction heart failure. Except renin-angiotensin pathway and adrenergic system, inhibition of neprilysin activity by RDN may be another possible mechanism for the reduction of VAs in rats after MI.
Previous study on the comparison of efficacy of RDN versus β-blocker on VAs was limited to the acute period of MI. Linz et al.57 demonstrated that the effect of RDN on VAs during acute ischemia period was similar to β-blockers. The occurrence of VAs on the early period might result from the triggered activity from Purkinje fibers in ischemic regions in response to increased catecholamine levels58. Hence, RDN might have similar effect with β-blockers on reducing the activity of catecholamine during the early period. But during the subacute period after MI, except the increased activity of catecholamine, VAs could also result from sympathetic neural remodeling, the distribution of Cx4338 and cardiac fibrosis. In conclusion, according to this study, RDN is not inferior to β-blocker in reducing the remodeling of connexin43 and sympathetic nerve after MI.
Limitations
The current study existed several limitations. Firstly, RDN in this study was performed only on the adventitia of the renal artery, which differs from clinical renal artery ablation. Secondly, cardiac dysfunction is one of the predictors of VAs in ischemic cardiomyopathy. In this study, RDN can improve the cardiac function after MI. However, we did not investigate the relationship between cardiac function and VAs. Hence, whether the reduction of VAs benefits from improvements in cardiac function requires further study. Furthermore, despite reported by relevant literature55,56, we did not further confirm the direct effect of RDN on VAs by inhibiting neprilysin.
Conclusions
RDN is effective on reducing VAs inducibility and the effect is not inferior to Metoprolol. The mechanism could be associated with cardiac fibrosis reducing, Cx43 expression regulating and sympathetic nerve remodeling.
Materials and Methods
Animals and Experimental Protocols
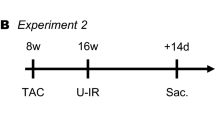
All procedures in this study were approved by the Ethics Committee of Nanjing Medical University. The animal experiments were performed conform the Guide for the Care and Use of Laboratory Animals (National Institutes of Health publication 8th edition, 2011). Sixty six-week male Sprague-Dawley rats (200–220 g) were provided by Nanjing Medical University Laboratory Animal Center. After a one-week-adaption, 54 rats underwent ligation of left anterior descending coronary artery to induce MI, while 6 rats underwent sham-MI surgery served as the control. Subsequently, 47 surviving MI rats were randomly divided into 3 groups by random number method: MI with RDN operation (RDN group, n = 16), MI with metoprolol (metoprolol group, n = 16) and MI with sham-RDN operation (MI group, n = 15). Metoprolol was administrated intragastrically at a dose of 20 mg/kg/day for 5 weeks starting on day 1 after MI surgery59,60. The dosing regimen of metoprolol was based on previous study61. The RDN or Sham-RDN procedure was performed bilaterally 1 week after MI surgery. All the data in this research was collected by double-blind experiment.
Myocardial infarction model
MI model was created as described previously. In brief, the rats were weighted before intraperitoneal injection with 2% sodium pentobarbital (50 mg/kg). After they were anesthetized, the rats were endotracheally intubated and mechanically ventilated. Thoracotomy was performed at the forth intercostal space, then the left anterior descending coronary artery was ligated with a 7–0 silk suture at about 1–2 mm at the starting point of the branch. After ligation, a local pale could be seen at the surface of heart, and then sutured the thoracic cavity and skin. All the rats underwent myocardial infarction were given penicillin intramuscularly in order to prevent infection. Rats in control group only underwent thoracotomy without ligation. All MI procedures were performed by the same operators.
Renal denervation model
One week after MI surgery, rats in RDN group underwent the second operation. RDN was implemented as described previously. The rats were anesthetized by intraperitoneal injection with 2% sodium pentobarbital (50 mg/kg). Next, the skin was cut at about 2 transverse fingers below the costalspinal angle in order to find the kidneys and perirenal adipose tissue. And then, all visible nerves were severed. After that, 20% phenol in an alcohol solution were painted on renal vessels to destroy the remaining nerves. Same procedures were performed on the rats in sham group just without the destruction of the nerves. The RDN/sham-RDN procedure was conducted by the same operators.
Electrical Programmed Stimulation
Five weeks post MI, rats underwent ventricular electrical programmed stimulation before sacrificed. After anesthetized by intraperitoneal injection with 2% sodium pentobarbital (50 mg/kg), the rat was recorded electrocardiography by three needle electrodes placed on right upper limb and legs. And then, the EPS was used to stimulate the left ventricular apex of the heart through a bipolar electrode and the incidence of VAs was investigated. By a cycle length of 140 ms, the threshold potential for stable pacing was gained. Pacing was started with twice as much as the threshold and the cycle length of 140 ms, which was the interval of 8 stimulus (S1). An extra stimulus (S2) was applied until failed to induce ventricular depolarization, while the interval between S1 and S2 was progressively shortened by 10 ms. The operators were blinded to the treatment of the rats.
Echocardiography
Echocardiography was performed at week 1 and week 5 before RDN and EPS, respectively. After the rats were anesthetized with isoflurane, the structure and function were evaluated by Vevo2100 (VisualSonics, Canada) system equipped with a MS-250, 16.0–21.0 MHZ imaging transducer. The investigators were blinded to the treatment of the rats.
Histological analysis
Rats were sacrificed immediately after EPS. The heart and bilateral kidneys were taken after perfusion with phosphate-buffered saline and washed with phosphate buffered saline. The heart was cut horizontally along the long axis at the pale area of infarct and fixed with 4% paraformaldehyde for 24 hours. The longitudinal kidney was also cut along the long axis incision and fixed with 4% paraformaldehyde for 24 hours. After being fixed, dehydration, and paraffin embedding, the heart and kidney were made into pathological sections. Hearts were subjected to Masson’s trichrome staining, TH staining and GAP43 staining. Kidneys were subjected to tyrosine hydroxylase staining. After staining, they were observed under a normal light microscope and six representative fields were randomly selected for analysis by Image-Pro Plus 6.0.
Immunofluorescence labelling
Immunofluorescence labelling was used to investigate the distribution of Cx43 in the infarcted border zone. The samples were evaluated under a fluorescence microscope (Nikon, Japan).
Western Blot
Protein expression of Cx43 (Abnova, China) and p-Cx43 (Abnova, China) in myocardial tissue were detected by western blotting technique. After the heart samples were lysed in lysis buffer (Abnova, China), the protein concentrations were determined using the BCA method as previously. ACTIN (Abnova, China) was used to normalize protein levels.
Statistical analysis
SPSS 16.0 software was used for statistical analysis, and GraphPad Prism5 software was for mapping. Quantitative data were shown as mean ± SEM, for two-group comparison, data were analyzed with two-tailed unpaired t tests, for multiple-groups comparisons, data were performed using one-way ANOVA followed by LSD test. Qualitative data were analyzed with Fisher exact test. P < 0.05 was considered statistically significant.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Thom, T. et al. Heart disease and stroke statistics–2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 113, e85–151, https://doi.org/10.1161/circulationaha.105.171600 (2006).
Chu, M. et al. Increased Cardiac Arrhythmogenesis Associated With Gap Junction Remodeling With Upregulation of RNA-Binding Protein FXR1. Circulation 137, 605–618, https://doi.org/10.1161/circulationaha.117.028976 (2018).
Cardiac innervation and sudden cardiac death. 116, 2005–2019, https://doi.org/10.1161/circresaha.116.304679 (2015).
de Haan, S. et al. Scar size and characteristics assessed by CMR predict ventricular arrhythmias in ischaemic cardiomyopathy: comparison of previously validated models. Heart (British Cardiac Society) 97, 1951–1956, https://doi.org/10.1136/heartjnl-2011-300060 (2011).
Yamada, S. et al. Impact of Renal Denervation on Atrial Arrhythmogenic Substrate in Ischemic Model of Heart Failure. Journal of the American Heart Association 7, https://doi.org/10.1161/jaha.117.007312 (2018).
Li, Z. et al. The effect of the left stellate ganglion on sympathetic neural remodeling of the left atrium in rats following myocardial infarction. Pacing and clinical electrophysiology: PACE 38, 107–114, https://doi.org/10.1111/pace.12513 (2015).
Xu, B. et al. Intermedin improves cardiac function and sympathetic neural remodeling in a rat model of post myocardial infarction heart failure. Mol Med Rep 16, 1723–1730, https://doi.org/10.3892/mmr.2017.6776 (2017).
Yang, N. et al. Atorvastatin attenuates sympathetic hyperinnervation together with the augmentation of M2 macrophages in rats postmyocardial infarction. Cardiovascular therapeutics 34, 234–244, https://doi.org/10.1111/1755-5922.12193 (2016).
Gui, Y. J. et al. Soluble epoxide hydrolase inhibitors, t-AUCB, regulated microRNA-1 and its target genes in myocardial infarction mice. Oncotarget 8, 94635–94649, https://doi.org/10.18632/oncotarget.21831 (2017).
Esler, M. D. et al. Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 Trial): a randomised controlled trial. Lancet (London, England) 376, 1903–1909, https://doi.org/10.1016/s0140-6736(10)62039-9 (2010).
Krum, H. et al. Catheter-based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof-of-principle cohort study. Lancet (London, England) 373, 1275–1281, https://doi.org/10.1016/s0140-6736(09)60566-3 (2009).
Wang, K. et al. Renal Denervation Attenuates Multi-Organ Fibrosis and Improves Vascular Remodeling in Rats with Transverse Aortic Constriction Induced Cardiomyopathy. Cellular physiology and biochemistry: international journal of experimental cellular physiology, biochemistry, and pharmacology 40, 465–476, https://doi.org/10.1159/000452561 (2016).
Lu, D. et al. Beneficial effects of renal denervation on cardiac angiogenesis in rats with prolonged pressure overload. Acta physiologica (Oxford, England) 220, 47–57, https://doi.org/10.1111/apha.12793 (2017).
Oparil, S. & Schmieder, R. E. New approaches in the treatment of hypertension. Circulation research 116, 1074–1095, https://doi.org/10.1161/circresaha.116.303603 (2015).
Hoffmann, B. A., Steven, D., Willems, S. & Sydow, K. Renal sympathetic denervation as an adjunct to catheter ablation for the treatment of ventricular electrical storm in the setting of acute myocardial infarction. Journal of cardiovascular electrophysiology 24, 1175–1178, https://doi.org/10.1111/jce.12207 (2013).
Hou, Y. et al. Catheter-based renal sympathetic denervation significantly inhibits atrial fibrillation induced by electrical stimulation of the left stellate ganglion and rapid atrial pacing. PloS one 8, e78218, https://doi.org/10.1371/journal.pone.0078218 (2013).
Bradfield, J. S., Vaseghi, M. & Shivkumar, K. Renal denervation for refractory ventricular arrhythmias. Trends in cardiovascular medicine 24, 206–213, https://doi.org/10.1016/j.tcm.2014.05.006 (2014).
Ryden, L. et al. A double-blind trial of metoprolol in acute myocardial infarction. Effects on ventricular tachyarrhythmias. The New England journal of medicine 308, 614–618, https://doi.org/10.1056/nejm198303173081102 (1983).
Roffi, M. et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Giornale italiano di cardiologia (2006) 17, 831–872, https://doi.org/10.1714/2464.25804 (2016).
Chen, Z. M. et al. Early intravenous then oral metoprolol in 45,852 patients with acute myocardial infarction: randomised placebo-controlled trial. Lancet (London, England) 366, 1622–1632, https://doi.org/10.1016/s0140-6736(05)67661-1 (2005).
Andersen, S. S. et al. Mortality and reinfarction among patients using different beta-blockers for secondary prevention after a myocardial infarction. Cardiology 112, 144–150, https://doi.org/10.1159/000143389 (2009).
Leyva, F. et al. Outcomes of Cardiac Resynchronization Therapy With or Without Defibrillation in Patients With Nonischemic Cardiomyopathy. Journal of the American College of Cardiology 70, 1216–1227, https://doi.org/10.1016/j.jacc.2017.07.712 (2017).
Cleland, J. G. F., Halliday, B. P. & Prasad, S. K. Selecting Patients With Nonischemic Dilated Cardiomyopathy for ICDs: Myocardial Function, Fibrosis, and What’s Attached? Journal of the American College of Cardiology 70, 1228–1231, https://doi.org/10.1016/j.jacc.2017.07.748 (2017).
Jiang, Z. et al. Renal Denervation for Ventricular Arrhythmia in Patients with Implantable Cardioverter Defibrillators. Int Heart J 59, 328–332 (2018).
Nademanee, K. et al. Fibrosis, Connexin-43, and Conduction Abnormalities in the Brugada Syndrome. Journal of the American College of Cardiology 66, 1976–1986, https://doi.org/10.1016/j.jacc.2015.08.862 (2015).
Ben Salem, C., Slim, R. & Fathallah, N. Fibrosis–A Common Pathway to Organ Injury and Failure. The New England journal of medicine 373, 95, https://doi.org/10.1056/NEJMc1504848 (2015).
Vasquez, C., Benamer, N. & Morley, G. E. The cardiac fibroblast: functional and electrophysiological considerations in healthy and diseased hearts. Journal of cardiovascular pharmacology 57, 380–388, https://doi.org/10.1097/FJC.0b013e31820cda19 (2011).
Iles, L. et al. Myocardial fibrosis predicts appropriate device therapy in patients with implantable cardioverter-defibrillators for primary prevention of sudden cardiac death. Journal of the American College of Cardiology 57, 821–828, https://doi.org/10.1016/j.jacc.2010.06.062 (2011).
Nakamori, S. et al. Increased myocardial native T1 relaxation time in patients with nonischemic dilated cardiomyopathy with complex ventricular arrhythmia. Journal of magnetic resonance imaging: JMRI 47, 779–786, https://doi.org/10.1002/jmri.25811 (2018).
Liu, Q. et al. Renal Denervation Findings on Cardiac and Renal Fibrosis in Rats with Isoproterenol Induced Cardiomyopathy. Sci Rep 5, 18582, https://doi.org/10.1038/srep18582 (2015).
Litchenberg, W. H. et al. The rate and anisotropy of impulse propagation in the postnatal terminal crest are correlated with remodeling of Cx43 gap junction pattern. Cardiovascular research 45, 379–387 (2000).
Garcia-Dorado, D., Rodriguez-Sinovas, A. & Ruiz-Meana, M. Gap junction-mediated spread of cell injury and death during myocardial ischemia-reperfusion. Cardiovascular research 61, 386–401, https://doi.org/10.1016/j.cardiores.2003.11.039 (2004).
Menk, M. et al. Nucleated red blood cells as predictors of mortality in patients with acute respiratory distress syndrome (ARDS): an observational study. Annals of intensive care 8, 42, https://doi.org/10.1186/s13613-018-0387-5 (2018).
Pervolaraki, E., Dachtler, J. & Anderson, R. A. Ventricular myocardium development and the role of connexins in the human fetal heart. 7, 12272, https://doi.org/10.1038/s41598-017-11129-9 (2017).
Gomes, J. et al. Electrophysiological abnormalities precede overt structural changes in arrhythmogenic right ventricular cardiomyopathy due to mutations in desmoplakin-A combined murine and human study. European heart journal 33, 1942–1953, https://doi.org/10.1093/eurheartj/ehr472 (2012).
Adesse, D. et al. Gap junctions and chagas disease. Advances in parasitology 76, 63–81, https://doi.org/10.1016/b978-0-12-385895-5.00003-7 (2011).
Wang, D., Xing, W., Wang, X. & Zhu, H. Taxol stabilizes gap junctions and reduces ischemic ventricular arrhythmias in rats in vivo. Mol Med Rep 11, 3243–3248 (2015).
Roell, W. et al. Engraftment of connexin 43-expressing cells prevents post-infarct arrhythmia. Nature 450, 819–824 (2007).
Lerner, D., Yamada, K., Schuessler, R. & Saffitz, J. Accelerated onset and increased incidence of ventricular arrhythmias induced by ischemia in Cx43-deficient mice. Circulation 101, 547–552 (2000).
Hussain, W. et al. The Renin-Angiotensin system mediates the effects of stretch on conduction velocity, connexin43 expression, and redistribution in intact ventricle. J. Cardiovasc. Electrophysiol. 21, 1276–1283 (2010).
Kim, E. & Fishman, G. Designer gap junctions that prevent cardiac arrhythmias. Trends Cardiovasc. Med. 23, 33–38 (2013).
Rutledge, C. et al. c-Src kinase inhibition reduces arrhythmia inducibility and connexin43 dysregulation after myocardial infarction. J. Am. Coll. Cardiol. 63, 928–934 (2014).
Zipes, D. P. Influence of myocardial ischemia and infarction on autonomic innervation of heart. Circulation 82, 1095–1105 (1990).
Li, W., Knowlton, D., Van Winkle, D. M. & Habecker, B. A. Infarction alters both the distribution and noradrenergic properties of cardiac sympathetic neurons. American journal of physiology. Heart and circulatory physiology 286, H2229–2236, https://doi.org/10.1152/ajpheart.00768.2003 (2004).
Meloni, M. et al. Nerve growth factor promotes cardiac repair following myocardial infarction. Circulation research 106, 1275–1284, https://doi.org/10.1161/circresaha.109.210088 (2010).
Cao, J. M. et al. Nerve sprouting and sudden cardiac death. Circulation research 86, 816–821 (2000).
Jiang, H. et al. Effects of sympathetic nerve stimulation on ischemia-induced ventricular arrhythmias by modulating connexin43 in rats. Archives of medical research 39, 647–654, https://doi.org/10.1016/j.arcmed.2008.07.005 (2008).
Rubart, M. & Zipes, D. P. Mechanisms of sudden cardiac death. The Journal of clinical investigation 115, 2305–2315, https://doi.org/10.1172/jci26381 (2005).
Ajijola, O. A. et al. Focal myocardial infarction induces global remodeling of cardiac sympathetic innervation: neural remodeling in a spatial context. American journal of physiology. Heart and circulatory physiology 305, H1031–1040, https://doi.org/10.1152/ajpheart.00434.2013 (2013).
Gu, Y. et al. Artemisinin prevents electric remodeling following myocardial infarction possibly by upregulating the expression of connexin 43. Mol Med Rep 10, 1851–1856, https://doi.org/10.3892/mmr.2014.2431 (2014).
Jackson, N. et al. Effects of Renal Artery Denervation on Ventricular Arrhythmias in a Postinfarct Model. Circulation. Cardiovascular interventions 10, e004172, https://doi.org/10.1161/circinterventions.116.004172 (2017).
Donazzan, L., Mahfoud, F., Schirmer, S. H. & Bohm, M. Renal nerve ablation. Heart (British Cardiac Society) 101, 320–328, https://doi.org/10.1136/heartjnl-2013-304702 (2015).
Chang, S.-N. et al. Renal Denervation Decreases Susceptibility to Arrhythmogenic Cardiac Alternans and Ventricular Arrhythmia in a Rat Model of Post-Myocardial Infarction Heart Failure. JACC: Basic to Translational Science 2, 184–193, https://doi.org/10.1016/j.jacbts.2017.01.008 (2017).
Wilson, L. D. et al. Heart failure enhances susceptibility to arrhythmogenic cardiac alternans. Heart rhythm 6, 251–259, https://doi.org/10.1016/j.hrthm.2008.11.008 (2009).
Polhemus, D. J. et al. Renal Sympathetic Denervation Protects the Failing Heart Via Inhibition of Neprilysin Activity in the Kidney. Journal of the American College of Cardiology 70, 2139–2153, https://doi.org/10.1016/j.jacc.2017.08.056 (2017).
de Diego, C. et al. Effects of angiotensin-neprilysin inhibition compared to angiotensin inhibition on ventricular arrhythmias in reduced ejection fraction patients under continuous remote monitoring of implantable defibrillator devices. Heart rhythm 15, 395–402, https://doi.org/10.1016/j.hrthm.2017.11.012 (2018).
Linz, D. et al. Renal denervation suppresses ventricular arrhythmias during acute ventricular ischemia in pigs. Heart rhythm 10, 1525–1530, https://doi.org/10.1016/j.hrthm.2013.07.015 (2013).
Schomig, A., Fischer, S., Kurz, T., Richardt, G. & Schomig, E. Nonexocytotic release of endogenous noradrenaline in the ischemic and anoxic rat heart: mechanism and metabolic requirements. Circulation research 60, 194–205 (1987).
Sorrentino, S. A. et al. Nebivolol exerts beneficial effects on endothelial function, early endothelial progenitor cells, myocardial neovascularization, and left ventricular dysfunction early after myocardial infarction beyond conventional beta1-blockade. Journal of the American College of Cardiology 57, 601–611, https://doi.org/10.1016/j.jacc.2010.09.037 (2011).
Wu, A. & Zhao, M. Effect of Wenxin Granules on Gap Junction and MiR-1 in Rats with Myocardial Infarction. 2017, 3495021, https://doi.org/10.1155/2017/3495021 (2017).
Cannavo, A. et al. beta1-Blockade Prevents Post-Ischemic Myocardial Decompensation Via beta3AR-Dependent Protective Sphingosine-1 Phosphate Signaling. Journal of the American College of Cardiology 70, 182–192, https://doi.org/10.1016/j.jacc.2017.05.020 (2017).
Acknowledgements
This study was supported by the National Nature Science Foundation of China (No. 81770333).
Author information
Authors and Affiliations
Contributions
W.J., C.C. and Q.S. wrote the main manuscript text. J.H., D.L. and Z.J. prepared Figures 1–5, H.X. and J.G. prepared Figures 6–8. All authors reviewed the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jiang, W., Chen, C., Huo, J. et al. Comparison between renal denervation and metoprolol on the susceptibility of ventricular arrhythmias in rats with myocardial infarction. Sci Rep 8, 10206 (2018). https://doi.org/10.1038/s41598-018-28562-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-28562-z
This article is cited by
-
Possible organ-protective effects of renal denervation: insights from basic studies
Hypertension Research (2023)
-
Effects and mechanism of renal denervation on ventricular arrhythmia after acute myocardial infarction in rats
BMC Cardiovascular Disorders (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.